Abstract
Background
Recently, the Latin American Association for Palliative Care developed 10 indicators to monitor the development of palliative care and enhance the development of regional and national strategies.
Aim
To compare the status of palliative care development across Latin American nations using the Latin American Association for Palliative Care indicators and to classify the countries into three levels of palliative care development.
Methods
A secondary analysis using the following indicators (number of indicators in each category): Policy (1), Education (3), Service Provision (3), and Opioids (3). A Latin American Association for Palliative Care Index was constructed adding the standard score (z-score) of each indicator.
Setting/participants
Nineteen Spanish and Portuguese-speaking countries of Latin America.
Results
Indicators significantly associated with the number of palliative care services per million inhabitants included: the proportion of medical schools with palliative care at the undergraduate level (p = 0.003), the number of accredited physicians working in palliative care (p = 0.001), and opioids consumed per capita (p = 0.032). According to the Latin American Association for Palliative Care Index, Costa Rica registered the highest score (8.1). Three ranking groups were built to measure palliative care development; Costa Rica, Chile, Mexico, and Argentina ranked in the high group, while Bolivia, Honduras, Dominican Republic, and Guatemala ranked in the lowest group.
Conclusion
Most of the Latin American Association for Palliative Care indicators are useful for assessing national levels of palliative care development. These indicators may be applicable to other world regions. Additional studies are needed to evaluate the specificity of each indicator.
Keywords: Palliative care, development, Latin America, indicators
Introduction
For many years, the palliative care (PC) community has advocated and taken steps for systematic monitoring of PC at national and global levels. As a result, several PC organizations have published reports on the status of PC development,1–4 and in 2012, the Latin American Association for Palliative Care (ALCP for its acronym in Spanish) published the ALCP Atlas of Palliative Care.5 In addition, several organizations and PC groups have published indicators to monitor the quality of PC provision.6 A systematic review on PC indicators published recently also demonstrated that the vast majority of indicators are focused on the quality of care provision and patient outcomes.7,8 These indicators have proven to be useful at the patient and care-provider level. However, there are no published studies of PC indicators in Latin America, and at the time of this publication, the United Nations (UN) member states were not required to monitor or report on PC in international forums such as the World Health Assembly (WHA).
The World Health Organization’s (WHO) new Global Action Plan for the Prevention and Control of Noncommunicable Diseases (NCDs) 2013–20209 provides a comprehensive global monitoring framework and includes indicators and a set of voluntary global targets for the prevention and control of NCDs. One of these is the following PC indicator:
Access to palliative care assessed by morphine-equivalent consumption of strong opioid analgesics (excluding methadone) per death from cancer.
The international PC community supports the inclusion of a macro indicator, as this will contribute to the development of the field and represents a step forward toward advancement of the field. However, given that PC covers numerous other aspects in addition to pain treatment in patients with advanced cancer, PC associations have identified the need to develop additional indicators which could be used to monitor PC globally and at national levels.10
Based on the above, the ALCP requested support from the International Association for Hospice and Palliative Care (IAHPC) to help develop PC indicators that the ALCP could use to monitor and report on the development and progress of PC in the region.
The indicators were developed by a group of 10 experts convened by the ALCP in November 2012 in Lima, Peru. Members of the group included epidemiologists, clinicians, statisticians, public health specialists, pharmacists, and health administrators.11
The indicators were developed following the WHO public health model with the following components: Policy, Education, Service Provision, and Medications.12 Participants of the meeting were asked to develop macro indicators that they believed would be applicable in all countries and provide a framework that governments could use if they decided to monitor PC development. Box 1 includes the 10 indicators that were developed.
Box 1. ALCP indicators.11.
Health care policy indicator
PO.1: Existence of a current national PC plan/program (yes/no)
educational indicators
ED.1: Proportion of medical schools which include PC education in undergraduate curricula (ratio of medical schools with PC at undergraduate level/total medical schools). Here, there would be no differentiation whether the course was mandatory or voluntary, whether it was an independent course, or based on the numbers of hours or the contents.
Ed.2: Proportion of nursing schools which include PC education in undergraduate curricula (ratio of nursing schools with PC at undergraduate level/total nursing schools)
Ed.3: Number of specialized PC educational programs for physicians, accredited by the national responsible authority (absolute number). Specialized PC education is defined as specialty, sub-specialty, master, or diploma, as defined by the respective competent authority and includes all formal post-graduate degrees.
Service provision: infrastructure indicators
PS.1: Inclusion of PC in the list of services provided in the primary care level (yes = 1/no = 0)
PS.2: Number of PC care services per 1 million inhabitants defined according to the Atlas ALCP criteria
PS.3: Number of accredited/specialized physicians working in PC per 1 million inhabitants
Medication indicators
ME.1: Consumption of strong opioids per cancer death (mg per number of deaths)
ME.2: Consumption of strong opioids per capita (mg per capita)
ME.3: Number of pharmaceutical establishments that dispense strong opioids per 1 million inhabitants
The resulting indicators were shared with representatives of the Cancer Control Program at the Pan American Health Organization (PAHO) office in Washington, DC (regional WHO office for the Americas), and with Dr Willem Scholten (WHO consultant in access to controlled medicines), who also provided feedback and suggestions which were incorporated into the final report published by the ALCP.11
The aim of this study was to compare the PC status of 19 Latin American countries using the ALCP indicators and to classify the countries into three levels of PC development (ranking groups) based on percentile distributions. The purpose of this study was not to evaluate the quality of systems and provision of care.
Methods
Study design, setting/participants, and data collection
In conjunction with the ALCP indicators,5 we used secondary data collected in 2011–2012 cross-sectionally in 19 countries of the region for the ALCP Atlas for Palliative Care and databases such as the Pain & Policy Studies Group (PPSG)–Opioid Consumption Data13 and GLOBOCAN Project.14
Measurements and statistical analyses
Descriptive statistics (frequencies, percentages, means, and medians) for all variables of interest were calculated. Bivariate analyses were conducted to determine the associations between the number of PC services per 1 million inhabitants (outcome/dependent variable) and other indicators (independent variables). Although not an established gold standard for measuring “Palliative care development,” the number of PC services per 1 million inhabitants was selected as the outcome variable since this indicator represents more accurately the scope and reach of PC for patients and families in need. Service coverage implies resource allocation and may reflect advances in policy, education, and availability of medications. Statistical tests used corresponded to the variable type. Non-parametric tests were used because data were not normally distributed. Test results at a significance level of p ≤ 0.05 were considered statistically significant.
Raw scores were transformed into z-scores using this formula: z = (raw score – average) /standard deviation. A z-score indicates how many standard deviations an observation is above or below the mean. The larger the figure, the greater the distance from the average and the direction of the sign (positive or negative) indicates whether the z-score lies above or below the average.
The z-scores were calculated in order to obtain the distance between values and the distance of each value from the mean, which would not have been possible with a simple ranking. For instance, regarding PS.2 (number of PC services per 1 million inhabitants), a simple ranking would miss the distance between the first and second (Chile, 16.059 and Costa Rica, 14.645) and the second and third (Costa Rica and Uruguay 6.999). In addition, indicators with higher rankings would overshadow ones with lower rankings. Standardizing also places scores on equal parameters by avoiding raw points, and enables the comparison and aggregation of different data sets, and the scoring of countries on the basis of their comparative performance.
A national index was constructed for each country, by adding the z-score of each indicator. The distribution of this index was analyzed with percentiles building three ranking groups (75% highest, 25% lowest).
Results
Table 1 shows the distribution of the different indicators. These values were used for the analysis.
Table 1.
Countries (listed in alphabetical order) and indicators.
| Country | PS.2 | PS.1 | PS.3 | PO.1 | ED.1 | Ed.2 | Ed.3 | ME.1 | ME.2 | ME.3 |
|---|---|---|---|---|---|---|---|---|---|---|
| Argentina | 3.76 | 1 | 2.50 | 0 | 22.22 | No data | 4 | 8665.29 | 12.88 | No data |
| Bolivia | 0.58 | 1 | 0.00 | 0 | 0.00 | No data | 0 | 337.93 | 0.16 | No data |
| Brazil | 0.48 | 1 | 0.00 | 1 | 1.11 | No data | 1 | 11138.79 | 11.16 | No data |
| Chile | 16.06 | 1 | 4.10 | 1 | 9.52 | No data | 0 | 7629.77 | 10.97 | No data |
| Colombia | 0.50 | 1 | 0.90 | 0 | 5.26 | No data | 2 | 7948.43 | 6.59 | No data |
| Costa Rica | 14.65 | 1 | 11.40 | 0 | 28.57 | No data | 4 | 5305.38 | 9.63 | No data |
| Cuba | 4.54 | 1 | 3.30 | 1 | 100.00 | No data | 1 | 1223.43 | 2.16 | No data |
| Dominican Republic | 0.80 | 1 | 0.00 | 0 | 10.00 | No data | 0 | 1242.39 | .99 | No data |
| Ecuador | 0.83 | 1 | 0.00 | 0 | 25.00 | No data | 0 | 1644.88 | 1.51 | No data |
| El Salvador | 0.64 | 1 | 0.00 | 0 | 0.00 | No data | 0 | 3597.65 | 3.05 | No data |
| Guatemala | 0.48 | 1 | 0.00 | 0 | 11.11 | No data | 0 | 1779.53 | 0.92 | No data |
| Honduras | 0.24 | 1 | 0.00 | 0 | 0.00 | No data | 0 | 904.36 | 0.63 | No data |
| Mexico | 1.06 | 1 | 2.20 | 1 | 9.26 | No data | 7 | 9096.19 | 8.76 | No data |
| Nicaragua | 2.14 | 1 | 0.00 | 0 | 0.00 | No data | 0 | 2150.00 | 1.18 | No data |
| Panama | 2.64 | 1 | 0.60 | 1 | 25.00 | No data | 1 | 3666.45 | 3.03 | No data |
| Paraguay | 0.61 | 1 | 0.00 | 0 | 14.29 | No data | 0 | No data | No data | No data |
| Peru | 0.42 | 1 | 0.80 | 1 | 0.00 | No data | 0 | 2029.69 | 1.64 | No data |
| Uruguay | 7.00 | 1 | 6.10 | 0 | 100.00 | No data | 1 | 2071.62 | 5.86 | No data |
| Venezuela | 1.56 | 1 | 0.10 | 1 | 12.50 | No data | 1 | 3806.08 | 2.88 | No data |
Green: 75th percentile, red: 25th percentile, gray: no data available.
PS.2: Number of palliative care services per 1 million inhabitants, PS.1: Inclusion of palliative care in the list of services provided in the primary care level (No = 0/Yes = 1), PS.3: Number of accredited/specialized physicians working in palliative care per 1 million inhabitants, PO.1: Existence of a current national palliative care plan/program (No = 0/Yes = 1), ED.1: Proportion of medical schools which include palliative care education in undergraduate curricula (ratio medical schools with palliative care at undergraduate level/total medical schools), Ed.2: Proportion of nursing schools which include palliative care education in undergraduate curricula (ratio nursing schools with palliative care at undergraduate level/total nursing schools), Ed.3: Number of specialized palliative care educational programs for physicians, accredited by the national responsible authority (absolute number), ME.1: Consumption of strong opioids per cancer death (milligrams per cancer death), ME.2: Consumption of strong opioids per capita (milligrams per capita), ME.3: Number of pharmaceutical establishments that dispense strong opioids per 1 million inhabitants.
Two indicators were excluded from this analysis since these data were not available in the ALCP Atlas: Ed.2 (Proportion of nursing schools which include PC education in undergraduate curricula) and ME.3 (Number of pharmaceutical establishments that dispense strong opioids per 1 million inhabitants).
Health care policy indicator
PO.1: Existence of a current national PC plan/program
This indicator is aimed at monitoring the provision of PC through a public health strategy. According to national PC leaders, seven countries have a national program. However, there were no statistically significant differences between countries with or without a national program and the number of PC services per million inhabitants (Mann–Whitney t test, p = 0.499).
Educational indicators
ED.1: The proportion of medical schools which include PC education in their undergraduate curricula
Countries ranged between 0% and 100% (mean = 20; SD = 29.808; median = 10). There was a positive, statistically significant correlation (Rs = 0.656, p = 0.003) between the proportion of medical schools with PC in undergraduate curricula and the number of PC services per million inhabitants.
Ed.2: Proportion of nursing schools which include PC education in undergraduate curricula
There was no information available regarding this indicator.
Ed.3: The number of specialized PC educational programs for physicians, accredited by the national responsible authority
Only nine countries have at least one post-graduate program, with Mexico, Argentina, and Costa Rica having more and diverse active educational programs. The existence of specialized PC educational programs was moderately correlated with the number of PC services per million inhabitants, yet not statistically significant at p ≤ 0.05 (Rs = 0.411, p = 0.080).
Service provision: infrastructure indicators
PS.1: Inclusion of PC in the list of services being provided on primary care level
All participating countries had some kind of service provision on the primary level such as ambulatory consultation, home care services, or in-/outpatient hospice care.
PS.2: Number of PC services per million inhabitants
This indicator was considered the dependent variable (outcome). The number of PC services ranked from 0.24 to 16.6 per million inhabitants. Ten countries had less than one service per million inhabitants, two countries more than 10 services.
PS.3: Number of physicians working in PC per million inhabitants
The number of physicians working in PC accredited by the national responsible authority averages 1.7 per million inhabitants (SD = 2.924; median = 0.1) and ranges from 0 to 11.4 per million inhabitants. This number was positively and significantly associated (Rs = 0.694, p = 0.001) with the number of PC services per million inhabitants.
Medications indicators
ME.1: Consumption of strong opioids per cancer death
This indicator was calculated using the data of opioid consumption from the PPSG8 (nominator) as well as data from the GLOBOCAN project of the International Agency for Research on Cancer (IARC) in the ratio of the number of cancer deaths (denominator).9 Data from Paraguay were not available. The amount of strong opioids consumed per cancer patient was on average 3907 ME morphine. This measure was not significantly associated with the number of PC services per million inhabitants (Rs = 0.296, p = 0.218).
ME.2: Consumption of strong opioids per capita
This indicator was calculated using data on opioid consumption from the Pain & Policy Studies Group.8 It was positively and statistically significantly associated (Rs = 0.493, p = 0.032) with the number of palliative services per million inhabitants.
ME.3: Number of pharmaceutical establishments that dispense strong opioids per million inhabitants
No information was available regarding this indicator.
ALCP Index of PC development
The level of PC development in each country was determined by standardizing every indicator. Resulting z-scores for each were added to build a national index (Table 2). For example, a z-score was calculated for all indicators in Costa Rica and then added, obtaining a total score (index) for the country of 8.1.
Table 2.
Values of z-scores of each indicator and their summations.
| Countrya | PS.2 | PS.3 | PO.1 | ED.1 | Ed.3 | ME.1 | ME.2 | ALCP Index |
|---|---|---|---|---|---|---|---|---|
| Costa Rica | −0.78 | 0.28 | 1.44 | 2.4 | 3.23 | 0.35 | 1.17 | 8.10 |
| Chile | 1.22 | −0.34 | −0.63 | 2.69 | 0.78 | 1.05 | 1.49 | 6.25 |
| Mexico | 1.22 | −0.35 | 3 | −0.46 | 0.14 | 1.49 | 0.96 | 6.00 |
| Argentina | −0.78 | 0.07 | 1.44 | 0.11 | 0.24 | 1.36 | 1.94 | 4.39 |
| Uruguay | −0.78 | 2.61 | −0.11 | 0.79 | 1.45 | −0.62 | 0.28 | 3.63 |
| Cuba | 1.22 | 2.61 | −0.11 | 0.27 | 0.51 | −0.87 | −0.59 | 3.03 |
| Brazil | 1.22 | −0.62 | −0.11 | −0.58 | −0.6 | 2.1 | 1.53 | 2.94 |
| Panama | 1.22 | 0.16 | −0.11 | −0.13 | −0.4 | −0.14 | −0.39 | 0.22 |
| Colombia | −0.78 | −0.48 | 0.4 | −0.58 | −0.29 | 1.15 | 0.45 | −0.12 |
| Venezuela | 1.22 | −0.24 | −0.11 | −0.35 | −0.56 | −0.1 | −0.42 | −0.58 |
| Peru | 1.22 | −0.65 | −0.63 | −0.59 | −0.33 | −0.63 | −0.71 | −2.33 |
| El Salvador | −0.78 | −0.65 | −0.63 | −0.55 | −0.6 | −0.16 | −0.38 | −3.74 |
| Ecuador | −0.78 | 0.16 | −0.63 | −0.51 | −0.6 | −0.74 | −0.74 | −3.84 |
| Nicaragua | −0.78 | −0.65 | −0.63 | −0.23 | −0.6 | −0.59 | −0.82 | −4.30 |
| Guatemala | −0.78 | −0.29 | −0.63 | −0.58 | −0.6 | −0.7 | −0.88 | −4.46 |
| Dominican Republic | −0.78 | −0.33 | −0.63 | −0.51 | −0.6 | −0.86 | −0.87 | −4.58 |
| Honduras | −0.78 | −0.65 | −0.63 | −0.63 | −0.6 | −0.97 | −0.95 | −5.21 |
| Bolivia | −0.78 | −0.65 | −0.63 | −0.56 | −0.6 | −1.14 | −1.06 | −5.42 |
Dark gray: countries with a high development in comparison with the region (3.81 = 75th percentile); light gray: countries with middle development; no color: low development (less than −4.34 = 25th percentile).
ALCP: Latin American Association for Palliative Care.
PS.2: Number of palliative care services per 1 million inhabitants. PS.3: Number of accredited/specialized physicians working in palliative care per 1 million inhabitants. PO.1: Existence of a current national palliative care plan/program. ED.1: Proportion of medical schools which include palliative care education in undergraduate curricula (ratio medical schools with PC at undergraduate level/total medical schools). Ed.3: Number of specialized palliative care educational programs for physicians accredited by the national responsible authority (absolute number). ME.1: Consumption of strong opioids per cancer death (mg per cancer death). ME.2: Consumption of strong opioids per capita (mg per capita). ME.3: Number of pharmaceutical establishments that dispense strong opioids per 1 million inhabitants. ALCP Index: the summation of all z-scores.
Paraguay was excluded from this analysis since values for variable ME.1 and ME.2 were not available.
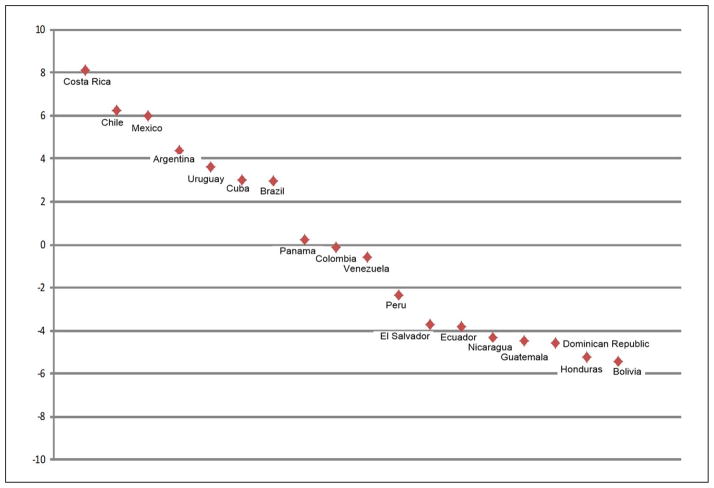
Using the index, three ranking groups were built based on the 25th and 75th percentiles for a more objective (less arbitrary) distribution. Costa Rica, Chile, Mexico, and Argentina were in the high ranking group or higher than 3.8 (75th percentile), reflecting a higher development of PC relative to the region. Bolivia, Honduras, Dominican Republic, and Guatemala were in the low ranking group with less than −4.3 (25th percentile), reflecting less development (Figure 1).
Figure 1.
State of development in palliative care according to the Latin American Association for Palliative Care (ALCP) Index.
Discussion
The level of development in each country as well as cross-country comparisons were possible using the ALCP indicators and current data available from the ALCP Atlas,5 as well as other secondary data such as the PPSG Opioid Consumption Data13 and GLOBOCAN Project.14
Countries with national programs do not appear to have more PC services than countries without national programs. This finding may suggest that the existence of a national program on paper alone does not guarantee the existence of services. Similarly, the number of specialized PC educational programs for physicians and the consumption of opioids per cancer deaths were not significantly associated with the number of PC services per 1 million inhabitants.10 Statistically significant associations between our main outcome variable and the following independent variables were found: proportion of medical schools with PC at undergraduate level, number of accredited physicians working in PC, and opioid consumption per capita. Although it is not possible to infer causality, these associations are important since they address three of the four major WHO public health model components (i.e. Education, Service Provision, and Medications). The policy indicator used by our study had no variability and ALCP should consider modifying it to capture policy differences that may exist across nations.
Our findings in general confirm expert opinion consensus regarding the level of PC development in the nations of Latin America, as well as earlier cross-national surveys assessing access to PC in Latin America.15,16 The ALCP indicators provide a general picture of the state of development of PC in Latin America, and identify three different ranking groups from highest to lowest. A vast distribution is observed, where most values occur in the tail of both sides of the individual z-values, indicating that Latin America is quite diverse and heterogeneous in relation to levels of PC development.
Findings from this study confirmed most of the results reported in the Worldwide Palliative Care Alliance (WPCA) global mapping of PC development by Lynch et al.,4 with the exception of a few countries as illustrated in Table 3. For instance, Uruguay had an ALCP Index score of 3.63 (lower than Argentina’s Index score of 4.39), yet it is rated in the WPCA map in category 4a, higher than Argentina’s category of 3b. These differences are probably due to the use of different methodologies. Lynch’s study was based on the existing literature—which is limited in Latin America—and the opinion of one local leader and the existence of a national PC association in the country.4 On the other hand, the source of data for this article was the ALCP Atlas, which included information by three and sometimes four experts from each nation. Each was required to provide specific data and the final report had to be based on consensus.
Table 3.
Comparison of ALCP Index and WPCA categorization of palliative care development, 2011.4
| Countrya | ALCP Index | WPCA global mapping (group) |
|---|---|---|
| Costa Rica | 8.10 | 4a |
| Chile | 6.25 | 4a |
| Mexico | 6.00 | 3a |
| Argentina | 4.39 | 3b |
| Uruguay | 3.63 | 4a |
| Cuba | 3.03 | 3a |
| Brazil | 2.94 | 3a |
| Panama | 0.22 | 3a |
| Colombia | −0.12 | 3a |
| Venezuela | −0.58 | 3a |
| Peru | −2.33 | 3a |
| El Salvador | −3.74 | 3a |
| Ecuador | −3.84 | 3a |
| Nicaragua | −4.30 | 2 |
| Guatemala | −4.46 | 3a |
| Dominican Republic | −4.58 | 3a |
| Honduras | −5.21 | 2 |
| Bolivia | −5.42 | 2 |
Dark gray: countries with a high development in comparison with the region (3.81 = 75th percentile); light gray: countries with middle development; no color: low development (less than −4.34 = 25th percentile).
ALCP: Latin American Association for Palliative Care; WPCA: Worldwide Palliative Care Alliance.
ALCP Index: the summation of all z-scores.
Global mapping: Group 2 = Capacity building activity; Group 3a = Isolated provision; Group 3b = Generalized provision; Group 4a = Preliminary integration.
Currently, there is no gold standard for measuring the development of PC at national levels or for international comparative studies. The indicators were elaborated based on the WHO public health model for PC and defined by a group of interdisciplinary experts in the field, providing content validity. Overall, results are consistent with the observed level of PC development in the region and reports from different countries, achieving a face validation as well.
Composite indicators as the ALCP Index are a way of simplifying complex issues into manageable concepts. The ALCP Index of PC development could be used for monitoring national and regional development and may be applicable to other regions of the world.
Limitations
This study has several limitations. Given that the indicators are intended to help member states monitor PC development at a macro level, they are not applicable in quality assessment studies at micro or mezzo levels.
The availability and quality of the data for each indicator are not the same. For example, data on the proportion of medical schools which include PC education in undergraduate curricula (ED.1) are relatively easy to collect, while others such as MS.3 (Number of pharmaceutical establishments that dispense strong opioids per million inhabitants) are very difficult to obtain.
The ALCP Atlas did not collect information on the proportion of nursing schools which include PC education in undergraduate curricula (Ed.2). Therefore, it was not possible to use this indicator in our analyses. However, based on anecdotal evidence, including the authors’ expertise and experience in PC in the region, it may be assumed that the collection of data and analysis of this indicator would be similar to ED.1 (“Proportion of medical schools which include PC education in undergraduate curricula”).
This study demonstrated that the ALCP should consider refining the following indicators:
PS.1 (Inclusion of PC in the list of services provided in the primary care level). All the responses were “YES” (variance = 0). An option may be measuring the ratio of PC services for each level of health provision to the total of services at all.
Ed.3 (The number of specialized PC educational programs for physicians, accredited by the national competent authorities). This should be adjusted for population, and not an absolute number.
ME.3 (Number of pharmaceutical establishments that dispense strong opioids per million inhabitants). A mechanism to collect this information should be identified or the indicator needs to be replaced by a more feasible one.
In general, indicators assessed in a binary way (“YES”/”NO”) such as PO.1 or PS.1 could provide more detailed information if assessed using an ordinal scale.
This ALCP Index facilitates a comprehensive and precise assessment of the state of PC development by taking into account the difference between the values of the variables and their means in units of the standard deviation. One major shortcoming of using z-scores is that the inclusion of an additional country changes scores of the others, as does a changed score in one country alone. The score cannot be taken as an absolute value which qualified the country; rather falling into a specific ranking group and its relationship with other countries in the region are more relevant.
Conclusion
The ALCP Index is a starting point for further discussion and changes in policy that will lead to improved allocation of limited resources. Additional studies are needed to evaluate the specificity of each indicator as well as validity of the indicators. Further testing and refinement of these indicators and scale may allow for the systematic and regular inclusion of PC measures in annual performance assessments of national health systems—measures imperative for improving accessibility and quality of PC.15
What is already known about the topic?
The international palliative care (PC) community has advocated the systematic monitoring of PC at national and global levels but reliable indicators are lacking. The Latin American Association for Palliative Care (ALCP) recently developed a set of PC indicators which has not been evaluated.
What does this paper add?
This study demonstrates that most of the ALCP indicators are useful to assess and monitor the level of PC development in a country and provides an index which allows for cross-country comparisons.
Implications for practice, theory, or policy
The ALCP Index of PC development could be used for monitoring national as well as comparative development of the region, and may be applicable to other regions of the world. These indicators could be applied in performance assessments of health systems to improve PC in the region.
Acknowledgments
The authors thank Professor Ralf-Dieter Hilgers (Institute for Medical Statistics at the RWTH Aachen University, Germany) for the statistical support and Dr Willem Scholten (Pharm D) for his comments.
Funding
Dr Torres-Vigil was supported in part by the National Cancer 1K01CA151785-01.
Footnotes
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
References
- 1.Centeno C, Clark D, Lynch T, et al. Facts and indicators on palliative care development in 52 countries of the WHO European region: results of an EAPC Task Force. Palliat Med. 2007;21(6):463–471. doi: 10.1177/0269216307081942. [DOI] [PubMed] [Google Scholar]
- 2.Centeno C, Lynch T, Donea O, et al. EAPC atlas of palliative care in Europe 2013—full edition. Milano: European Association for Palliative Care (EAPC); 2013. [Google Scholar]
- 3.Connor SR, Sepulveda Bermedo MC. Global atlas of palliative care at the end of life. London: Worldwide Palliative Care Alliance; 2014. http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf. [Google Scholar]
- 4.Lynch T, Clark D, Connor S. [accessed 21 November 2013];Mapping levels of palliative care development: a global update 2011. doi: 10.1016/j.jpainsymman.2012.05.011. http://www.thewpca.org/resources/ [DOI] [PubMed]
- 5.Pastrana T, De Lima L, Wenk R, et al. Atlas de Cuidados Paliativos de Latinoamérica. Houston, TX: IAHPC Press; 2012. http://cuidadospaliativos.org/atlas-de-cp-de-latinoamerica/ [Google Scholar]
- 6.Woitha K, Van Beek K, Ahmed N, et al. Development of a set of process and structure indicators for palliative care: the Europall project. BMC Health Serv Res. 2012;12:381. doi: 10.1186/1472-6963-12-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Roo ML, Leemans K, Claessen SJ, et al. Quality indicators for palliative care: update of a systematic review. J Pain Symptom Manage. 2013;46(4):556–572. doi: 10.1016/j.jpainsymman.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Stiel S, Pastrana T, Balzer C, et al. Outcome assessment instruments in palliative and hospice care—a review of the literature. Support Care Cancer. 2012;20(11):2879–2893. doi: 10.1007/s00520-012-1415-x. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization (WHO) [accessed 21 November 2013];Global action plan for the prevention and control of NCDs 2013–2020. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf.
- 10.De Lima L, Wenk R, Krakauer E, et al. Global framework for noncommunicable diseases: how can we monitor palliative care? J Palliat Med. 2013;16(3):226–229. doi: 10.1089/jpm.2012.0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Lima L, Perez-Castells M, Berenguel M, et al. Palliative care indicators—ALCP. Houston, TX: IAHPC Press; 2013. http://cuidadospaliativos.org/uploads/2013/3/Palliative%20Care%20Indicators%20ALCP%20%28english%29.pdf. [Google Scholar]
- 12.Stjernsward J, Foley KM, Ferris FD. The public health strategy for palliative care. J Pain Symptom Manage. 2007;33(5):486–493. doi: 10.1016/j.jpainsymman.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Pain & Policy Studies Group. [accessed 19 November 2013];Opioid consumption data. 2010 http://www.painpolicy.wisc.edu/opioid-consumption-data.
- 14.International Agency for Research on Cancer (IARC) [accessed 19 November 2013];The GLOBOCAN project 2010. http://globocan.iarc.fr/
- 15.Torres-Vigil I, Aday LA, De Lima L, et al. What predicts the quality of advanced cancer care in Latin America? A look at five countries: Argentina, Brazil, Cuba, Mexico and Peru. J Pain Symptom Manage. 2007;34(3):315–327. doi: 10.1016/j.jpainsymman.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Torres-Vigil I, Aday LA, Reyes-Gibby C, et al. Health care providers’ assessments of the quality of advanced-cancer care in Latin American medical institutions: a comparison of predictors in five countries: Argentina, Brazil, Cuba, Mexico and Peru. J Pain Palliat Care Pharmacother. 2008;22(1):7–20. doi: 10.1080/15360280801989195. [DOI] [PubMed] [Google Scholar]