Abstract
As is true for its predecessors, the recently published DSM-5 uses arbitrary criteria and cutoffs to define categories of mental disorders that are of questionable validity and that provide no guidance for treatment. Recently, the NIMH introduced an alternative classification system, the Research Domain Criteria (RDoC). Both the DSM-5 and the RDoC initiative make the strong assumption that psychological problems are expressions of specific latent disease entities. In contrast, the complex causal network approach conceptualizes psychological problems as mutually interacting, often reciprocally reinforcing, elements of a complex causal network. The cognitive behavioral model offers a classification framework that is compatible with the complex causal network approach and offers a treatment-relevant alternative to the latent disease model that is the basis for the DSM-5 and the RDoC initiative.
Keywords: Cognitive Behavioral Model, DSM-5, CBT, RDoC, nosology, classification, mental disorders
The recently published DSM-5 (APA, 2013) sparked a significant amount of controversy that also gathered attention by the national and international public media, such as the New York Times (Belluck & Carey, 2013) and Der Spiegel (Blech, 2013). Some of the notable critics of the DSM-5 include Alan Francis, the former chairman of the DSM-IV Task Force (Francis, 2013) and Thomas Insel, the director of the National Institute of Mental Health (e.g., Insel, Cuthbert, Carvey, Heinssen, Pine, Quinn, Sanislow, & Wang, 2010). Moreover, the publication of the DSM-5 has been criticized by numerous professional organizations, including the American Psychological Association (2012).
Aside from political and financial issues (the DSM-5 is a major source of income for the American Psychiatric Association), some of the frequently raised arguments included the following (in random order): the DSM-5 pathologizes normality using arbitrary cut-points; deriving a diagnosis is merely based on subjective judgment by a clinician, rather than objective measures, such as biological tests; the DSM-5 is overly symptom-focused and ignores the etiology of the disorder; the DSM-5 categories include a heterogeneous group of individuals and a large number of different symptom combinations can define the same diagnosis; the comorbidity problem (i.e., co- occurrence of two or more different diagnoses) remains unresolved; and most clinicians will continue to use the residual diagnosis (“not otherwise specified”) because most patients do not fall neatly into any of the diagnostic categories, which are derived by consensus agreement of experts (for a summary, see Gornall, 2013). Essentially the same concerns also apply to the 11th edition of International Classification of Diseases of the World Health Organization, which is due by 2015.
For the purpose of full disclosure, I served as an advisor to the DSM-5 Development Process (Social Anxiety Disorder, Specific Phobia, and Panic Disorder) and was a member of the DSM-5 Anxiety Disorders Sub-Work Group. In this role, I assisted with literature reviews, was a co-author of two of them, and I took part in most of the bi-weekly hour-long conference calls. During these calls, we discussed the newly proposed changes in the diagnostic definitions of specific disorders. For this discussion, the work group members followed general guidelines that were created to improve the clinical usefulness for classifying and diagnosing mental disorders based on current knowledge and predictions of where the science might be heading (Kendler, Kupfer, Narrow, Phillips, & Fawcett, 2009). The guidelines further encouraged workgroup members to revisit the entirety of the categorical system with the goal of improving the system. At the beginning of the DSM-5 revision process, four principles were laid out: (1) The DSM is a manual to be used by clinicians, and changes must be implementable in routine practices; (2) the recommendations have to be guided by empirical evidence; (3) if possible, continuity with previous editions should be maintained; and (4) there will be no a priori constraints on the degree of change between DSM-IV (APA, 1994) and DSM-5 (APA, 2013). In general, the empirical evidence for any change introduced in DSM-5 had to be proportional to the magnitude of the change. Therefore, the larger and more significant the change, the stronger the required level of empirical support had to be. The amount of evidence needed for a change further depended on the magnitude of the problem with the existing criteria or definitions. Existing diagnostic categories were considered for removal if they showed low clinical utility and if there was minimal evidence for their validity. Adding a new diagnosis or changes in diagnostic criteria were made based on literature reviews and secondary data analyses that documented the clinical validity of such changes.
The work groups consisted of well-known experts in their respective fields with different academic backgrounds (the majority being psychiatrists and doctoral-level psychologists) from all around the world. People were only able to participate in the DSM process if they had no significant conflict of interest, such as receiving significant financial compensation from the pharmaceutical industry. Despite these precautions and carefully drafted guidelines, the process resulted in much controversy, including among members of the same workgroups.
The goal of this article is not to re-hash many of the criticisms that have already been raised. Instead, my objective is to outline possible solutions to these problems. One possible solution, the RDoC initiative, has already been offered by the NIMH. Another possible solution is the adoption of the complex causal network approach. A third approach, which has not yet been discussed, is to develop a treatment-relevant classification approach that is grounded in empirical data and a solid scientific model. Cognitive-behavioral theory offers such a model. As outlined below, this approach combines features of both, the complex causal network approach and RDoC. Similar to RDoC, it encourages clinicians to expand the paradigm beyond subjective clinical judgments to include biological and behavioral data. However, the cognitive behavioral approach questions the existence of latent disease entities. This is consistent with the complex causal network approach. Before discussing these alternative classification systems, it is important to address the fundamental question: Why do we need to define and classify mental disorders?
The Need to Define and Classify Mental Disorders
Psychiatrists and psychologists alike have been engaged in a long, heated, and still ongoing battle over how to best define a mental disorder (for a review, see Varga, 2012). The contemporary official definition of a mental disorder is “a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underling mental functioning” (APA, 2013, p. 20).
This definition reflects an attempt to integrate diverse perspectives. However, the structure of the DSM is firmly rooted in a medical model, assuming that symptoms reflect underlying and latent disease entities. Whereas earlier versions of the DSM were grounded in psychoanalytic theory and assumed that mental disorders are rooted in deep-seated conflicts, modern versions implicate dysfunctions in genetic, biological, psychological, and developmental processes as the root-cause.
A highly influential and still widely accepted definition is to conceptualize a mental disorder as a harmful dysfunction (Wakefield, 1992). It is a dysfunction, because having the problem means that the person cannot perform a natural function as designed by evolution; and it is harmful because the problem has negative consequences for the person and also because the dysfunction is negatively viewed by society (see McNally, 2011, for an in-depth discussion and critique).
In contrast, Szasz (1961) argued that psychiatric disorders are simply labels attached to normal human experiences by society and are essentially arbitrary and social constructions with no clear empirical basis. The same experiences that are labeled as a disease in one culture or at one point in history may be considered normal or even desirable in another culture or at another point in history. Although culture clearly colors, and to some degree even determines psychopathology (as acknowledged by the DSM-5), the radical position that all mental disorders are merely social constructions is more a political than a scientific statement. Moreover, this criticism becomes without foundation if the question moves from “do specific diagnostic labels exist” to “do humans experience suffering than can be alleviated?”
The current view of the National Institute of Mental Health is that “mental illnesses are brain disorders. In contrast to neurological disorder with identifiable lesions, mental disorders can be addressed as disorders of brain circuits” (Insel et al., 2010, p. 749).” Therefore, NIMH has been calling for an integration of findings from modern brain sciences for defining and diagnosing mental disorders, instead of relying on subjective impressions, resulting in arbitrarily defined categories that comprise heterogeneous and overlapping diagnostic groups (Insel et al., 2010).
The cognitive-behavioral approach embraces the general diathesis-stress model, which assumes that individual vulnerability factors in conjunction with environmental stressors can lead to the development of the disorder. However, and in contrast to all other perspectives, the contemporary cognitive-behavioral perspective makes a critical distinction between initiating factors (factors that contribute to the development of a problem) and maintaining factors (factors that are responsible for the maintenance of a problem), and these factors are typically not the same. Unlike other models of mental disorders, the cognitive-behavioral perspective is much more concerned about the maintenance factors of problems and much less concerned about the initiating factors. Therefore, from a cognitive-behavioral perspective, classifying individuals based on maintenance factors is of far greater importance than based on their vulnerabilities (i.e., genetic factors or malfunctioning brain circuits), because CBT is focused on the here and now rather than past experiences. Moreover, psychological problems are targeted in line with functional analysis from the behavioral tradition.
Regardless of the specific definition, a classification system for mental disorders is necessary for at least the following reasons: First, it provides the field with a common language to reliably assess patients. This is of great practical value because it simplifies communication among practitioners, provides a coding system for third party payers. Second, science may be advanced by studying people who share similar psychopathology. It is hoped that the underlying pathology and etiology becomes apparent by studying individuals who share similar symptoms. Third, it is hoped that eventually this information can be used to optimize and tailor existing treatments or to develop new interventions. This latter issue is explicitly acknowledged by the DSM-5: “The diagnosis of mental disorders should have clinical utility: it should help clinicians to determine prognosis, treatment plans, and potential treatment outcomes for their patients” (APA, 2013; p. 20). More specifically, the DSM-5 states:
“Approaches to validating diagnostic criteria for discrete categorical mental disorders have included the following types of evidence: antecedent validators (similar genetic markers, family traits, temperament, and environmental exposures), concurrent validators (similar neural substrates, biomarkers, emotional and cognitive processing, and symptom similarity), and predictive validators (similar clinical course and treatment response)” (p. 20).
However, despite recognizing the importance of validators, the DSM-5 emphasizes clinical utility: “Until incontrovertible etiological or pathophysiological mechanisms are identified to fully validate specific disorders or disorder spectra, the most important standard for the DSM-5 disorder criteria will be their clinical utility…” (APA, 2013, p. 20). As a result, the DSM-5 offers little that is new compared to its predecessors, sparking a great degree of dissatisfaction in the medical and research community. The NIMH RDoC initiative is an attempt to move the field of psychiatry forward by creating a classification system that integrates biological and behavioral data rather than solely relying on the clinical impression and subjective symptom report.
The RDoC Initiative
The National Institute of Mental Health (NIMH) was charged to develop new ways of classifying mental disorder based on dimensions of observable behavior and neurobiological measures (NIMH, 2008). In response, NIMH began the Research Domain Criteria (RDoC) project with the goal of developing a classification system for mental disorders based on biobehavioral dimensions that cut across current heterogeneous DSM categories. More specifically, RDoC followed three guiding principles:
“First, the RDoC framework conceptualizes mental illnesses as brain disorders. In contrast to neurological disorders with identifiable lesions, mental disorders can be addressed as disorders of brain circuits. Second, RDoC classification assumes that the dysfunction in neural circuits can be identified with the tools of clinical neuroscience, including electrophysiology, functional neuroimaging, and new methods for quantifying connections in vivo. Third, the RDoC framework assumes that data from genetics and clinical neuroscience will yield biosignatures that will augment clinical symptoms and signs for clinical management. Examples where clinically relevant models of circuitry-behavior relationships augur future clinical use include fear/extinction, reward, executive function, and impulse control. For example, the practitioner of the future could supplement a clinical evaluation of what we now call an “anxiety disorder” with data from functional or structural imaging, genomic sequencing, and laboratory-based evaluations of fear conditioning and extinction to determine prognosis and appropriate treatment, analogous to what is done routinely today in many other areas of medicine” (Insel et al., 2010, p. 749).
Thus, the RDoC initiative uses different units of levels of analysis (molecular, brain circuit, behavioral and symptom level) in order to define constructs that are assumed to be the core symptoms of mental disorders.
Although it could be argued that neither clients nor practitioners will want to rely on expensive medical tests that are unlikely to inform treatment, some recent studies do, in fact, suggest that some of these methods, such as fMRI, can accurately predict treatment outcome (Doehrmann, Ghosh, Polli, Reynolds, Whitfield-Gabrieli, Hofmann, Pollack, & Gabrieli, 2013) and newer techniques, such a functional connectivity analyses, provide clinically useful data and are considerably less expensive than other techniques (Anteraper, Triantafyllou, Sawyer, Hofmann, Gabrieli, & Whitfield-Gabrieli, S. (in press). Similarly, the cost for genetic analyses is unlikely to be a barrier for their clinical use in the near future.
Whereas neuroscientists generally applauded the RDoC initiative (Casey, Craddock, Cuthbert, Hyman, Klee, & Ressler, 2013), others criticized the initiative’s over-emphasis on biological processes and its reductionist perspective equating mental disorders as brain disorders (Deacon, 2013; Miller, 2010). Moreover, determining which of the more than 20,000 protein-coding genes predispose some individuals to psychological problems is a very difficult, if not impossible, puzzle to solve. Even if we knew the identity and combinations of those genes, it would be very difficult to predict who will and will not develop a psychological problem, because genes are not the only biological determinants for psychopathology, as has been shown by the evolving field of epigenetics. This body of research suggests that environmental experiences can lead to the expression or deactivation of genes, and these changes not only lead to long-term changes in traits within an individual, but it might also be transmitted to later generations. This highlights the importance of learning and experience within and between generations. Therefore, and as acknowledged by the authors of this initiative, RDoC has limited clinical utility because it is primarily intended to advance future research, but is not yet intended as a guide for clinical decision making (Cuthbert & Kozak, 2013).
Most importantly, the RDoC initiative shares with the DSM the strong theoretical assumption that, similar to a viral infection, psychological problems are caused by a latent disease. In the case of the DSM, these latent constructs are measured through symptom reports and clinical impressions, whereas in the case of RDoC, the latent disease is measured through sophisticated behavioral tests and biological instruments, such as genetic tests and neuroimaging. The complex causal network approach offers an alternative, less restrictive, theoretical foundation for an empirically-based classification system.
The Complex Causal Network Perspective
A classification system of psychiatric disorders is an example of a complex system, because each disorder is defined by a number of interrelated symptoms and no symptom is specific to any particular disorder. As is true for any complex system, a better understanding of the pieces of the system cannot solve the complexity problem (Barabasi, 2012). For example, consciousness or cancer cannot be reduced to a single synaptic activity or mutations of a single gene, but are associated with hundreds of genes and billions of synapses, resulting in an elusive combinatorial problem. Understanding the workings of individual genes or synapses does not advance our understanding of the system as whole (Barabasi, 2012).
Traditionally, there are two primary models - the reflective and the formative model - for relating psychological attributes to observable variables (e.g., Schmittman et al., 2013, for further discussion). An example of a formative model is socio-economic status. In this model, the indicators define the construct and changing the indicators will also alter the formative construct. In contrast, the reflective model, which is the model of the DSM, assumes that different attributes (e.g., symptoms) are caused by the same latent construct (e.g., a mental disorder). In other words, a mental disorder is thought to be a reflective construct that causes the observable symptoms. This model is also consistent with causal essentialism in kinds (Ahn, Taylor, Kato, Marsh, & Bloom, 2013), because clinicians are more likely to believe that symptoms result from a single cause, that all patients with the disorder have this cause, and that the causal relations among symptoms are similar among patients with these disorders if the symptoms are correlated.
The current disease model of the DSM assumes that a psychiatric problem is caused by an underlying disease entity. Analogous to a flu virus, which causes high temperature, respiratory problems, sneezing, etc, it is assumed that there is an underlying cause for major depression, panic disorder, schizophrenia, etc. In other words, the symptoms of psychiatric illnesses are assumed to correlate because they are assumed to be caused by the same underlying disorder.
The primary conceptual problems with these traditional approaches include the uncertainty about causal pathways and processes between the latent construct and symptoms and the disregard of the causal relationships between the symptoms (Schmittmann et al., 2013). Adopting a complex causal network approach provides the opportunity to study the entire complexity of the system and has the advantage of not being limited to the assumption that symptoms of a psychiatric disorder are caused by the same latent disease (as is the case for the reflective model) or are merely labels for an arbitrary set of symptoms (as is the case for the formative model): Instead, disorders are assumed to exist as systems, rather than as entities (Borsboom & Cramer, 2013). An excellent analysis of the causal system approach for understanding posttraumatic stress disorder is provided by McNally (2012). A simple and illustrative example is the causal link between fear and avoidance: some people worry about having future panic attacks in certain situations after having experienced panic attacks in the past. This leads them to avoid certain places.
Thus, some symptoms (avoidance) depend causally on the presence of others (having experienced panic attacks in the past and worrying about future attacks). Interestingly, the DSM-5 separated agoraphobia from panic disorder, ignoring the causal relationship between concerns about experiencing panic attacks and avoidance of certain situations or places, which will likely introduce a high comorbidity between the two newly created distinct diagnostic categories, panic disorder and agoraphobia.
Adopting a complex causal network approach would further pave the way toward personalized medicine. Between-subjects networks are useful for investigating the general structure of psychiatric disorders because they can generate testable hypotheses about trajectories toward developing a psychiatric disorder that are shared by individuals. However, such patterns of individual differences provide limited information about how and why individuals develop psychiatric problems and how to best intervene. Each individual shows specific vulnerabilities and unique experiences, leading to particular problems, thus forming individual networks. Analyzing such individual, person-specific networks requires methodologies to capture the relevant variables to gather an individual’s thoughts, experiences, and behaviors in situations with specific triggers. The cognitive-behavioral framework provides the theoretical foundation to develop such a between-subjects and person-specific complex causal network.
The Cognitive-Behavioral Approach
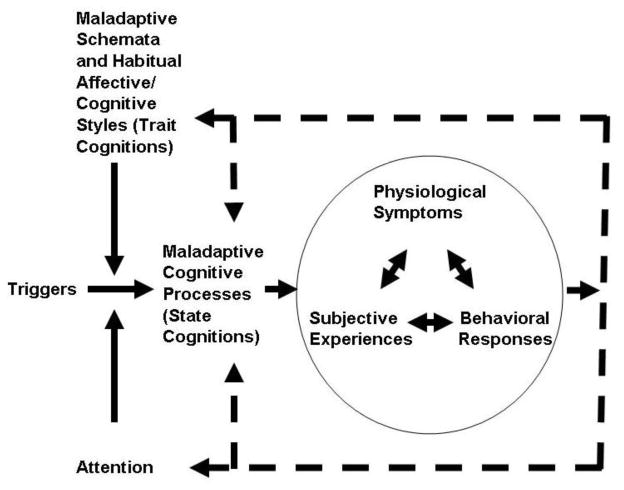
The general cognitive-behavioral model is schematically presented in Figure 1. This model depicts the components that provide the framework for the general, between- subjects complex causal network approach. In this model, maladaptive beliefs (schemata) lead to maladaptive specific (and often automatic) cognitions when attention is allocated to aspects of certain triggers, such as situations, events, sensations, or even other thoughts. These attention processes typically show a high degree of automaticity and can occur on a subconscious level. Once these processes reach the level of consciousness, the triggers are evaluated and interpreted. These appraisal processes then lead to specific subjective experiences, physiological symptoms, and behavioral responses.
Figure 1.
Between-subjects complex causal network based on the cognitive behavioral model of psychopathology (adopted from Hofmann, 2011).
The cognitive behavioral perspective to human suffering resulted in a highly effective treatment approach, cognitive behavioral therapy (CBT). Cognitive-behavioral researchers and clinicians have taken advantage of the semblance of order that these atheoretical classification systems offer to the field of psychopathology and, from that order, have developed models for a wide range of conditions.
CBT is a highly effective strategy for dealing with virtually all psychiatric disorders. A review of the efficacy of CBT for mental disorders would easily fill a textbook. CBT is not a single treatment protocol. Rather, CBT describes a family of interventions that share the same basic elements of the treatment model that focus on the importance of cognitive processes for emotion regulation. Although the specific treatment techniques depend on the symptoms that are targeted, the CBT protocols have been developed to be aligned with DSM categories. A recent review of meta-analyses identified 269 meta-analytic reviews examining CBT for virtually every psychiatric and psychological problem, including substance use disorder, schizophrenia and other psychotic disorders, depression and dysthymia, bipolar disorder, anxiety disorders, somatoform disorders, eating disorders, insomnia, personality disorders, anger and aggression, criminal behaviors, general stress, distress due to general medical conditions, chronic pain and fatigue, distress related to pregnancy complications and female hormonal conditions (Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012). The strongest support of CBT was found for anxiety disorders, somatoform disorders, bulimia, anger control problems, and general stress. These treatments are typically effective with children, adults, and older adults and they last longer and are less likely to require additional treatments than pharmacotherapy. Although effective, there is clearly still considerable room for further improvement of these treatments. Nevertheless, the success of the CBT protocols is remarkable, given that the interventions target the DSM categories that are grounded in a medical disease model. More recently, some authors have begun to develop CBT protocols that cut across diagnostic categories that are focused on specific dysfunctional emotion regulation strategies (unified treatment; e.g., Barlow, Allen, & Choate, 2004).
The general cognitive-behavioral model, as depicted in Figure 1, offers a framework for classifying mental disorders using a complex causal network perspective. At the core of the model are maladaptive cognitive processes. These cognitions can take on the form of trait or state variables.
The primary components of this complex causal network include maladaptive cognitive processes that are activated by specific triggers and moderated by attentional processes and trait cognitions, which include beliefs (schemata) and habitual affective/cognitive styles. Once activated, the maladaptive cognitive processes then cause specific subjective experiences, physiological symptoms, and behavioral responses. The following provides a more detailed description of the core components of this model. Although emotional disorders are often used as examples, the discussion is relevant for virtually all mental disorders (for a review, see Hofmann, 2011).
Triggers
Triggers are stimuli that set off the cognitive behavioral network associated with a psychological problem. These triggers can be external/situational, physiological/interoceptive, or cognitive in nature and they can be assessed via questionnaires, interviews, or psychological experiments. The triggers can be associated with the development of the disorder. However, as already noted for most psychological problems, initiating and maintaining factors are very different, because the reason a problem developed in the first place is often unrelated, or only tangentially related, to the reason the problem persists. The cognitive-behavioral perspective focuses on the here and now and on the factors maintaining a problem rather than the initiating factors. Identifying the former is essential to understand and modify psychological problems. In contrast, it is neither necessary nor sufficient to identify the initiating factors in order to treat a psychological problem.
Attention
Attentional processes are important elements in this model, especially for anxiety disorders. Attentional bias can be measured with the dot-probe paradigm, the modified Stroop task (e.g., Stroop, 1938), or other methods (McLeod, Mathews, & Tata, 1986). The dot-probe paradigm measures the distribution of visual attention. As part of a typical dot-probe experiment, participants are asked to press one of two buttons to identify the location of a dot that follows one of two words presented on a computer screen. These words typically vary in their emotional valence. The dot detection latencies determine whether visual attention has shifted toward or away from the threatening stimulus. A typical modified Stroop test asks participants to name the color of words with different emotional significance while ignoring the words” content.
Maladaptive Schemata and Habitual Affective/Cognitive Styles (Trait Cognitions)
Schemata are general, overarching beliefs that give rise of specific automatic thoughts in a given situation. These schemata often develop early on, often during childhood and adolescence, and take on the form of early maldaptive schemata (Young et al., 2003). These maladaptive schemata are longstanding characterological problems and viewed as general vulnerability factors for psychopathology as they are relevant for a broad range of psychiatric diagnoses.
In the formation of schemata, temperament can interact with early adverse relational experiences leading the person to feel that psychological core needs (e.g., secure attachment, autonomy, freedom to express valid needs and emotions, realistic limits) are not met. When a schema is triggered, the person responds with a maladaptive coping style (e.g., overcompensation, avoidance, surrender) that perpetuates the schema. Schemata can be assessed with the Young Schema Questionnaire (Young, 2003). However, interview data and behavioral/experimental tests can also provide information to identify the schemata.
Closely associated with schemata are maladaptive core beliefs and meta- cognitions (cognitions about cognitions) that often identify rules that determine how one ought to respond to a given situation. These beliefs can exist at a lower level of awareness such that the patient has rarely been able to reflect on them. Other times patients may be aware of their conditional beliefs and are able to state the rules that seem to govern their emotional and behavioral responses to situations. Core beliefs represent extreme, one-sided views towards the self, others, and the world that give rise both to the conditional assumptions and automatic thoughts. They are assumed to be primitive, extreme views that are formed as a result of early experiences. Core beliefs often take on the form of an absolute statement such as “I“ m a failure,” “I am unlovable,” or “I am in constant danger.”
Other important determinant trait factors of psychopathology are habitual affective/cognitive styles. It has been shown that some strategies tend to be maladaptive and associated with greater psychopathology (i.e., rumination, avoidance, suppression), whereas others tend to be adaptive (i.e., acceptance, reappraisal, and problem solving) and associated with less psychopathology (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Hofmann, Sawyer, Fang, & Asnaani, 2012). Similarly, the reliance on suppression to cope with emotional distress is associated with greater vulnerability for both the development of emotional disorders and the persistence of symptoms (Amstadter, 2008).
An effective strategy to regulate emotions is the ability to distance oneself from one’s own thoughts. In the more recent literature, this is often referred to as decentering (Hayes, 2004). This concept is closely related to distancing in traditional CBT (Beck, 1979). This may be achieved through mindfulness and other meditation practices that encourage a present-focused, nonjudgmental stance in regard to thoughts and feelings. People differ in their habitual tendency to use mindfulness as a coping strategy (trait mindfulness). It has been shown that more mindful people are less vulnerable to stress than less mindful individuals (Arch & Craske, 2010; Brown, Weinstein, & Creswell, 2012; Bullis, Boe, Asnaani, & Hofmann, 2014).
Although experimental studies generally identify some affective/cognitive styles as being adaptive (e.g., reappraisal, acceptance, being mindful) and others as maladaptive (rumination, worrying, avoidance, suppression), it is likely there is no single style that is always adaptive or maladaptive in all situations. Rather, mental health appears to be associated with the ability to flexibly apply the most adaptive strategy to the situational demands (Bonnano, Papa, Lalande, Westphal, & Coifman, 2004; Kashdan & Rottenberg, 2010). Therefore, it is quite possible that the ability to flexibly use the most adaptive regulation strategy in a given situation is a trait that is most predictive of mental health.
Some of these habitual affective/cognitive styles can be measured with self-report instruments (e.g., Gratz & Roemer, 2004; Hayes et al., 2004; Hofmann & Kashdan, 2010; Meyer, Miller, Metzger, & Borkovec, 1990; Treynor, Gonzalez, & Nolen-Hoeksema, 2003).
Maladaptive Cognitive Processes (State Cognitions) and their Consequences
The cognitive-behavioral model assumes that maladaptive cognitive processes are the primary mediators between the triggers and the psychological distress and are, therefore, the optimal treatment target. Cognitive processes are broadly defined and include attempts to regulate unwanted experiences, such as emotional distress. Effective treatments focus on promoting beneficial emotion regulation strategies and discouraging the use of ineffective strategies. Emotion regulation has been defined as the process by which people influence which emotions they have, when they have them, and how they experience and express these emotions (Gross, 2002). Thus, emotion regulation is a willful, cognitive activity that requires executive control. If the cognitive strategies underlying emotion regulation are insufficient or maladaptive, psychological problems can result as a consequence. As is true for trait reappraisal, state reappraisal is often an adaptive strategy. In contrast, attempts to suppress unwanted experiences are typically maladaptive because they tend to produce increased physiological arousal, greater autonomic instability, and more stress-related symptoms, despite the desire to down- regulate arousal (Campbell-Sills, Barlow, Brown, & Hofmann, 2006).
Negative self-statements and other negative self-referential cognitions are, to varying degrees, common in many forms of psychopathologies (Ingram, 1990; Schwartz & Garamoni, 1989). State rumination and state worrying are examples of maladaptive cognitive processes that are associated with negative affect (Mennin & Fresco, 2013; Segerstrom, Tsao, Alden, & Craske, 2000). It has been shown that both worrying and rumination become negatively reinforced by the reduction in aversive emotions (Borkovec et al., 1998; Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). Moreover, both are cognitive processes that involve primarily verbal activity and, to a lesser extent, imagery. Imagery and verbal processes are two cognitive processes that have different effects on the psychophysiological response to emotional material. For example, verbalizing a fearful situation can induce less cardiovascular response than visually imagining the same situation, possibly because verbalizations are used as a strategy for abstraction and disengagement (Borkovec et al., 1998; but also see Newman & Llera, 2011, and Newman, Llera, Erickson, Przeworski, & Castonguay, 2013, who did not find support for this). The physiological, subjective, and behavioral responses are best assessed with behavioral/experimental tests, but can also be measured through self-report and interview measures.
As shown in Table 1, behavioral/experimental tests should be well suited to assess many aspects of the cognitive behavioral system. Some of these tests could be face-valid situations that mirror real-world scenarios (e.g., a public speaking test for individuals with fear of public speaking). Other tests could be designed to assess specific cognitive biases using the dot-probe or Stroop test, or specific state or trait strategies.
Table 1.
Treatment-relevant classification components based on the cognitive-behavioral model.
| Components | Examples | Typical Data Source | ||
|---|---|---|---|---|
| Questionnaires | Interview | Experimental | ||
|
|
||||
| Triggers | External/situational, physiological/interoceptive, cognitive | √ | √ | √ |
|
| ||||
| Attention | Engagement/disengagement of attention allocation | √ | ||
|
| ||||
| Maladaptive Schemata | Core beliefs about self/future/world and meta-cognitions | √ | √ | √ |
|
| ||||
| Habitual Affective/Cognitive Styles (Trait Cognitions) | Negative self-perception, trait rumination, trait worrying, trait suppression, trait mindfulness | √ | √ | √ |
|
| ||||
| Maladaptive Cognitive Processes (State Cognitions) | Negative self-statements, state rumination, state worrying, state suppression, state mindfulness | √ | √ | √ |
|
| ||||
| Physiological Symptoms | Sympathetic activation, autonomic inflexibility | √ | ||
|
| ||||
| Subjective Experiences | Experience of fear/anxiety, anger, sadness, shame, disgust | √ | ||
|
| ||||
| Behavioral Responses | Avoidance, use of safety signals, withdrawal, disengagement | √ | ||
Note: The Table shows treatment relevant components for classifying mental disorders based on the between-subject complex causal cognitive-behavioral network model. Also depicted are examples how these components are expressed and methods for assessing them.
Discussion
The recently published DSM-5 (APA, 2013) generated a significant degree of criticism in the mental health care community. RDoC offers a dimensional alternative for classifying psychiatric disorders in order to capture the full variation from normal to abnormal. This approach implies that mental disorders are complex traits that are extremes on a spectrum of normal functioning. The goal is to determine cut-points along these dimensions, similar to defining the pathological state of hypertension on the blood- pressure dimension (Cuthbert & Insel, 2013). The cognitive-behavioral perspective also embraces a dimensional system of psychopathology that is based on behavioral, psychophysiological, interview, and self-report data. However, the cognitive-behavioral framework makes less restrictive model assumptions; RDoC is based on the strong and unsubstantiated assumption that symptoms of psychiatric disorders reflect the existence of latent disease entities. This premise is incompatible with the comorbidity problem. Moreover, the system is of questionable clinical utility and disconnected from the treatment literature, especially the overwhelming evidence from the cognitive-behavioral literature.
The complex causal network approach offers a less restrictive approach toward classifying mental disorders. Proponents of this approach argue that that it is neither necessary nor useful to accept the existence of a latent disorder construct to explain why the symptoms of a disorder hang together: Instead, the symptoms are strongly correlated because they are part of the same system, i.e., because they causally influence one another. Moreover, if one accepts that symptoms and causal connections between them are what constitute a mental disorder, the term “comorbidity” gathers a different meaning, because comorbidity can no longer meaningfully explained as a correlation between two distinct disorders, or as the result of a common underlying (neurobiological) dysfunction. Instead, the causal relations between symptoms constitute pathways that can connect different disorders via characteristics that are part of both disorders (e.g., negative self-perception can result in low mood and social anxiety).
It should be noted that many of these ideas are not new. Behaviorally and cognitively oriented clinicians and scholars have been advocating for a clinical case formulation approach rather than targeting a latent disease for decades (Eells, 2010; Goldfried & Wolfe, 1998; Lazarus, 1973; Staats, 1999). In fact, the person-specific complex causal network approach is fully in line with this behavioral and cognitive tradition. In addition, the proposed approach also provides a heuristically useful model of between-subjects complex causal network that allows for the basis of a treatment-relevant classification system.The limitations of the complex causal network approach include the overemphasis on self-reported symptoms (which was one of the major objections of RDoC toward the DSM) and the lack of a theoretical framework that explains why some symptoms or features of a disorder should cause others. What is missing in this innovative approach is a testable psychopathology model that explains why and how certain symptoms are causally related.
The cognitive-behavioral model offers such a system. Not only does it derive clearly testable predictions about the causal relationship between its components (e.g., self-deprecating thoughts cause low mood), but it also considers moderating variables (e.g., a negative self-schemata moderates the influence of triggers experiences on specific thoughts). Most importantly, the cognitive behavioral approach offers a treatment- relevant classification system. For example, two individuals, Harry and Sally, might receive the same DSM-5 diagnosis of social anxiety disorder and are, therefore, indistinguishable on a diagnostic level. However, their problems are maintained by different factors, requiring different interventions because their problems form two very different complex causal networks. Sally holds the core belief I am worthless and cannot inconvenience people. A simple task, such as needing to return a sweater to a store might become a highly dreaded task that she avoids. If she is forced to do it, she experiences self-deprecating thoughts (I will be judged negatively), which causes her a great degree of distress, feeling of shame, and submissive behaviors, such as avoiding eye-contact and lowering her voice.
In contrast, Harry is not very much bothered by negative self-focused statements. Instead, he might hold the core belief “I need to be in control of my body at all times,” and “people should not see my anxiety.” As a result, a public speaking event becomes a highly dreaded experience, because it causes him to experience strong physiological symptoms (heart racing and sweaty palms). He attempts to suppress his anxiety, but often shows clear behavioral signs of anxiety (stuttering and shaking of his hands) and he typically cuts his speech short as a form of avoidance. In both cases, the physiological symptoms, behaviors, and the subjective experience feed onto each other and further support the maladaptive cognitive appraisal of the situation, establishing a positive feedback loop and vicious cycle.
Adopting such a cognitive behavioral complex causal network framework not only provides an individually-tailored approach for classification purposes, but it also gives concrete guidance for treatment. Harry’s network of problems could be targeted by raising his level of distress tolerance and giving up control of his physiological symptoms. Therapeutic techniques to specifically target his beliefs about needing to be in control of his body at all times could be combined with exposure practices to induce strong physiological symptoms while performing in front of others while using acceptance and mindfulness strategies to counter his tendency to suppress his physiological symptoms. In contrast, Sally is likely to benefit more from interventions targeting her self-perception and her belief that she should not inconvenience others. A logical treatment approach for Sally would be to instruct Sally to purposely inconvenience others for no good reason (e.g., sending back a meal in a restaurant). For neither case, the diagnosis social anxiety disorder provides any clear guidance for therapy. In contrast, developing such a cognitive-behavioral case conceptualization can lead to very clear and specific treatment recommendations.
The limitation of the present cognitive behavioral model is also one of its advantages – its simplicity. Many additional factors that have not been considered in this simplistic model might contribute to an individual’s psychopathology, resulting in a considerably more complex network that is depicted in Figure 1. For example, in the case of anxiety, important specific dimensions include anxiety sensitivity, perfectionism, and intolerance to uncertainty, to name only few. These dimensions might factor into the model as specific expressions of trait or state cognitions.It could be argued that the CBT model as depicted in Figure 1 does not consider conditioning, extinction, and other mechanisms. However, it can be argued that cognitive processes are determinant factors of conditioning and extinction learning. More specifically, fear extinction in animals and exposure therapy in humans share similar cognitive processes that are associated with changes in CS-US (harm) expectancy (Hofmann, 2008). The model depicted in Figure 1 is compatible with these processes.
In conclusion, the cognitive-behavioral approach not only offers a treatment model, but also constitutes a sound theoretical framework for developing a classification system that is in line with the complex causal network approach. In line with the RDoC initiative, the cognitive behavioral approach is not restricted to clinician judgments and self-report data, but necessitates other data sources, including psychophysiological and behavioral measures. The biggest advantage of the cognitive behavioral approach is that the system is based on a refutable and empirically-based theoretical model that integrates different scientific disciplines and that can (and will) change as science further advances.
Highlights.
DSM-5 uses arbitrary cutoffs to define mental disorders
RDoC offers a biological alternative, but lacks clinical utility
The complex causal network approach moves beyond the latent disease model
The cognitive-behavioral model offers a possible classification framework.
The cognitive-behavioral model is consistent with the complex causal network approach.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahn WJ, Taylor EG, Kato D, Marsh JK, Bloom P. Causal essentialism in kinds. The Quarterly Journal of Experimental Psychology. 2013;66:1113–1130. doi: 10.1080/17470218.2012.730533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4. Washington, D.C: Author; 1994. (DSM-IV) [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. (DSM-5) [Google Scholar]
- American Psychological Association. APA’s statement on the DSM-5 development process. Washington, DS: Author; Jan, 2012. Retrieved from: http://www.apa.org/monitor/2012/01/statement-dsm.aspx. [Google Scholar]
- Amstadter A. Emotion regulation and anxiety disorders. Journal of Anxiety Disorders. 2008;22:211–221. doi: 10.1016/j.janxdis.2007.02.004. http://dx.doi.org/10.1016/j.janxdis.2007.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anteraper SA, Triantafyllou C, Sawyer AT, Hofmann SG, Gabrieli JD, Whitfield-Gabrieli S. Hyper-connectivity of subcortical resting state networks in social anxiety disorder. Brain Connectivity. doi: 10.1089/brain.2013.0180. (in press) [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: New American Library/Meridian; 1979. [Google Scholar]
- Arch JJ, Craske MG. Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behaviour Research and Therapy. 2006;44:1849–1858. doi: 10.1016/j.brat.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Barabasi AL. The network takeover. Nature Physics. 2012;8:14–16. doi: 10.1038/nphys2188. [DOI] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Belluck P, Carey B. Psychiatry’s guide is out of touch with science, experts say. The New York Times. 2013 May 6; Retrieved from http://www.nytimes.com.
- Blech J. Wahnsinn wird normal. Der Spiegel. 2013 Janaury; Retrieved from http://www.spiegel.de/spiegel/print/d-90638343.html.
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: The ability to enhance and suppress emotional expression predicts long-term adjustment. Psychological Science. 2004;157:482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Ray WJ, Stöber J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research. 1998;22:561–576. doi: 10.1023/A:1018790003416. [DOI] [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Brown KW, Weinstein N, Creswell JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012;37:2037–1241. doi: 10.1016/j.psyneuen.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullis JR, Boe HJ, Asnaani A, Hofmann SG. The benefits of being mindful: Trait mindfulness predicts less stress reactivity to suppression. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45:57–66. doi: 10.1016/j.jbtep.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Effects of suppression and acceptance on emotional responses of individuals with anxiety and mood disorders. Behaviour Research and Therapy. 2006;44:1251–1263. doi: 10.1016/j.brat.2005.10.001. http://dx.doi.org/10.1016/j.brat.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Craddock N, Cuthbert BN, Hyman SE, Lee FS, Ressler KJ. DSM-5 and RDoC: Progress in psychiatry research? Nature Reviews: Neuroscience. 2013;14:810–814. doi: 10.1038/nm3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Kozak MJ. Constructing constructs for psychopathology: The NIMH Research Domain Criteria. Journal of Abnormal Psychology. 2013;122:928–937. doi: 10.1037/a0034028. [DOI] [PubMed] [Google Scholar]
- Deacon BJ. The biomedical model of mental disorder: A critical analysis of its validity, utility, and effects on psychotherapy research. Clinical Psychology Review. 2013;33:846–861. doi: 10.1016/j.cpr.2012.09.007. [DOI] [PubMed] [Google Scholar]
- Doehrmann O, Ghosh SS, Polli FE, Reynolds GO, Whitfield-Gabrieli S, Hofmann SG, Pollack M, Gabrieli JD. Predicting treatment response in social anxiety disorder from functional magnetic resonance imaging. JAMA Psychiatry. 2013;70:87–97. doi: 10.1001/2013.jamapsychiatry.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eells TD. Handbook of psychotherapy case formulation. 2. New York, NY: Guilford Press; 2010. [Google Scholar]
- Francis A. Saving Normal: An Insider Revolt against Outdiagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life. New York, NY: HarverCollins; 2013. [DOI] [Google Scholar]
- Goldfried MR, Wolfe BE. Toward a more clinically valid approach to therapy research. Journal of Consulting and Clinical Psychology. 1998;66:143–150. doi: 10.1037/0022-006X.66.1.143. [DOI] [PubMed] [Google Scholar]
- Gornall J. DSM-5: A fatal diagnosis? BMJ. 2013;346:f3256. doi: 10.1136/bmj.f3256. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gross JJ. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/S0048577201393198. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Polusny MA, Dykstra TA, Batten SV, Bergan J, Stewart SH, Zvolensky MJ, Eifert GH, Bond FW, Forsyth JP, Karekla M, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. http://opensiuc.lib.siu.edu/tpr/vol54/iss. [Google Scholar]
- Hofmann SG. Cognitive processes during fear acquisition and extinction in animals and humans: Implications for exposure therapy of anxiety disorders. Clinical Psychology Review. 2008;28:199–210. doi: 10.1016/j.cpr.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. An introduction to modern CBT: Psychological solutions to mental health problems. Chichester, UK: Wiley-Blackwell; 2011. [Google Scholar]
- Hofmann SG, Asnaani A, Vonk JJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research. 2012;36:427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Kashdan TB. The Affective Style Questionnaire: Development and psychometric properties. Journal of Psychopathology and Behavioral Assessment. 2010;32:255–263. doi: 10.1007/s10862-009-9142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety. 2012;29:409–416. doi: 10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- Ingram RE. Self-focused attention in clinical disorders: Review and a conceptual model. Psychological Bulletin. 1990;107:156–176. doi: 10.1037/0033-2909.107.2.156. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Carvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30:865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K, Kupfer D, Narrow W, Phillips K, Fawcett J. Guidelines for making changes to DSM-V. 2009 Retrieved from: http://www.dsm5.org/ProgressReports/Documents/Guidelines-for-Making-Changes-to-DSM_1.pdf.
- Lazarus AA. Multimodal behavior therapy: Treating the “basic id. Journal of Nervous and Mental Disease. 1973;156:404–411. doi: 10.1097/00005053-197306000-00005. [DOI] [PubMed] [Google Scholar]
- MacLeod C, Mathews A, Tata P. Attentional bias in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037/0021-843X.95.1.15. [DOI] [PubMed] [Google Scholar]
- McNally RJ. What is mental illness? Cambridge, MA: Harvard University Press; 2011. [Google Scholar]
- McNally RJ. The ontology of posttraumatic stress disorder: Natural kind, social construction, or causal system? Clinical Psychology: Science and Practice. 2012;19:220–228. doi: 10.1111/cpsp.12001. [DOI] [Google Scholar]
- Mennin DS, Fresco DM. What, me worry and ruminate about DSM-5 and RDoC?: The importance of targeting negative self-referential processing. Clinical Psychology: Science and Practice. 2013;20:259–268. doi: 10.1111/cpsp.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miller GA. Mistreating psychology in the decades of the brain. Perspectives on Psychological Science. 2010;5:716–743. doi: 10.1177/1745691610388774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. NIMH Strategic Plan. 2008 Retrieved from: http://www.nimh.nih.gov/about/strategic-planning-reports/nimh-strategic-plan-2008.pdf.
- Newman MG, Llera SJ. A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a Contrast Avoidance Model of worry. Clinical Psychology Review. 2011;31:371–382. doi: 10.1016/j.cpr.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: A review and theoretical synthesis of research on nature, etiology, and treatment. Annual Review of Clinical Psychology. 2013;9:275–297. doi: 10.1146/annurev-clinpsy-050212-185544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Persons JB. Case formulation-driven psychotherapy. Clinical Psychology: Science and Practice. 2006;13:167–170. doi: 10.1111/j.1468-2850.2006.00019.x. [DOI] [Google Scholar]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas in Psychology. 2013;31:43–53. doi: 10.1016/j.newideapsych.2011.02.007. [DOI] [Google Scholar]
- Schwartz RM, Garamoni GL. Cognitive balance and psychopathology: Evaluation of an information processing model of positive and negative states of mind. Clinical Psychology Review. 1989;9:271–294. doi: 10.1016/0272-7358(89)90058-5. [DOI] [Google Scholar]
- Segerstrom SC, Tsao JCI, Alden LE, Craske MG. Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognitive Therapy and Research. 2000;24:671–688. doi: 10.1023/A:1005587311498. [DOI] [Google Scholar]
- Staats AW. Unifying psychology requires new infrastructure, theory, method, and a research agenda. Review of General Psychology. 1999;3:3–13. doi: 10.1037/1089-2680.3.1.3. [DOI] [Google Scholar]
- Stroop JR. Factors affecting speed in serial verbal reactions. Psychological Monographs. 1938;50:38–48. doi: 10.1037/h0093516. [DOI] [Google Scholar]
- Szasz T. The myth of mental illness: Foundations of a theory of personal conduct. New York: Hoeber-Harper; 1961. [Google Scholar]
- Treynor W, Gonzalez R, Noeln-Hoeksema S. Rumination reconsidered: A psychometric analyisis. Cognitive Therapy and Research. 2003;27:248–259. doi: 10.1023/A:1023910315561. [DOI] [Google Scholar]
- Varga S. Defining mental disorder: Exporing “the natural function” approach. Philosophy, Ethics, and Humanities in Medicine. 2012;6:1. doi: 10.1186/1747-5341-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JE, Klosko MW, Weishaar ME. Schema therapy: A practitioner’s guide. New York: Guilford Press; 2003. [DOI] [Google Scholar]