Abstract
Objectives
To assist researchers and clinicians considering using the Santa Clara Strength of Religious Faith Questionnaire (SCSRFQ) with older-adult samples, the current study analyzed the psychometrics of SCSRFQ scores in two older-adult samples.
Method
Adults age 55 or older who had formerly participated in studies of cognitive-behavioral therapy for anxiety and/or depression were recruited to complete questionnaires. In Study 1 (N = 66), the authors assessed the relations between the SCSRFQ and other measures of religiousness/spirituality, mental health, and demographic variables, using bivariate correlations and nonparametric tests. In Study 2 (N = 223), the authors also conducted confirmatory and exploratory factor analyses of the SCSRFQ, as well as an Item Response Theory analysis.
Results
The SCSRFQ was moderately to highly positively correlated with all measures of religiousness/spirituality. Relations with mental health were weak and differed across samples. Ethnic minorities scored higher than White participants on the SCSRFQ, but only in Study 2. Factor analyses showed that a single-factor model fit the SCSRFQ best. According to Item Response Theory analysis, SCSRFQ items discriminated well between participants with low-to-moderate levels of the construct but provided little information at higher levels.
Conclusion
Although the SCSRFQ scores had adequate psychometric characteristics, the measure’s usefulness may be limited in samples of older adults.
Keywords: religion, spirituality, aging, mental health, measurement
Introduction
Religion and spirituality (R/S1) play significant roles in the mental and physical health of many older adults, who generally endorse higher levels of R/S than younger respondents (e.g., Idler et al., 2003; Newport, 2006, 2012). For instance, multiple dimensions of R/S are positively related to psychological well-being in older adults, even after controlling for demographic variables, stressors, health, and social resources (Fry, 2000). Having high levels of intrinsic religiousness at baseline predicts improvements in depressive symptoms over a four-year period (Sun et al., 2012). High R/S is also related to desirable psychosocial variables, such as positive relationships, generativity, personal growth, and wisdom (Wink & Dillon, 2008). In addition, R/S is linked with reduced mortality (Helm, Hays, Flint, Koenig, & Blazer, 2000; Sullivan, 2010) and improved functioning in activities of daily living (Ai, Peterson, Bolling, & Rodgers, 2006). Given the salience of R/S in late life, some have argued that conceptual models of successful aging and related interventions for older adults should take R/S into account (Crowther, Parker, Achenbaum, Larimore & Koenig, 2002). To assess older adult R/S effectively, researchers and clinicians need adequate information on the psychometric characteristics of R/S measure scores in older-adult samples. Such information may help identify measures appropriate for older adults and avoid inappropriate measures.
The Santa Clara Strength of Religious Faith Questionnaire (SCSRFQ; Plante & Boccaccini, 1997a) is a measure of R/S that is based on a broad conceptualization of religious faith. Although fine distinctions can be made between numerous facets of R/S, measures of these facets tend to be strongly related to a general R/S factor (Gorsuch, 1984). The SCSRFQ was developed to provide a brief (10 items), theoretically simple measure of R/S that touches on a variety of R/S facets, such as public and private R/S behaviors, R/S coping, subjective R/S, and R/S meaning-making and identity. The items were derived from aspects of R/S that Plante observed in his clinical experiences with patients (Plante & Boccaccini, 1997b).
Given its brevity and simplicity, this measure may appeal to researchers and clinicians for use with older adults. However, research using this measure has involved samples composed primarily of young and middle-aged adults. Factor analyses support the unidimensionality of SCSRFQ scores in previous samples (Freiheit, Sonstegard, Schmitt, & Vye, 2006; Lewis, Shevlin, McGuckin, & Navrátil, 2001; Plante, 2010), and internal consistency reliability coefficients range from .94 to .97 (Plante, 2010). The SCSRFQ also correlates positively with a variety of R/S variables, including private and public religious behaviors, intrinsic religiousness, and positive religious coping, supporting the construct validity of SCSRFQ scores in particular samples (Freiheit et al., 2006; Plante, Yancey, Sherman, Guertin, & Pardini, 1999; Sherman et al., 1999; Sherman et al., 2001). The evidence for negative relations with anxiety and depression is mixed (Plante & Boccaccini, 1997a; Plante & Canchola, 2004; Plante, Saucedo, & Rice, 2001; Plante, Yancey, Sherman & Guertin, 2000; Plante et al., 1999; Sherman et al., 1999; Sherman, Simonton, Latif, Spohn, & Tricot, 2005). There is also mixed evidence on the relations between the SCSRFQ and demographic variables. In some cases, ethnic minorities (Sherman et al., 2001) and women (Plante et al., 1999; Plante & Boccaccini, 1997b) have scored higher on the SCSRFQ than White participants and men. No relations with age, education, income, or marital status have been found (Sherman et al., 1999; Sherman et al., 2001).
Despite the substantial psychometric information available for the SCSRFQ, several gaps exist in the literature. First, no study of the SCSRFQ has specifically targeted older adults, for whom R/S is often highly important. Second, although the measure was developed for use in mental health research and practice and has been used in several studies assessing its relations with mental health in medical samples (e.g., Sherman et al., 1999; Sherman et al., 2001; Sherman et al., 2005), only one study has tested its performance using a sample specifically selected for having mental health concerns (recovering substance abusers; Pardini, Plante, Sherman, & Stump, 2001). Third, there is no information as to how well each item (and the measure as a whole) discriminates between individuals across the range of the underlying construct (i.e., strength of faith). Conducting an Item Response Theory (IRT) analysis (Embretson & Reise, 2000) is ideal to answer this question and has proven useful in evaluating other R/S measures (Gomez & Fisher, 2005; Hall, Reise, & Haviland, 2007).
To help those interested in the mental health of older adults make an informed decision about whether to use the SCSRFQ, the current study addresses the gaps noted above by examining the psychometric properties of SCSRFQ scores in two samples of older adults with prior or current diagnoses of anxiety and/or depression. We evaluated the internal consistency reliability of SCSRFQ scores, their convergent validity with respect to scores on other measures of R/S, and correlations with measures of psychological functioning. Based on previous findings described above, it was hypothesized that the SCSRFQ would be positively correlated with all measures of R/S and life satisfaction but negatively correlated with anxiety and depression. Relations with demographic variables were also examined. Although SCSRFQ scores are typically unidimensional in other samples, we conducted factor analysis to verify the factor structure in older adults with anxiety and/or depression. Finally, an IRT analysis was performed to extend these methods by providing a more in-depth view of how the items and overall measure perform in a sample of older adults with current or former anxiety and/or depression.
Study 1
Method
Participants
Participants in Study 1 were adults age 55 or older who had previously participated in studies of cognitive-behavioral therapy (CBT) for anxiety and/or depression and received medical services from the Michael E. DeBakey Veterans Affairs Medical Center or insurance-based medical practice (Calleo et al., 2013; Cully, Paukert, Falco, & Stanley, 2009; Stanley et al., 2009). Of 142 patients originally contacted to participate in the study, one was deceased, one was ineligible because of current participation in a sister study, and 20 did not respond. This left 120 eligible participants, 66 (55%) of whom decided to participate. More information about how this sample was recruited is reported elsewhere (Stanley et al., 2011).
Materials and procedure
Participants had the option of participating in person or by telephone. Thirty-seven (56%) participated by phone, and twenty-nine (44%) participated in person. Subjects who participated by phone were sent an informed-consent document and interviewed following the return of the signed form. Informed consent was obtained immediately before study participation by those who chose to participate in person. Trained research assistants administered the interviews in a single session, lasting approximately one hour. Participants received $20 for completing the interview.
SCSRFQ
The SCSRFQ is used to assess the general role of faith or a higher being in one’s life (items can be found in Plante & Boccaccini, 1997a). Participants indicated how strongly they agreed with each item, using a 4-point Likert-type scale (1=strongly disagree; 4 = strongly agree); we summed responses such that higher scores represent higher strength of religious faith. As noted above, studies of younger and middle-aged adults have found internal consistency reliability coefficients ranging from .94 to .97 (Plante, 2010) and support the unidimensionality of SCSRFQ scores (Freiheit et al., 2006; Lewis et al., 2001; Plante, 2010).
Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS)
The BMMRS uses multiple subscales to assess different facets of R/S (Fetzer Institute/ National Institute on Aging, 1999). The current study included two subscales: Daily Spiritual Experiences (BMMRS-DSE) and Private Religious Practices (BMMRS-PRP). The BMMRS-DSE comprises six items about how often participants feel God’s presence, find strength and comfort in religion, and/or are spiritually touched by the beauty of creation (1 = “Many times a day,” 6 = “Never”). Participants report how often (1 = “More than once a day,” 8 = “Never”) they pray, meditate, read religious literature, and engage in other religious activities, as well as how often they say prayers or grace before meals (1 = “At all meals,” 5 = “Never”) on the five-item BMMRS-PRP. Because of the difference in response options, items for the BMMRS-PRP were standardized; resulting z scores were summed to create an overall score. Where necessary, items were reverse scored so that higher scores represent higher levels of R/S. In the current study, the Cronbach’s α coefficients for BMMRS-DSE and BMMRS-PRP scores were .88 and .85, respectively.
Brief Religious Coping Scale
The Brief Religious Coping Scale (Pargament, Smith, Koenig, & Perez 1998) includes 14 items that assess the frequency of using positive and negative religious coping techniques to deal with a negative life event on a Likert-type scale ranging from 0 (“I didn’t do this”) to 3 (“I did this a lot”). The positive subscale consists of seven items and asks questions related to seeking spiritual support and religious forgiveness. Responses to items composing this subscale were summed such that higher scores indicate more positive coping. The Brief Religious Coping Scale has been used with a variety of populations, including college students and adults living with physical and mental illnesses (Pargament et al., 1998). It is related to other measures of physical and mental health outcomes (Pargament, Feuille, & Burdzy, 2011; Pargament et al., 1998). The Cronbach’s α coefficients for the Positive and Religious Coping subscale score in the current study was .94.
Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being Scale (FACIT-Sp)
The Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being Scale ( Peterman, Fitchett, Brady, Hernandez, & Cella, 2002) is a 12-item instrument designed to measure spirituality in patients with chronic and/or life-threatening illnesses. Participants respond using a five-point scale (1 = “Not at all,” 5 = “Very much”). It contains an overall score, in addition to two subscales: Meaning/Peace and Faith. High scores on the eight-item Meaning/Peace subscale indicate a strong sense of meaning and purpose in life. High scores on the four-item Faith subscale represent great comfort and strength derived from one’s faith or spiritual beliefs. The measure is related to other measures of R/S, including organizational R/S activity, nonorganizational R/S activity, and the Spiritual Beliefs Inventory (Peterman et al., 2002). The Cronbach’s α coefficients in the current study were .92, .86, and .92 for the overall score, the Faith subscale score, and the Meaning/Peace subscale score, respectively.
Geriatric Depression Scale – Short Form (GDS-SF)
The Geriatric Depression Scale (Herrmann et al., 1996) is a 15-item measure designed to assess symptoms of depression in older adults. Participants indicate whether they agree (1) or disagree (0) with each of the items. High scores indicate high levels of depressive symptoms. GDS-SF scores have demonstrated good validity (Herrmann et al., 1996). The Cronbach’s α coefficient in the current study was .83.
Geriatric Anxiety Inventory (GAI)
The Geriatric Anxiety Inventory (Pachana et al., 2007) is a 20-item measure designed to assess symptoms of anxiety in older adults. Participants indicate whether they agree (1) or disagree (0) with each item. High scores indicate high levels of anxiety. The GAI is related to other measures of anxiety, such as the Beck Anxiety Inventory and the Penn State Worry Questionnaire (Pachana et al., 2007). The Cronbach’s α coefficient in the current study was .88.
Satisfaction with Life Scale (SWLS)
The SWLS (Diener, Emmons, Larsen, & Griffin, 1985) is a five-item measure of global life satisfaction. Respondents indicate the extent to which they agree with each statement (1 = “Strongly Disagree,” 7 = “Strongly Agree). SWLS scores typically have good psychometric properties, including high test–retest reliability and predictive validity (Diener et al., 1985; Pavot, Diener, Colvin, & Sandvik, 1991). High scores indicate great satisfaction with life. The Cronbach’s α coefficient in the current study was .86.
Data analysis
Descriptive statistics (frequencies or means and standard deviations) were calculated for each variable. Additionally, Cronbach’s α coefficient was calculated for SCSRFQ scores to assess internal consistency reliability. The distribution of SCSRFQ scores was examined, and the Shapiro-Wilk statistic was used to examine deviation from normality. As described below in the results section, the Shapiro-Wilk test indicated that SCSRFQ scores were not normally distributed. Therefore, the Spearman rank-order correlation coefficient (rsp) was used to examine the relations between the SCSRFQ and each of the following: the BMMRS-DSE, BMMRS-PRP, Positive Religious Coping, FACIT Total, FACIT Meaning/Peace, FACIT Faith, GDS-SF, GAI, SWLS, and age. The Mann Whitney U test was used to test relations between SCSRFQ scores and dichotomized categorical variables of gender (male vs. female), race (White vs. ethnic minority), education level (some college education or less vs. college degree or more), and marital status (married/cohabiting vs. other). All analyses were conducted using IBM SPSS Statistics version 19.
Results
Table 1 presents the demographic characteristics of the sample. Participants were predominantly female, non-Hispanic White, married, educated, and Christian. SCSRFQ scores had a Cronbach’s α of .95 and were not normally distributed, W = .90, p < .001, skewness = −0.885. There were no significant associations between the SCSRFQ and demographic variables. However, there was strong evidence of convergent validity with other measures of R/S, with correlations ranging from rsp = .38 to .84 (see Table 1). The SCSRFQ was most weakly related to the Meaning/Peace subscale of the FACIT and most strongly related to the Positive Religious Coping scale. It was moderately to strongly correlated with most other R/S measures.
Table 1.
Study 1: Descriptive Statistics and Relations Between the SCSRFQ and Measures of Demographic Variables, Religiousness/Spirituality, and Psychological Functioning (N = 66)
| N(%)a | Relation with SCSRFQ (r or z) |
|
|---|---|---|
| SCSRFQ, mean (SD) | 32.9(6.6) | |
| Demographic Variables | ||
| Age, mean (SD) | 69.3(5.9) | −.01 |
| Education | −0.65b | |
| High school or less | 5(7.6) | |
| Some college | 26(39.4) | |
| College degree | 13(19.7) | |
| Graduate school | 22(33.3) | |
| Gender | −1.01c | |
| Male | 22(33.3%) | |
| Female | 44(66.7%) | |
| Raced | −1.41e | |
| American Indian or Alaska Native | 1(1.5%) | |
| Asian | 2(3.0%) | |
| Black or African American | 12(18.2%) | |
| White | 48(72.7%) | |
| Marital Status | −0.72f | |
| Married/living as | 39(59.1%) | |
| Divorced | 17(25.8%) | |
| Widow or widower | 7(10.6%) | |
| Never married | 3(4.5%) | |
| Religious Affiliation | ||
| Protestant | 28(42.4%) | |
| Catholic | 21(31.8%) | |
| Other Christian | 5(7.6%) | |
| Jewish | 2(3.3%) | |
| Other religion | 4(6.7%) | |
| None | 6(9.1%) | |
| Religiousness/Spirituality Variables | ||
| BMMRS-DSE, mean (SD) | 26.2(6.6) | .77*** |
| BMMRS-PRP, mean (SD) | 0.0(3.9) | .66*** |
| Positive Religious Coping, mean (SD) | 14.0(6.8) | .84*** |
| FACIT Total, mean (SD) | 34.3(9.3) | .58*** |
| FACIT Meaning/Peace, mean (SD) | 23.0(6.6) | .38** |
| FACIT Faith, mean (SD) | 11.3(4.0) | .74*** |
| Psychological Functioning Variables | ||
| Geriatric Depression Scale – Short Form, mean (SD) |
3.7(3.3) | −.10 |
| Geriatric Anxiety Inventory, mean (SD) | 7.0(5.1) | −.20 |
| Satisfaction with Life Scale, mean (SD) | 22.1(7.4) | .22 |
p <.01,
p <.001
N(%), unless otherwise noted
Some college or less versus college degree or more
Male versus female
N = 63
White versus ethnic minority
Married or living as married versus divorced, widowed, or never married
SCSRFQ = Santa Clara Strength of Religious Faith Questionnaire; BMMRS-DSE = Brief Multidimensional Measure of Religiousness and Spirituality – Daily Spiritual Experiences; BMMRS-PRP = Brief Multidimensional Measure of Religiousness and Spirituality – Private Religious Practices; FACIT = Functional Assessment of chronic Illness Therapy
Study 2
Method
Participants
Participants in Study 2 were adults age 60 and older who were enrolled in a controlled trial of CBT for older primary care patients with Generalized Anxiety Disorder (GAD) (Ivan et al., 2013). Participants were recruited through internal medicine, family practice, and geriatric clinics at the Michael E. DeBakey Veterans Administration Medical Center and Baylor College of Medicine. Patients who met eligibility criteria were sent a letter or contacted by telephone to invite them to participate (Ivan et al., 2013). Patients expressing interest were screened for anxiety and, if meeting criteria for the study, scheduled for an in-person visit to review the consent form. Of 493 individuals who participated in a diagnostic interview, 223 (45.2%) completed the full assessment and participated in the study. In addition to having a primary or coprimary diagnosis of GAD, 130 (58.3%) participants had a comorbid mental disorder, 90 (40.4%) had an additional anxiety disorder, and 86 (38.6%) also had a depressive disorder.
Materials and procedure
A Master’s-level independent evaluator administered the baseline measures via telephone. All measures used in the current analyses were administered during this assessment prior to participation in the clinical trial. The SCSRFQ, GAI, and SWLS were used (see Measures, Study 1).
Patient Health Questionnaire (PHQ-8)
The Patient Health Questionnaire-8 (Kroenke & Spitzer, 2002) is an eight-item measure of depression based on the PHQ-9 (Kroenke, Spitzer, & Williams, 2001) that omits the item concerning suicidal ideation. Participants rate how often in the preceding two weeks they have experienced each symptom (0 = “Not at all,” 3 = “Nearly every day”). Responses to the eight items were summed, with high scores indicating more depression. PHQ-8 scores generally show good sensitivity and specificity in detecting depressive disorders (Kroenke & Spitzer, 2002) and are highly correlated with PHQ-9 scores (Razykov, Ziegelstein, Whorley & Thombs, 2012), which show good psychometric properties among older adults. In the current study, the Cronbach’s α coefficient for PHQ-8 scores was .83.
Data analysis
Descriptive statistics (either frequencies or means and standard deviations) and Cronbach’s α coefficients were computed. SCSRFQ scores were again significantly negatively skewed, so Spearman rank-order correlations (between the SCSRFQ and age, years of education, PHQ-8, GAI, and SWLS) and Mann Whitney U tests (between the SCSRFQ and dichotomized gender, race, income, and marital status) were calculated. These analyses were conducted using IBM SPSS Statistics version 19.
Since previous analyses have reported that scores on the SCSRFQ demonstrate unidimensionality (Freiheit et al., 2006; Lewis et al., 2001), we initially conducted a confirmatory factor analysis (CFA), with all items treated as ordinal variables loading on a single latent variable. The fit between the data and the model was assessed using the χ2 statistic, the comparative fit index (CFI), the parsimonious goodness of fit index (PGFI), and the root-mean-square error of approximation (RMSEA). CFI and PGFI values greater than 0.90 are acceptable (Kline, 1998), and RMSEA values below .05 suggest close fit, values near .08 are acceptable, and values above .10 represent poor fit (Browne & Cudeck, 1993). As described in the results section, when the CFA showed mixed evidence for a single-factor model, a first-order exploratory factor analysis (EFA) was conducted on the polychoric correlation matrix. The factors were estimated using an unweighted least-squares method, extracted with a principal solution, and rotated with a promax oblique rotation. Examination of the scree plot (eigenvalues) and parallel analysis (Hayton, Allen, & Scarpello, 2004) were used to determine the best number of factors.
The Graded Response Model (Samejima, 1969, 1996) was applied for IRT analyses to estimate discrimination (α) and threshold parameters (βi) for each item of the SCSRFQ. IRT first calculates an overall score called θ to represent the degree to which a respondent possesses the underlying trait (i.e., strength of faith). Then, threshold response curves are plotted to describe the probability that participants at various levels of the underlying construct (i.e., strength of faith [θ]) will select response options above a given threshold for each item. Because there are four response options (from 1 = “Strongly Disagree” to 4 = “Strongly Agree”) for the SCSRFQ, there are three thresholds. β1 refers to the threshold for choosing 2, 3, or 4 versus 1; β2 corresponds to choosing 3 or 4 versus 1 or 2; and β3 reflects choosing 4 versus 1, 2, or 3. Each threshold parameter refers to the value of θ at which a respondent has a 50% likelihood of choosing a response above the threshold and at which the slope of the curve is steepest. In other words, the threshold parameters represent the levels of faith at which the SCSRFQ best distinguishes between respondents. It is, therefore, best for threshold parameters of the individual items to be spread across the range of levels of faith. The discrimination parameter corresponds to the slope of the response curves; the higher the discrimination, the better the item distinguishes between people with different levels of faith. Item-information curves are derived from the discrimination and threshold parameters to represent graphically how well each item distinguishes between respondents at different levels of faith. The total information curve performs the same function, yet for the entire scale. The factor analyses were conducted using MPlus version 5.21 (Muthén & Muthén, Los Angeles, CA), and the IRT analyses were conducted using IRT Pro software (Scientific Software International, Lincolnwood, IL).
Results
Table 2 presents the demographic characteristics of the sample. Participants were predominantly female, non-Hispanic White, and educated. In the Study 2 sample, the internal consistency reliability of SCSRFQ scores again was high (Cronbach’s α = .96). The histogram and Shapiro-Wilk test indicated that the SCSRFQ was not normally distributed, W = .89, p < .001, skewness = −1.013. The SCSRFQ was not significantly related to age, gender, education, income, or marital status. White participants scored significantly lower (mean rank = 107.2) than ethnic-minority participants (mean rank = 130.0), z = −2.16, p < .05. The SCSRFQ was negatively correlated with anxiety and positively correlated with satisfaction with life but unrelated to depression (see Table 2).
Table 2.
Study 2: Descriptive Statistics and Relations Between the SCSRFQ and Measures of Demographic Variables, Religiousness/Spirituality, and Psychological Functioning (N = 223)
| N(%)a | Relation with SCSRFQ (r or z) |
|
|---|---|---|
| SCSRFQ, mean(SD) | 31.7(7.7) | |
| Age, mean(SD) | 66.9(6.6) | .08 |
| Education (in years), mean(SD) | 15.5(2.9) | .01 |
| Income | −.84b | |
| <$10,000/year | 21(9.4) | |
| $10,000–19,999 | 26(11.7) | |
| $20,000–29,999 | 32(14.3) | |
| $30,000–39,999 | 31(13.9) | |
| $40,000–49,999 | 24(10.8) | |
| $50,000–59,999 | 24(10.8) | |
| >$60,000/year | 58(26.0) | |
| Gender | −1.76c | |
| Male | 104(46.6%) | |
| Female | 119(53.4%) | |
| Race | −2.16d* | |
| American Indian or Alaska Native | 1(0.4%) | |
| Asian | 3(1.3%) | |
| Black or African American | 40(17.9%) | |
| Multiracial | 3(1.3%) | |
| White | 176(78.9%) | |
| Marital Status | −.24e | |
| Married/cohabiting | 121(54.3%) | |
| Divorced/separated | 60(26.9%) | |
| Widowed | 33(14.8%) | |
| Never married | 9(4.0%) | |
| Religious Affiliation | ||
| Catholic | 50(22.4%) | |
| Jewish | 11(4.9%) | |
| None | 16(7.2%) | |
| Other | 16(7.2%) | |
| Protestant | 127(57.0%) | |
| Refused to answer | 3(1.3%) | |
| Patient Health Questionnaire-8, mean(SD) | 9.9(5.5) | −.09 |
| Geriatric Anxiety Inventory, mean(SD) | 9.6(5.5) | −.17* |
| Satisfaction with Life Scale, mean(SD) | 19.3(7.1) | .16* |
p <.05
N(%), unless otherwise noted
< $40,000/year versus ≥ $40,000/year
Male versus female
White versus ethnic minority
Married or living as married versus divorced, widowed, or never married
SCSRFQ = Santa Clara Strength of Religious Faith Questionnaire
Table 3 presents descriptive statistics for items of the SCSRFQ in the Study 2 sample. All items except one had means above 3.00 (where 3 = “Slightly Agree”). The table also presents corrected item-total correlations, which ranged from .69 to .90. Examination of the Shapiro-Wilk tests and histograms indicated that scores on all items were not normally distributed, .65 < Ws < .87, ps < .001, −1.705 < skewness < −0.283.
Table 3.
Study 2: SCSRFQ Item-Level Descriptive Statistics, EFA Loadings, and IRT Parameter Estimates (N = 223)
| Item | M(SD) | Item-total r |
Shapiro- Wilk |
EFA Factor Loading |
Slope | β1 | β2 | β3 |
|---|---|---|---|---|---|---|---|---|
| 1 | 3.33(.83) | .82 | .74*** | .903 | 3.87 | −1.84 | −1.26 | 0.02 |
| 2 | 3.16(.95) | .79 | .79*** | .871 | 2.97 | −1.63 | −0.83 | 0.15 |
| 3 | 3.20(.89) | .90 | .79*** | .973 | 7.60 | −1.57 | −0.87 | 0.18 |
| 4 | 3.17(.89) | .90 | .80*** | .968 | 6.29 | −1.66 | −0.79 | 0.20 |
| 5 | 2.70(1.02) | .73 | .87*** | .816 | 2.52 | −1.20 | −0.31 | 0.79 |
| 6 | 3.21(.92) | .86 | .77*** | .925 | 4.67 | −1.45 | −0.98 | 0.14 |
| 7 | 3.49(.81) | .78 | .65*** | .914 | 3.64 | −1.85 | −1.41 | −0.37 |
| 8 | 3.08(.91) | .69 | .82*** | .784 | 2.29 | −1.75 | −1.00 | 0.39 |
| 9 | 3.24(.89) | .87 | .77*** | .944 | 4.88 | −1.59 | −0.99 | 0.10 |
| 10 | 3.10(.93) | .84 | .81*** | .903 | 3.88 | −1.54 | −0.80 | 0.28 |
p <.001
SCSRFQ = Santa Clara Strength of Religious Faith Questionnaire; EFA = exploratory factor analysis; IRT = Item Response Theory
The CFA provided mixed support for the unidimensional model. The model chi-square indicated poor fit between the model and the data, χ2 (15) = 82.15, p < .001. Additionally, the RMSEA of .14 was unacceptable and the PFGI of .69 indicated poor fit taking complexity of the model into account. However, the CFI of .98 was acceptable. Factor loadings were strong (ranging from .78 for item 8 to .97 for item 3), and the amount of variance in each item accounted for by the model ranged from 62.7% to 95.4%; these findings are consistent with a unidimensional model. Due to the mixed results of the CFA, we conducted an EFA to assess the possibility that a greater number of factors would provide a better fit. There was a substantial drop between the eigenvalues of the first (8.24) and second factors (0.53). Parallel analysis indicated the eigenvalues of the second through tenth factors likely occurred by chance, lending additional support to a unidimensional model. All item loadings on the first factor were .78 or higher (see Table 3).
IRT analysis revealed high item-discrimination parameters, or slopes, for all 10 items (above 2.00), meaning that the items are good at distinguishing between respondents with different levels of faith. Items 3, 4, 6, and 9 had particularly high slopes. These items refer to faith as a source of inspiration, meaning and purpose, sense of identity, and comfort.
None of the threshold parameters was more than 2.0 standard deviations above or below the average strength of faith (θ = 0). For all items, respondents who were more than 1.85 standard deviations below the average strength of faith were more likely to strongly disagree with the item than to select the other response options. Most of the β2 were more than 0.5 standard deviations below the mean. Finally, the highest β3 was 0.79 and most of the β3 were below 0.5. In other words, even respondents whose strength of faith was around the average or within half a standard deviation above average were likely to strongly agree with the SCSRFQ items.
Figure 1 presents the item information curves for all 10 items. Items 2 (daily prayer), 5 (active participation in faith or church), and 8 (enjoying the company of others who share one’s faith) generally provide low levels of information across the range of strength of faith. In contrast, items 3 (inspiration) and 4 (meaning and purpose) provide high levels of information and their information peaks around one and two standard deviations below the mean, as well as half a standard deviation above the mean. The total information curve in Figure 2 shows that, overall, SCSRFQ scores provide high information for respondents with low-to-moderate strength of faith. Since measurement precision is inversely related to scale information, the SCSRFQ measures strength of faith poorly for respondents with very low levels of faith (about 2.5 or more standard deviations below the mean) and those with moderately higher levels of faith (approximately 0.5 or more standard deviations above the mean).
Figure 1.
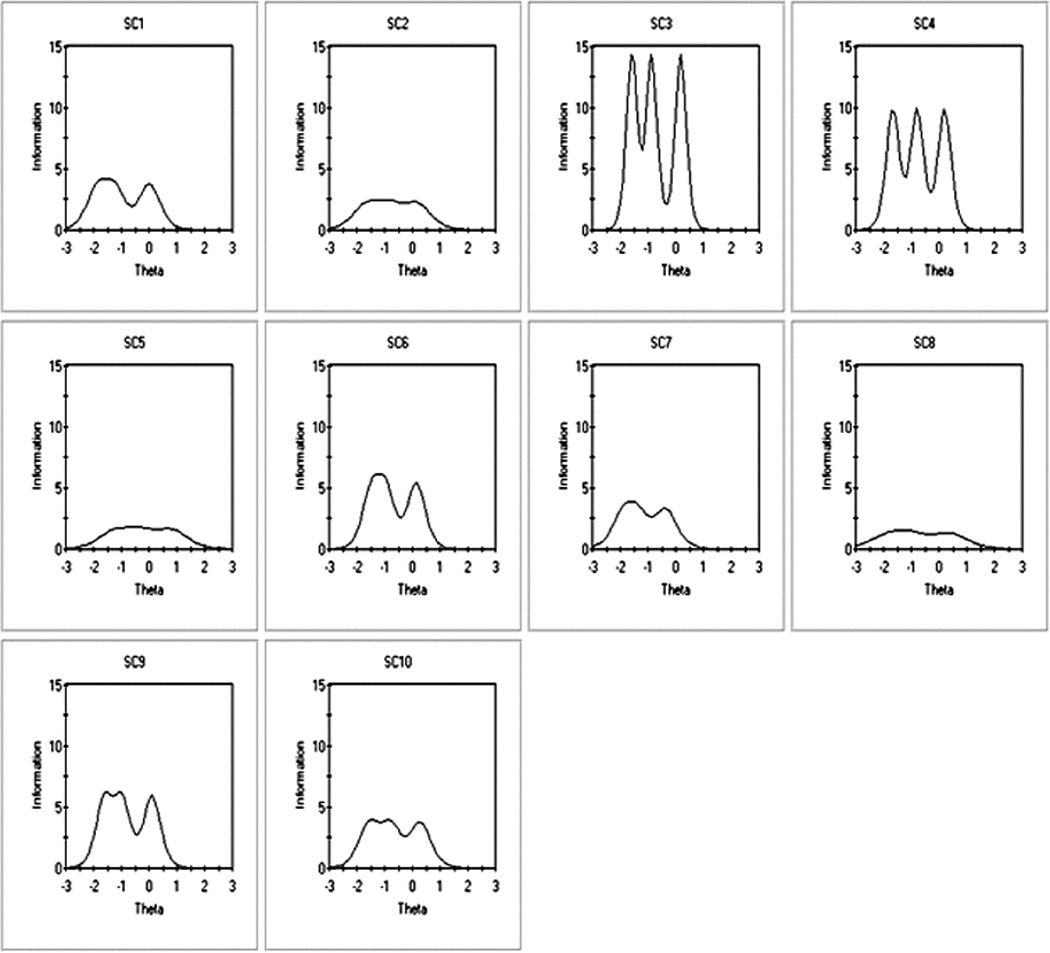
Study 2: Santa Clara Strength of Religious Faith Questionnaire Item Information Curves (N = 223).
Figure 2.
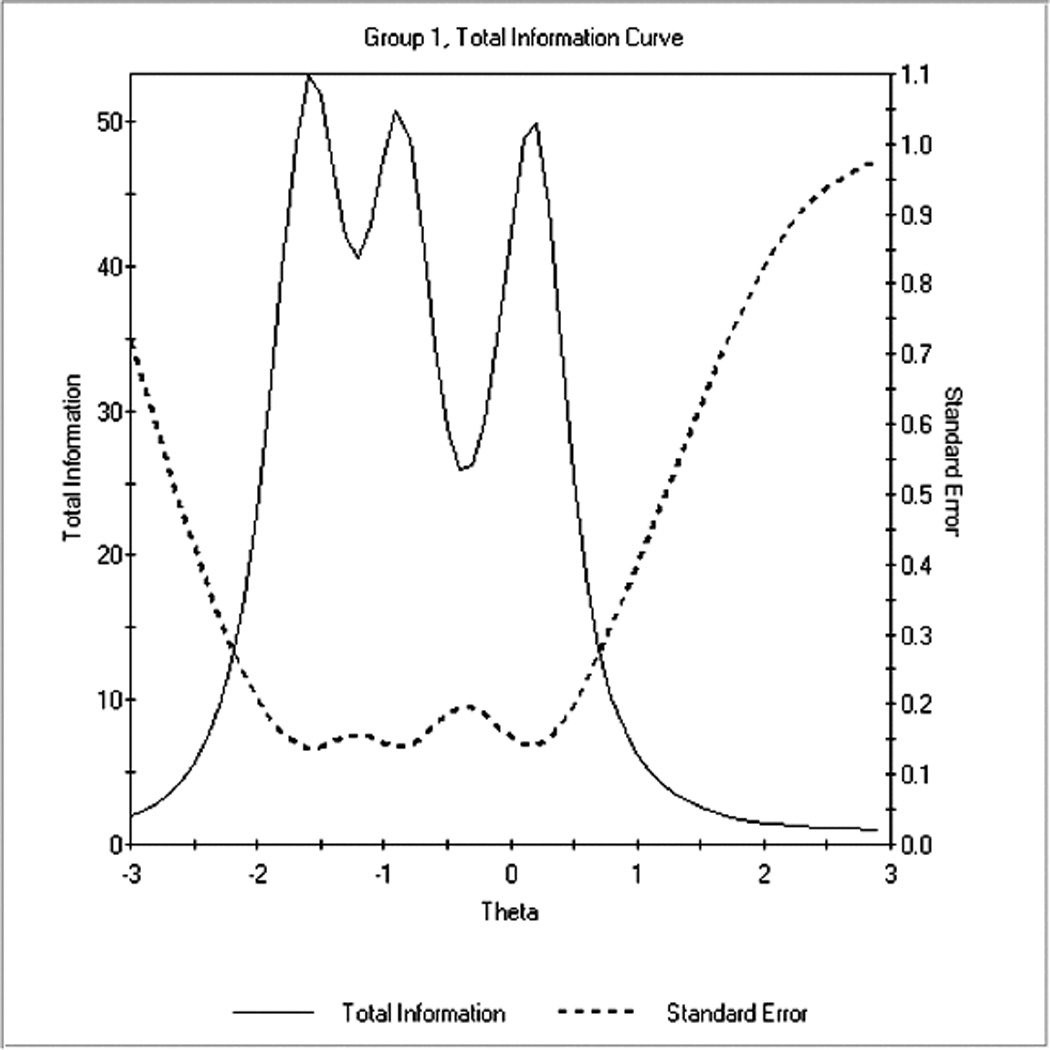
Study 2: Santa Clara Strength of Religious Faith Questionnaire Total Information Curve (N = 223).
General discussion
On the basis of these studies, SCSRFQ scores exhibited adequate reliability and convergent validity among older adults with prior or current anxiety or depression. Both studies found high internal consistency coefficients comparable to those reported in other populations (Plante, 2010). The positive correlations of the SCSRFQ with measures of R/S were consistent with prior research (Freiheit et al., 2006; Plante et al., 1999; Sherman et al., 1999; Sherman et al., 2001). The fact that most correlations are above .60 and three are above .80 raises the question of how distinct the SCSRFQ is from other measures of R/S when used in older-adult samples. Multicollinearity could be problematic if the SCSRFQ were included with other R/S measures in multiple regression models, so researchers should carefully consider which measures are most relevant to their research question.
The SCSRFQ was not significantly related to most demographic variables in either sample. This indicates that the construct measured by the SCSRFQ may be distributed relatively evenly across older adults who differ in terms of age, gender, marital status, and socioeconomic status. Demographic factors may, therefore, be less likely to confound relations between the SCSRFQ and other variables. On the other hand, the statistically significant difference between White and ethnic-minority participants in Study 2 echoes previous findings that ethnic minorities may score higher than Whites on the SCSRFQ (Sherman et al., 2001) and other measures of R/S (Newport, 2006). In this sense, the SCSRFQ behaves similarly to other measures of R/S among older adults.
As in previous studies of the SCSRFQ (Plante et al., 1999; Sherman et al., 1999; Sherman et al., 2005), there were mixed results concerning the relations of the SCSRFQ with measures of mental health. The SCSRFQ was not significantly related to depression in either sample, but it was significantly related to anxiety and life satisfaction in Study 2. The differences in findings across Studies 1 and 2 could be because of a lack of power to detect small effects in Study 1, considering that the direction and magnitude of the correlations were comparable to those in Study 2. Moreover, whereas Study 2 participants were beginning treatment for an anxiety disorder, those in Study 1 had completed treatment for depression or anxiety. R/S may be more strongly related to positive outcomes in individuals experiencing a high level of stress than in those not experiencing that level of stress (Pargament, 1997).
The findings of the CFA and EFA were generally consistent with a unidimensional model, in keeping with the theoretical basis of the SCSRFQ and previous factor analyses (Plante, 2010). A possible explanation for the mixed findings in the CFA is that because most participants in the Study 2 sample scored high on the SCSRFQ, the restricted variance in the items may have attenuated their interrelations and, therefore, reduced the fit of the single-factor CFA model. Further research is needed to confirm these findings.
According to the IRT analysis, the items generally do well in discriminating between respondents. However, items 2, 5, and 8 provide relatively little information and their elimination might not significantly reduce the value of the SCSRFQ. Furthermore, although most items provide adequate information, they do not do so equally across the full range of strength of faith. The individual items, as well as the overall scale, are weak in detecting differences between participants with great strength of faith. This is particularly true for item 7, which has the highest mean and lowest β3 parameter. Item 7’s reference to God could heighten participants’ tendency to endorse the maximum response option out of a desire to please God or give a socially desirable answer. Alternatively, item 7 (importance of one’s relationship with God) and others might be worded in such a way that it is too easy for respondents to endorse. Perhaps using more extreme wording (e.g., “My relationship with God means everything to me,” or “My relationship with God is the most important thing in my life”), would make the items more difficult to endorse and would, therefore, distinguish better among those falling at higher levels of strength of faith. Modifying the Santa Clara measure based on these IRT findings and then cross-validating the modified measure in a different sample is an important future direction.
Items on the SCSRFQ may be written such that even participants with relatively little strength of faith are able to easily endorse the highest response options. This problem has been reported in other IRT analyses of R/S measures (Gomez & Fisher, 2005; Hall et al., 2007). If such were the case, researchers could develop new items or reword the content of current items so that only those with the highest strength of faith would select the highest response option. The number of response options could also be increased and the anchors could be modified to permit more fine-grained distinctions in the upper ranges.
One could also argue that, instead of modifying the SCSRFQ, researchers should reconsider using it with older adults with past or present depression and/or anxiety. As noted above, American older adults tend to have higher R/S than people of other ages (Newport, 2006, 2012). The SCSRFQ may, simply, not perform optimally in samples where high R/S is prevalent. Thus, the measure may be best suited to samples that have low-to-moderate levels of R/S.
Others have suggested that certain R/S variables may function more as latent types rather than continuous variables (Hall et al., 2007). In other words, people might be divided into two groups – those who have high strength of faith and those who do not. If so, researchers would need to analyze strength of faith more as a dichotomous variable.
Given the relations between R/S and mental health, as well as patients’ desire to incorporate R/S in their care, clinicians should assess R/S routinely. Although the SCSRFQ may be of limited utility in research with older adults with high levels of R/S, it may still be useful in clinical work as a screening tool in populations exhibiting a wide range of levels of R/S. The SCSRFQ enables clinicians to assess various aspects of R/S (e.g., public and private R/S behaviors, subjective importance of R/S, positive functions of R/S) using only 10 items. In contrast, the other R/S measures used in Study 1 focus on particular aspects of R/S; to obtain as broad a picture of patient R/S as the SCSRFQ offers, one would have to use several of the other measures, which could become burdensome to patients. Clinicians could administer the SCSRFQ and conduct follow-up assessments of R/S based on the items patients endorse or refer those who endorse items to pastoral care. The SCSRFQ has been studied in medical settings, particularly with cancer patients (Plante, 2010), so clinicians in such settings might be especially interested in using this measure. Future work should test its clinical utility in other settings and with other populations.
The studies reported in this article were subject to a few limitations. The Study 1 sample was predominantly female, White, well educated, Christian, and highly religious; hence, the results may not generalize to demographically different populations. These participants also volunteered to participate in a survey related to R/S and might, therefore, be different from individuals who declined to participate. The Study 2 sample was larger and, therefore, permitted detecting smaller effect sizes; but its demographic composition was similar to that of Study 1, raising similar questions about external validity. Moreover, because all Study 2 participants met criteria for a current mental disorder, the results may not generalize to those without a mental disorder. Another limitation is that all measures in both studies were self-report, limiting conclusions to participant perceptions of their R/S and psychological functioning. Finally, given the skewness of SCSRFQ scores, the results must be interpreted with caution. Where possible, nonparametric tests were used to mitigate the effects on nonnormal distributions.
On the whole, SCSRFQ scores exhibited adequate psychometric characteristics in the two older-adult samples in this study. However, this measure may not detect differences between older adults who are highly religious or spiritual. Researchers and clinicians should keep this in mind to ensure that the R/S measure they choose demonstrates optimal precision in their target sample. In the future, conducting IRT analyses in a sample with a wide range in age and R/S may clarify whether the lack of precision at high SCSRFQ scores is specific to older adults. It may also be worthwhile to modify the SCSRFQ to increase its precision in the upper range.
Acknowledgments
Funding
This research was supported by funding from the National Institute of Mental Health (R01-MH53932) and the Veterans Affairs South Central Mental Illness Research, Education, and Clinical Center (MIRECC) and in part with resources and the use of facilities at the Houston VA Health Services Research and Development Center of Innovations in Quality, Effectiveness and Safety (CIN 13–413) at the Michael E. DeBakey VA Medical Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, the National Institutes of Health, the Department of Veterans Affairs, the US Government or Baylor College of Medicine. The NIMH had no role in the design and conduct of the study; the collection, management, analysis and interpretation of the data; or the preparation, review or approval of the manuscript.
Appendix
Santa Clara Strength of Religious Faith Questionnaire Items
My religious faith is extremely important to me.
I pray daily.
I look to my faith as a source of inspiration.
I look to my faith as providing meaning and purpose in my life.
I consider myself active in my faith or church.
My faith is an important part of who I am as a person.
My relationship with God is very important to me.
I enjoy being around others who share my faith.
I look to my faith as a source of comfort.
My faith impacts many of my decisions.
Footnotes
We adhere to the definitions of religion and spirituality outlined by the editors of the APA Handbook of Psychology, Religion and Spirituality (Pargament, Mahoney, Exline, Jones, & Shafranske, 2013). They define spirituality as a “search for the sacred” (Pargament et al., 2013, p. 14) in which people seek to connect with or understand that which is ultimate, transcendent, or boundless. Religion is “the search for significance that occurs within the context of established institutions that are designed to facilitate spirituality” (Pargament et al., 2013, p. 15). Because these definitions suggest spirituality is the core function of religion, and because the SCSRFQ and other measures used in this paper assess both religious and spiritual factors, we elected to refer to the constructs jointly as “R/S.”
References
- Ai AL, Peterson C, Bolling SF, Rodgers W. Depression, faith-based coping, and short-term postoperative global functioning in adult and older patients undergoing cardiac surgery. Journal of Psychosomatic Research. 2006;60(1):21–28. doi: 10.1016/j.jpsychores.2005.06.082. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sage Focus Editions. 1993;154:136–136. [Google Scholar]
- Calleo J, Bush AL, Cully JA, Wilson N, Rhoades H, Novy D, Masozera N, Williams S, Kunik M, Stanley M. Treating late-life GAD in primary care: An effectiveness pilot study. Journal of Nervous and Mental Disease. 2013;20(5):414–420. doi: 10.1097/NMD.0b013e31828e0fd6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowther MR, Parker MW, Achenbaum WA, Larimore WL, Koenig HG. Rowe and Kahn's model of successful aging revisited: Positive spirituality—The forgotten factor. The Gerontologist. 2002;42:613–620. doi: 10.1093/geront/42.5.613. [DOI] [PubMed] [Google Scholar]
- Cully JA, Paukert A, Falco J, Stanley MA. Cognitive-behavioral therapy: Innovations for cardiopulmonary patients with depression and anxiety. Cognitive and Behavioral Practice. 2009;16:394–407. [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item response theory for psychologists. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Fetzer Institute and the National Institute on Aging Working Group. Multidimensional measurement of religiousness/spirituality for use in health research. Kalamazoo, MI: John E. Fetzer Institute; 1999. [Google Scholar]
- Freiheit SR, Sonstegard K, Schmidt A, Vye C. Religiosity and spirituality: A psychometric evaluation of the Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychology. 2006;55:27–33. [Google Scholar]
- Fry PS. Religious involvement, spirituality and personal meaning in life: existential predictors of psychological wellbeing in community-residing and institutional care elders. Aging & Mental Health. 2000;4:375–387. [Google Scholar]
- Gomez R, Fisher JW. Item response theory analysis of the Spiritual Well-being Questionnaire. Personality and Individual Differences. 2005;38:1107–1121. [Google Scholar]
- Gorsuch RL. Measurement: The boon and bane of investigating religion. American Psychologist. 1984;39(3):228. [Google Scholar]
- Hall TW, Reise SP, Haviland MG. An item response theory analysis of the Spiritual Assessment Inventory. The International Journal for the Psychology of Religion. 2007;17:157–178. [Google Scholar]
- Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational Research Methods. 2004;7:191–205. [Google Scholar]
- Helm HM, Hays JC, Flint EP, Koenig HG, Blazer DG. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55:M400–M405. doi: 10.1093/gerona/55.7.m400. [DOI] [PubMed] [Google Scholar]
- Herrmann N, Mittmann N, Silver IL, Shulman KI, Busto UA, Shear NH, Naranjo CA. A validation study of the Geriatric Depression Scale Short Form. International Journal of Geriatric Psychiatry. 1996;11:457–460. [Google Scholar]
- Idler EL, Musick MA, Ellison CG, George LK, Krause N, Ory MG, Williams DR. Measuring multiple dimensions of religion and spirituality for health research. Research on Aging. 2003;25:327–365. [Google Scholar]
- IRTPRO for Windows [Computer software] Lincolnwood, IL: Scientific Software International; [Google Scholar]
- Ivan MC, Amspoker AB, Nadorff MR, Kunik ME, Cully JA, Wilson N, Calleo J, Kraus-Schuman C, Stanley MA. Alcohol use, anxiety, and insomnia in older adults with generalized anxiety disorder. American Journal of Geriatric Psychiatry. 2013 doi: 10.1016/j.jagp.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford; 1998. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CA, Shevlin M, McGuckin C, Navrátil M. The Santa Clara Strength of Religious Faith Questionnaire: Confirmatory factor analysis. Pastoral Psychology. 2001;49:379–384. [Google Scholar]
- Mplus (Version 5.21) [Computer Software] Los Angeles, CA: Muthén & Muthén; [Google Scholar]
- Newport F. Religion most important to blacks, women, and older Americans. 2006 Retrieved from http://www.gallup.com/poll/25585/Religion-Most-Important-Blacks-Women-Older-Americans.aspx.
- Newport F. Seven in 10 Americans are very or moderately religious. 2012 Retrieved from http://www.gallup.com/poll/159050/seven-americans-moderately-religious.aspx#1.
- Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and validation of the Geriatric Anxiety Inventory. International Psychogeriatrics. 2007;19:103–114. doi: 10.1017/S1041610206003504. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Plante TG, Sherman A, Stump JE. Religious faith and spirituality in substance abuse recovery: Determining the mental health benefits. Journal of Substance Abuse Treatment. 2000;19:347–54. doi: 10.1016/s0740-5472(00)00125-2. [DOI] [PubMed] [Google Scholar]
- Pargament KI. The psychology of religion and coping: Theory, research, practice. New York, NY: The Guilford Press; 1997. [Google Scholar]
- Pargament K, Feuille M, Burdzy D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions. 2011;2(1):51–76. [Google Scholar]
- Pargament KI, Smith BW, Koenig HG, Perez L. Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion. 1998;37:710–724. [Google Scholar]
- Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the Satisfaction With Life Scale: Evidence for the cross-method convergence of well-being measures. Journal of Personality Assessment. 1991;57:149–161. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- Peterman AH, Fitchett GD, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy - Spiritual Well-being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- Plante TG. The Santa Clara Strength of Religious Faith Questionnaire: Assessing faith engagement in a brief and nondenominational manner. Religions. 2010;1(1):3–8. [Google Scholar]
- Plante TG, Boccaccini M. The Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychology. 1997a;45:375–387. [Google Scholar]
- Plante TG, Boccaccini M. Reliability and validity of the Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychology. 1997b;45:429–437. [Google Scholar]
- Plante TG, Canchola EL. The association between strength of religious faith and coping with American terrorism regarding the events of September 11, 2001. Pastoral Psychology. 2004;52:269–278. [Google Scholar]
- Plante TG, Saucedo B, Rice C. The association between religious faith and coping with daily stress. Pastoral Psychology. 2001;49:291–300. [Google Scholar]
- Plante TG, Yancey S, Sherman A, Guertin M. The association between strength of religious faith and psychological functioning. Pastoral Psychology. 2000;48:405–412. [Google Scholar]
- Plante TG, Yancey S, Sherman A, Guertin M, Pardini D. Further validation for the Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychology. 1999;48:11–21. [Google Scholar]
- Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8 - Is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. Journal of Psychosomatic Research. 2012;73:163–168. doi: 10.1016/j.jpsychores.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Samejima F. Estimation of latent ability using a response pattern of graded scores. Psychometrika Monograph Supplement. 1969 [Google Scholar]
- Samejima F. The graded response model. In: van WJ, Linden der Hambleton RK, editors. Handbook of modern item response theory. New York, NY: Springer; 1996. pp. 85–100. [Google Scholar]
- Sherman AC, Plante TG, Simonton S, Adams DC, Burris SK, Harbison C. Assessing religious faith in medical patients: cross-validation of the Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychology. 1999;48:129–141. [Google Scholar]
- Sherman AC, Simonton S, Adams DC, Latif U, Plante TG, Burns SK, Poling T. Measuring religious faith in cancer patients: Reliability and construct validity of the Santa Clara Strength of Religious Faith Questionnaire. Psychooncology. 2001;10:436–443. doi: 10.1002/pon.523. [DOI] [PubMed] [Google Scholar]
- Sherman AC, Simonton S, Latif U, Spohn R, Tricot G. Religious struggle and religious comfort in response to illness: Health outcomes among stem cell transplant patients. Journal of Behavioral Medicine. 2005;28:359–367. doi: 10.1007/s10865-005-9006-7. [DOI] [PubMed] [Google Scholar]
- Stanley M, Bush A, Camp M, Jameson J, Phillips L, Barber C, Cully J. Older adults' preferences for religion/spirituality in treatment for anxiety and depression. Aging & Mental Health. 2011;15(3):334–343. doi: 10.1080/13607863.2010.519326. [DOI] [PubMed] [Google Scholar]
- Stanley MA, Wilson N, Novy DM, Rhoades H, Wagener P, Greisinger AJ, Kunik ME. Cognitive behavior therapy for older adults with generalized anxiety disorder in primary care. A randomized clinical trial. Journal of the American Medical Association. 2009;301:1460–1467. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan AR. Mortality differentials and religion in the United States: Religious affiliation and attendance. Journal for the Scientific Study of Religion. 2010;49:740–753. doi: 10.1111/j.1468-5906.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun F, Park NS, Roff LL, Klemmack DL, Parker M, Koenig HG, … Allman RM. Predicting the trajectories of depressive symptoms among southern community-dwelling older adults: The role of religiosity. Aging & Mental Health. 2012;16:189–198. doi: 10.1080/13607863.2011.602959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wink P, Dillon M. Religiousness, spirituality, and psychosocial functioning in late adulthood: Findings from a longitudinal study. Psychology of Religion and Spirituality. 2008;(1):102–115. doi: 10.1037/0882-7974.18.4.916. S. [DOI] [PubMed] [Google Scholar]


