Abstract
Background
Management of the patella during total knee arthroplasty (TKA) is controversial. Multiple studies have examined mechanical and clinical results of TKA with native and resurfaced patellae with no clear consensus.
Methods
We surveyed a large cohort of consultant surgeons in a questionnaire based study in order to assess the indications for patella resurfacing and to correlate practice with degree of specialization, experience and volume of procedures performed.
Results
Six hundred and nineteen surgeons were included. The main indication for patella resurfacing was patellofemoral arthritis. The ratio of those who always:sometimes:never resurfaced was 1:2:1 irrespective of experience or volume performed. There was no difference between knee specialists and non-specialists (p = 0.977) or between high and lower volume surgeons (p = 0.826). Senior and high volume surgeons tended to always resurface.
Conclusions
The majority of surgeons only sometimes resurfaced the patella. The number who always and never resurfaced were similar. There was a tendency for more experienced and high volume surgeons to always resurface.
Keywords: Patella, Resurfacing, Knee, Arthroplasty
There is no clear consensus on the optimal management of the patella during total knee arthroplasty (TKA). While original prosthetic designs did not include a patella resurfacing option,1) all contemporary designs provide this option. Indications for resurfacing include grade2,3) cartilage degeneration as well as the presence of inflammatory arthritis.4)
The main contraindication to resurfacing is insufficient patellar bone stock. Arguments for and against resurfacing the patella exist. While anterior knee pain has been described after TKA when the patella is not resurfaced3) complications including patella fracture, osteonecrosis, instability, and patella clunk syndrome have been described in cases in which it was resurfaced.4) Contributing to this therapeutic dilemma is a large body of evidence supporting both practices.
Waters and Bentley2) found a significantly higher incidence of anterior knee pain in unresurfaced patients. They also found that patients who had bilateral TKAs where only one side was resurfaced reported better outcomes on the resurfaced side. Burnett and Bourne5) in the longest published follow-up study to date found a 4 times revision rate in the nonresurfaced group (primarily for anterior knee pain) but no difference in functional outcome at 10 years.
Recent meta-analyses by Parvizi et al.,6) Pakos et al.,7) and Nizard et al.8) have all concluded that resurfacing the patella decreases the incidence of anterior knee pain post-TKA and reduces the risks of revision surgery.
Given this large number of studies comparing these practices and the inconclusive results of these, we set out to examine the views of practicing orthopaedic surgeons in the United Kingdom on patella resurfacing during TKA as well as their practice and the rationale for this in order to derive a consensus on this issue.
METHODS
A postal survey of members of the British Orthopaedic Association who were practicing consultant level surgeons in the United Kingdom was carried out.
A questionnaire was constructed (Fig. 1) and an application made to the British Orthopaedic Association for permission for this questionnaire to be sent to its registered members. Approval was granted and 1,601 questionnaires were sent out to registered British Orthopaedic Association consultant members in the United Kingdom. These were sent with return envelopes to maximize the response rate.
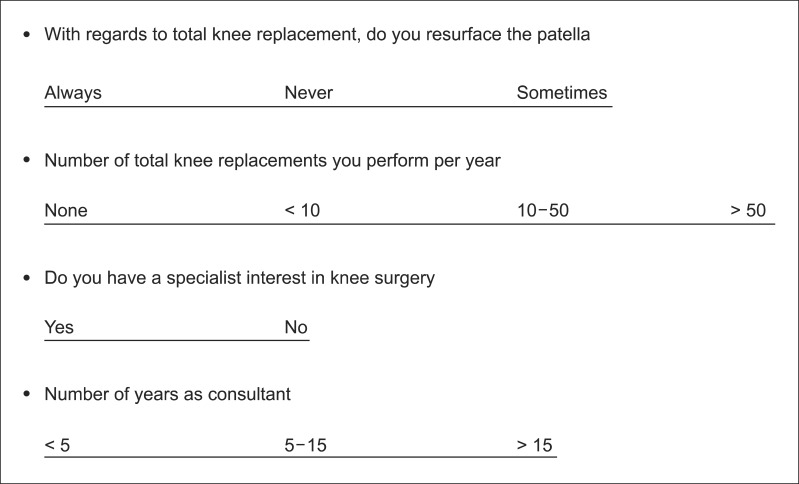
Fig. 1.
Questionnaire used for this study.
The questionnaire was designed to fit in a single page and enquired about indications for resurfacing, whether they resurfaced routinely, their experience based on years of experience and volume of surgery along with their subspecialist interests.
Results were tabulated using Microsoft Excel (Microsoft, Redmond, WA, USA) and statistical analysis was performed using the Mantel-Haenszel test-a specialized chi-square test for 3-dimensional data.
RESULTS
A total of 1,601 questionnaires were sent out. Seven hundred and sixty surgeons (47.4%) responded. Of these, 141 respondents had retired or did not perform TKAs and were excluded from further analysis. Six hundred and nineteen practicing consultant orthopaedic surgeons were therefore included in the survey.
Of this cohort 370 surgeons (67.3%) expressed a subspecialist interest in knee surgery. One hundred and ninety-two (31%) had been in consultant practice for more than 15 years and 235 surgeons (38%) performed > 50 TKAs per year.
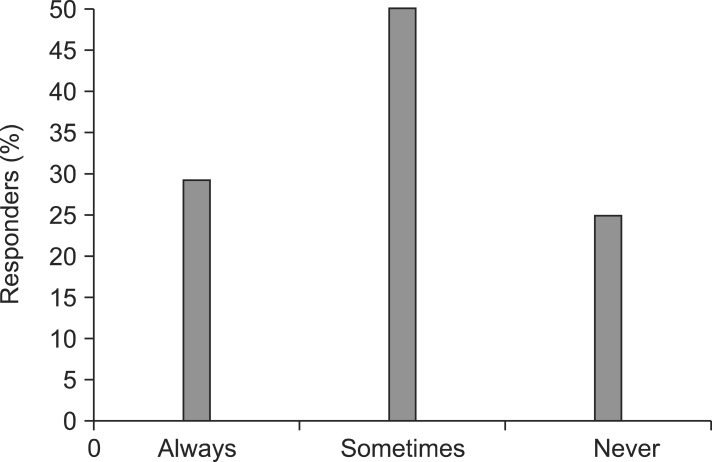
Overall 296 surgeons (48%) resurfaced the patella sometimes while 173 (28%) always resurfaced and 149 (24%) never performed patella resurfacing during TKA (Fig. 2).
Fig. 2.
Overall results.
Results are summarized in Table 1.
Table 1.
Summary of Results (n = 619)
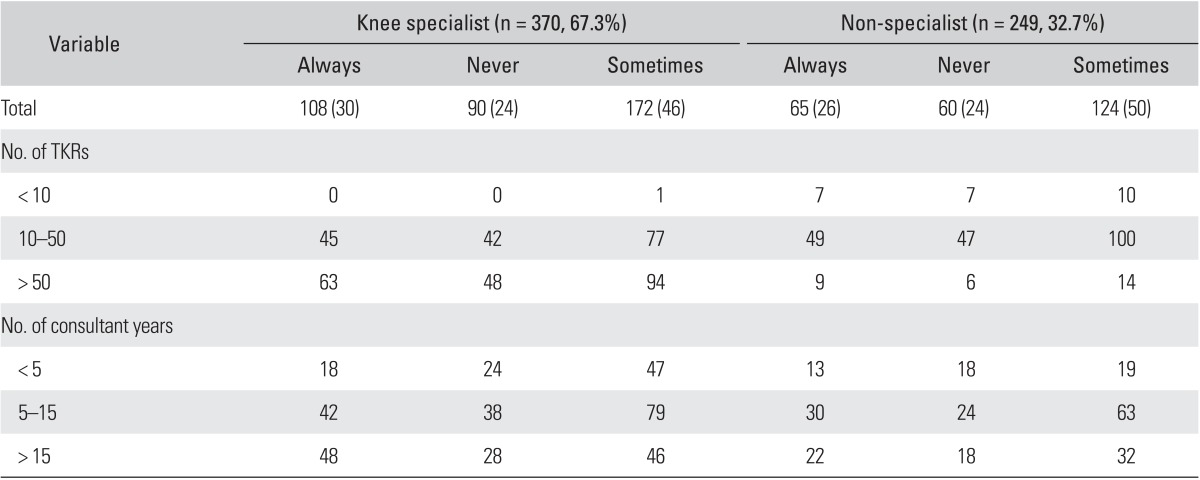
Values are presented as number (%).
TKR: total knee replacement.
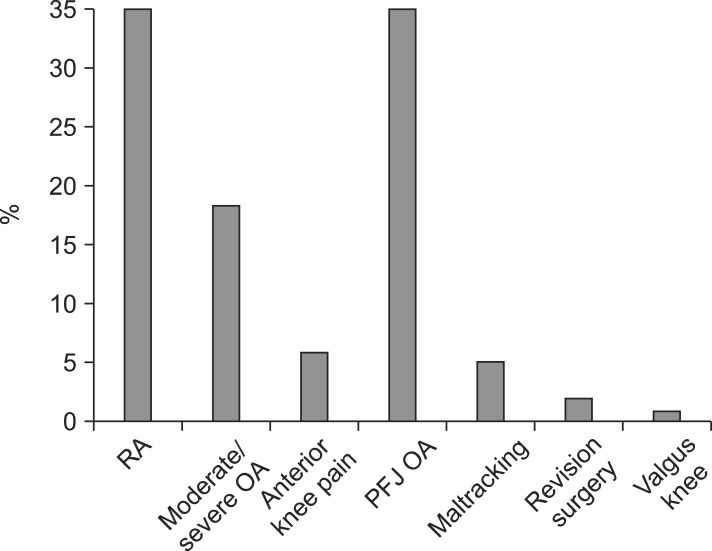
Indications for Patella Resurfacing
Indications for resurfacing the patella included rheumatoid arthritis, advanced osteoarthritis of the tibiofemoral joint and patellofemoral arthritis, among others (Fig. 3). The above three factors accounted for 86% of all indications given for resurfacing the patella.
Fig. 3.
Indications for patella resurfacing. RA: rheumatoid arthritis, OA: osteoarthritis, PFJ OA: patellofemoral joint osteoarthritis.
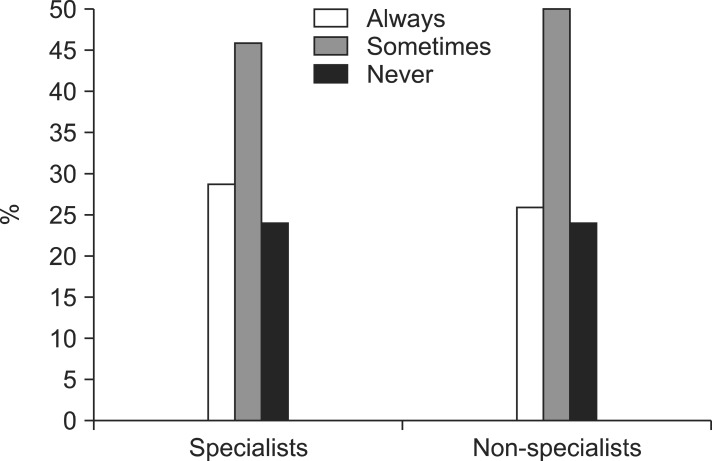
Practice Relative to Specialist Interest
Three hundred and seventy responders (60%) indicated specialist interest in knee surgery. In this group, 46% sometimes resurfaced the patella while 29% and 24% always and never resurfaced, respectively. In the non-specialist group, 50% sometimes resurfaced the patella compared to 26% who always resurfaced and 24% who never resurfaced the patella. There was no statistical difference between the specialist and non-specialist groups (p = 0.977) (Fig. 4).
Fig. 4.
Practice based on specialist interest.
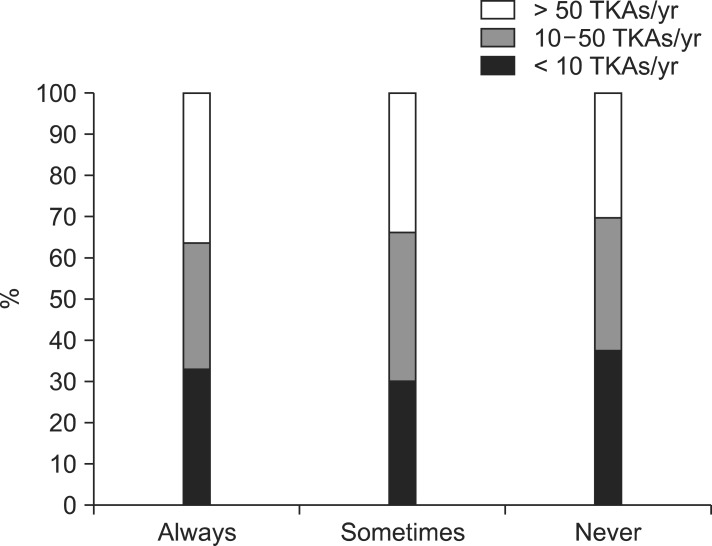
Practice Based on Volume of Procedures Performed
Fifty-eight percent (359 surgeons) of those who responded performed 10-50 TKA per year while 38% (235) performed > 50 procedures per year and 4% (25 surgeons) performed < 10 per year. In each group similar trends were noted with the majority resurfacing the patella sometimes while similar numbers always and never performing this procedure (Fig. 5).
Fig. 5.
Practice based on volume of total knee arthroplasties (TKAs) performed annually.
In the group performing greater > 50 procedures annually, 31% always and 23% never resurfaced compared to 28% and 28%, respectively, in the group performing < 10 per year (p = 0.752).
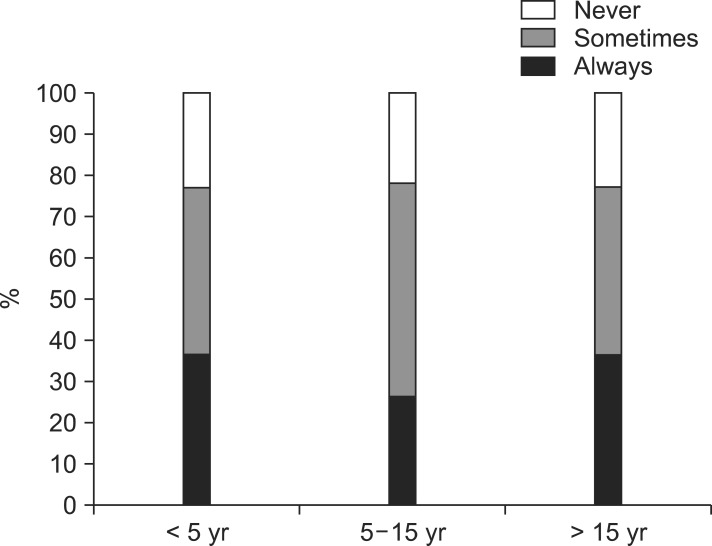
Practice Based on Experience (Fig. 6)
Fig. 6.
Practice based on experience.
One hundred and ninety-two (31%) surgeons had > 15 years consultant level experience. Seventy percent of all responders had been practicing consultants for a minimum of 5 years. Thirty-six percent of those with > 15 years experience always resurfaced the patella compared to 20% of those with < 5 years experience (p = 0.546).
DISCUSSION
Patella resurfacing during primary TKA remains a controversial issue. The 8th report of the United Kingdom National Joint Registry (NJR) revealed that the patella is resurfaced in 44% of all primary TKA procedures in the United Kingdom. Proponents of resurfacing cite higher revision rate for nonresurfaced knee due to persistent anterior knee pain while those against site the possible complications of resurfacing and no mid- to long-term benefit.
This divide is exacerbated by the presence in literature of randomized control trials and meta-analyses which are often inconclusive and therefore do not firmly support either practice. Pavlou et al.9) found no clinical difference between patients who had their patellae resurfaced and a nonresurfaced grouping a population of over 7,000 patients. They did note however that there was a higher rate of revision in the nonresurfaced group.
Calvisi et al.10) found in their appraisal of one systemic review and six randomized controlled trials, that resurfacing the patella reduces the risk for anterior knee pain when compared with patients with native patellae. They also found that patients in the nonresurfaced group experienced more anterior knee pain while climbing stairs and were less satisfied with surgery. A review of the functional outcome in 946 patients with a minimum follow-up of two years in Norwegian Arthroplasty Registry by Lygre et al.11) found no differences between the primarily resurfaced and nonresurfaced groups. Longer 10 year follow-up studies have also found no difference between the two groups.12,13)
The evidence at best is inconclusive hence we sought to derive a consensus from a large body of practicing surgeons rather than repeat studies which have already been published. Over a decade ago Phillips et al.14) examined the practice of TKA in the United Kingdom by performing a similar study. Their response rate was 62% which is possibly due to a larger number of surgeons performing TKA as practice was less specialized compared to present day. They found that 49% of surgeons sometimes resurfaced, 19% never resurfaced while 32% always resurfaced the patella during TKA but no further analysis of this subject was made. Since their study the UK NJR has been established and such epidemiological data is now readily available and though this group quantitatively assessed the number of surgeons who resurfaced the patella during TKA, no further analysis was made.
The questionnaire used in this study focused specifically on the surgeon factors which might influence the practice of patella resurfacing including level of experience in terms of years in practice and also by volume of cases. It was designed to be clear, simple to read and complete and was sent with a return envelope to maximize the response rate. The majority of consultants who replied to our survey were knee specialists (67.3%) compared to non-specialists (32.7%). This bias probably reflects the fact that those with a knee subspecialty interest are more likely to return a knee related questionnaire.
We found that comparable number of surgeons always resurface the patella as do never during TKA (28% and 24%, respectively, overall). Twice as many surgeons sometimes resurface as do always or never in a ratio of 1 : 2 : 1 (always : sometimes : never). When our results are compared to Phillips et al.,14) we find that the percentage of surgeons who sometimes resurface is relatively unchanged while those who never resurface have increased from 19% of respondents to 24%. This is perhaps accounted for by a marginal decrease from 32% to 28% in those who always resurface.
We categorized surgeons in order to ascertain whether there was a difference in practice based on specialization and experience. We found no significant difference in practice. The trend of always : sometimes : never of 1 : 2 : 1, respectively, persisted in all categories, indicating an equal proportion of surgeons who always and who never resurface the patella, regardless of whether they are knee specialists or not and likewise, a cohort who always resurface. It is interesting that surgeons believe that they can identify the patellae that need resurfacing yet find this difficult to define.
We tried to assess whether there was a difference in practice between high and low volume surgeons. We asked how many TKAs individual surgeons carried out. Surgeons were assigned into 3 groups, low volume (i.e., < 10 per year), intermediate volume (10-50 per year, i.e., up to 1 per week on average) and high volume (> 50 per year). It seems logical that surgeons with a knee subspecialty interest perform a larger volume of procedures compared to those without a specialist interest. Our results showed that 55% of the knee specialist group performed > 50 TKAs per year compared to only 11% in the non-specialist group. Overall, the majority of surgeons (58%) performed between 10-50 TKAs annually. This is comparable to findings by Phillips et al.14) where the majority performed between 20-40 procedures per year.
In the low volume group, the proportion who always and never re-surface the patella are equally divided. Similarly, in the intermediate group, the proportion of always to never is equal. In the high volume group, a larger proportion of surgeons always resurface the patella.
We also attempted to ascertain a relationship between experience (i.e., duration of time as a consultant) and clinical practice. Among those with < 5 years experience, more never resurfaced than always (28% and 20%, respectively). In the group with 5-15 years experience, almost equal numbers always and never resurfaced the patella (26% and 22%, respectively). Among the more experienced surgeons (> 15 years practice) however a larger proportion always resurfaced compared to those that never do (38% as opposed to 23%) although this was not statistically significant (Fig. 4). The reason for this trend is unclear. Two possible factors might account for this trend. Firstly the less experienced surgeons are potentially less likely have seen complications and experienced difficulties with managing patients with pain after TKA with an unresurfaced patella compared to the more experienced group. Also it is possible that time is a more important issue to the younger group as not resurfacing the patella often leads to a shorter tourniquet time. Being a 'quick surgeon' is often equated to being a good surgeon, particularly by theatre staff and this might be much more important to a surgeon in the earlier stage of their career.
In conclusion, almost half the total number of respondents (296/619, 48%) sometimes resurface the patella. However our cohort was categorized the largest proportion of surgeons sometimes resurface the patella during TKA. We believe that this reflects a diagnostic process in which each patient (and each knee) is assessed individually at the time of surgery prior to final decision-making. There is however a trend for more experienced surgeons-experienced both in terms of time in practice and volume of surgery performed-to always resurface the patella although this is not statistically significant. Future studies with a larger volume of responders might help to explain this trend.
Limitations
We recognize that a relatively small cohort of practicing surgeons (i.e., 760 of 1,601) are represented in this study; however, this cohort consists solely of practicing consultant level surgeons almost over 30% of whom have over 10 years of experience at this level of practice. Over 75,000 primary TKAs are entered into the UK NJR annually.15) Of these, 43% patellae are resurfaced at the index procedure. This almost exactly matches practice in our sample which, therefore, seems representative of national practice.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Holt GE, Dennis DA. The role of patellar resurfacing in total knee arthroplasty. Clin Orthop Relat Res. 2003;(416):76–83. doi: 10.1097/01.blo.0000092991.90435.fb. [DOI] [PubMed] [Google Scholar]
- 2.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003;85(2):212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Boyd AD, Jr, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75(5):674–681. doi: 10.2106/00004623-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Rosen AL, Scuderi GR. Patella resurfacing. Tech Knee Surg. 2002;1(1):72–76. [Google Scholar]
- 5.Burnett RS, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. Instr Course Lect. 2004;53:167–186. [PubMed] [Google Scholar]
- 6.Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438:191–196. doi: 10.1097/01.blo.0000166903.69075.8d. [DOI] [PubMed] [Google Scholar]
- 7.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2005;87(7):1438–1445. doi: 10.2106/JBJS.D.02422. [DOI] [PubMed] [Google Scholar]
- 8.Nizard RS, Biau D, Porcher R, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;(432):196–203. doi: 10.1097/01.blo.0000150348.17123.7f. [DOI] [PubMed] [Google Scholar]
- 9.Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011;93(14):1301–1309. doi: 10.2106/JBJS.J.00594. [DOI] [PubMed] [Google Scholar]
- 10.Calvisi V, Camillieri G, Lupparelli S. Resurfacing versus nonresurfacing the patella in total knee arthroplasty: a critical appraisal of the available evidence. Arch Orthop Trauma Surg. 2009;129(9):1261–1270. doi: 10.1007/s00402-008-0801-9. [DOI] [PubMed] [Google Scholar]
- 11.Lygre SH, Espehaug B, Havelin LI, Vollset SE, Furnes O. Does patella resurfacing really matter? Pain and function in 972 patients after primary total knee arthroplasty. Acta Orthop. 2010;81(1):99–107. doi: 10.3109/17453671003587069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years' followup. Clin Orthop Relat Res. 2004;(428):12–25. [PubMed] [Google Scholar]
- 13.Rodriguez-Merchan EC, Gomez-Cardero P. The outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res. 2010;468(5):1254–1257. doi: 10.1007/s11999-009-1123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips AM, Goddard NJ, Tomlinson JE. Current techniques in total knee replacement: results of a national survey. Ann R Coll Surg Engl. 1996;78(6):515–520. [PMC free article] [PubMed] [Google Scholar]
- 15.National Joint Registry for England and Wales, 8th annual report 2011 [Internet] Hemel Hempstead: National Joint Registry; 2011. [cited 2014 Aug 30]. Available from: http://www.njrcentre.org.uk/NjrCentre/LinkClick.aspx?fileticket=1TQ%2bEiNejm0%3d&tabid=86&mid=523. [Google Scholar]