Abstract
Background
A number of instruments have been developed to measure health-related quality-of-life (HRQoL), differing in the health domains covered and their scoring. While few such measures have been consistently included in U.S. national health surveys over time, the surveys have included data on a broad range of symptoms and impairments, which enables the tracking of population health trends.
Objectives
To compare trends in HRQoL as measured using existing instruments vs. using a broader range of symptoms and impairments collected in multiple years of nationally representative data.
Data and Measures
Data were from the 2000 to 2010 Medical Expenditure Panel Survey (MEPS), which is nationally representative of the non-institutionalized U.S. population. Level of and trends in HRQoL derived from a broad range of survey symptoms and impairments (SSI) was compared to HRQoL from the SF-6D, the HALex, and, between 2000 and 2003, the EuroQol-5D (EQ-5D) and EQ-5D Visual Analog Scale.
Results
Trends in HRQoL were similar using different measures. The SSI scores correlated 0.66 to 0.80 with scores from other measures and mean SSI scores were between those of other measures. Scores from all HRQoL measures declined similarly with increasing age and with the presence of comorbid conditions.
Conclusion
Measuring HRQoL using a broader range of symptoms and impairments than those in a single instrument yields population health trends similar to those from other measures while making maximum use of existing data and providing rich detail on the factors underlying change.
Keywords: Health measurement; Health trends, Health status; Health-related quality of life; Health monitoring; Population health; Quality of life
A number of nationally representative health surveys are conducted in the U.S. with the goal of monitoring population health over time. Particularly valuable for tracking overall health are measures that consider a range of symptoms and impairments and weight their severity and relative importance, combining them to yield a single overall score on a 0 to 1 scale. This score can then be combined with life expectancy to form a measure of quality-adjusted life expectancy (QALE). Some of the best known of these measures include the EuroQol-5D (EQ-5D),1 the Short-Form 6-D (SF-6D),2 and the Health Utilities Index (HUI).3 Such measures have seldom been included in multiple years of national health surveys,4 in part due to the additional survey space required to ask the questions specific to a single instrument, and in part because no gold standard measure has been identified; each has strengths and weaknesses and different measures are best suited for different purposes.
However, the breadth of symptoms and impairments asked about in current national surveys is actually greater than that covered by any one of these specific instruments. For example, surveys often include questions about specific sensory, cognitive, and physical abilities (such as walking and bending) that are not included in specific instruments. By calculating disutilties associated with this broader set of symptoms and impairments,5 we have made use of the wide range of existing data to develop HRQoL scores and track health over a longer time period and in a more comprehensive population than possible using an existing measure.6 While this approach has the strength of enabling detailed tracking and disaggregation of HRQoL change, it is important to examine how the HRQoL scores formed in this manner compare to those from existing measures, at a point in time and over time. This paper compares the level of and trends in HRQoL scores derived from the broad range of questions in national health data from 2000–2010 to HRQoL scores from several other measures that can be calculated in the same national data set: the SF-6D, the Health and Activity Limitations Index (HALex),7 and, for a shorter time period, EQ-5D and EQ-5D Visual Analog Scale (VAS).
Methods
The Medical Expenditure Panel Survey (MEPS) is a household-based medical expenditure survey sponsored by the Agency for Healthcare Research and Quality (AHRQ) that is nationally representative of the non-institutionalized civilian U.S. population in each survey year.8 In the year 2000 two existing health measurement instruments were added to MEPS: the SF-12, which continues to be included in the survey, and the EQ-5D, which was included through 2003. The SF-6D can be calculated using a subset of 7 questions from the SF-12 questionnaire that cover physical and emotional role function, mobility, vitality, depression, and pain.2 The EQ-5D asks broad questions in 5 domains of health: mobility, self-care, usual activities, pain/discomfort and anxiety/depression, with respondents indicating either no difficulty, moderate difficulty, or extreme difficulty in each domain. An additional measure from the EQ-5D is an overall rating of general health on a scale from 0 (equivalent to the worst imaginable health state) to 100 (the best health imaginable), which is administered as a visual thermometer. We divide these scores by 100 to transform them to a 1-0 scale, and refer to this as the visual analogue scale (or VAS) in our comparisons.
Another HRQoL measure that can be estimated using data collected in MEPS is the HALex,7 which was developed as part of the Healthy People 2000 initiative and is scored based on the presence of impairments in self-care (Activities of Daily Living, or ADLs) and a self-rating of overall health on a 5-point scale, from excellent to poor. The original HALex was developed for the National Health Interview Survey, which includes a question about being “limited in any way in any activities because of any impairment or health problem.” We used an alternate HALex scoring that was developed for the MEPS survey, which does not contain this question.9
The SF-6D, EQ-5D, and HALex measures use different scoring/weighting algorithms to yield scores on a 0 to 1 scale. The SF-6D and EQ-5D use community-elicited preference weights for each health state. That is, individuals were asked to rate the potential impact of different combinations of health problems on HRQoL, yielding disutility weights for all of the instrument’s possible combinations of problems. While the original weights for EQ-5D scoring were measured in the U.K., we used preference weights measured in the U.S. population.10 HAlex weights for each combination of self-rated health and ADL function were imputed using mathematical techniques and reference to preference weights developed for the HUI instrument.7
As a result of the inclusion of the EQ-5D and SF-12 as well as many other specific questions on health and functioning, MEPS is the national survey that has included the broadest array of symptoms and impairments over time. Table 1 groups symptoms and impairments into seven broad domains: problems with primary activity (working, keeping house, school) or social activity; physical activity limitations (self-care; performance of tasks for routine needs, and specific movement difficulties); pain; mental health symptoms; low energy; sensory problems (vision and hearing impairment); and cognitive impairment.
Table 1.
Symptom/Impairment Question Coverage Across Instruments
| MEPS 2000–2010 | SF-6D | EQ-5D | HALex |
|---|---|---|---|
| Primary Activity: | Primary Activity: | Primary Activity: | |
| Major, Social | Major, Social | Major/ Social Combined | |
| Physical Activity: | Physical Activity: | Physical Activity: | Physical Activity: |
| Self-care, Routine needs | Moderate Activities | Self-care/Routine needs Combined Walking | Self-care, Routine needs |
| Bending, Lifting, Walking | Walking | ||
| Standing, Reaching, Dexterity | |||
| Mental: Depressive, Anxious | Mental: Depressive | Mental: Depressive/Anxious Combined | |
| Sensory: Vision, Hearing | |||
| Pain | Pain | Pain | |
| Cognitive | |||
| Energy | Energy | ||
| Self-Rated Health |
To estimate the impact of this broad range of symptoms and impairments on QOL, we used a previously published method to develop disutility weights for each problem by relating them to the EQ-5D VAS in MEPS 2002.6 We regressed the VAS rating on the set of symptoms and impairments and their interactions, and then calculated disutility weights for each symptom and impairment that were independent of the others and reflected the effects of interactions. To do this we calculated mean predicted scores, first assuming that everyone reported the item (worst case) and then assuming no one reported the item (best case). The difference between these mean predicted scores yielded a weight that captured the broadest possible impact of having the symptom or impairment in light of the other symptoms and impairments that people have. These weights were then used to calculate HRQoL scores based on an individual’s reported symptoms and impairments.6 A decrement equal to the intercept of the regression was added to each score to represent the average utility loss not accounted for by this set of symptoms and impairments. We refer to this as the Survey-based Symptom/Impairment (SSI) method of deriving HRQoL scores.
The wording of the relevant questions in MEPS remained the same between 2000 and 2010 with the exception of those that were part of the SF-12, which changed slightly in 2003 due to the adoption the SF-12v2 questionnaire. Specifically, in version 2, questions about the frequency of depressive feelings, anxious feelings, and energy omitted the response category ‘good bit of the time’, thus dropping from 6 response categories to 5. In addition, role performance questions were expanded from having only 2 response categories (yes/no) in v1 to having 5 categories in v2 (all, most, some, a little, or none of the time). To adjust for the change in depressive and energy questions, the SF-6D v1 scoring was revised to randomly assign half of those who responded ‘a good bit of the time’ to the adjacent categories on either side (“most of the time” and “some of the time.”) To adjust for the change in role performance questions, the SF-6D v2 scoring assigned all categories to “Yes” except “None of the time.”11
For the SSI, we used role performance questions in the MEPS survey that were not part of the SF-12. For depressive, anxious and tired symptoms, we examined different methods for handling of the question changes as described in the online Appendix (Supplemental Digital Content 1, http://links.lww.com/MLR/A757). Not adjusting for the changes had virtually the same effect as holding constant the change in these symptoms from 2002 to 2003, since the effects of the question changes acted in different directions for different symptoms.
Scores on each measure were derived for respondents with complete data on all other measures examined over each time period. Sample sizes for each year are shown in the Appendix (Supplemental Digital Content 1, http://links.lww.com/MLR/A757). We restrict our comparison of trends to the same sample over time, comparing SF-6D, SSI, and HALEx only among those nonmissing on all measures. We did not condition these trends on non-missing response to VAS and EQ5d, since they were only available for the first 4 years. To examine convergent validity, we tested correlations between measures, plotted them against one another, tested time trends in each measure and compared their rank order over time. To plot SSI scores against those from other measures, we divided each other measure into categories based on the distribution of scores. The categories for these plots were as close to quartiles as possible while keeping those with the same score grouped together. Time trends were tested by regressing a continuous MEPS year variable on each measure in pooled data, controlling for 10-year age group, sex, race (black, with white and other in referent group), and sex interacted with race.
To assess construct validity, we also examined scores on each HRQoL measure by age and by the presence of none, one, or two or more of the following self-reported conditions: diabetes, emphysema, stroke or transient ischemic attack (TIA), coronary heart disease (CHD), myocardial infarction (MI), or any other kind of heart condition/disease (other than CHD/MI/angina).
Analyses were performed using SAS (version 9 for Unix; The SAS Institute, Cary, NC) and Stata (version 12.1 for Unix; StataCorp, College Station, TX) using statistical methods designed for survey data to account for sampling factors including stratification, clustering, oversampling of minorities, and nonresponse to the overall survey and the mail-in health questionnaire.
Results
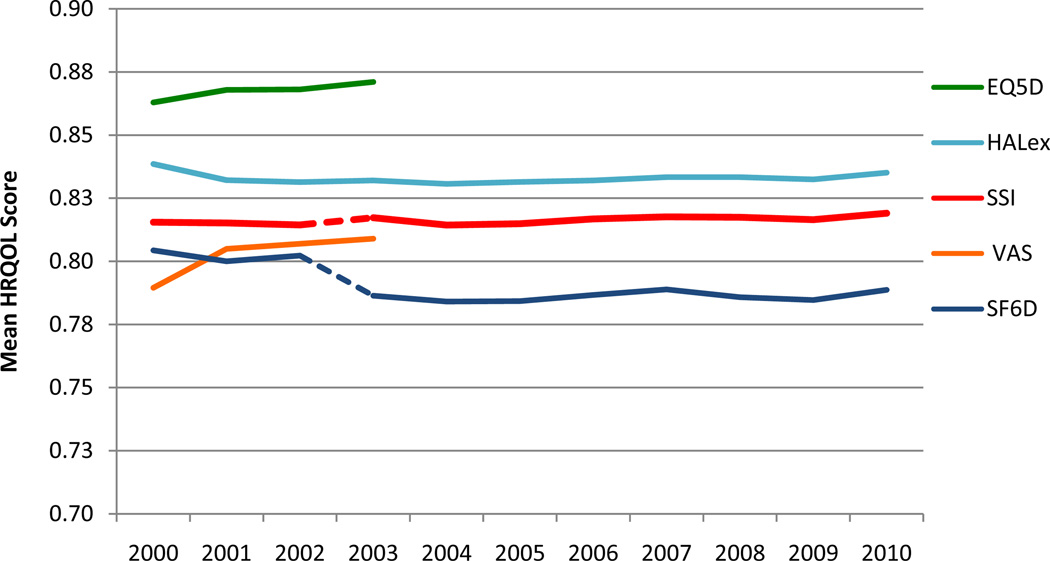
Figure 1 shows trends in HRQoL using each of the measures, adjusted by 10-year age group to the 2010 population. We show the data points without confidence intervals because the standard errors were sufficiently small to be unnoticeable (ranging from 0.001 to 0.002). Scores increased significantly from 2000–2010 using the SSI (p= 0.016), SF-6D (p <.0001), and from 2000–2003 using the EQ-5D (0.0004) and VAS (< 0.0001), while HALex was unchanged (p=0.7480). The notable drop in SF-6D scores in 2003 was due to the recoding of responses to role model questions in SF-6D scoring to try to match the binary question used in prior years, which resulted in a higher prevalence of role performance problems in 2003 and beyond. Separately testing trends from before and after the SF-12 questionnaire change, from 2000 to 2003 there was no significant change in mean SSI (p=0.661) or SF-6D (p= 0.368) scores, HALex scores declined (p=.030), and there was an increase in mean EQ-5D (p=0.0004) and VAS (p <.0001) scores. From 2003–2010, SSI increased significantly (p=0.023), but not the SF-6D (p= 0.312) or HALex (p=0.313).
Figure 1.
Comparison of Trends in Health-Related Quality of Life Using Different Measures, Overall Population, Aged 18 and Over, MEPS Survey Years 2000–2010, Age-Adjusted to the 2010 Population by 10-Year Age Group
Notes: EQ-5D and VAS trends are truncated at 2003 because they were discontinued from the MEPS in 2004. Trends are shown for those with complete data on HALex, SSI, and SF-6D. Those missing on EQ-5D and VAS from 2000–2003 are not omitted, however trends are almost identical when these additional respondents are omitted (not shown).
The notable drop in SF-6D scores in 2003 was at least partially due to the adoption of the new SF-12 questionnaire in that year and the reassignment of responses to role model questions to try to match to the dichotomous response categories in the earlier SF-12 version. All those responding in version 2 that they had any problems (a little of the time, some of the time, most of the time, or all of the time) were assigned as having problems (to match ‘yes’ in version 1), resulting in a higher prevalence of role performance problems in 2003 and beyond. Survey Based Symptom/Impairment scores did not use the role performance questions. They did use other SF-12 questions that changed in 2003 (depressive and anxious symptoms and energy). Adjustments are discussed in the Appendix (Supplemental Digital Content 1, http://links.lww.com/MLR/A757).
Differences between the measures at a point in time were larger than the differences in trends over time. Compared to SSI scores, the mean EQ-5D and HALex scores were significantly higher and the mean SF-6D and VAS scores were significantly lower (p for all comparisons <0.0001). Two factors contributing to the slightly lower scores with the SF-6D than with the other measures were the additional disutility assigned to those with higher levels of any given problem, and the disutility assigned to milder levels of depressive symptoms (feeling down a little of the time), and low energy (had a lot of energy most of the time but not all of the time). Despite these differences, mean scores on all measures remained within 0.07 of one another. Table 2 shows correlations between pairs of measures in pooled data from 2000–2002, the years that included the EQ-5D/VAS and were prior to the switch in SF-12 versions. All correlations were significant (p < 0.0001) and they ranged from 0.54 to 0.80; correlations between the SSI and other measures were the highest.
Table 2.
Correlations Between Measuresin Pooled 2000–2002 MEPS Data
| Survey Based Symptom/Impairment (SSI) |
Short-Form 6-D (SF-6D) |
Health and Activity Limitations Index (HALex) |
EuroQoL 5D (EQ-5D) |
|
|---|---|---|---|---|
| SF-6D | 0.80 | |||
| HALex | 0.66 | 0.54 | ||
| EQ-5D | 0.75 | 0.71 | 0.59 | |
| VAS | 0.69 | 0.64 | 0.63 | 0.64 |
Correlations between all pairs of measures were significant (p < 0.0001).
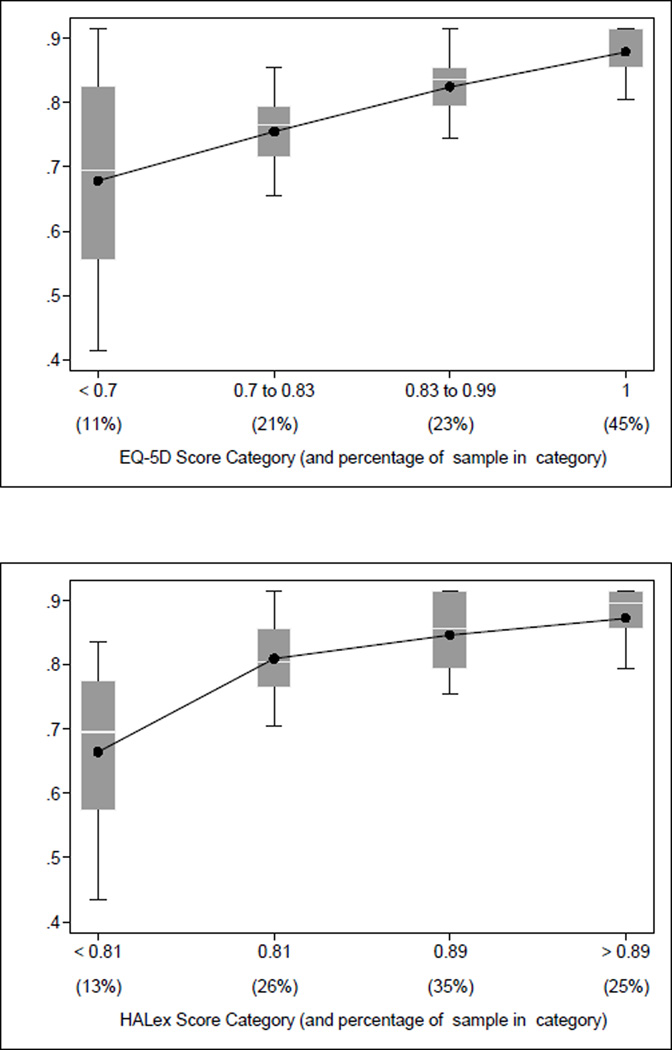
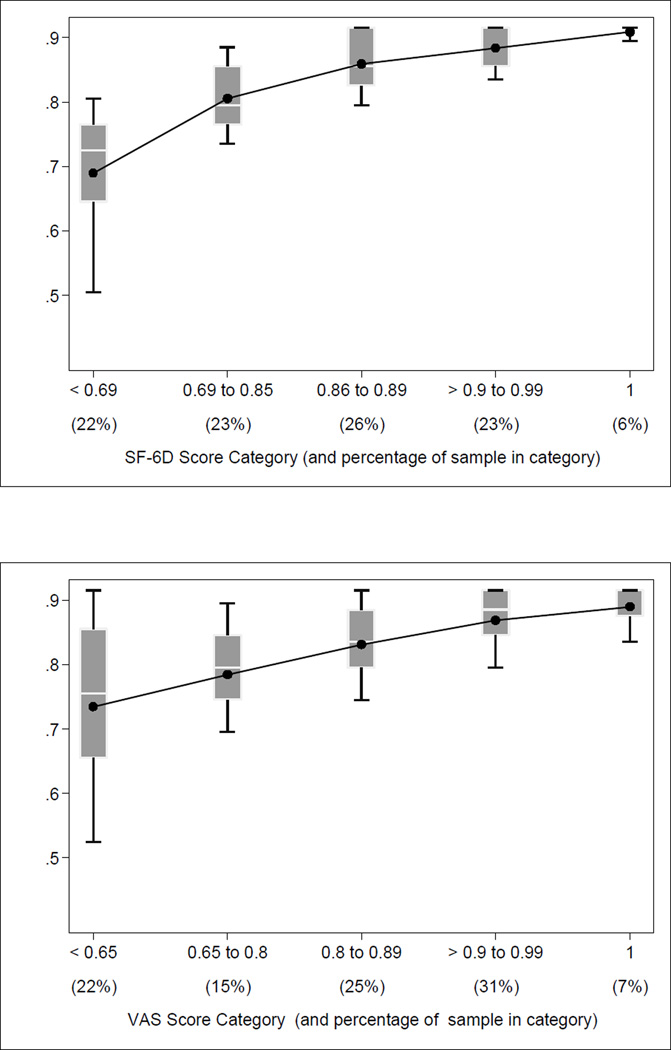
Figure 2 depicts relationships between the SSI and the other measures in pooled data from 2000–2002, with each other measure divided into categories based on the distribution of scores. As shown in box plots, mean SSI scores increased with each ascending category of SF-6D, EQ-5D, and VAS scores. The proportion of respondents with scores in each category is shown below its range on the plot.
Figure 2.
Relationships Between SSI and Other Measures in Pooled MEPS Data from 2000-2002
a) Mean SSI Scores by Categories of SF-6D Scores
b) Mean SSI Scores by Categories of HALex Scores
c) Mean SSI Scores by Categories of EQ-5D Scores
d) Mean SSI Scores by Categories of VAS Scores
Line connects mean SSI scores among those in each category of the other measure. Box plots depict range of SSI scores from 25th to 75th percentile, and 10 and 90 percent confidence intervals. White line within each bar indicates median SSI score. Percentages in categories may not sum to 100 due to rounding.
Regarding the distribution of scores on each measure, SSI scores ranged from 0.1 to 0.9, with 29% of respondents reporting none of the problems and thus having the maximum possible score of 0.92 (27% in 2000, peaking at 31% in 2003). In comparison, SF-6D scores ranged from 0.3 to 1; only 6% had no disutility/perfect scores in 2000, rising to 8% in 2010. The EQ-5D and HALex, which allow scores below zero (when a health state is considered worse than death), had the broadest range of scores (−0.14 to 0.95). On the EQ-5D, 46% had the top score (1) in 2000 (rising to 49% in 2003), indicating a ceiling effect. On the HALex, 27% had the top score (0.95) in 2000, falling slightly to 24% in 2010. Mean self-rated overall health using the VAS ranged from 0 to 1, with 7.3% reporting a score of 1 in 2000, rising to 7.8% in 2003.
SSI scores were lowered by the presence of additional impairments not asked about in other HRQOL instruments, including specific physical abilities and cognitive impairment. At least one of the broader set of symptoms and impairments was reported by 16% of those with perfect SF-6D scores, 33% of those with perfect VAS ratings, 48% of those with perfect EQ-5D scores, and 50% of those with the top HALex score. Conversely, among those with the top SSI score, 79% had a disutility on the SF-6D, 57% on the HALex, 13% on the EQ-5D, and 82% on the VAS. For EQ5D, a few people with the top SSI score reported imperfect mobility (15%) or trouble with usual activity (7%) but the majority (93%) reported some pain, showing that our use of the SF-6D pain item (pain affects work) is different than just asking about pain separate from work.
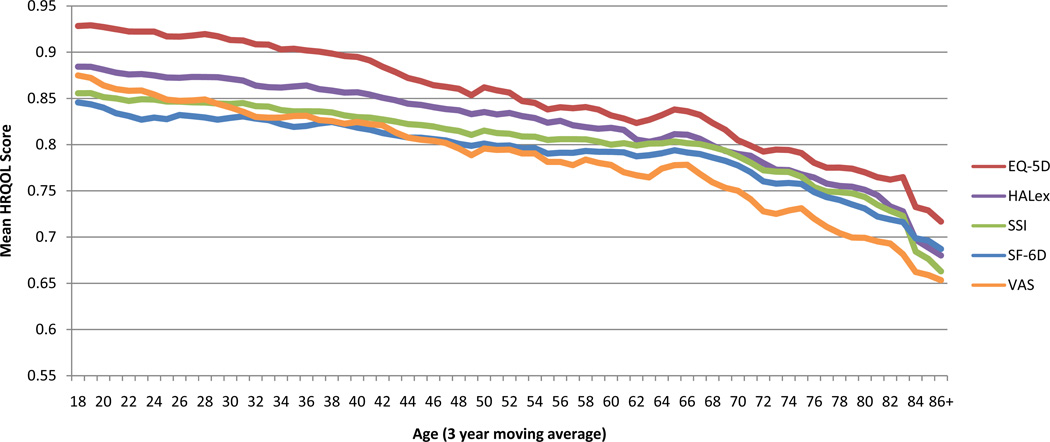
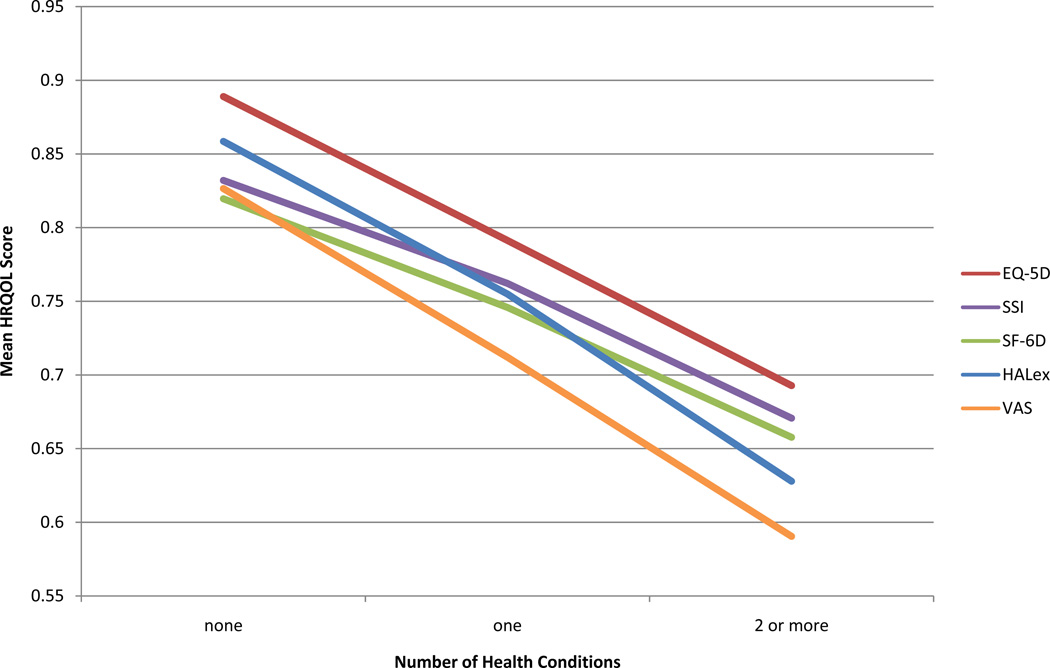
Scores on all measures declined similarly with age, as shown in Figure 3a. The VAS dropped slightly more steeply with age than other measures, yielding the lowest scores from middle age onward. Measures also showed similar trends across increasing numbers of self-reported diseases, as shown in Figure 3b. The HALex and VAS measures showed the steepest drop with increasing numbers of diseases.
Figure 3.
Comparison of Trends in Health-Related Quality of Life Using Different Measures in Pooled 2000–2002 Data
a) Comparison of Age Trends Across Measures
Note: To smooth trends, means by age are depicted using a three year moving average centered around the indicated year.
b) Comparison Scores Across Measures Among Those With None, One, or 2+ Self-Reported Health Conditions: Coronary Heart Disease, Myocardial Infarction, Other Heart Disease, Stroke, Diabetes, and Emphysema
Discussion
While there were some differences across the five measures in the level of HRQoL, the trends in HRQoL over time were similar regardless of the measure used. Comparison of HRQOL levels across measures were consistent with previous studies finding similar rank ordering of instrument scores across diseases12 and similar distributions of scores on different measures by age.13 Our estimate of HRQoL based on the broader range of survey-based symptoms and impairments questions yielded scores in between those of the other measures, made maximal use of available data, and provided the same information about trends in HRQOL as the other measures.
Our results are consistent with past findings of correlation between different HRQoL measures. The correlation among measures, particularly those based on the presence of specific impairments, supports their convergent validity. However, the measures clearly differed in their manner of capturing health, as demonstrated by the only partial overlap between top scores on different measures. Given the differences in questions and weighting/scoring across measures, this is not surprising: researchers have cautioned against assuming equivalence between scores from different questionnaires.14 Indeed, for the calculation of cost-effectiveness ratios, different measures can yield widely divergent results.15 However, while these differences across measures in the levels of HRQOL at a point in time are important, this is not the case for tracking population health trends over time, where we find similar results across measures.
In terms of the point-in-time comparisons of the level of HRQOL, our results are consistent with prior studies finding that the EQ-5D exhibits a ceiling effect in healthier populations16,17,18 Scores based on the broader range of symptoms and impairments fell between other measures in terms of the proportion with top scores, but had a lower worst possible score than the SF-6D (0.1 vs. 0.4), thus perhaps being less susceptible to floor effects among less healthy subpopulations. The EQ-5D is based on a small number of broad health questions, and thus does not capture decrements to health that may occur due to more specific symptoms and impairments. The VAS health rating may capture these decrements, but the specific problems contributing to VAS scores are unmeasured. An instrument with very broad coverage, the Quality of Well-Being Scale (QWB),19 has been recommended for avoiding ceiling effects and providing extensive detail on health in a broad swath of the population,20 however, it is lengthy to administer and its questions are not a part of MEPS so QWB scores could not be calculated for the current study. For tracking health trends over time, it appears that the scores derived from the broad range of questions already asked in national data capture the largest level of detail possible without adding unnecessarily to survey length. In support of their construct validity, all measures yielded lower mean scores with increased age and among those with increased burden of self-reported diseases. The finding that VAS ratings and HALex scores dropped more than other measures in successive age groups and among those with more diseases suggests that self-rated health (which is also part of the HALex scoring) may reflect an element of poor health or frailty not captured by other measures.21,22 However, general health ratings lack detail regarding the specific symptoms and impairments that may contribute to overall health—detail which is important in enabling understanding of the specific factors driving trends in population health over time. Global self-ratings of health have also shown discrepant trends across different nationally representative U.S. health surveys, suggesting that they may be unsuitable for population health tracking and reinforcing recommendations to use more detailed measures.23
While an examination of the underlying factors contributing to the overall QOL trend is beyond the scope of this paper, we have examined this in detail for the SSI measure in a prior paper.6 From 2000–2008, we found that HRQOL remained unchanged among non-elderly adults, and increased slightly among those over age 65. This increase was driven primarily by improved energy, as well as increased ability to work, and decreased pain, ADL limitations, and depressive symptoms. Comparing HRQOL change by gender and race, HRQOL improved among black and white respondents of both genders, with dips in the mid-2000’s for all groups, and some variation across groups. A HRQOL rise among white males in 2001 was driven by small reductions in severe depressive symptoms and low energy.
There are some limitations to our method. The SSI measure does not use traditional utility measures such as Standard Gamble or Time-Tradeoff, which require respondents to rate health scenarios directly by indicating what they would give up in order live without the health problem. Thus, our SSI scores do not reflect a true health utility in decision analytic terms. However, our scores are derived from the Visual Analog Scale, which is often used to rate health states and has been defended as a choice-based health instrument with advantages over others.24 Another limitation of our method, which is shared with utility-based measures, is our assumption that the effects of impairments and symptoms on health remain the same over time. While we have found stability in the effects of symptoms and impairments on overall health in different years of MEPS5 (2000 and 2002), these effects may be expected to change over longer time periods, as population norms and the built environment change. The occasional re-inclusion of the VAS scale in a national health survey would enable reassessment of these relationships over time. However, the effects of symptoms and impairments on health are much more stable than the effects of diseases on health over time. For example, while improved diabetes management in a population can dramatically affect the proportion of diabetics who develop impairments (such as problems with walking or vision), the effect of a walking or vision impairment on overall health would not be expected to change dramatically. Finally, our analyses exclude those living in institutions and children. While in other work we have included the institutionalized using additional data sources,6 the current comparison was restricted to the MEPS survey, which is a sample of the non-institutionalized only.
Conclusion
Calculating HRQOL using a broad range of symptoms and impairments already collected in existing national data yields population health trends similar to those seen with other well-known measures and has several important advantages. It maximizes the use of existing data and avoids the ceiling effects frequently seen with the EQ5D. It allows trends in HRQoL to be disaggregated into the specific symptoms and impairments with the greatest (and smallest) contribution to health change over time.6 Finally, HRQoL scores can be calculated based on the full set of symptoms and impairments available in any national data set,25 and do not require the consistent inclusion of a particular instrument in the same data set over time. Given the competition for space in national surveys and the absence of a gold-standard health measure for inclusion in national surveys, this is an important advantage.
Supplementary Material
Acknowledgments
This research was supported by National Institute on Aging research grant P01AG031098
Contributor Information
Susan T. Stewart, National Bureau of Economic Research, 1050 Massachusetts Ave, Cambridge, MA 02138, (phone: 1-617-852-8419, fax: 1-617-868-2742, sstewart@nber.org)
David M. Cutler, Department of Economics, Harvard University, 1875 Cambridge Street, Cambridge, MA 02138. (phone: 1-617-496-5216, fax: 1-617-495-7730, dcutler@harvard.edu) Harvard University Interfaculty Program for Health Systems Improvement, Cambridge, MA; National Bureau of Economic Research, Cambridge, MA.
Allison B. Rosen, Department of Quantitative Health Sciences and Meyer’s Primary Care Institute, University of Massachusetts Medical School, 55 Lake Avenue North, AC7-057, Worcester, MA 01605, (phone: 1-508-856-3548, fax: 1-508-856-8993, Allison.Rosen@umassmed.edu) National Bureau of Economic Research, Cambridge, MA.
References
- 1.Brooks R, Rabin RE, de Charro F, editors. The measurement and valuation of health status using EQ-5D: a European perspective. Dordrecht: Kluwer Academic Publishers; 2003. [Google Scholar]
- 2.Brazier JE, Roberts J. Estimating a preference-based index from the SF-12. Med Care. 2004;42(9):851–859. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- 3.Horsman J, Furlong W, Feeny D, et al. The Health Utilities Index (HUI(R)): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia H, Zack MM, Thompson WW. State quality-adjusted life expectancy for U.S. adults from 1993 to 2008. Qual Life Res. 2011;20(6):853–863. doi: 10.1007/s11136-010-9826-y. [DOI] [PubMed] [Google Scholar]
- 5.Stewart ST, Woodward RM, Rosen AB, Cutler DM. The impact of symptoms and impairments on overall health in US national health data. Med Care. 2008;;46(9):954–962. doi: 10.1097/MLR.0b013e318179199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart ST, Cutler DM, Rosen AB. U.S. Trends in Quality-Adjusted Life Expectancy from 1987 to 2008: Combining National Surveys to More Broadly Track the Health of the Nation. AM J Pub Hlth. 2013;103(11):e78–e87. doi: 10.2105/AJPH.2013.301250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erickson P. Evaluation of a population-based measure of quality of life: the Health and Activity Limitation Index (HALex) Qual Life Res. 1998;7(2):101–114. doi: 10.1023/a:1008897107977. [DOI] [PubMed] [Google Scholar]
- 8.Medical Expenditure Panel Survey Background. [Accessed August 31, 2012, at]; http://www.meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
- 9.Lawrence WF, Yabroff KR, Fleishman JA. Measuring health utilities in national data sets: a new approach to valuing the HALex. J Gen Intern Med. 2003;18(Suppl 1):164. [Google Scholar]
- 10.Shaw J, Johnson J, Coons S. US valuation of the EQ-5D health states: development and testing of the D1 model. Med Care. 2005;43:203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Program for calculation of SF-6D scores, personal communication from Janel Hanmer. An alternate item mapping for the SF-6D using version 1 of the SF-12 is described in the online appendix.
- 12.Franks P, Hanmer J, Fryback DG. Relative Disutilities of 47 Risk Factors and Conditions Assessed with Seven Preference-Based Health Status Measures in a National U.S. Sample: Toward Consistency in Cost-Effectiveness Analyses. Med Care. 2006;44(5):478–485. doi: 10.1097/01.mlr.0000207464.61661.05. [DOI] [PubMed] [Google Scholar]
- 13.Fryback DG, Dunham NC, Palta M, Hanmer J, Buechner J, Cherepanov D, Herrington SA, Hays RD, Kaplan RM, Ganiats TG, Feeny D, Kind P. US Norms for Six Generic Health-Related Quality-of-Life Indexes From the National Health Measurement Study. Med Care. 2007;(45):1162–1170. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kopec JA, Willison KD. A comparative review of four preference-weighted measures of health-related quality of life. J Clin Epidemiol. 2003;56(4):317–325. doi: 10.1016/s0895-4356(02)00609-1. [DOI] [PubMed] [Google Scholar]
- 15.Davis JC, Liu-Ambrose T, Khan KM, Robertson MC, Marra CA. SF-6D and EQ-5D result in widely divergent incremental cost-effectiveness ratios in a clinical trial of older women: implications for health policy decisions. Osteoporos Int. 2012 Jul;23(7):1849–1857. doi: 10.1007/s00198-011-1770-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bharmal M, Thomas J., III Comparing the EQ-5D and the SF-6D Descriptive Systems to Assess Their Ceiling Effects in the US General Population. Value in Health. 2006;9(4):262–271. doi: 10.1111/j.1524-4733.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- 17.Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Economics. 2004;13:873–884. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
- 18.Seymour J, McNamee P, Scott A, Tinelli M. Shedding new light onto the ceiling and floor? A quantile regression approach to compare EQ-5D and SF-6D responses. Health Econ. 2010 Jun;19(6):683–96. doi: 10.1002/hec.1505. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan RM, Bush JW, Berry CC. Health status: types of validity and the index of well-being. Health Services Research. 1976;11(4):478–507. [PMC free article] [PubMed] [Google Scholar]
- 20.Kopec JA, Willison KD. A comparative review of four preference-weighted measures of health-related quality of life. J Clin Epidemiol. 2003;;56:317–325. doi: 10.1016/s0895-4356(02)00609-1. [DOI] [PubMed] [Google Scholar]
- 21.Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50:S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- 22.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 23.Salomon JA, Nordhagen S, Oza S, Murray CJL. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170:343–351. doi: 10.1093/aje/kwp144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parkin D, Devlin N. Is there a case for using visual analogue scale valuations in cost-utility analysis? Health Econ. 2006;15:653–664. doi: 10.1002/hec.1086. [DOI] [PubMed] [Google Scholar]
- 25.Stewart ST, Woodward RM, Cutler DM. A Proposed Method for Monitoring U.S. Population Health: Linking Symptoms, Impairments, Chronic Conditions, and Health Ratings. NBER Working Paper No. 11358. Cambridge: National Bureau of Economic Research; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.