Abstract
According to some lay groups, the nation is experiencing an autism epidemic—a rapid escalation in the prevalence of autism for unknown reasons. However, no sound scientific evidence indicates that the increasing number of diagnosed cases of autism arises from anything other than purposely broadened diagnostic criteria, coupled with deliberately greater public awareness and intentionally improved case finding. Why is the public perception so disconnected from the scientific evidence? In this article we review three primary sources of misunderstanding: lack of awareness about the changing diagnostic criteria, uncritical acceptance of a conclusion illogically drawn in a California-based study, and inattention to a crucial feature of the “child count” data reported annually by the U.S. Department of Education.
Keywords: autism, epidemiology, epidemic
If you have learned anything about autism lately from the popular media, you most likely have learned—erroneously— that there is “a mysterious upsurge” in the prevalence of autism (New York Times, October 20, 2002, Section 4, p. 10), creating a “baffling … outbreak” (CBSnews.com, October 18, 2002), in which new cases are “exploding in number” (Time, May 6, 2002, p. 48), and “no one knows why” (USA Today, May 17, 2004, p. 8D). At least a handful of U.S. Congress members decree on their .govWeb sites that the nation is facing an autism epidemic. Several national media have erroneously concluded that a set of data from California “confirms the autism epidemic,” and the largest autism-advocacy organization in the world has expressed alarm over astronomical percentage increases in the number of autistic children served in the public schools since 1992. However, no sound scientific evidence indicates that the increase in the number of diagnosed cases of autism arises from anything other than intentionally broadened diagnostic criteria, coupled with deliberately greater public awareness and conscientiously improved case finding. How did public perception become so misaligned from scientific evidence? In this article, we review three major sources of misunderstanding.
THE CHANGING DIAGNOSIS OF AUTISM
The phenomenon of autism has existed most likely since the origins of human society. In retrospect, numerous historical figures—for instance, the 18th-century “wild boy of Aveyron”— fit autism diagnostic criteria but were not so diagnosed in their day (Frith, 1989). Only in the 1940s did a constellation of differences in social interaction, communication, and focused interests come to be categorized by Leo Kanner as “autism.” However, another 40 years would elapse before American psychiatric practice incorporated criteria for autism into what was by then the third edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-III; American Psychiatric Association, APA, 1980). Thus, estimates of the prevalence of autism prior to 1980 were based on individual clinicians’ (e.g., Kanner & Eisenberg, 1956) or specific researchers’ (e.g., Rutter, 1978) conceptions—and fluctuated because of factors that continue to introduce variation into current-day estimates (e.g., variation in the size of the population sampled and the manner of identification).
Autism has remained in the DSM (under the title, Pervasive Developmental Disorders), but not without modification through subsequent editions. Whereas the 1980 DSM-III entry required satisfying six mandatory criteria, the more recent 1994 DSM-IV (APA, 1994) offers 16 optional criteria—only half of which need to be met. Moreover, the severe phrasing of the 1980 mandatory criteria contrasts with the more inclusive phrasing of the 1994 optional criteria. For instance, to qualify for a diagnosis according to the 1980 criteria an individual needed to exhibit “a pervasive lack of responsiveness to other people” (emphasis added; APA, 1980, p. 89); in contrast, according to 1994 criteria an individual must demonstrate only “a lack of spontaneous seeking to share … achievements with other people” (APA, 1994, p. 70) and peer relationships less sophisticated than would be predicted by the individual’s developmental level. The 1980 mandatory criteria of “gross deficits in language development” (emphasis added; APA, 1980, p. 89) and “if speech is present, peculiar speech patterns such as immediate and delayed echolalia, metaphorical language, pronominal reversal” (APA, 1980, p. 89) were replaced by the 1994 options of difficulty “sustain[ing] a conversation” (APA, 1994, p. 70) or “lack of varied … social imitative play” (p. 70). “Bizarre responses to various aspects of the environment” (emphasis added; APA, 1980, p. 90) became “persistent preoccupation with parts of objects” (APA, 1994, p. 71).
Furthermore, whereas the earlier 1980 (DSM-III) entry comprised only two diagnostic categories (infantile autism and childhood onset pervasive developmental disorder), the more recent 1994 (DSM-IV) entry comprises five. Three of those five categories connote what is commonly called autism: Autistic Disorder, Pervasive Developmental Disorder Not Otherwise Specified (PDDNOS), and Asperger’s Disorder. Autistic Disorder requires meeting half of the 16 criteria, but Asperger’s Disorder, which did not enter the DSM until 1994, involves only two thirds of that half, and PDDNOS, which entered the DSM in 1987, is defined by subthreshold symptoms. Therefore, Asperger’s Disorder and PDDNOS are often considered “milder variants.” These milder variants can account for nearly three fourths of current autism diagnoses (Chakrabarti & Fombonne, 2001). Consider also the recent practice of codiagnosing autism alongside known medical and genetic conditions (e.g., Down syndrome, Tourette’s syndrome, and cerebral palsy; Gillberg & Coleman, 2000); the contemporary recognition that autism can exist among people at every level of measured intelligence (Baird et al., 2000), the deliberate efforts to identify autism in younger and younger children (Filipek et al., 2000), and the speculation that many individuals who would meet present-day criteria were previously mis- or undiagnosed (Wing & Potter, 2002), including some of the most accomplished, albeit idiosyncratic, historical figures such as Isaac Newton, Lewis Carroll, W.B. Yeats, Thomas Jefferson, and Bill Gates (Fitzgerald, 2004).
THE CALIFORNIA DATA
In California, persons diagnosed with autism (and other developmental disabilities) qualify for services administered by the statewide Department of Developmental Services (DDS). In 1999, the California DDS reported that from 1987 to 1998 the number of individuals served under the category of “autism” had increased by 273% (California DDS, 1999). Alarmed by this 273% increase, the California legislature commissioned the University of California Medical Investigation of Neurodevelopmental Disorders (M.I.N.D.) Institute to determine whether the increase could be explained by changes in diagnostic criteria. The M.I.N.D. Institute (2002) concluded, on the basis of data we describe next, that there was “no evidence that a loosening in the diagnostic criteria has contributed to the increased number of autism clients served by the [California DDS] Regional Centers” (p. 5). Although this unrefereed conclusion made national headlines and continues to be articulated on innumerable Web sites, it is unwarranted.
The study involved two samples of children who had been served under the California DDS category of “autism”: One sample was born between 1983 and 1985 (the earlier cohort); the other sample was born between 1993 and 1995 (the more recent cohort). Both cohorts were assessed with the same autism diagnostic instrument (an interview conducted with care providers). However, the autism diagnostic instrument was based on DSM-IV criteria—criteria that were not even published until 1994. When the same percentage of children in the earlier and the more recent cohort met the more recent DSM-IV criteria, the researchers imprudently concluded that the “observed increase in autism cases cannot be explained by a loosening in the criteria used to make the diagnosis” (M.I.N.D. Institute, 2002, p. 7).
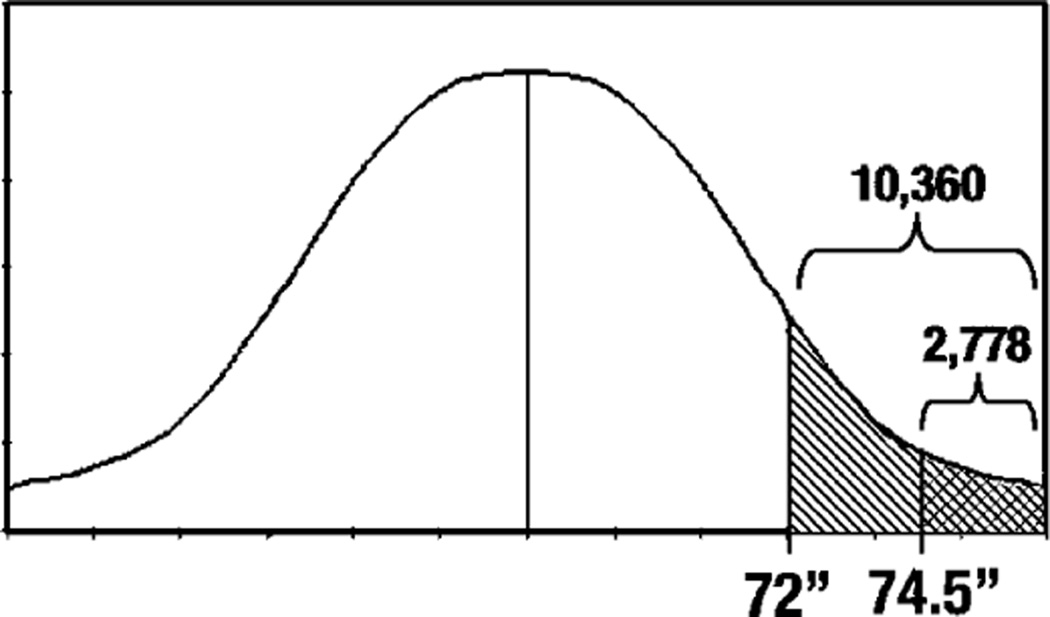
To understand the fallacy of the conclusion, consider the following analogy, based on male height and graphically illustrated in Figure 1. Suppose the criterion for “tall” was 74.5 in. and taller in the mid-1980s, but the criterion was loosened to 72 in. and taller in the mid-1990s. A diagnostic instrument based on the looser, more recent criterion of 72 in. would identify males who met the 74.5-in. criterion as well as those who met the 72-in. criterion.1 Although a perfectly reliable diagnostic instrument based on a looser criterion would identify 100% of the individuals who meet the looser criterion along with 100% of the individuals who meet the more restricted criterion, a highly reliable instrument might identify about 90% of each group; this is the percentage of each cohort in the California study who met the more recent autism criteria.
Fig. 1.
Distribution of male height in McClennan County, Texas. Shaded areas represent segments of the population defined as “tall” according to two standards: men over 74.5 in. (2,778) versus men over 72 in. (10,360).
Most crucially, broadening the criterion will result in a dramatic increase in diagnosed cases. For instance, census data allow us to estimate that 2,778 males in McClennan County, Texas would be called tall by the more restricted 74.5-in. criterion, and 10,360 males would be called tall by the broader 72-in. criterion; if those two criteria had been applied a decade apart, a 273% increase in the number of males called tall would have emerged—without any real increase in Texans’ height. In the same way, the 273% increase from 2,778 versus 10,360 California children who received services for “autism” in 1987 versus 1998 could well be a function of broadened criteria.
As we have already detailed, the commonly applied diagnostic criteria for autism broadened nationally from the 1980s to the 1990s; thus, it would be unusual if the criteria used for eligibility in California had not also broadened during this time. Two further aspects of the California data suggest that the criteria must have broadened. First, children in the more recent cohort were dramatically less likely to have intellectual impairment: Whereas 61% of the children in the earlier cohort were identified as having intellectual impairments, only 27% of the children in the more recent cohort were so identified. The lower rate of intellectual impairment in the more recent cohort matches recent epidemiological data, and the difference between the two rates suggests a major difference between the two cohorts (e.g., that the more recent cohort was drawn from a less cognitively impaired population).
Second, on two of the three dimensions measured by the autism diagnostic instrument, the children in the more recent cohort were, on average, less symptomatic than the children from the earlier cohort. The researchers stated that although these differences were statistically significant (i.e., they exceeded the criterion of a statistical test), they were likely not clinically significant (i.e., they were likely not of significance to the clinical presentation); therefore, the researchers suggested that these differences should not be taken as evidence that the diagnostic criteria had broadened. However, refer again to the tallness analogy: Comparing two cohorts of males in McClennan County diagnosed according to our more restricted (74.5-in.) versus our broader (72-in.) criterion would probably result in a statistically significant difference between the two cohorts’ average height—but the difference would be just about an inch (i.e., most likely not a clinically significant difference).
THE “CHILD COUNT” DATA
The purpose of the federal Individuals With Disabilities Education Act (IDEA), passed in 1991, is to ensure that all children with disabilities are provided a free, appropriate, public education including an individually designed program. Schools comply with the IDEA by reporting to the federal Department of Education an annual “child count” of the number of children with disabilities served. It is the data from these annual child counts that have been the most egregiously misused in arguments for an autism epidemic.
For example, in October 2003, the Autism Society of America sent its 20,000 members the following electronic message: “Figures from the most recent U. S. Department of Education’s 2002 Report to Congress on IDEA reveal that the number of students with autism [ages 6 to 21] in America’s schools jumped an alarming 1,354% in the eight-year period from the school year 1991–92 to 2000–01” (emphasis added). What the Autism Society failed to note is the following fact (available in the Report to Congress, immediately under the autism data entries): Prior to the 1991–1992 school year, there was no child count of students with autism; autism did not even exist as an IDEA reporting category. Moreover, in 1991–1992, use of the autism reporting category was optional (it was required only in subsequent years).
Whenever a new category is introduced, if it is viable, increases in its usage will ensue. Consider another IDEA reporting category introduced along with autism in 1991–1992: “traumatic brain injury.” From 1991–1992 to 2000–2001, this category soared an astronomical 5,059%. Likewise, the reporting category “developmental delay,” which was introduced only in 1997–1998, grew 663% in only 3 years.
After the initial year, the number of children reported under the IDEA category of autism has increased by approximately 23% annually. Why the continuing annual increase? As is the case with new options in the marketplace, like cellular phones and high-speed Internet, new reporting categories in the annual child count are not capitalized upon instantaneously; they require incrementally magnified awareness and augmentation or reallocation of resources. Currently no state reports the number of children with autism that would be expected based on the results of three recent, large-scale epidemiological studies, which identified 5.8 to 6.7 children per 1,000 for the broader autism spectrum (Baird et al., 2000; Bertrand et al., 2001; Chakrabarti & Fombonne, 2001). In 2002–2003, front-runners Oregon and Minnesota reported 4.3 and 3.5 children with autism per 1,000, respectively, while Colorado, Mississippi, and New Mexico reported only 0.8, 0.7, and 0.7 children with autism per 1,000. Thus, most likely IDEA child counts will continue to increase until the number reported by each state approaches the number of children identified in the epidemiological studies.
Why do states vary so widely in the number of children reported (or served)? Each state’s department of education specifies its own diagnostic criteria, and states differ (as do school districts within states, and individual schools within school districts) in the value given to a diagnosis in terms of services received. States also vary from year to year in the number of children served and reported. For instance, Massachusetts historically reported the lowest percentage of children with autism: only 0.4 or 0.5 per 1,000 from 1992 through 2001. Then, in 2002, Massachusetts reported a 400% increase in one year, when it began using student-level data (i.e., actually counting the students) rather than applying a ratio, which was calculated in 1992, based on the proportion of students in each disability classification as reported in 1992. In their 2002 IDEA report to Congress, Massachusetts state officials warned that the increase will continue for several years as “districts better understand how to submit their data at the student level” (IDEA, 2002, p. 4) and “all districts comply completely with the new reporting methods” (IDEA, 2002, p. 4).
OTHER REASONS NOT TO BELIEVE IN AN AUTISM EPIDEMIC
In this article we have detailed three reasons why some laypersons mistakenly believe that there is an autism epidemic. They are unaware of the purposeful broadening of diagnostic criteria, coupled with deliberately greater public awareness; they accept the unwarranted conclusions of the M.I.N.D. Institute study; and they fail to realize that autism was not even an IDEA reporting category until the early 1990s and incremental increases will most likely continue until the schools are identifying and serving the number of children identified in epidemiological studies. Apart from a desire to be aligned with scientific reasoning, there are other reasons not to believe in an autism epidemic.
Epidemics solicit causes; false epidemics solicit false causes. Google autism and epidemic to witness the range of suspected causes of the mythical autism epidemic. Epidemics also connote danger. What message do we send autistic children and adults when we call their increasing number an epidemic? A pandemic? A scourge? Realizing that the increasing prevalence rates are most likely due to noncatastrophic mechanisms, such as purposely broader diagnostic criteria and greater public awareness, should not, however, diminish societal responsibility to support the increasing numbers of individuals being diagnosed with autism. Neither should enthusiasm for scientific inquiry into the variety and extent of human behavioral, neuroanatomical, and genotypic diversity in our population be dampened.
Footnotes
Wing and Potter (2002) provide a similar illustration. The same percentage of children who met Kanner’s earlier, more restricted criteria met DSM-IV’s more recent, broadened criteria; if the child was autistic according to Kanner’s restricted criteria, the child was autistic according to DSM-IV’s broadened criteria. Of course, the reverse was not true. Only 33 to 45% of the children who met more recent DSM-IV criteria met earlier Kanner criteria.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Baird G, Charman T, Baron-Cohen S, Cox A, Swettenham J, Wheelwright S, Drew A. A screening instrument for autism at 18 months of age: A 6 year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:694–702. doi: 10.1097/00004583-200006000-00007. [DOI] [PubMed] [Google Scholar]
- Bertrand J, Mars A, Boyle C, Bove F, Yeargin-Allsopp M, Decoufle P. Prevalence of autism in a United States population: The Brick Township, New Jersey, investigation. Pediatrics. 2001;108:1155–1161. doi: 10.1542/peds.108.5.1155. [DOI] [PubMed] [Google Scholar]
- California Department of Developmental Services. A report to the legislature. Sacramento, CA: California Health and Human Services Agency; 1999. Changes in the population with autism and pervasive developmental disorders in California’s developmental services system: 1987–1998. [Google Scholar]
- Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. Journal of the American Medical Association. 2001;285:3093–3099. doi: 10.1001/jama.285.24.3093. [DOI] [PubMed] [Google Scholar]
- Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook EHJr, Dawson G, Gordon B, Gravel JS, Johnson CP, Kallen RJ, Levy SE, Minshew NJ, Ozonoff S, Prizant BM, Rapin I, Rogers SJ, Stone WL, Teplin SW, Tuchman RF, Volkmar FR. Practice parameter: Screening and diagnosis of autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology. 2000;55:468–479. doi: 10.1212/wnl.55.4.468. [DOI] [PubMed] [Google Scholar]
- Fitzgerald M. Autism and creativity: Is there a link between autism in men and exceptional ability? London: Brunner-Routledge; 2004. [Google Scholar]
- Frith U. Autism: Explaining the enigma. Oxford, England: Blackwell; 1989. [Google Scholar]
- Gillberg C, Coleman M. The biology of the autistic syndromes. 3rd ed. London: MacKeith Press; 2000. [Google Scholar]
- IDEA. Data Notes for IDEA, Part B. 2002 Retrieved April 22, 2005, from IDEAdata Web side: http://www.ideadata.org/docs/bdatanotes2002.doc.
- Kanner L, Eisenberg J. Early infantile autism 1943–1955. American Journal of Orthopsychiatry. 1956;26:55–65. [Google Scholar]
- M.I.N.D. Institute. Report to the Legislature on the principal findings from The Epidemiology of Autism in California: A Comprehensive Pilot Study. Davis: University of California-Davis; 2002. [Google Scholar]
- Rutter M. Diagnosis and definition. In: Rutter M, Schopler E, editors. Autism: A reappraisal of concepts and treatments. New York: Plenum Press; 1978. pp. 1–25. [Google Scholar]
- U.S. Department of Education. Twenty-fourth annual report to Congress on the implementation of the Individuals With Disabilities Education Act. Washington, DC: Author; 2002. [Google Scholar]
- Wing L, Potter D. The epidemiology of autistic spectrum disorders: Is the prevalence rising? Mental Retardation and Developmental Disabilities Research Reviews. 2002;8:151–162. doi: 10.1002/mrdd.10029. [DOI] [PubMed] [Google Scholar]
Recommended Reading
- Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders. 2003;33:365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Immunization safety review: Vaccines and autism. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Wing L, Potter D. 2002 (See References) [Google Scholar]