Abstract
Adding to the growing literature explicating the links between romantic relationships and health, this study examined how both couple-level characteristics, particularly union type (e.g. dating, cohabiting, or marriage) and interracial pairing, and interpersonal characteristics (e.g. partner strain and support) predicted young adults’ physical and mental health. Using dyadic data from a sample of 249 young, primarily African American couples, we hypothesized and found support for the importance of couple-level context, partner behavior, and their interaction in predicting health. Interracial couples (all Black/non-Black pairings) reported worse health than monoracial Black couples. Union type, however, did not directly predict health but was a significant moderator of partner strain. That is, the negative association between partner strain and self-reported health was stronger for cohabiting and married couples versus their dating counterparts, suggesting that coresidence more so than marital status may be important for understanding partner effects on physical health. For psychological distress, however, partner support proved equally beneficial across union types.
Keywords: Dyadic data analysis, romantic relationships, self-reported health, psychological distress, African Americans, young adulthood, relationship status
In the past decade, interdisciplinary research has begun to explore the social origins of health across the life course. Much attention has been paid to the health benefits associated with marriage, and, in general, this work has found married people to be healthier than their unmarried counterparts (Liu & Umberson, 2008; Mastekaasa, 1994). This protective effect, however, appears to be contingent upon marital quality (Donoho, Crimmins, & Seeman, 2013; Umberson, Williams, Powers, Liu, & Needham, 2006). More recent work has begun to focus on the potential health benefits of intimate relationships other than marriage. Such work, however, tends to lack the attention to relationship characteristics that have proven informative in the marital literature, as the focus has primarily been on health comparisons between people in different relationship statuses (e.g. Musick & Bumpass, 2012) rather than on processes within and across such statuses that are linked to health. Consequently, we know that relationship strains and supports are important predictors of physical and mental health for the married, but we know little about the extent to which these same strains and supports predict health for those in cohabiting and dating relationships and, more importantly, if these relationship factors matter differently across union types.
Given the increased prominence of cohabitation, rising age at first marriage, and increased rates of nonmarriage in the United States over the past several decades (Cherlin, 2010), as well as the continued investment in promoting marriage by the U.S. government (Heath, 2012), understanding the extent to which relationship stressors and supports affect health similarly or differently in dating, cohabiting, and marital unions is an important undertaking. This task may be ever more relevant in minority populations given that the demographic trends cited above are even more evident for racial minorities, particularly for African Americans (Chambers & Kravitz, 2011). In addition to disparities in demographic trends, research consistently finds that African Americans, partly as a consequence of “weathering” persistent exposure to discrimination and minority stress (Geronimus, Hicken, Keene, & Bound, 2006), have worse health than other racial groups in the United States (Williams, 2012). Such inequalities underscore the importance of investigating the potential effects of supports and stressors within various types of African American romantic relationships.
The present study utilizes a sample of young couples, all of which contain at least one African American partner, to examine how both relationship strain (partner hostility) and support (partner warmth) are associated with physical and mental health across multiple union types. In doing so, it builds on and expands past research in several ways. Like past work, we attend to multiple dimensions of relationships as well as multiple dimensions of health. Unlike most past research, however, our data permit us to distinguish between couple, actor, and partner effects on health, thus allowing us to assess more precisely the “truly relational” (Kenny, Kashy, & Cook, 2006, p. 147) character of young adults’ health. For instance, the “marriage benefit” posited to date is essentially a dyad-level effect but has not been studied as such. Likewise, as indicated above, African Americans report worse health than members of other racial groups, but emerging research suggests that couple-level racial context (i.e. interracial pairing) also matters for health (e.g. Bratter & Eschbach, 2006). Hence, our data allow us not only to explore these contextual effects but also to place the effect of partner support and strain within this couple-level context.
A second contribution of the current study, then, is that it not only assesses couple- and individual-level effects at their proper level of analysis, but it also explores the potential cross-level interactions between couple-level context and individual actor and partner effects. Although there is some evidence suggesting that different union types may entail differing degrees of interdependence between partners (Saxbe & Repetti, 2010), it is unclear the extent to which this is the case. The use of dyadic data allows us to test differences in this interdependence by attending to the ways in which partner effects may vary across relationship statuses.
COUPLE CONTEXT AND HEALTH: UNION TYPE AND INTERRACIAL PAIRINGS
There has been an ongoing debate amongst family and health scholars regarding the health benefits of marriage. In general, research has found that married people tend to be healthier than their unmarried counterparts on several measures, including mortality (Rendall, Weden, Favreault, & Waldron, 2011), psychological distress (Mastekaasa, 1994), self-rated health, and physical disabilities (Schoenborn, 2004). As several scholars (e.g. Carr & Springer, 2010) have pointed out, however, our understanding of this “marriage benefit” has been muddied in the past decade.
Work by Liu and Umberson (2008) provided evidence that the marriage benefit is dependent on sociohistorical context, in that the self-reported health gap between married and never-married individuals has closed over time, particularly for men. Others have pointed to the heterogeneity among never-married individuals and have asked to what extent the health benefits of marriage might also extend to nonmarital cohabitation. For instance, Liu and Reczek (2012) recently reported that, among Whites in the United States, married respondents had a lower mortality risk compared to their cohabiting counterparts. Alternatively, using a Danish sample, Drefahl (2012) found that, when education and other selective factors were considered, married and cohabiting men did not differ on mortality risk. In fact, at high levels of education, cohabitation resulted in reduced mortality risk for men. Likewise, using fixed effects models, Musick and Bumpass (2012) found that married persons did report better health than cohabitors, but the opposite pattern was found for happiness and self-esteem outcomes.
Much of this research on the marriage benefit has been limited by its heavy focus on White and relatively older samples. This emphasis is problematic not only because older samples provide little insight into the development and origins of health problems but also because it precludes in-depth analyses on populations for whom nonmarital relationship statuses, rather than marriage, predominate. For instance, roughly three-fourths of American men and two-thirds of American women aged 20–29 have never been married (Kreider & Ellis, 2011). Marriage is even less common among Blacks and particularly among Black young adults, as the median age at first marriage for Blacks is 30.8 for men and 30.3 for women compared to 28.3 and 26.4 for White men and women, respectively (Payne, 2012). Correspondingly, cohabitation is now the most common form of first union and the normative route to marriage (Bumpass & Lu, 2000). Further, some evidence suggests that the role of cohabitation relative to marriage may differ for Blacks and Whites, in that cohabitation may be more of an alternative to marriage for Blacks than it is for Whites (Chambers & Kravitz, 2011). These data suggest that the portrait of marriage and health painted thus far in the literature may not be applicable to recent cohorts of young people, especially young Blacks.
In fact, research that focuses specifically on young adults has tended to find few differences in relationship quality by union type (e.g. Kamp Dush & Amato, 2005) and few differences between cohabiting and married partners on indicators of health (e.g. Uecker, 2012). Further, some work that examines race differences in the marriage benefit finds that marriage and cohabitation do not differentially predict mortality for Blacks as they do for Whites (Liu & Reczek, 2012). Such findings may reflect the normality of cohabitation in relation to marriage among both young people and Blacks, as much research suggests that differences between cohabitation and marriage (in both their character and their association with wellbeing) are less striking in contexts where cohabitation is more normative (e.g. Lee & Ono, 2012).
Emerging research suggests, however, that another couple-level factor—interracial pairing—may prove particularly predictive of health. While interracial marriages have increased over the past several decades, interracial unions with Blacks continue to be less common and more stigmatized than those between non-Blacks (Burton, Bonilla-Silva, Ray, Buckelew, & Freeman, 2010). Black-White interracial couples have been shown to receive less social support than their monoracial counterparts (Chito Childs, 2005), and as Onwuachi-Willig & Willig-Onwuachi (2009) argue, monoracial heterosexual couples enjoy social and legal privileges that interracial couples often do not. In fact, they assert that certain privileges that people enjoy outside of the context of intimate relationships (e.g. gender or race privileges) may disappear in the context of an interracial romantic pairing and that partners of an interracial couple may face unique stressors, like the “daily microaggression of having [their] status as a family assumed away” (p. 240). In light of such stressors, researchers have found that interracial marriages are at a higher risk for divorce than monoracial marriages (Bratter & King, 2008), and that members of interracial couples, particularly those involving a Black partner, report more psychological distress (Bratter & Eschbach, 2006; Kroeger & Williams, 2011).
There is mixed evidence as to the extent to which such patterns are a result of lower relationship quality in interracial couples. Kroeger & Williams (2011) found, for instance, that young adults who are involved in interracial relationships with Black partners reported lower relationship satisfaction than those involved with non-Black partners and that these differences in relationship satisfaction partially explained the association between interracial coupling and psychological distress. In contrast, Troy, Lewis-Smith, and Laurenceau (2006) found that partners in interracial unions actually reported greater relationship satisfaction and no more conflict than those in monoracial unions. Hence, it is unclear whether the interracial pairing effect may be accounted for by the stressors and supports inherent in interracial relationships. We now turn to a discussion of these stressors and supports and of their implications for health.
RELATIONSHIP STRAIN, RELATIONSHIP SUPPORT, AND HEALTH
Perhaps the most robust complication of the marriage benefit literature to date has come from research highlighting the important role of relationship quality in understanding the effects of romantic relationships on health. This work follows from the stress/social support hypothesis (Burman & Margolin, 1992), which views intimate relationships not only as a likely source of support but also as a possible stressor. Using a variety of health outcomes, research operating from this perspective has consistently shown that marital supports and stressors not only help to explain health differentials among married individuals but also help to condition the marriage benefit. For instance, marital supports and stressors have been associated with metabolic syndrome (Whisman, Uebelacker, & Settles, 2010), blood pressure (Holt-Lunstad, Birmingham, & Jones, 2008), self-reported health (Umberson et al., 2006), and psychological distress (Whisman & Kaiser, 2008). As for conditioning the marriage benefit, several studies have suggested that “being married is not advantageous if the marriage is of poor quality” (Holt-Lunstad et al., 2008, p. 242). Work on nonmarital relationships also suggests that the supports, particularly wanted supports (Maisel & Gable, 2009), and stressors within these unions have positive and negative health implications, respectively, although most of this work has focused only on mental health (e.g. Simon & Barrett, 2010). Taken together, this work suggests that a stressful relationship, no matter its form, should be negatively linked to health, and a supportive relationship should be positively linked to health.
Mechanisms Linking Relationship Support and Strain to Health
Based largely on research among married couples, three physiological pathways – cardiovascular function, endocrine function, and immune function (Robles & Kiecolt-Glaser, 2003)— linking the supports and stressors within romantic relationships to health have been identified. The latter pathway, however, has been gaining prominence among family researchers, as inflammatory biomarkers involved in immune system dysregulation have been implicated in the development of many chronic diseases and have been linked to relationship supports and stressors in both correlational and experimental studies (Donoho et al., 2013; Kiecolt-Glaser, Gouin, & Hantsoo, 2010; Whisman & Sbarra, 2012). Importantly, recent research suggests that inflammation is strongly implicated in people’s global assessments of their own health (Christian et al., 2011) and in depressive symptomatology (Howren, Lamkin, & Suls, 2009), the two dimensions of health attended to in the current study.
Such physiological processes imply a direct effect of partner support and strain on health. It is possible, however, that partner support and strain may be linked to health more indirectly through relationship satisfaction (South & Krueger, 2013; Whitton & Whisman, 2010). Although this indirect pathway may not be wholly distinct from physiological processes, it suggests that one avenue linking a partner support and strain to health is through one’s own cognitive appraisal of the relationship. We attend to this possibility by exploring the ways in which relationship satisfaction may help to attenuate the effects of partner support and strain.
Gender, Romantic Relationships, and Health
There is much debate within the literature concerning the degree to which both romantic relationship status and quality are differentially associated with health for men and women (Simon, 2002). In recent work, there is mixed evidence on the potentially gendered effects of relationship supports and stressors on health. For instance, Umberson et al. (2006) found that marital quality affected men’s and women’s health in similar ways over the life course. On the other hand, both Whisman & Sbarra (2012) and Donoho, Crimmins, and Seeman (2013) reported marital support to be linked to markers of inflammation in women but not men, while Whisman, Uebelacker, and Settles (2010) found similar gendered effects when examining the link between marital distress and metabolic syndrome. Like most relationship research, much of the work exploring gender differences has focused on White married samples.
Limitations of Past Research
Although the literature cited thus far has certainly provided a more nuanced understanding of when, how, and for whom relationships affect health, this work has been limited in several regards. First, because studies rarely contain individuals in multiple relationship statuses and measures of relationship stressors and supports across these different statuses, we are often comparing relationships based simply on union type or are restricted to making relatively simple comparisons by relationship quality (e.g. high/low-quality marriage versus no marriage; for an exception, see Kamp Dush & Amato, 2005). This lack of data has prevented researchers from examining whether the relationship factors that predict health among the married also predict health among those in nonmarital relationships and the extent to which they do so to similar degrees. Further, given evidence that relationship status may be confounded with relationship quality, the lack of attention to quality across multiple relationship statuses may have led us to overestimate union type effects.
A second limitation of existing work is its lack of couple-level or dyadic analyses, particularly among young people and persons across multiple relationship statuses. As a consequence of this data restriction, most of the effects examined to date have primarily been of a particular type, that of actor effects, or the effect of one’s own report of the situation on one’s own outcomes (Kenny et al., 2006). Not only is a reliance on this method plagued by shared method variance but it prevents us from examining partners’ influences on one another, or partner effects, and from distinguishing these individual-level effects from the contextual influence of the couple. Such distinctions not only allow for proper contextualization of actor and partner effects but also allow for an examination of the extent to which the couple-level context may condition such effects. These potential cross-level interactions become particularly relevant to the current research in light of recent findings by Saxbe and Repetti (2010) showing that the coregulation of partners’ affect and cortisol levels was “fueled by time spent in shared environments” (100). This work suggests that couples who live together and presumably spend more time together in shared living spaces may be more influenced by their partners than those not living together. Such differential partner effects, however, cannot be adequately assessed with data from only one member of a couple.
Current Study
In light of these limitations of past work, the current study utilizes a sample of young African American couples to address four goals: (1) to examine how couple-level context, particularly union type and interracial pairing, is associated with both physical and mental health, (2) to assess how individual-level relationship support (partner warmth) and strain (partner hostility), embedded within their proper relational context, are linked to health, (3) to evaluate the extent to which these partner effects differ in their association with health by union type, and (4) to explore the extent to which relationship satisfaction helps to mitigate the link between partner support/strain and health.
Related to our first research goal regarding the couple-context of relationships, given the inconsistent evidence regarding relationship status differences in health, particularly for young and Black samples, we do not expect union type to exert a direct influence on health. Consistent with past work on the external stressors faced by interracial couples, however, we do expect that such couples will report lower levels of self-reported health and greater levels of psychological distress than their monoracial counterparts (Hypothesis 1). If this couple-level effect, however, is due to the stressors and (lack of) supports internal to these interracial relationships, it should be largely attenuated when such stressors and supports are taken into consideration. Within the couple-level context of untion type and interracial pairing, we anticipate that, consistent with the stress/social support hypothesis, partner warmth will be positively and partner hostility will be negatively associated with health (Hypothesis 2). Given the theoretically increased interdependence of partners sharing living space, however, we also expect these partner effects will be stronger among cohabiting and married couples than among their dating counterparts (Hypothesis 3). Finally, we posit that relationship satisfaction will be positively associated with health and may help to explain the links between partner support/strain and health (Hypothesis 4). Given the mixed evidence suggesting that men and women may respond to relationship supports and stressors differently, we also test the extent to which gender moderates the links between partner support/strain and health but do not hypothesize any specific gendered patterns.
METHOD
To test the above hypotheses, we utilized the most recent wave of data from the Family and Community Health Study (FACHS), an ongoing research project aimed at understanding the social, psychological, and contextual risk and protective factors associated with African Americans’ health and wellbeing across the life course (see [authors names removed for blind review] for a detailed description of sampling procedure). In 1997, a total of 889 African American families from Iowa and Georgia1 participated in the first wave of data collection. Each family had a child who was in the 5th grade in the public school system at this time, and follow-up interviews with these children and their families were conducted every 2–3 years thereafter.
A total of 699 target youth (78.63% of original sample) completed surveys at Wave VI, the most recent wave, in 2010 and 2011. At this time, the romantic partners of those targets who were involved in a romantic relationship were invited to participate in the study. In total, 307 respondents (43.69% of the total Wave VI sample, or 78.32% of those involved in a romantic relationship) had partners participate in the study. There was little evidence of selection bias when comparing those respondents who had participating romantic partners to those whose partners did not participate. For instance, these groups did not differ significantly with regards to age, education, work status, school status, income, relationship commitment, relationship satisfaction, religious involvement, and self-reported health. Those with participating romantic partners, however, were more likely to have a child together than those whose romantic partner did not participate. There was also little evidence of selective attrition across the study waves, as those who participated in Wave VI did not differ from their nonparticipating counterparts on educational aspirations and expectations, household income, family structure, or parental hostility at Wave I. Respondents were, however, slightly more likely to be female at Wave VI than at Wave I.
In the current study, the same-sex couples (n = 5, or 1.63% of all couples) were dropped from the sample. Further, 23 couples who responded that they were dating one person on a regular basis but were “still free to see other people” were excluded from the analyses given our interest in committed dating, cohabiting, and married relationships. An additional 30 couples (9.77%) were excluded for one or both partner’s incomplete data on the key variables of interest. The present study, then, focused upon the subset of respondents who were involved in a committed romantic relationship with a different-sex partner and who provided complete data. The final sample consisted of 498 individuals, or 249 dyads. Importantly, as indicated above, although the original FACHS data were restricted to African American targets, the romantic partners of these targets were not required to be African American in order to participate in the study. Hence, all couples in the sample were comprised of at least one African American partner, but the vast majority (76%) was comprised of two.
Dependent Variables
Self-reported Health
For both members of the dyad, self-reported health was assessed via one item that asked respondents how they would describe their health “right now.” Potential responses included 1 = Not very good to 5 = Excellent. Because only 18 respondents (3.61%) reported their health as “not very good,” this response was combined with response category 2 (fair health), resulting in a 4-category, ordered variable.
It is important to note that this single-item, self-reported measure of health has been shown to be a robust indicator of chronic inflammation, indicated by the presence of serum proinflammatory cytokines, particularly interleukin (IL)-6 and C-reactive protein (CRP). Christian et al. (2011) showed that associations between self-reported health and both IL-6 and CRP were robust even to statistical controls for perceived change in health, body mass index (BMI), diagnosed health conditions, depressive symptoms, and health behaviors and were not diminished by any particular facet of health (e.g. bodily pain or disability). The authors conclude that global self-assessments of health “provide important clinical information regarding inflammatory status, beyond traditional objective risk factors, even among generally healthy individuals” (p. 1496). Hence, although the single-item, self-reported measure of health used here lacks multidimensionality, it is a robust indicator of physical health and, hence, mortality (Idler & Benyamini, 1997).
Psychological Distress
For both members of the dyad, psychological distress was assessed with a 9-item index based on the items found in the University of Michigan Composite Diagnostic Interview (UM-CIDI; Kessler 1994). Respondents were asked to report whether or not they experienced several symptoms of depression (e.g. “felt sad, empty, or depressed most of the day” and “lost interest in things”) for at least a two-week period in the past year. Responses ranged from 0 = No to 1 = Yes. All respondents were asked all 9 items, and items were summed to create a measure of psychological distress for each relationship partner (α = .84).
Primary Independent Variables
Prior to discussing relationship support and strain, two dyad-level predictors, union type and interracial couple, are relevant to the above hypotheses. Target report of current union type was used to distinguish those couples who were married, cohabiting (living together with or without plans to marry), and dating (in a committed relationship but not living together). Given that the initial FACHS sample contained only African American youth, interracial couples were identified by asking the targets’ romantic partners which racial group they considered themselves to be a member of. Dyads in which the romantic partner identified as something other than African American were coded 1 for being an interracial couple. Hence, all interracial couples contain one African American partner and one non-African American partner. The remaining predictors of interest concern those individual-level factors internal to the relationship: relational hostility, warmth, and satisfaction.
Hostility
Both partners of the dyad were asked 5 questions concerning the degree to which their partner displayed hostile behaviors (e.g. criticized or insulted) toward them during the past month and 5 questions concerning the degree to which they displayed these same behaviors toward their partner. Such questions were drawn from the Revised Conflict Tactics Scale (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Responses ranged from 1 = Never to 7 = Always. In total, four measures of hostility were created; these included respondents’ report of their own behavior, respondents’ report of their partners’ behavior, partners’ report of respondents’ behavior, and partners’ report of their own behavior. To gain the least biased assessment of each partner’s hostile behavior, to lesson bias due to shared method variance, and to reduce multicollinearity in the models, a final measure of respondent (actor) hostility was created by summing the actor report of his/her own hostile behavior with the partner report of the actor’s hostile behavior. Likewise, a final measure of partner hostility was created by summing the partner report of his/her own hostile behavior and the actor report of the partner’s hostile behavior. In other words, given no third-party observations, each partner’s behavior was a compilation of self- and partner-perceptions (α ranged from .71 to .73).
Warmth
Both partners of the dyad were asked 3 questions concerning the degree to which their partner displayed warm and supportive behaviors (e.g. helped do something important or showed affection) toward them during the past month and 3 questions concerning the degree to which they displayed these same behaviors toward their partner (Surjadi, Lorenz, Wickrama, & Conger, 2011). Responses ranged from 1 = Never to 7 = Always. Actor and partner reports of their own and their partner’s warm behaviors were combined in the same way as with the hostility items above such that each partner’s behavior was a combination of self- and partner-perceptions (α ranged from .82 to .83).
Satisfaction
For both partners, relationship satisfaction was assessed via two questions, one asking how “happy” (1 = Extremely unhappy to 6 = Extremely happy) and the other asking how “satisfied” (1 = Not at all satisfied to 5 = Completely satisfied) respondents were with their relationship. Because there were different metrics for each item, responses were standardized and then summed to form an index of relationship satisfaction (α = .71) for each partner.
Moderating and control variables
It was necessary to include statistical covariates that have been linked to either health or relationship quality in past research in order to help mitigate the risk of spuriousness in the associations of interest. Gender, which was self-reported by dyad members is controlled in all models and also serves as a potential moderating variable. At the dyad level, controls included whether or not the romantic partners shared a child (1 = yes) and the length of the relationship (measured in years). At the individual level, demographic controls included highest level of education (in years), current school status (1 = currently enrolled in school) given that many respondents had not yet finished their education, age (in years), and work status (1 = employed). Further, objective and behavioral indicators of health were controlled. These controls included body mass index (BMI), calculated using respondents’ self-reported weight and height, insurance status (1 = respondent lacks health insurance), and frequency of vigorous exercise (measured in number of days in the last week).
Plan of Analysis
As previously mentioned, a major limitation of much relationship and health research to date has been its focus on the individual as the unit of analysis and, hence, its tendency to focus on actor effects, or the association between one’s own characteristics and one’s own health outcomes. Although such analyses are insightful, they often do not take seriously the fact that “humans exist within relationships and are therefore reactive and responsive to inputs from friends, partners, and children” (Saxbe & Repetti, 2010:92). In other words, focusing on the individual as the unit of analysis fails to consider the possibility that each person’s outcome is affected not only by his/her own characteristics (actor effects) but also by the relationship context (dyad-level effects) and the characteristics of the romantic partner (partner or transactional effects). To the extent to which dyad and partner effects have been considered in the literature, they have typically been examined with individual-level data and, hence, have not accounted for the interdependence between romantic partners. In order to overcome these limitations, we utilized the Actor-Partner Interdependence Model (APIM; Kenny et al., 2006).
Given the large number of control variables and the absence of latent constructs from the analyses, a multilevel modeling approach for dyadic data analysis was used via HLM version 6.0 (Raudenbush & Bryk, 2002). The present data, like all dyadic data, have a hierarchical structure of individuals nested within couples. For self-reported health, a 4-category, ordered dependent variable, ordinal hierarchical generalized linear modeling (HGLM) was used. The ordinal HGLM model provides the log-odds of being in the lowest category on the dependent variable. Hence, for the regression analyses, the dependent variable of self-reported health was reverse-coded such that the log-odds presented are predictive of better health. For psychological distress, an overdispersed count variable, a negative binomial HGLM was used. Such a model predicts the log of the event rate. For easier interpretation of results, the coefficients for both the ordinal and negative binomial HGLMs were exponentiated, thereby transforming them into odds ratios and event rate ratios, respectively. For each model, the intercept was allowed to vary randomly across couples. In addition, all continuous predictors were centered at the grand mean.
The analyses proceeded in several steps. First, we explored the unconditional or baseline HGLMs, which provided us with the average physical and mental health of the sample. We then moved on to the conditional models. For each outcome, we began with a model consisting of all dyad-level predictors and individual-level control variables. This model was followed by two models that examined the associations of actor and partner hostility and warmth on health. Following an assessment of these direct associations, cross-level interaction terms between relationship factors and union type were considered. Finally, we tested the effect of relationship satisfaction and the role that it may play in mitigating the partner effects of interest.
RESULTS
Descriptive Statistics and Unconditional Model
Table 1 provides the means and standard deviations for all variables used in the study. Due to space limitations, we do not discuss these descriptive statistics here. Prior to examining the hypothesized predictors of self-reported health, three preliminary analyses are worth noting, however. First, given that we were interested in understanding the extent to which union type may condition the associations between partner supports/strains and health, it was important to identify if and how partner support/strain may vary by union type. Analyses of variance suggested that warmth (F = .42, p > .10), hostility (F = .44, p > .10), and relationship satisfaction (F = 2.00, p > .10) did not differ significantly by union type. Also of interest are the results of the unconditional HGLMs (not shown). For self-reported health, this empty model indicated that the mean log-odds of reporting “excellent” health versus the other health categories was −1.82, which translates into an odds ratio of .16 [exp(−1.82)] and a probability of .14 [1/(1+exp− (−1.82))]. On average, then, respondents had only a 14% probability of reporting “excellent” health. The unconditional model for psychological distress indicated that the mean number of depressive symptoms was 1.69. As indicated by a significant random effect for each outcome (self-reported health: μ0 = 0.48, X2 = 321.74, p < .01; psychological distress: μ0 = 0.25, X2 = 341.73, p < .001), there was significant between-couple variation, or partner dependence, for each outcome. Confirming this interdependence, actor and partner self-reported health (r = .13, p < .01) and actor and partner psychological distress (r = .07, p < .10) were positively correlated.
Table 1.
Descriptive Statistics
| Mean | Std. Deviation | |
|---|---|---|
| Child | .514 | .500 |
| Relationship Length | 3.301 | 1.669 |
| Dating | .683 | .466 |
| Cohabiting | .213 | .410 |
| Married | .104 | .306 |
| Interracial Couple | .237 | .426 |
| Women | Men | Gender difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean | Std Deviation | Min | Max | Mean | Std. Deviation | Min | Max | ||
| Self-reported health | 2.197 | .978 | 1.000 | 4.000 | 2.598 | .992 | 1.000 | 4.000 | *** |
| Psychological distress | 1.888 | 2.430 | 0.000 | 9.000 | 1.635 | 2.108 | 0.000 | 9.000 | |
| Age | 23.582 | 2.173 | 19.000 | 37.000 | 25.490 | 3.921 | 18.000 | 44.000 | *** |
| Education | 12.827 | 1.598 | 8.000 | 17.000 | 12.414 | 1.582 | 3.000 | 17.000 | ** |
| In school | .594 | .492 | 0.000 | 1.000 | .378 | .486 | 0.000 | 1.000 | *** |
| Employed | .659 | .475 | 0.000 | 1.000 | .663 | .474 | 0.000 | 1.000 | |
| No health insurance | .329 | .471 | 0.000 | 1.000 | .486 | .501 | 0.000 | 1.000 | *** |
| BMI | 29.581 | 8.386 | 16.072 | 70.684 | 27.132 | 5.908 | 18.457 | 62.312 | *** |
| Frequency of exercise | 1.984 | 1.103 | 1.000 | 5.000 | 2.574 | 1.243 | 1.000 | 5.000 | *** |
| Warmth | −.015 | 1.623 | −4.673 | 2.066 | −.019 | 1.550 | −4.976 | 2.066 | |
| Hostility | .349 | 1.964 | −1.564 | 8.776 | −.338 | 1.114 | −1.564 | 5.376 | *** |
| Satisfaction | −.156 | 1.825 | −6.615 | 2.534 | .073 | 1.726 | −6.615 | 2.534 | |
p≤.10,
p≤.05,
p≤.01,
p≤.001
N = 249 different-sex dyads
Conditional Ordinal HGLM Results
Tables 2 and 3 present the conditional ordinal HGLM results for self-reported health and psychological distress, respectively. Relevant to the study research questions, model 1 shows that only one of the dyad-level variables interracial couple – was significantly associated with both self-reported health and psychological distress. More specifically, compared to those in monoracial Black relationships, the odd of reporting better health were roughly 49% lower (e^b = .508, p < .01) for partners in interracial (Black/non-Black) couples. Likewise, the expected number of symptoms of psychological distress for interracial couples was about 1.59 times that of their monoracial counterparts. These findings support hypothesis 1. Importantly, the strength of these associations was not attenuated in the later models that take into consideration relational hostility, warmth, and satisfaction. As expected, there were no significant differences in levels of health for those in cohabiting and marital unions versus those in dating unions.
Table 2.
Ordered Logit Actor-Partner Independence Model Predicting Self-reported Health
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| e^b | e^b | e^b | e^b | e^b | |
| Dyad-level predictors | |||||
| Child | 1.138 | 1.256 | 1.344 | 1.428 | 1.528 † |
| Relationship Length | 1.076 | 1.058 | 1.062 | 1.057 | 1.055 |
| Cohabiting | .884 | .878 | .866 | .883 | .845 |
| Married | 1.129 | 1.131 | 1.099 | 1.102 | .971 |
| Interracial Couple | .508 ** | .526** | .550 ** | .527 ** | .509 ** |
| Actor Predictors | |||||
| Female | .520 ** | .513 ** | .521 ** | .499 ** | .483 ** |
| Age | .990 | .984 | .986 | .985 | .982 |
| Education | 1.132 * | 1.089 | 1.091 * | 1.132 † | 1.120 † |
| In school | .936 | .944 | .966 | .943 | .990 |
| Employed | .931 | .914 | .928 | .906 | .896 |
| No health insurance | .663 * | .685 * | .680* | .627 * | .618 * |
| BMI | .924 *** | .921 *** | .923 *** | .915 *** | .912 *** |
| Frequency of exercise | 1.115 | 1.099 | 1.093 | 1.108 | 1.122 |
| Hostility | .875 * | .900 | .811 * | .869 † | |
| x Cohabiting | 1.251 | 1.186 | |||
| x Married | 2.038 * | 2.025 * | |||
| Warmth | 1.067 | .979 | .958 | ||
| x Cohabiting | 1.213 | 1.328 | |||
| x Married | 1.836 * | 1.734 † | |||
| Satisfaction | 1.357*** | ||||
| x Cohabiting | .843 | ||||
| x Married | .788 | ||||
| Partner Predictors | |||||
| Age | .995 | .988 | .989 | .979 | .985 |
| Education | 1.151 * | 1.126 † | 1.132 | 1.104 | 1.129 † |
| In school | 1.250 | 1.259 | 1.270 | 1.278 | 1.263 |
| Employed | .897 | .885 | .902 | .897 | .867 |
| No health insurance | 1.106 | 1.130 | 1.118 | 1.106 | 1.070 |
| BMI | .990 | .987 | .987 | .991 | .992 |
| Frequency of exercise | .997 | .985 | .978 | .983 | .961 |
| Hostility | .851 * | .881 † | .973 | .969 | |
| x Cohabiting | .756 † | .744† | |||
| x Married | .507 * | .534* | |||
| Warmth | 1.068 | 1.099 | .998 | ||
| x Cohabiting | 1.099 | 1.154 | |||
| x Married | .762 | .843 | |||
| Satisfaction | .956 | ||||
| x Cohabiting | .920 | ||||
| x Married | 1.242 | ||||
| Intercept | .224 | .207 | .200 | .189 | .183 |
p≤.10,
p≤.05,
p≤.01,
p≤.001 (two-tailed)
N = 249 different-sex dyads: All continuous variables centered at their grand mean.
Table 3.
Negative Binomial Actor-Partner Independence Model Predicting Psychological Distress
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| e^b | e^b | e^b | e^b | e^b | |
| Dyad-level predictors | |||||
| Child | .902 | .818 | .810 | .799 † | .777 † |
| Relationship Length | .937 † | .952 | .954 | .954 | .960 |
| Cohabiting | .869 | .864 | .857 | .848 | .858 |
| Married | .805 | .762 | .761 | .640 † | .800 |
| Interracial Couple | 1.592 *** | 1.605 *** | 1.594 *** | 1.563 *** | 1.552 *** |
| Actor Predictors | |||||
| Female | 1.351 * | 1.255 | 1.218 | 1.210 | 1.204 |
| Age | 1.032 * | 1.035 * | 1.034 * | 1.036 * | 1.031 † |
| Education | .907 ** | .922 * | .918 * | .916 * | .922 * |
| In school | 1.094 | 1.057 | 1.066 | 1.057 | 1.045 |
| Employed | .987 | .990 | 1.005 | 1.019 | 1.018 |
| No health insurance | 1.169 | 1.156 | 1.141 | 1.165 | 1.146 |
| BMI | 1.000 | 1.001 | 1.000 | .999 | 1.001 |
| Frequency of exercise | .986 | 1.001 | .998 | .986 | .993 |
| Hostility | 1.152 *** | 1.168 *** | 1.164 *** | 1.149 *** | |
| x Cohabiting | 1.008 | ||||
| x Married | 1.117 | ||||
| Warmth | 1.092 † | 1.103 † | 1.104 * | ||
| x Cohabiting | .884 | ||||
| x Married | 1.291 | ||||
| Satisfaction | .931 * | ||||
| Partner Predictors | |||||
| Age | 1.008 | 1.014 | 1.014 | 1.017 | 1.012 |
| Education | 1.007 | 1.035 | 1.039 | 1.043 | 1.038 |
| In school | 1.159 | 1.177 | 1.165 | 1.181 | 1.153 |
| Employed | .962 | .957 | .954 | .987 | .958 |
| No health insurance | 1.145 | 1.119 | 1.123 | 1.181 | 1.132 |
| BMI | 1.005 | 1.010 | 1.011 | 1.012 | 1.011 |
| Frequency of exercise | .925 † | .940 | .940 | .927 | .936 |
| Hostility | 1.044 | 1.026 | 1.007 | 1.018 | |
| x Cohabiting | 1026 | ||||
| x Married | 1.024 | ||||
| Warmth | .906* | .909 † | .935 | ||
| x Cohabiting | 1.067 | ||||
| x Married | .754 | ||||
| Satisfaction | .980 | ||||
| Intercept | 1.142 | 1.248 | 1.266 | 1.211 | 1.291 |
p≤.10.
p≤.05.
p≤.01.
p≤.001 (two-tailed)
N = 249 different-sex dyads: All continuous variables centered at their grand mean.
Model 2 of each table considers the association between both actor and partner hostility and health. Although actor hostility was significantly associated with both self-reported health (e^b = .875, p < .05) and psychological distress (e^b = 1.152, p <.001), partner hostility was significant only in predicting self-reported health (e^b = .851, p <.05). These results provide partial support for hypothesis 2. Holding all else constant in the model, including actor hostility, a 1-unit increase in partner hostility was associated with roughly a 15% decrease in the odds of reporting “excellent” health. Gender x hostility interaction terms (not shown) revealed that neither the actor nor partner effect for hostility varied significantly by gender.
Model 3 of each table considers the associations between actor and partner warmth and health. Surprisingly, actor warmth was marginally significant in predicting greater psychological distress (e^b = 1.09, p < .10) and was positively but not significantly associated with better self-reported health (e^b = 1.067, p > .10). Consistent with hypothesis 2, partner warmth was significantly predictive of psychological distress (e^b = .906, p <.05), such that a 1-unit increase in partner warmth predicted a 10% decrease in the expected count of depressive symptoms. As with hostility, the gender x warmth interaction terms (not shown) revealed that neither the actor nor partner effect for warmth varied by gender. These findings support hypothesis 2 but indicate that partner support and strain are differentially linked to physical and mental health.
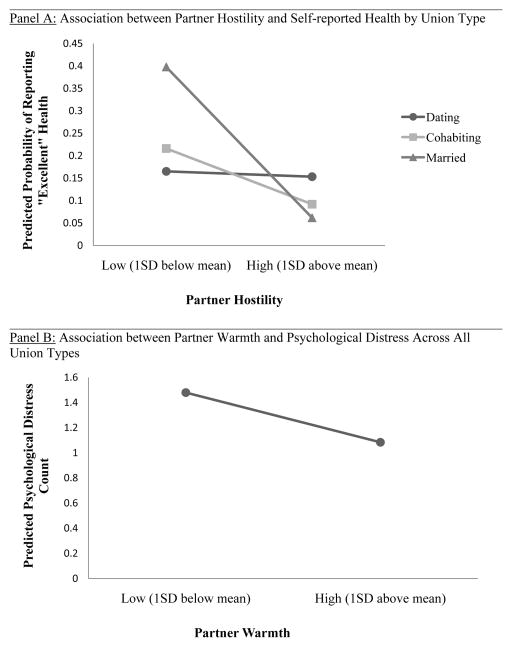
Model 4 in each table tests hypothesis 3 by introducing the cross-level interactions between relationship support and stress and union type. For self-reported health, the association between partner hostility and health was indeed conditioned by union type. As predicted, the negative association between partner hostility and self-reported health was exacerbated for married and cohabiting couples versus their dating counterparts. This cross-level interaction can be seen in Panel A of Figure 1. Post-hoc tests revealed that the slope for partner hostility did not significantly differ between cohabiting and married couples. Interestingly, although not hypothesized, actor effects predicting self-reported health also varied by union type. For instance, the negative association between actor hostility and self-reported health was diminished among married couples relative to their dating counterparts. For psychological distress, however, hypothesis 3 was not supported in that neither actor nor partner effects of warmth or hostility significantly differed by union type. Hence, the direct association between partner warmth and psychological distress found in model 3 of Table 3 is graphed in Panel B of Figure 1.
Figure 1.
Associations between Partner Support/Strain and Health
Notes: Associations in Panel A graphed from Model 4 of Table 2; Associations in Panel B graphed from Model 3 of Table 3.
Model 5 of each table tests our final hypothesis regarding the role that relationship satisfaction might play in predicting health. As expected, actor satisfaction was significantly associated with both self-reported health (e^b = 1.357, p < .001) and psychological distress (e^b = .931, p < .05).2 A 1-unit increase in relationship satisfaction predicted a 36% increase in the odds of reporting “excellent” health and roughly a 7% decline in the expected count of depressive symptoms. These associations were similar across union type and did not vary by gender (gender interactions and cross-level interactions for psychological distress not shown). Further, consistent with hypothesis 4, adding relationship satisfaction to the model attenuated the association between partner warmth and psychological distress to nonsignificance. Although the cross-sectional data utilized here make it difficult to establish causal priority, post-hoc mediation tests revealed that relationship satisfaction mediated roughly 28% of the partner warmth association with psychological distress (Kenny, Korchmaros, & Bolger, 2003).
DISCUSSION
Much of the research on relationships and health to date has focused on understanding how and why marriage, particularly a high-quality marriage, impacts health. In the present study, we expanded this line of inquiry using dyadic data to explore how both the couple-level context and individual strains and stressors within romantic relationships were associated with young adults’ mental and physical health. We also considered the potential interplay between these two levels of analysis by assessing the degree to which relationship strain/support were differentially associated with health across different union types. In doing so, we found couple-level context, individual-level experiences, and their interaction to be important predictors of health.
As hypothesized, we found that interracial couples reported worse health than their monoracial Black counterparts. Given generally poorer health among Black individuals, this couple-level effect indicating that Black/Black couples actually report better health than Black/non-Black couples highlights the importance of couple-level racial context and is consistent with mounting evidence suggesting that partners in interracial relationships, particularly with a Black partner, face unique stressors that ultimately prove detrimental to health. Importantly, these stressors seem to be external to the romantic relationship, as the negative association of interracial pairing with health was not mitigated by a consideration of relationship hostility, warmth, and satisfaction. Given that all of our interracial couples were Black/non-Black pairings and all of our monoracial couples were Black/Black pairings, however, future research must continue to explore these issues with more complexity.
Unlike the hypothesized interracial pairing effect, we found that union type had no direct association with health. This null finding is consistent with a growing literature suggesting the blurring of lines between cohabitation and marriage, particularly for Blacks. Not only did cohabiters and married relationships not differ from one another in either the average health status of their members or several relationship quality indicators, but they also did not differ from their dating counterparts. This may be attributable to the relatively young age of our couples, as recent research has shown that the “marriage benefit” is less applicable to those who marry when it is nonnormative in the life course (Uecker, 2012). It may also be due, however, to the fact that the dating couples in the FACHS sample tended to be in relatively long-term relationships (an average of 3.12 years) and hence approximated the characteristics of cohabiting and married couples, with the exception of coresidence.
The lack of direct union type effects does not mean that union type did not matter at all, however, as it helped to condition the effect of partner hostility on self-reported health. That is, partner hostility was more strongly associated with reduced health among both married and cohabiting respondents, relative to their dating counterparts. These findings support the continued insistence among scholars that it is difficult to understand health benefits of romantic relationships without understanding the internal characteristics of such relationships. Both married and cohabiting partners reported better health than their dating counterparts when partner hostility was low but reported worse health than their dating counterparts when partner hostility was high (see Panel B of Figure 1). It appears, then, that the negative health implications of having a hostile partner may be exacerbated when that partner is a marital or cohabiting partner versus a dating partner. This was not the case for partner warmth, however, as it proved equally beneficial for health, particularly mental health, across union types.
In no case did partner effects differ significantly between those in married and cohabiting unions. Such findings are consistent with the notion that, although seemingly not necessary for partner interdependence, a shared living environment may help to enhance this interdependence. Scanzoni and colleagues (1989) predicted such findings over two decades ago when they stated that “residence/degree of physical proximity is actually becoming more significant than is legal [marital] status in terms of understanding and intervening in close relationships” (p. 121). Further exploration into this possibility will allow for a better understanding of the processes through which romantic relationships affect health and will also allow for a more complex understanding of what enhances or diminishes interdependence between romantic partners.
Importantly, in the current sample, relationship satisfaction was similarly associated with both mental and physical health across union types and mediated the effect of partner warmth on psychological distress. The association between partner hostility and self-reported health, however, maintained significance even when controlling for relationship satisfaction. Such findings point to the necessity of examining both multiple indicators of relationship quality and multiple indicators of health. Doing so will allow for a more nuanced understanding of the extent to which the relationship factors and processes predicting mental and physical health differ.
This study’s findings should be interpreted in light of several limitations. Most importantly, the present sample included primarily African American couples and was limited in regional variation. Future work should consider these associations with more generalizable samples. Second, the FACHS data lack measures of family and economic background for romantic partners and, hence, this study was unable to control for factors like parents’ marital history or socioeconomic status. It is possible that such family background characteristics serve as “fundamental causes” (Phelan, Link, & Tehranifar, 2010) of disadvantage across the life course, making the association between relationship quality and health spurious. Our inclusion of respondents’ own educational attainment, work status, and access to health insurance as controls, however, makes the possibility of complete spuriousness less likely. Third, although self-reported health has proven to be a good indicator of inflammation and a robust predictor of mortality, biomarker data could provide more direct, objective, and multidimensional assessments of physical health. Fourth, recent research has pointed out that the benefits of received support from a partner depend on the extent to which that support is responsive to the recipient’s needs (e.g. Maisel & Gable, 2009). The current study could not assess this dimension of support, but doing so in future work may help refine the associations found here. Fifth, our cross-sectional data could not parse out true causal effects, and the associations found here should be further examined with longitudinal data. Finally, given that measures of health and relationship characteristics were all self-reported by relational partners, future work might reduce same-reporter bias in the associations found here by using third-party observations reports.
Despite these limitations, the current study was one of the few that contains dyadic data from relational partners across dating, cohabiting, and married relationships as well as extensive measures of the character of such relationships, allowing us to test new hypotheses that have both theoretical and practical implications. The current work suggests that individual differences in both self-reported health and psychological distress are evident amongst young people and are affected by relational experiences during the transition to adulthood, long before many chronic diseases become diagnosable. Hence, national attention and resources oriented toward promoting marriage (Heath, 2012), might be better oriented toward enabling high quality intimate relationships, in general; for it is clear that the character of relationships outside of and/or prior to marriage are important for both mental and physical health. Given the many barriers to high quality marriages among African Americans (Chambers & Kravitz, 2011), calling attention to and building upon the strengths of romantic relationships, no matter their form, may be particularly important for this group of young people.
Footnotes
Consistent with past work, by the later waves of the FACHS, there were some differences between the now-young adult respondents initially drawn from Iowa and Georgia. For example, those drawn from Iowa were significantly more likely to be involved in interracial or cohabiting relationships as young adults, and their relationships were marked by lower satisfaction and less partner warmth than those initially drawn from Georgia. Region of recruitment, however, was unrelated to the health outcomes in all of the models presented here. Further, the inclusion of this control did not affect the size, significance, or substance of the current findings.
For self-reported health, actor and partner satisfaction, along with their cross-level interactions with union type, were entered into the model given the significant variation in the effect of partner hostility by union type.
Contributor Information
Ashley B. Barr, Email: abbarr@buffalo.edu, 430 Park Hall, University at Buffalo, SUNY, Department of Sociology, Buffalo, NY 14260, Phone: (814) 876-0426, Fax: (716) 645-3934
Ronald L. Simons, Email: rlsimons@uga.edu, Distinguished Research Professor, 324 Baldwin Hall, University of Georgia, Department of Sociology, Athens, GA 30602, Phone: (706) 424-2626, Fax: (706) 542-4320
References
- Bratter JL, Eschbach K. ‘What about the couple?’: Interracial marriage and psychological distress. Social Science Research. 2006;35:1025–1047. doi: 10.1016/j.ssresearch.2005.09.001. [DOI] [Google Scholar]
- Bratter JL, King RB. “But will it last?”: Marital instability among interracial and same-race couples. Family Relations. 2008;57:160–171. doi: 10.1111/j.1741-3729.2008.00491.x. [DOI] [Google Scholar]
- Bumpass L, Lu HH. Trends in cohabitation and implications for children’s family contexts in the United States. Population Studies: A Journal of Demography. 2000;54:29–41. doi: 10.1080/713779060. [DOI] [PubMed] [Google Scholar]
- Burman B, Margolin G. Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin. 1992;112:39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Burton LM, Bonilla-Silva E, Ray V, Buckelew R, Freeman EH. Critical race theories, colorism, and the decade’s research on families of color. Journal of Marriage and Family. 2010;72:440–459. doi: 10.1111/j.1741-3737.2010.00712.x. [DOI] [Google Scholar]
- Carr D, Springer KW. Advances in families and health research in the 21st century. Journal of Marriage and Family. 2010;72:743–761. doi: 10.1111/j.1741-3737.2010.00728.x. [DOI] [Google Scholar]
- Chambers AL, Kravitz A. Understanding the disproportionately low marriage rate among African Americans: An amalgam of sociological and psychological constraints. Family Relations. 2011;60:648–660. doi: 10.1111/j.1741-3729.2011.00673.x. [DOI] [Google Scholar]
- Cherlin AJ. Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and Family. 2010;72:403–419. doi: 10.1111/j.1741-3737.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chito Childs E. Navigating interracial borders: Black-white couples and their social worlds. Piscataway, NJ: Rutgers University Press; 2005. [Google Scholar]
- Christian LM, Glaser R, Porter K, Malarkey WB, Beversdorf D, Kiecolt-Glaser JK. Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology. 2011;36:1495–1504. doi: 10.1016/j.psyneuen.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donoho CJ, Crimmins EM, Seeman TE. Marital quality, gender, and markers of inflammation in the midus cohort. Journal of Marriage and Family. 2013;75:127–141. doi: 10.1111/j.1741-3737.2012.01023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drefahl S. Do the married really live longer? The role of cohabitation and socioeconomic status. Journal of Marriage and Family. 2012;74:462–475. doi: 10.1111/j.1741-3737.2012.00968.x. [DOI] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/ajph.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath M. One marriage under god: The campaign to promote marriage in America. New York: New York University Press; 2012. [Google Scholar]
- Holt-Lunstad J, Birmingham W, Jones BQ. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Annals of Behavioral Medicine. 2008;35:239–244. doi: 10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosomatic Medicine. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Kamp Dush CM, Amato PR. Consequences of relationship status and quality for subjective well-being. Journal of Social and Personal Relationships. 2005;22:607–627. doi: 10.1177/0265407505056438. [DOI] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychological Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neuroscience and Biobehavioral Reviews. 2010;35:33–38. doi: 10.1016/j.neubiorev.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreider RM, Ellis R. Current Population Reports. Washington, DC: United States Census Bureau; 2011. Number, timing, and duration of marriages and divorces: 2009; pp. 70–125. [Google Scholar]
- Kroeger RA, Williams K. Consequences of black exceptionalism? Interracial unions with blacks, depressive symptoms, and relationship satisfaction. The Sociological Quarterly. 2011;52:400–420. doi: 10.1111/j.1533-8525.2011.01212.x. [DOI] [PubMed] [Google Scholar]
- Lee KS, Ono H. Marriage, cohabitation, and happiness: A cross-national analysis of 27 countries. Journal of Marriage and Family. 2012;74:953–972. doi: 10.1111/j.1741-3737.2012.01001.x. [DOI] [Google Scholar]
- Liu H, Reczek C. Cohabitation and U.S. adult mortality: An examination by gender and race. Journal of Marriage and Family. 2012;74:794–811. doi: 10.1111/j.1741-3737.2012.00983.x. [DOI] [Google Scholar]
- Liu H, Umberson D. The times they are a changin’: Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior. 2008;49:239–253. doi: 10.1177/002214650804900301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisel NC, Gable SL. The paradox of received social support: The importance of responsiveness. Psychological Science. 2009;20:928–932. doi: 10.1111/j.1467-9280.2009.02388.x. [DOI] [PubMed] [Google Scholar]
- Mastekaasa A. Marital status, distress, and well-being: An international comparison. Journal of Comparative Family Studies. 1994;25:183–205. [Google Scholar]
- Musick K, Bumpass L. Reexamining the case for marriage: Union formation and changes in well-being. Journal of Marriage and Family. 2012;74:1–18. doi: 10.1111/j.1741-3737.2011.00873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onwuachi-Willig A, Willig-Onwuachi J. A house divided: The invisibility of the multiracial family. Harvard Civil Rights-Civil Liberties Law Review. 2009;44:231–253. [Google Scholar]
- Payne KK. Family Profiles (FP-12-07) National Center for Family and Marriage Research; 2012. Median age at first marriage, 2010. [Google Scholar]
- Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51:S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Rendall M, Weden M, Favreault M, Waldron H. The protective effect of marriage for survival: A review and update. Demography. 2011;48:481–506. doi: 10.1007/s13524-011-0032-5. [DOI] [PubMed] [Google Scholar]
- Robles TF, Kiecolt-Glaser JK. The physiology of marriage: Pathways to health. Physiology & Behavior. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Saxbe D, Repetti RL. For better or worse? Coregulation of couples’ cortisol levels and mood states. Journal of Personality and Social Psychology. 2010;98:92–103. doi: 10.1037/a0016959. [DOI] [PubMed] [Google Scholar]
- Scanzoni J, Polonko K, Teachman J, Thompson L. The sexual bond: Rethinking families and close relationships. Los Angeles: Sage; 1989. [Google Scholar]
- Schoenborn CA. Advance Data from Vital and Health Statistics; no 351. Hyattsville, Maryland: National Center for Health Statistics; 2004. Marital status and health: United states,1999–2002. [PubMed] [Google Scholar]
- Simon RW. Revisiting the relationships among gender, marital status, and mental health. American Journal of Sociology. 2002;107:1065–1096. doi: 10.1086/339225. [DOI] [PubMed] [Google Scholar]
- Simon RW, Barrett AE. Nonmarital romantic relationships and mental health in early adulthood: Does the association differ for men and women? Journal of Health and Social Behavior. 2010;51:168–182. doi: 10.1177/0022146510372343. [DOI] [PubMed] [Google Scholar]
- South SC, Krueger RF. Marital satisfaction and physical health: Evidence for an orchid effect. Psychological Science. 2013 doi: 10.1177/0956797612453116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Surjadi FF, Lorenz FO, Wickrama KAS, Conger RD. Parental support, partner support, and the trajectories of mastery from adolescence to early adulthood. Journal of Adolescence. 2011;34:619–628. doi: 10.1016/j.adolescence.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troy AB, Lewis-Smith J, Laurenceau JP. Interracial and intraracial romantic relationships: The search for differences in satisfaction, conflict, and attachment style. Journal of Social & Personal Relationships. 2006;23:65–80. doi: 10.1177/0265407506060178. [DOI] [Google Scholar]
- Uecker JE. Marriage and mental health among young adults. Journal of Health and Social Behavior. 2012;53:67–83. doi: 10.1177/0022146511419206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers D, Liu H, Needham B. You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA, Kaiser R. Marriage and relationship issues. In: Dozois KSDDJA, editor. Risk Factors in Depression. San Diego: Academic Press; 2008. pp. 363–384. [Google Scholar]
- Whisman MA, Sbarra DA. Marital adjustment and interleukin-6 (IL-6) Journal of Family Psychology. 2012;26:290–295. doi: 10.1037/a0026902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker L, Settles T. Marital distress and the metabolic syndrome: Linking social functioning with physical health. Journal of Family Psychology. 2010;24:367–370. doi: 10.1037/a0019547. [DOI] [PubMed] [Google Scholar]
- Whitton SW, Whisman MA. Relationship satisfaction instability and depression. Journal of Family Psychology. 2010;24:791–794. doi: 10.1037/a0021734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR. Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior. 2012;53:279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]