Abstract
Since typical inflammatory responses may be diminished in children following bone marrow transplant (BMT), computed tomography (CT) imaging of the sinuses has been increasingly ordered to diagnose sinusitis in this group. The objective of this study was to determine the association between clinical sinusitis symptoms and sinus opacification on CT scans in post BMT versus immunocompetent children. Our sample was comprised of 64 post BMT and 86 immunocompetent children with sinus CT scans. CT sinus opacification was scored using the modified Lund–Mackay staging system. The relationship between clinical sinusitis symptoms (rhinorrhea, nasal congestion, cough, headache, and facial pain) and opacification was compared for the two groups. The severity of sinus opacification in the BMT group was significantly higher compared to the immunocompetent group. In combined patient groups the odds ratio (OR) for moderate/severe sinusitis was significantly elevated for rhinorrhea (OR=3.00; 95% confidence interval [CI], 1.27–7.12), cough (OR=2.80; 95% CI, 1.22–6.42), and having either rhinorrhea, nasal congestion, or cough (OR= 4.76; 95% CI, 1.71–13.24). While the immunocompetent group had a greater number of sinusitis symptoms compared to the post BMT group, both groups had a significant increase in the severity on CT with increasing number of symptoms.
Conclusion
In post BMT patients, our data demonstrated higher odds of moderate/severe sinusitis on CT scans associated with rhinorrhea, cough or nasal congestion. These finding suggest that in post BMT children, detailed sinus history may still play a vital role in the diagnosis of sinusitis.
Keywords: Sinusitis, Children, Bone marrow transplant, Computed tomography, Paranasal sinuses, Symptoms
Introduction
Sinusitis is one of the most common infectious diseases encountered in the pediatric population. Children have an average of six to eight viral upper respiratory tract infections per year [15] and 5–13% of these are complicated by the development of acute bacterial sinusitis [7]. Post bone marrow transplant (BMT) pediatric patients are particularly vulnerable to acute sinusitis because of immunosuppression due to marrow aplasia [2]. Two-thirds of BMT patients have been reported to develop sinusitis within the first 120 days of receiving bone marrow allograft [11].
Symptoms of sinusitis include cough, rhinorrhea, nasal congestion, facial pressure, and headache [7, 15]. While these clinical symptoms are usually sufficient for diagnosis of sinusitis in immunocompetent patients, it is believed that fever might be the only presenting sign in patients who are immunosuppressed, because the typical inflammatory response may be diminished [1]. As a result, computed tomography (CT) imaging of the sinuses has been increasingly ordered to diagnose sinusitis in this vulnerable population. A comparison of CT imaging and clinical evaluation in diagnosing sinusitis in children is particularly important in light of the risks of cumulative diagnostic radiation exposure at a time of rapid body development and organ growth [4].
The primary aim of this study is to investigate the relationship between clinically obtained sinusitis symptoms and severity of sinus opacification on CT scans in post BMT and immunocompetent children. To our knowledge, no previous studies have examined this relationship in pediatric post BMT patients.
Materials and methods
Design
A computer-assisted search was performed to identify all post BMT and immunocompetent patients younger than 21 years who underwent sinus CT scans between January 2002 and January 2007 at our institution. Demographic characteristics and clinical symptoms were collected from electronic patient records and sinus CT scans were evaluated from the Picture Archiving and Communications System. Post BMT patients with missing CT images (n=5) or patients having more than one BMT (n=5) were excluded from the study sample. Immunocompetent children included those who had recurrent, chronic or persistent sinusitis symptoms, total white blood cell count over 1,500, absolute neutrophil count over 500, and no history of allergy. Immunocompetent patients were excluded if the indication for the sinus CT was not related to sinusitis (n=18), if sinus anatomy was distorted due to prior sinus surgery (n=11), or if CT images were missing (n=1). Institutional review board approval was obtained for this HIPPA-compliant study.
Sinus CT scans
Sinus CT scans were evaluated by an experienced neuroradiologist (I.I.) and a research fellow trained to perform the CT severity scoring (S.A.). Contiguous CT scans in the axial or coronal plane using 3-mm-thick sections were obtained from 2002 to 2004 without routine production of multiplanar reconstructions. Following 2004, helical CT scans of the paranasal sinuses and two-dimensional thin section coronal and axial reconstructions in bone and soft tissue algorithms were available for review from 1 mm thick raw data in the axial plane.
Sinus CT scoring
All CT examinations were retrospectively scored using the modified Lund and Mackay criteria to establish the severity of sinusitis [9]. The Lund–Mackay system quantifies radiographic findings on the sinus CT scan with a numerical score. The ten sinuses evaluated in each patient included the frontal, maxillary, sphenoid, anterior ethmoid and posterior ethmoid sinuses for both the right and left sides. Degree of opacification of the sinuses, patency of the osteomeatal complex, and number of developed sinuses were documented for each patient. For each sinus, a score of 0 to 3 was applied, with “0” for no opacification, “1” for 1–49% opacification, “2” for 50–99% opacification, and “3” for total opacification. Undeveloped sinuses were given no score. Each osteomeatal complex was given a score of either 0 or 2 for patent and occluded, respectively. Severity score was calculated by first adding up the scores from all developed sinuses (0–30) and osteomeatal complexes (0–4) so that the total score ranged from 0 to 34. Since number of developed sinuses varies in the growing body, we standardized the score by dividing the total score obtained in each patient by the total number of developed sinuses. Based on this percentage, the severity of sinusitis on CT was categorized into four groups: 0% for no evidence of sinusitis, 1–25% for mild sinusitis, 26–50% for moderate sinusitis and 51–100% for severe sinusitis. The severity of sinus opacification on CT was compared between the post BMT patient group and the immunocompetent group.
To validate the scoring, inter- and intraobserver reliability was measured using Pearson’s correlation coefficients. The interobserver correlation of sinus CT severity scores measured by the two scorers was 0.91 (p<0.001), and the intraobserver correlation on repeated measurements by scorer I was 0.92 (p<0.001).
Sinusitis symptoms
The distribution of sinusitis symptoms was determined in patients across severity categories and compared between the post BMT and immunocompetent groups. The odds of each sinusitis symptom, in addition to fever, were compared for patients with no/mild sinusitis to those with moderate/severe sinusitis in both groups. In addition, a clinical symptom score ranging from 0 to 5 was calculated by adding the total number of symptoms present for each patient: rhinorrhea, nasal congestion, cough, headache, and facial pain. The change in sinus severity score corresponding to a unit increase in the number of clinical symptoms was determined for both the post BMT and immunocompetent groups.
Analysis
Differences between the frequencies of sinus symptoms in post BMT and immunocompetent groups after adjusting for age was determined using logistic regression. Differences of severity on CT between the post BMT group and the immunocompetent group after adjusting for age were determined using linear regression. Logistic regression was used to determine the odds ratio of moderate/severe sinusitis versus no/mild sinusitis and clinical symptoms after adjusting for age. Linear regression analysis was also used to determine the association between severity on CT and total number of symptoms. We considered also adjusting for sex in regression models, but this variable did not affect results so it was not included in the final models. A value of p<0.05 was considered statistically significant. All statistical computations were performed using the STATA software Version 11.0 (STATA Corporation, College Station, TX).
Results
Characteristics of study sample
The post BMT study sample consisted of 64 patients, 41 (64%) males and 23 (36%) females. Nineteen (30%) patients underwent allogenic HLA-matched related BMTs, 18 (28%) HLA-matched unrelated donor BMTs, 12 (19%) autologous transplants, ten (16%) allogenic cord blood transplants and five (8%) allogeneic haploidentical BMTs. The age range of post BMT patients at the time of BMT was 6 months to 20 years with a median of age of 10.1 years (interquartile range, 4.0–14.8). Sinus CT scans were performed at an average of 6 weeks post BMT. The immunocompetent group consisted of 86 patients, 43 (50%) males and 43 (50%) females. The age range of the immunocompetent group was 5 months to 21 years with a median age of 12.0 years (interquartile range, 6.9–17.8).
The indications for sinus CT scans in both BMT group and the immunocompetent group are shown in Table 1. The majority of post BMT patients (49/64, 77%) underwent sinus CT scans due to persistent fever of unknown etiology with or without sinus specific symptoms. The majority of the patients in the immunocompetent group underwent sinus CT scans due to chronic or recurrent sinusitis symptoms (62/86, 72%).
Table 1.
Frequency of indications for sinus CT scans in bone marrow transplant and immunocompetent patients
| n | Percent | |
|---|---|---|
| Post BMT patients (n=64) | ||
| Acute fever onlya | 35 | 55% |
| Acute sinus symptoms and fever | 14 | 22% |
| Acute sinus symptoms only | 9 | 14% |
| Other | 6 | 9% |
| Immunocompetent patients (n=86) | ||
| Acute fever | 3 | 3% |
| Chronic or recurrent sinus specific symptomsb | 62 | 72% |
| Recurrent headache | 7 | 8% |
| Obstructive sleep apnea | 4 | 5% |
| Epistaxis | 4 | 5% |
| Other | 9 | 10% |
BMT bone marrow transplant
Acute is defined as symptoms lasting less than 4 weeks
Chronic is defined as symptoms lasting longer than 8 weeks
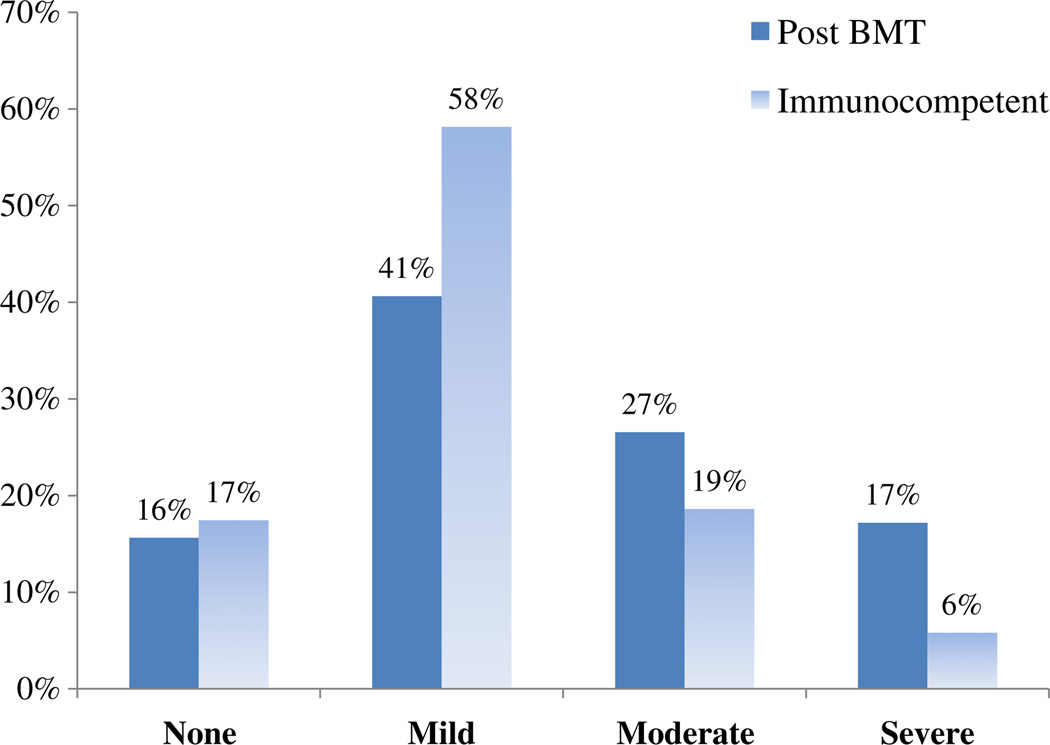
Sinus CT severity
The distribution of severity on CT within the post BMT patient group and the immunocompetent group is shown in Fig. 1. Among the post BMT patients, ten (16%) BMT patients had no, 26 (41%) patients had mild, 17 (27%) had moderate and 11 (17%) had severe sinus opacification. Among the immunocompetent group 15 (17%) had no, 50 (58%) had mild, 16 (19%) had moderate and five (6%) had severe opacification. Severity of sinus opacification in the post BMT group (severity score=1.45, SD=0.96) was higher than that in the immunocompetent group (severity score=1.13, SD=0.76), but this increase did not reach statistical significance (p=0.08) (Table 2).
Fig. 1.
Distribution of sinus CT severity in post BMT and immunocompetent patients
Table 2.
Clinical sinusitis symptoms in post bone marrow transplant and immunocompetent patients
| Post BMT | Immunocompetent | P value | |||
|---|---|---|---|---|---|
| n | Percent | n | Percent | ||
| All patients | 64 | 86 | |||
| Rhinorrhea | 13 | 20% | 41 | 48% | <0.01 |
| Cough | 16 | 25% | 26 | 30% | 0.25 |
| Nasal congestion | 7 | 11% | 45 | 52% | <0.01 |
| Headache | 2 | 3% | 23 | 27% | <0.01 |
| Facial pain | 2 | 3% | 13 | 15% | 0.06 |
| Fever | 44 | 69% | 3 | 3% | <0.01 |
| Symptom score,a mean (SD) | 0.63 | 0.92 | 1.72 | 1.05 | <0.01 |
| Severity score,b mean (SD) | 1.45 | 0.96 | 1.13 | 0.76 | 0.08 |
| None | 10 | 15 | |||
| Rhinorrhea | 0 | 0% | 5 | 33% | – |
| Cough | 0 | 0% | 3 | 20% | – |
| Nasal congestion | 0 | 0% | 5 | 33% | – |
| Headache | 1 | 10% | 3 | 20% | 0.48 |
| Facial pain | 0 | 0% | 1 | 7% | – |
| Fever | 6 | 60% | 0 | 0% | – |
| Symptom score,a mean (SD) | 0.10 | 0.32 | 1.13 | 1.13 | 0.01 |
| Mild sinusitis | 26 | 50 | |||
| Rhinorrhea | 4 | 15% | 22 | 44% | 0.02 |
| Cough | 4 | 15% | 13 | 26% | 0.24 |
| Nasal congestion | 2 | 7% | 27 | 54% | <0.01 |
| Headache | 1 | 4% | 15 | 30% | 0.02 |
| Facial pain | 2 | 7% | 10 | 20% | 0.26 |
| Fever | 21 | 81% | 1 | 2% | <0.01 |
| Symptom score,a mean (SD) | 0.50 | 0.86 | 1.74 | 0.99 | <0.01 |
| Moderate or severe sinusitis | 28 | 21 | |||
| Rhinorrhea | 9 | 32% | 14 | 66% | 0.02 |
| Cough | 12 | 42% | 10 | 48% | 0.7 |
| Nasal congestion | 5 | 18% | 13 | 62% | <0.01 |
| Headache | 0 | 0% | 5 | 24% | – |
| Facial pain | 0 | 0% | 2 | 9% | – |
| Fever | 17 | 61% | 2 | 10% | <0.01 |
| Symptom score,a mean (SD) | 0.93 | 1.02 | 2.10 | 1.00 | <0.01 |
BMT bone marrow transplant
P value from Wald tests in logistic regression for categorical variables and linear regression for scores, after adjusting for age
Symptom score is total number of symptoms present for each patient except fever
Severity score is based on sinus opacification on CT from modified Lund–Mackay criteria
Symptoms of sinusitis
Fever was present in 77% (49/64) of patients who underwent post BMT sinus CT scans (Table 1). In the immunocompetent group only 3% (3/86) of the patients had fever. The overall frequency of sinus specific symptoms in the post BMT group and the immunocompetent group is shown in Table 2. Among all patients with mild sinusitis, there was a significant decrease in the frequency of rhinorrhea (p=0.02), nasal congestion (p< 0.01) and headache (p<0.01) in the post BMT group compared to immunocompetent group. Cough was not statistically different between the groups. Among those with moderate or severe sinusitis, there was a significant decrease in the frequency of rhinorrhea (p=0.02) and nasal congestion (p<0.01) in the BMT group compared to immunocompetent group. Cough was present in both groups with similar frequency (42% in BMT and 48% in immunocompetent patients, p=0.7). The overall symptom score was significantly smaller in post BMT patients compared to immunocompetent patients among those with none, mild, and moderate/severe sinusitis measured through CT.
Among post BMT patients, 63% (40/64) had no sinusitis symptoms. Of these, 78% (31/40) had fever. Out of the 40 BMT patients without symptoms, 18 had mild, 9 had moderate, and 4 had severe sinus opacification on CT (data not shown).
Symptoms of sinusitis and sinus CT severity
Table 3 presents odds ratios of having moderate or severe sinusitis versus mild or no sinusitis as measured by CT for established clinical symptoms and fever. In all patients, the odds ratio for moderate/severe sinusitis was significantly elevated for rhinorrhea (OR=3.00; 95% confidence interval [CI], 1.27–7.12), cough (OR, 2.80; 95% CI, 1.22–6.42), and having either rhinorrhea, nasal congestion, or cough (OR, 4.76; 95% CI, 1.71–13.24). The odds of moderate/severe sinusitis were not significantly different for patients presenting with nasal congestion, facial pain, headache, or fever. In post BMT patients, the odds of moderate/severe sinusitis were 0.46 times lower for patients presenting with fever than those without fever (OR=0.46; 95%CI, 0.13–1.57) and five times greater for patients presenting with cough than those without cough (OR=5.24; 95% CI, 1.31–20.99). Among immunocompetent patients the odds of moderate/severe sinusitis were over three times greater for patients presenting with rhinorrhea than those without this symptom (OR=3.09; 95% CI, 1.04–9.13).
Table 3.
Adjusted odds ratios of moderate/severe sinusitis compared to mild/none for clinical sinusitis symptoms
| Group | Clinical symptom | Odds ratio | 95% CI |
|---|---|---|---|
| All (n=150)a | Rhinorrhea | 3.00 | 1.27–7.12 |
| Nasal congestion | 1.93 | 0.77–4.83 | |
| Cough | 2.80 | 1.22–6.42 | |
| Headache | 1.07 | 0.33–3.47 | |
| Facial pain | 0.76 | 0.15–4.00 | |
| Fever | 0.71 | 0.24–2.06 | |
| Rhinorrhea, nasal congestion, or cough | 4.76 | 1.71–13.24 | |
| Post BMT (n=64)b | Rhinorrhea | 2.69 | 0.64–11.28 |
| Nasal congestion | 4.04 | 0.60–27.37 | |
| Cough | 5.24 | 1.31–20.99 | |
| Headache | – | ||
| Facial pain | – | ||
| Fever | 0.46 | 0.13–1.57 | |
| Rhinorrhea, nasal congestion, or cough | 4.46 | 1.29–15.36 | |
| Immunocompetent (n=86)b | Rhinorrhea | 3.09 | 1.04–9.13 |
| Nasal congestion | 1.53 | 0.54–4.35 | |
| Cough | 1.99 | 0.67–5.92 | |
| Headache | 1.29 | 0.37–4.46 | |
| Facial pain | 0.86 | 0.16–4.74 | |
| Fever | 5.10 | 0.36–72.66 | |
| Rhinorrhea, nasal congestion, or cough | 6.24 | 0.75–51.55 |
Adjusted for age and group (post BMT or immunocompetent)
Adjusted for age
Discussion
Over the past decade, CT scans have almost entirely replaced conventional radiographs for imaging the paranasal sinuses [3, 6]. According to the American College of Radiology (ACR) Appropriateness Criteria, CT is the gold standard imaging technique for guiding management of sinusitis [10]. This tool has the advantage of showing fine anatomic details, especially of the osteomeatal complexes, and has greater sensitivity in identifying mucosal thickening over plain radiographs [15]. However, mucosal thickening is a nonspecific finding and reflects inflammation which may occur following a viral upper respiratory tract infection, bacterial, viral or fungal sinusitis, or allergic reaction. Therefore mucosal thickening on imaging is not sufficient in diagnosing acute bacterial sinusitis [10]. According to the guidelines given by the American Academy of Pediatrics on management of sinusitis, CT scans of the sinuses should be reserved for children in whom surgery is being considered as a management strategy, including aspiration of the paranasal sinuses [5]. The ACR has recommended that the diagnosis of acute uncomplicated sinusitis should be made on clinical grounds alone and CT imaging should be reserved for patients who do not recover or who worsen during the course of appropriate antimicrobial therapy [10].
Acute sinusitis is one of the common infections following BMT procedures in children. When we examined the relationship between sinus opacification severity on CT scans and clinical sinusitis symptoms among BMT patients, we found the odds of moderate/severe sinus opacification was 4.46 (95% CI, 1.29–15.36) times greater for those with rhinorrhea, nasal congestion, or cough than for those without these symptoms. Among immunocompetent patients, the odds of moderate/severe sinusitis were 6.24 times greater for those with any sinusitis symptom than for those without (95% CI, 0.75–51.55). In both post BMT and immunocompetent patients a significant increase in the severity of sinusitis was noted with increasing number of symptoms.
A number of studies in the past have tried to compare the symptoms of sinusitis with the sinus CT findings. Most studies were conducted in immunocompetent adult patients and showed conflicting results regarding the association between the sinus symptoms and CT findings [8, 12–14]. A recent study suggests that symptomatic patients were much more likely to have positive CT scan findings [18]. Another study conducted in immunocompetent children found that the symptom score questionnaire (SN-5) correlated to the disease severity as measured by the Lund–Mackay CT scan score [16]. The authors concluded that the SN-5 provided clinically useful information regarding symptom severity and the effectiveness of therapeutic interventions, while decreasing the need for repeat CT scans in a population that is especially susceptible to radiation.
To our knowledge, there is no prior study in the literature that examines the association of sinusitis symptoms in pediatric patients with sinus CT scan findings after bone marrow transplantation. There is also no prior study that compares the sinusitis symptoms between age-matched immunocompromised and immunocompetent children. The few studies that have looked at the association between sinus symptoms and CT scan findings in immunocompromised patients were focused on utility of screening sinus CT scans during the pre BMT period to predict the occurrence of sinusitis in the post BMT period [2, 17]. Billings and colleagues reported that 70% of symptomatic pediatric patients in post BMT period had positive CT scan findings [2]. A study in adult immunocompromised patients found that there was a statistically significant association between symptoms of sinusitis and the presence of moderate to severe sinus disease on the pre BMT CT scans used for screening [17].
Our results suggest that immunocompetent group had a higher frequency of sinusitis symptoms (e.g., rhinorrhea, nasal congestion) compared to the post BMT group, consistent with the fact that immunosuppressed patients may not mount as much of an inflammatory response as immunocompetent patients. However, these findings may also reflect differences in questioning and documentation of sinus symptoms before ordering CT scans. Clinicians often order CT scans when high fever persists for more than several days in BMT patients, possibly before the sinusitis symptoms appear, whereas in immunocompetent children clinicians do not order CT scans unless symptoms are not responding to treatment or a complication is suspected.
Due to the retrospective collection of data for this study, it is possible that all sinus specific symptoms might not have been documented and thereby not included in the analysis. Another potential limitation is that in most cases with radiologic abnormalities, further diagnostic evaluations including sinus aspirate, biopsy or cultures were not performed. However, because these methods are invasive, potentially painful, might require sedation and not always feasible for primary care physicians or for children after bone marrow transplantation, they are not routinely used for the diagnosis of acute sinusitis. Lastly, rather than using a set of immunocompetent children with acute sinusitis as controls, this study used a group of immunocompetent children with chronic or persistent sinusitis that had already undergone CT scan. Although the immunocompetent and post BMT groups may have differed with regard to underlying disease susceptibility, it would not be ethical to expose healthy children with acute sinusitis to unnecessary radiation for research purposes. Future animal studies might address this limitation.
Conclusion
We found an association between sinusitis symptoms and opacification on CT scans in both immunocompetent and post BMT children and severity of opacification increases with increasing number of symptoms. Our findings suggest that in post BMT children, detailed sinus history may still play a vital role in the diagnosis of sinusitis. In the future, prospective multicenter studies with well documented symptom scoring might further help to weigh the potential costs and benefits of CT imaging in this vulnerable population.
Acknowledgements
We would like to thank Dr. David Yousem and Dr. Andrea Poretti for their help in the preparation of this manuscript.
Footnotes
Conflicts of interest The authors declare that they have no conflicts of interest.
Contributor Information
Sahayini Arulrajah, Neuroradiology, Department of Radiology and Radiological Science, Johns Hopkins Hospital, Baltimore, MD, USA.
Heather Symons, Sydney Kimmel Cancer Center, Department of Pediatrics and Oncology, Johns Hopkins Hospital, Baltimore, MD, USA.
Elizabeth Khaykin Cahoon, Department of Mental Health, Johns Hopkins School of Public Health, Baltimore, MD, USA.
Aylin Tekes, Pediatric Radiology, Department of Radiology and Radiological Science, Johns Hopkins Hospital, Baltimore, MD, USA.
Thierry A. G. M. Huisman, Pediatric Radiology, Department of Radiology and Radiological Science, Johns Hopkins Hospital, Baltimore, MD, USA
Izlem Izbudak, Email: iizbuda1@jhmi.edu, Neuroradiology, Department of Radiology and Radiological Science, Johns Hopkins Hospital, 600 North Wolfe Street, Phipps B-126-B, Baltimore, MD 21287-0842, USA.
References
- 1.Berlinger NT. Sinusitis in immunodeficient and immunosuppressed patients. Laryngoscope. 1985;95(1):29–33. doi: 10.1288/00005537-198501000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Billings KR, Lowe LH, Aquino VM, Biavati MJ. Screening sinus CT scans in pediatric bone marrow transplant patients. Int J Pediatr Otorhinolaryngol. 2000;52(3):253–260. doi: 10.1016/s0165-5876(00)00296-2. [DOI] [PubMed] [Google Scholar]
- 3.Branstetter BFt, Weissman JL. Role of MR and CT in the paranasal sinuses. Otolaryngol Clin North Am. 2005;38(6):1279–1299. doi: 10.1016/j.otc.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Brody AS, Frush DP, Huda W, Brent RL. Radiation risk to children from computed tomography. Pediatrics. 2007;120(3):677–682. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 5.Clinical practice guideline: management of sinusitis. Pediatrics. 2001;108(3):798–808. doi: 10.1542/peds.108.3.798. [DOI] [PubMed] [Google Scholar]
- 6.Fatterpekar GM, Delman BN, Som PM. Imaging the paranasal sinuses: where we are and where we are going. Anat Rec (Hoboken) 2008;291(11):1564–1572. doi: 10.1002/ar.20773. [DOI] [PubMed] [Google Scholar]
- 7.Friedman RA, Harris JP. Sinusitis. Annu Rev Med. 1991;42:471–489. doi: 10.1146/annurev.me.42.020191.002351. [DOI] [PubMed] [Google Scholar]
- 8.Hwang PH, Irwin SB, Griest SE, Caro JE, Nesbit GM. Radiologic correlates of symptom-based diagnostic criteria for chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2003;128(4):489–496. doi: 10.1016/S0194-59980223295-7. [DOI] [PubMed] [Google Scholar]
- 9.Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology. 1993;31(4):183–184. [PubMed] [Google Scholar]
- 10.McAlister WH, Parker BR, Kushner DC, Babcock DS, Cohen HL, Gelfand MJ, Hernandez RJ, Royal SA, Slovis TL, Smith WL, Strain JD, Strife JL, Kanda MB, Myer E, Decter RM, Moreland MS. Sinusitis in the pediatric population. American College of Radiology. ACR appropriateness criteria. Radiology. 2000;215(Suppl):811–818. [PubMed] [Google Scholar]
- 11.Savage DG, Taylor P, Blackwell J, Chen F, Szydlo RM, Rule SA, Spencer A, Apperley JF, Goldman JM. Paranasal sinusitis following allogeneic bone marrow transplant. Bone Marrow Transplant. 1997;19(1):55–59. doi: 10.1038/sj.bmt.1700601. [DOI] [PubMed] [Google Scholar]
- 12.Stankiewicz JA, Chow JM. A diagnostic dilemma for chronic rhinosinusitis: definition accuracy and validity. Am J Rhinol. 2002;16(4):199–202. [PubMed] [Google Scholar]
- 13.Stewart MG, Johnson RF. Chronic sinusitis: symptoms versus CT scan findings. Curr Opin Otolaryngol Head Neck Surg. 2004;12(1):27–29. doi: 10.1097/00020840-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Stewart MG, Sicard MW, Piccirillo JF, Diaz-Marchan PJ. Severity staging in chronic sinusitis: are CT scan findings related to patient symptoms? Am J Rhinol. 1999;13(3):161–167. doi: 10.2500/105065899781389704. [DOI] [PubMed] [Google Scholar]
- 15.Tan R, Spector S. Pediatric sinusitis. Curr Allergy Asthma Rep. 2007;7(6):421–426. doi: 10.1007/s11882-007-0064-5. [DOI] [PubMed] [Google Scholar]
- 16.Terrell AM, Ramadan HH. Correlation between SN-5 and computed tomography in children with chronic rhinosinusitis. Laryngoscope. 2009;119(7):1394–1398. doi: 10.1002/lary.20250. [DOI] [PubMed] [Google Scholar]
- 17.Thompson AM, Couch M, Zahurak ML, Johnson C, Vogelsang GB. Risk factors for post-stem cell transplant sinusitis. Bone Marrow Transplant. 2002;29(3):257–261. doi: 10.1038/sj.bmt.1703353. [DOI] [PubMed] [Google Scholar]
- 18.Wittkopf ML, Beddow PA, Russell PT, Duncavage JA, Becker SS. Revisiting the interpretation of positive sinus CT findings: a radiological and symptom-based review. Otolaryngol Head Neck Surg. 2009;140(3):306–311. doi: 10.1016/j.otohns.2008.12.007. [DOI] [PubMed] [Google Scholar]