Abstract
Aim
To evaluate the effectiveness of group education, led by health promoters using a guiding style, for people with Type 2 diabetes in public sector community health centres in Cape Town.
Methods
This was a pragmatic clustered randomized controlled trial with 17 randomly selected intervention and 17 control sites. A total of 860 patients with Type 2 diabetes, regardless of therapy used, were recruited from the control sites and 710 were recruited from the intervention sites. The control sites offered usual care, while the intervention sites offered a total of four monthly sessions of group diabetes education led by a health promoter. Participants were measured at baseline and 12 months later. Primary outcomes were diabetes self-care activities, 5% weight loss and a 1% reduction in HbA1c levels. Secondary outcomes were self-efficacy, locus of control, mean blood pressure, mean weight loss, mean waist circumference, mean HbA1c and mean total cholesterol levels and quality of life.
Results
A total of 422 (59.4%) participants in the intervention group did not attend any education sessions. No significant improvement was found in any of the primary or secondary outcomes, apart from a significant reduction in mean systolic (-4.65 mmHg, 95% CI 9.18 to -0.12; P = 0.04) and diastolic blood pressure (-3.30 mmHg, 95% CI -5.35 to -1.26; P = 0.002). Process evaluation suggested that there were problems with finding suitable space for group education in these under-resourced settings, with patient attendance and with full adoption of a guiding style by the health promoters.
Conclusion
The reported effectiveness of group diabetes education offered by more highly trained professionals, in well-resourced settings, was not replicated in the present study, although the reduction in participants’ mean blood pressure is likely to be of clinical significance.
What’s new?
The study adds to the scarce literature on diabetes education in Africa in the face of a growing public health problem in this continent.
The study demonstrates a statistically and clinically significant reduction in participants’ mean blood pressure 1 year after the educational intervention.
The study adds to the small amount of literature on group motivational interviewing type interventions for diabetes.
The study adds to the small amount of literature on the use of lower-/mid-level health workers for diabetes education.
Introduction
The greatest increase in the prevalence of Type 2 diabetes over the next 20 years will be in developing economies 1. South Africa is at the forefront of this increase and has higher baseline prevalence rates than most other African countries 1–3. The International Diabetes Federation estimates that the diabetes prevalence rate in South Africa was > 6% in 2011, which represents 1.9 million people with diabetes 1. In urbanized communities in Cape Town, rates as high as 28% have been reported 2.
Low- and middle-income countries not only have higher predicted increases in prevalence rates, but people diagnosed with diabetes in such countries also have worse glycaemic control than in high-income countries 1. More people with diabetes remain undiagnosed in Africa than in other regions 1. Poor glycaemic control leads to higher rates of complications at a younger age. In South Africa, Type 2 diabetes already contributes substantially to the burden of disease and is the fourth commonest diagnosis seen in ambulatory primary care clinics 4,5.
In Africa, care for diabetes had been overshadowed by vertical programmes focused on HIV/AIDS, tuberculosis, malaria, pneumonia, diarrhoea and other infectious diseases 6,7. Health services are often not organized for the needs of chronic non-communicable diseases, and health workers lack the knowledge and skills to manage such diseases. Health workers themselves are scarce and healthcare requires task-shifting to less trained cadres in order to cope with the workload 6. In South Africa primary care is predominantly offered by clinical nurse practitioners who may have had limited training in non-communicable diseases and are restricted in what they can prescribe independently 5,8.
In Cape Town the quality of care for patients with diabetes has improved from a low baseline over recent years 9. This improvement was in part driven by an appreciative inquiry process that focused on improving the annual review of patients with diabetes and worked with all the staff involved in diabetes care 10. This inquiry process recognized that one of the major deficiencies was a lack of a structured and systematic approach to education. The staff recommended that such an approach be developed to offer group education which would be delivered by health promoters. Health promoters are lay people employed by community health centres who have been trained to deliver health education messages and to counsel patients. Patients’ first choice of health promotion method in Cape Town was individual counselling from a doctor, but they were also open to health promotion in groups and from other health workers 11. Patients prefer education that is given during scheduled routine visits 12. Health promoters in Cape Town have been shown to have a level of knowledge regarding lifestyle modification similar to that of local doctors and much better than that of nurse practitioners 8.
A Cochrane systematic review of group education in diabetes concluded that such education had a significant effect on HbA1c and fasting blood glucose levels, body weight, systolic blood pressure and diabetes knowledge at 6–12 months 13. There was also a reduced need for medication. A more recent meta-analysis of group-based diabetes self-management education similarly concluded that it had a significant effect on HbA1c and fasting blood glucose levels, body weight, diabetes knowledge, self-efficacy, patient satisfaction and self-management skills at 6–12 months 14. There was no effect seen on BMI, blood pressure or lipid profiles. Notably, none of the studies in these reviews was conducted in Africa and most of the studies included highly trained staff such as doctors, specialist nurses or dieticians.
The effects of one-off educational programmes may dissipate in subsequent years if not reinforced and more evidence is needed for the long-term benefits 15; however, the results of lifestyle interventions in the short term are thought to be cost-effective 16. In more highly resourced settings, educational programmes have also been targeted at specific groups of patients with Type 2 diabetes, such as those newly diagnosed and those on insulin. In our context, with no systematic educational programmes in place, the establishment of structured education to raise patients’ basic understanding and to support essential lifestyle modification was the initial goal rather than differentiation into specific target groups. For this reason, the present study included all patients with Type 2 diabetes regardless of duration or type of therapy. The style of counselling is also thought to be important and, in particular, a guiding style that emphasizes collaboration, respect for choice and control, evocation of ideas about change and empathic listening has been highlighted as appropriate to behaviour change counselling. This guiding style is derived from motivational interviewing 17.
The present study aimed to evaluate an approach to group education for people with Type 2 diabetes in public sector community health centres in the Cape Town metropolitan area, where education was delivered by health promoters using a guiding style of communication.
Methods
Group diabetes education was evaluated by means of a pragmatic cluster randomized controlled trial; the full research proposal has been published elsewhere 18. The primary outcome measures were defined as improved diabetes self-care activities, 5% weight loss, and a 1% reduction in HbA1c level. Secondary outcomes were improved diabetes-specific self-efficacy, locus of control, mean blood pressure, mean weight loss, mean waist circumference, mean HbA1c and mean total cholesterol levels, and quality of life.
Patients with Type 2 diabetes attending 45 community health centres in the working class areas of the Cape Town Metropole were the target population. Data from a previous study in the same population (n = 450, 18 clinics) showed that the mean (sd) HbA1c was 73 mmol/mol [8.8% (3.3)] and intraclass correlation 0.1 19. Similarly, the mean (sd) weight was 78.2 (16.7) kg and intraclass correlation 0.05. These figures were used to calculate the sample and cluster size for a 5% weight reduction and a 1% reduction in HbA1c. Based on a level of significance of 0.05 and a power of 0.8 the study required 17 clusters in each arm with 40 patients per cluster. The total sample size, therefore, would be 34 clusters (health centres) and 1360 patients.
Out of 41 community health centres, 34 agreed to participate and were randomly allocated by computer-generated random numbers to either control or intervention groups. All patients with Type 2 diabetes attending the selected health centre on the recruitment days were invited to participate in the study. All patients with Type 2 diabetes who gave consent, regardless of the type of medication (oral and/or insulin) or time since diagnosis, were included. Patients with Type 1 diabetes, those who refused consent, or those who were judged unable to participate (e.g. those who were acutely ill) were excluded.
The intervention consisted of four 60-min sessions of group education that focused on understanding diabetes, living a healthy lifestyle, understanding the medication and avoiding complications. Although the training manual anticipated the sessions would last up to 120 min, in reality the sessions lasted up to 60 min. Health promoters recruited from the district health services were trained over a total of 6 days to deliver each session within the facility, using a guiding style of communication based on motivational interviewing principles and skills 17. Resource materials for group activities were developed for each session and the training manual was published elsewhere 18. The resource materials were made available in English, Afrikaans and Xhosa as necessary. Health promoters discussed the practical implementation during training and each identified a suitable location at their health centre for the group education prior to the intervention.
The patients in the control group received usual education at the health centre. Usual education consisted of ad hoc educational talks in the waiting or club room as well as any individual counselling that providers might have time for in the consultation.
Baseline data collection took place between September and December 2010. The intervention was delivered between October 2010 and April 2011. Follow-up data collection took place between September and December 2011. Patients were recruited on arrival for a routine appointment and nurses were employed to measure weight, waist circumference, blood pressure and to take blood for HbA1c and total cholesterol measurements. Trained field workers administered the questionnaires on self-efficacy, locus of control, self-care activities and quality of life. Data collection tools 20–24 are described more fully in the published protocol 18. After 12 months, the patients were again identified at the health centres during their routine appointments and if necessary were contacted via mobile phone.
It was not possible to blind the health promoters, patients or data collection teams as to whether the health centre was a control or intervention site.
Intention-to-treat analysis evaluated the primary and secondary outcomes. Any missing baseline data was imputed using the Markov chain Monte Carlo approach. Missing status at follow-up was modelled on baseline covariates and randomized group using logistic regression. Inverse probability weighting for not missing at follow-up was used for the final trial analysis. Models for comparing continuous outcomes used linear regression and for categorical outcomes used logistic regression with adjustment for baseline covariates and clustering. The same approach was also used for evaluating the effect of the number of sessions attended in an intervention group-specific analysis.
Results
There were 860 participants with Type 2 diabetes in the control group and 710 in the intervention group, giving a total of 1570 participants in the study overall, as shown in Fig.1. Of these participants, 1158 (73.8%) were women and 411 (26.2%) were men. The mean (sd) age was 56.1 (11.6) years.
Figure 1.
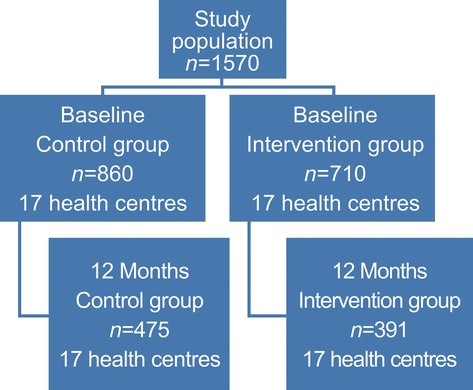
Flowchart of study groups.
Table1 shows the clinical profile of the study groups at baseline and Table2 the baseline scores for self-care activities, psychological factors and quality of life. The two groups were similar at baseline, although the intervention group had worse mean systolic blood pressure and greater mean male waist circumference, as well as lower mean foot care scores. Any differences in baseline measurements between the groups were accounted for in the analysis model.
Table 1.
Clinical profile of the study population at baseline
| Control group N = 860 | Intervention group N = 710 | |
|---|---|---|
| Mean (sd) age, years | 56.4 (11.6) | 55.8 (11.5) |
| Clinical measurements | ||
| Mean (sd) HbA1c, mmol/mol | 78 | 74 |
| Mean (sd)HbA1c,% | 9.3 (2.3) | 8.9 (2.3) |
| Mean (sd) cholesterol, mmol/l | 4.9 (1.3) | 5.0 (1.1) |
| Mean (sd) weight, kg | 83.9 (18.5) | 84.4 (18.7) |
| Mean (sd) waist circumference, cm | 100.3 (14.1) | 101.9 (14.1) |
| Mean (sd) diastolic blood pressure, mmHg | 85.4 (13.0) | 85.9 (11.7) |
| Mean (sd) systolic blood pressure, mmHg | 137.2 (24.3) | 140.2 (22.4) |
| Gender,n (%) | ||
| Male | 209 (24.3) | 202 (28.5) |
| Female | 650 (75.7) | 508 (71.5) |
| Level of control,n (%) | ||
| HbA1c < 53 mmol/mol (7%) | 134 (15.6) | 141 (19.9) |
| Cholesterol < 5.0 mmol/l | 458 (53.3) | 342 (48.2) |
| Diastolic blood pressure < 80 mmHg | 289 (33.6) | 212 (29.9) |
| Systolic blood pressure < 130 mmHg | 345 (40.1) | 245 (34.5) |
| Waist circumference: women, < 82 cm | 40/650 (6.2) | 32/508 (6.3) |
| Waist circumference: men, < 94 cm | 80/209 (38.3) | 57/202 (28.2) |
| Known complications/comorbidities in medical records,n (%) | ||
| Hypertension | 715 (83.1) | 539 (75.9) |
| Hypercholesterolaemia | 279 (32.4) | 239 (33.7) |
| Chronic kidney disease | 26 (3.0) | 12 (1.7) |
| Cataracts | 83 (9.7) | 67 (9.4) |
| Retinopathy | 5 (0.6) | 40 (5.6) |
| Peripheral vascular disease | 1 (0.1) | 13 (1.8) |
| Leg ulcers | 36 (4.2) | 24 (3.4) |
| Neuropathy | 12 (1.4) | 52 (7.3) |
| Amputation | 7 (0.8) | 8 (1.1) |
| Ischaemic heart disease | 26 (3.0) | 22 (3.1) |
| Cardiac failure | 35 (4.1) | 4 (0.6) |
| Stroke | 26 (3.0) | 20 (2.8) |
| Medication,n (%) | ||
| Metformin | 738 (85.8) | 595 (83.8) |
| Glibenclamide | 115 (13.4) | 118 (16.6) |
| Gliclazide | 324 (37.7) | 268 (37.7) |
| Insulin | 228 (26.5) | 213 (30.0) |
| Hydrochlorthiazide | 438 (50.9) | 337 (47.5) |
| Enalapril | 492 (57.2) | 420 (59.2) |
| Amlodipine | 288 (33.5) | 276 (38.9) |
| Simvastatin | 271 (31.5) | 258 (36.3) |
Table 2.
Self-care activities, psychological factors and quality of life at baseline
| Control group, N = 860 | Intervention group, N = 710 | |
|---|---|---|
| Mean (sd) self-care activities | ||
| Use of diet plan, days/week | 4.7 (2.0) | 4.0 (2.2) |
| Exercise, days/week | 3.0 (2.3) | 3.5 (2.4) |
| Foot care, days/week | 5.6 (2.1) | 4.7 (2.6) |
| Use of medication, days/week | 6.9 (0.5) | 6.7 (1.2) |
| Smokers, n (%) | 157 (18.3) | 130 (18.3) |
| Psychological factors, mean (sd) score | ||
| Self-efficacy (scale 1–10) | 3.4 (0.6) | 3.5 (0.7) |
| Internal locus of control (scale 1–6) | 4.8 (0.6) | 4.7 (0.8) |
| External locus of control (scale 1–6) | 4.4 (0.6) | 4.2 (0.9) |
| Chance locus of control (scale 1–6) | 3.7 (1.1) | 3.4 (1.2) |
| Quality of life, mean (sd) scores out of 100 | ||
| Physical functioning | 77.4 (20.8) | 74.8 (21.3) |
| Role functioning | 72.5 (27.9) | 79.2 (26.5) |
| Social functioning | 59.1 (28.3) | 65.9 (32.2) |
| Mental status | 60.2 (11.6) | 59.3 (14.3) |
| Health status | 56.8 (10.8) | 56.5 (13.9) |
| Pain | 53.6 (27.6) | 57.9 (28.1) |
A total of 422 participants (59.4%) in the intervention group did not attend any of the educational sessions. Out of the remaining participants, 70 (9.9%) attended one, 131 (18.4%) attended two, 25 (3.5%) attended three and 62 (8.7%) attended four sessions. Follow-up data were obtained in 475 participants (55.2%) in the control group and 391 participants (55.1%) in the intervention group as shown in Fig.1. There were no differences between the groups in those who dropped out and those who remained, apart from their score for internal locus of control. Those who scored low on their internal locus of control were more likely to drop out of the intervention group (odds ratio 2.6, 95% CI 1.09–6.19; P = 0.03).
There was no significant difference between the groups in reduction of HbA1c level by 1% (odds ratio 1.06, 95% CI 0.64–1.73) or in achievement of 5% weight loss (odds ratio 0.79, 95% CI 0.50–1.24). Table3 shows the results for the other primary and secondary outcomes. There were no significant differences in self-care activities, self-efficacy, locus of control, weight, waist circumference, total cholesterol, quality of life or in the prescription of medication for glycaemia and blood pressure. There was a significant decrease in both systolic and diastolic blood pressure in the intervention group.
Table 3.
Results for primary and secondary outcomes
| Outcomes | Control group, N = 475 | Intervention group, N = 391 | Difference: intervention – control (95% CI) | P |
|---|---|---|---|---|
| Self-care activities, mean (sd) score | ||||
| Physical activity | 4.0 (2.6) | 3.9 (2.3) | -0.25 (-1.13 – 0.63) | 0.574 |
| Use of diet plan | 4.8 (2.2) | 4.6 (2.1) | -0.08 (-0.69 – 0.53) | 0.802 |
| Use of medication | 6.9 (0.9) | 6.8 (0.8) | 0.01 (-0.13 – 0.15) | 0.897 |
| Foot care | 5.7 (1.8) | 5.5 (2.1) | -0.14 (-0.46 – 0.17) | 0.380 |
| Smoking, n/N (%) | 99/483 (20.5) | 78/409 (19.1) | -0.4 (-3.6 to 2.8) | 0.800 |
| Psychological factors, mean (sd) score | ||||
| Self-efficacy | 3.7 (0.6) | 3.7 (0.6) | -0.03 (-0.19 – 0.13) | 0.735 |
| Internal locus of control | 4.8 (0.5) | 4.8 (0.5) | 0.02 (-0.09 – 0.13) | 0.711 |
| External locus of control | 4.5 (0.6) | 4.4 (0.6) | 0.08 (-0.24 – 0.19) | 0.283 |
| Chance locus of control | 3.8 (1.1) | 3.6 (1,1) | -0.18 (-0.56 – 0.19) | 0.344 |
| Clinical measurements, mean (sd) | ||||
| HbA1c, mmol/mol | 71 | 68 | ||
| HbA1c,% | 8.8 (2.2) | 8.4 (2.0) | 0.01 (-0.27 – 0.28) | 0.967 |
| Weight, kg | 83.5 (18.3) | 83.8 (20.2) | -1.01 (-3.32 – 1.30) | 0.392 |
| Waist circumference, cm | 103.1 (13.1) | 103.6 (15.5) | -0.72 (-2.4 – 0.94) | 0.396 |
| Systolic blood pressure, mmHg | 146.1 (24.6) | 143.1 (24.2) | -4.65 (-9.18 – -0.12) | 0.044 |
| Diastolic blood pressure, mmHg | 88.2 (12.8) | 85.0 (11.9) | -3.30 (-5.35 - -1.26) | 0.002 |
| Total cholesterol, mmol/l | 4.9 (1.2) | 4.8 (1.1) | -0.13 (-0.27 – 0.01) | 0.066 |
| Quality-of-life measurements, mean (sd) score | ||||
| Physical functioning | 26.9 (6.0) | 26.4 (6.1) | -0.34 (-1.87- 1.20) | 0.668 |
| Role functioning | 79.1 (26.4) | 81.7 (25.6) | 2.05 (-3.95 – 8.05) | 0.503 |
| Social functioning | 63.7 (30.4) | 63.2 (30.8) | -0.34 (-10.89 – 10.21) | 0.950 |
| Mental health | 60.2 (13.2) | 60.1 (13.7) | -0.08 (-3.86-3.70) | 0.966 |
| General health | 60.0 (11.4) | 58.8 (10.8) | -1.24 (-3.03 – 0.57) | 0.179 |
| Pain | 56.0 (30.5) | 57.7 (29.9) | 0.06 (-5.96- 6.08) | 0.984 |
The mean values for control and intervention in Table3 are the unweighted mean values of the participants who completed the follow-up, whereas the differences reported use the weighted means as per the analysis model.
The intervention group data were also analysed by inverse probability-weighted regression to explore the relationship between the number of sessions attended and the key biological and self-care activity outcomes. This analysis showed that, in the intervention group, those who attended four sessions had a lower systolic (-4.8 mmHg, 95%CI -8.9 to -0.8; P = 0.02) and diastolic blood pressure (-2.5 mmHg, 95% CI -5.1 to 0.1, P = 0.06) compared with those who attended fewer sessions. Those who attended any sessions also had consistent significantly increased physical activity (1.1 days/week, 95% CI 0.2 to 2.0; P = 0.02). Apart from this, however, there was no other relationship seen between the number of sessions and outcomes.
Discussion
Group diabetes education did not have an effect on any of the primary or secondary outcomes after 12 months, apart from a significant reduction in mean systolic and diastolic blood pressure. The effect on blood pressure, however, is an important outcome, given that a reduction in blood pressure lowers cardiovascular risk as well as mortality and has been suggested to be of greater benefit than intensive glucose-lowering, particularly in older people with Type 2 diabetes 25–27.
Group diabetes education has been shown to be effective at 12 months in other contexts and so one must question why the same effects were not seen in the present study and why there was a reduction in blood pressure alone, despite no change in antihypertensive medication 28. Qualitative process evaluation, that is reported on elsewhere, showed that the health promoters struggled to find suitable space for the group education in the health centres 29. In many cases, space was unsuitable in terms of size or interruptions, or was not prioritized by the facility management for this purpose. Health promoters and study co-ordinators also struggled to communicate with patients regarding the dates and times of educational meetings or changes in arrangements. Many patients came from poor communities and had no landline or shared their cell phone with other family members. These factors may have been partly responsible for the poor attendance at the educational sessions and may have reduced the effect within the intention-to-treat analysis.
Another possible explanation is that the health promoters, who were less qualified mid-level health workers, were unable to deliver the intervention effectively. Evaluation of their fidelity to the intervention showed that they were effective at delivering the content and on average delivered 89.6% of the content for ‘understanding diabetes’, 87.5% for ‘understanding medication’, 78.1% for ‘understanding complications’ and 76.7% for ‘healthy lifestyle’ 29. Evaluation of their communication skills showed that overall they achieved a more collaborative style and were able to use open questions effectively; however, they did not demonstrate sufficient listening skills and were not fully consistent in their use of the guiding style 17. Patients who attended the sessions reported that they gained useful new knowledge which led to a change in their behaviour especially with diet, physical activity, medication and foot care 30. The educational material was experienced positively and enhanced recall and understanding. Health promoters were viewed as competent and as using useful communication skills and structuring the material well.
Another study of diabetes education from the Western Cape also identified that patients were not used to attending the health centre when they were well for the purpose of education and were ‘not always happy with their interaction with health care workers; fear, dishonesty, scare-tactics, and burnt-out doctors were all described’. Their expectations and motivation to attend may therefore have been low. That study also found that many staff did not believe in the effectiveness of behaviour change counselling and did not support it 31.
The international literature also suggests that more targeted education, for example only including newly diagnosed patients, or more intensive education with more than four sessions might also improve the impact 13,14.
It is possible that changes in self-care activities could have been detected in the shorter term and this has been demonstrated in an evaluation of a different group diabetes education programme that was initiated in another part of the Western Cape 31.
The study was limited by a high dropout rate in both groups, which necessitated a weighted analysis based on the probability of dropout in the final analysis. The study was also limited by poor attendance and therefore exposure to the intervention, although as this was a pragmatic study this may approximate what could be expected if the programme was actually implemented by the department of health. The study did not have sufficient funding to measure outcomes earlier than 1 year or to measure the full lipogram. Nevertheless, an effect that lasts < 1 year may not be clinically significant and there was no measurable difference in total cholesterol that needed further explanation. Self-care activities were self-reported using questionnaires delivered by the field workers and may have been influenced by social desirability and recall bias. For example, physical activity measured by a pedometer may be greater than that recalled by patients 32, while self-reporting of medication use may be higher than that measured by electronic tagging of medication bottles 33. Nevertheless, recall bias would have applied equally to both groups.
The pragmatic nature of the present study implies that the results should be generalizable to similar urban public sector primary care settings in southern Africa.
Overall, the results of the present study were disappointing and this approach to group diabetes education in our developing country context should be further evaluated. While the rationale for group education remains strong, given the large number of patients and limited human resources, the design of future interventions should be adapted for the infrastructural limitations and logistical barriers to patient retention. Local health policy is now pursuing community-based support groups for the patients who have better glycaemic control, where they can obtain their regular medication and receive education. This would leave a smaller number of patients with poor glycaemic control attending the health centre where they could receive more attention from clinical nurse practitioners or doctors. Another study is underway to explore an approach to individual counselling in the health centre that combines the ‘5As’ (Ask, Alert, Assess, Assist, Arrange) with a guiding style of communication in clinical nurse practitioners and doctors.
In conclusion, a structured programme of group education for patients with diabetes, delivered by health promoters (mid-level health workers) in a low-resource setting, demonstrated no significant effects on the primary outcomes of 5% weight loss, a 1% decrease in HbA1c level or self-care activities. A significant improvement in systolic and diastolic blood pressure was found at 1 year. The success of the educational programme was limited by poor attendance, limited space for group activities and only partial fidelity to the guiding style of interaction.
Funding sources
This project was supported by a BRIDGES Grant from the International Diabetes Federation. BRIDGES, an International Diabetes Federation project, is supported by an educational grant from Lilly Diabetes (ST09-040). Apart from the international funding received from BRIDGES, additional funds were received from the Chronic Diseases Initiative for Africa, of which Stellenbosch University is a member, and directly from strategic research funds within Stellenbosch University.
Competing interests
None declared.
Acknowledgments
We thank Sr Buyelwa Majikela-Dlangamandla and Dr Katherine Murphy who provided help with the training of the health promoters. Ms Unita van Vuuren and Ms Maureen McCrae provided essential support from the Department of Health.
References
- Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- Erasmus RT, Soita DJ, Hassan MS, Blanco-Blanco E, Vergotine Z, Kengne AP, et al. High prevalence of diabetes mellitus and metabolic syndrome in a South African coloured population: Baseline data of a study in Bellville, Cape Town. S Afr Med J. 2012;102:841–844. doi: 10.7196/samj.5670. [DOI] [PubMed] [Google Scholar]
- Peer N, Steyn K, Lombard C, Lambert V, Vythilingum B, Levitt NS. Rising diabetes prevalence among urban-dwelling Black South Africans. PloS One. 2012;7:e43336. doi: 10.1371/journal.pone.0043336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw D, Norman R, Schneider M. A clarion call for action based on refined DALY estimates for South Africa. S Afr Med J. 2007;97:438–440. [PubMed] [Google Scholar]
- Mash B, Fairall L, Adejayan O, Ikpefan O, Kumari J, Mathee S, et al. A morbidity survey of South African primary care. PloS One. 2012a;7:e32358. doi: 10.1371/journal.pone.0032358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economist Intelligence Unit. The future of healthcare in Africa. 2012. Geneva: Economist Intelligence Unit; 2012. [Google Scholar]
- Levitt NS, Steyn K, Dave J, Bradshaw D. Chronic noncommunicable diseases and HIV-AIDS on a collision course: relevance for health care delivery, particularly in low-resource settings—insights from South Africa. Am J Clin Nutr. 2011;94:1690S–1696S. doi: 10.3945/ajcn.111.019075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker W, Steyn NP, Levitt NS, Lombard CJ. They think they know but do they? Misalignment of perceptions of lifestyle modification knowledge among health professionals. Public Health Nutr. 2010;14:1429. doi: 10.1017/S1368980009993272. [DOI] [PubMed] [Google Scholar]
- Govender I, Ehrlich R, Van Vuuren U, De Vries E, Namane M, De Sa A, et al. Clinical audit of diabetes management can improve the quality of care in a resource-limited primary care setting. Int J Qual Health Care. 2012;24:612–618. doi: 10.1093/intqhc/mzs063. [DOI] [PubMed] [Google Scholar]
- Mash B, Levitt N, Van Vuuren U, Martell R. Improving the diabetic annual review in primary care: An appreciative inquiry in the Cape Town District Health Services. S Afr Fam Pract J. 2008;50:50–50d. [Google Scholar]
- Parker W, Steyn NP, Levitt NS, Lombard CJ. Health promotion services for patients having non-comminicable diseases: Feedback from patients and health care providers in Cape Town, South Africa. BMC Public Health. 2012;12:503. doi: 10.1186/1471-2458-12-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorter K, Tuytel G, De Leeuw J, Van Der Bijl J, Bensing J, Rutten G. Preferences and opinions of patients with Type 2 diabetes on education and self-care: a cross-sectional survey. Diabet Med. 2009;27:85–91. doi: 10.1111/j.1464-5491.2009.02886.x. [DOI] [PubMed] [Google Scholar]
- Deakin TA, McShane CE, Cade JE, Williams R. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005a;2:CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- Steinsbekk A, Rygg LØ, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12:213. doi: 10.1186/1472-6963-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khunti K, Gray LJ, Skinner T, Carey ME, Realf K, Dallosso H, et al. Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ. 2012;344:e2333. doi: 10.1136/bmj.e2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs-van derBruggenMAM, van BaalPH, Hoogenveen RT, Feenstra TL, Briggs AH, Lawson K, et al. Cost-effectiveness of lifestyle modification in diabetic patients. Diabetes Care. 2009;32:1453–1458. doi: 10.2337/dc09-0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollnick SMW, Butler C, Rollnick S, Miller W, Butler C. Motivational interviewing in health care: Helping patients change behaviour. London: Guilford Press; 2008. [Google Scholar]
- Mash B, Levitt N, Steyn K, Zwarenstein M, Rollnick S. Effectiveness of a group diabetes education programme in underserved communities in South Africa: pragmatic cluster randomized control trial. BMC Fam Pract. 2012b;13:126. doi: 10.1186/1471-2296-13-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt N, Bradshaw D, Zwarenstein M, Bawa A, Maphumolo S. Audit of public sector primary diabetes care in Cape Town, South Africa: high prevalence of complications, uncontrolled hyperglycaemia, and hypertension. Diabetic Med. 2004;14:1073–1077. doi: 10.1002/(SICI)1096-9136(199712)14:12<1073::AID-DIA498>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- Toobert D, Hampson S, Glasgow R. The summary of diabetes self-care activities measure. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- Trento M, Passera P, Miselli V, Bajardi M, Borgo E, Tomelini M, et al. Evaluation of the locus of control in patients with type 2 diabetes after long-term management by group care. Diabetes Metab. 2006;32:77–81. doi: 10.1016/s1262-3636(07)70250-1. [DOI] [PubMed] [Google Scholar]
- Diabetes Self-Management Study Group. Self-efficacy for diabetes. Available at: http://patienteducation.stanford.edu. Last accessed 2 May 2014.
- Westaway M, Rheeder P, Gumede T. The effect of type 2 diabetes mellitus on health-related quality of life. Curationis. 2001;24:74–78. doi: 10.4102/curationis.v24i1.805. [DOI] [PubMed] [Google Scholar]
- Rubin R, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–218. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Yudkin JS, Richter B, Gale EA. Intensive treatment of hyperglycaemia: what are the objectives? Lancet. 2010;376:1462–1463. doi: 10.1016/S0140-6736(10)61987-3. [DOI] [PubMed] [Google Scholar]
- Kaplan NM. Vascular outcome in type 2 diabetes: an ADVANCE? Lancet. 2007;370:804–805. doi: 10.1016/S0140-6736(07)61304-X. [DOI] [PubMed] [Google Scholar]
- Ferguson LD, Sattar N. Reducing cardiovascular disease risk in type 2 diabetes: is the focus on glycaemia warranted? Diabetes Obes Metab. 2013;15:387–391. doi: 10.1111/dom.12018. [DOI] [PubMed] [Google Scholar]
- Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005b;2:CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- Botes AS, Majikela- DlangamandlaB, Mash R. The ability of health promoters to deliver group diabetes education in South African primary care. Afr J Prm Health Care Fam Med. 2013;5(1):8. ), Art. #484, pages. [Google Scholar]
- Serfontein S, Mash B. Views of patients on a group diabetes education programme using motivational interviewing in South African primary care: Qualitative study. S Afr Fam Pract. 2013;55:453–458. [Google Scholar]
- Van der Does A, Mash R. Evaluation of the “Take Five School”: An education programme for people with Type 2 Diabetes in the Western Cape, South Africa. Prim Care Diabetes. 2013;7:289–295. doi: 10.1016/j.pcd.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Cook I, Alberts M, Lambert EV. Influence of cut-points on patterns of accelerometry-measured free-living physical activity in rural and urban black South African women. J Phys Act Health. 2012;9:300–310. doi: 10.1123/jpah.9.2.300. [DOI] [PubMed] [Google Scholar]
- Shi L, Liu J, Koleva Y, Fonseca V, Kalsekar A, Pawaskar M. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices. Pharmacoeconomics. 2010;28:1097–1107. doi: 10.2165/11537400-000000000-00000. [DOI] [PubMed] [Google Scholar]


