Abstract
Denture fractures are common in daily practice, causing inconvenience to the patient and to the dentists. Denture repairs should have adequate strength, dimensional stability and color match, and should be easily and quickly performed as well as relatively inexpensive.
Objective
The aim of this study was to evaluate the flexural strength of acrylic resin repairs processed by different methods: warm water-bath, microwave energy, and chemical polymerization.
Material and methods
Sixty rectangular specimens (31x10x2.5 mm) were made with warm water-bath acrylic resin (Lucitone 550) and grouped (15 specimens per group) according to the resin type used to make repair procedure: 1) specimens of warm water-bath resin (Lucitone 550) without repair (control group); 2) specimens of warm water-bath resin repaired with warm water-bath; 3) specimens of warm water-bath resin repaired with microwave resin (Acron MC); 4) specimens of warm water-bath resin repaired with autopolymerized acrylic resin (Simplex). Flexural strength was measured with the three-point bending in a universal testing machine (MTS 810 Material Test System) with load cell of 100 kgf under constant speed of 5 mm/min. Data were analyzed statistically by Kruskal-Wallis test (p<0.05).
Results
The control group showed the best result (156.04±1.82 MPa). Significant differences were found among repaired specimens and the results were decreasing as follows: group 3 (43.02±2.25 MPa), group 2 (36.21±1.20 MPa) and group 4 (6.74±0.85 MPa).
Conclusion
All repaired specimens demonstrated lower flexural strength than the control group. Repairs with autopolymerized acrylic resin showed the lowest flexural strength.
Keywords: Flexural strength, Denture fracture, Denture repair
INTRODUCTION
Fractures of the base of poly (methyl)-methacrylate dentures are common in clinical practice, happening more frequently in the midline of maxillary complete dentures3,5. These fractures are often related to poor fit of the denture base4,16, poorly balanced occlusion4,16, problems in design and manufacturing of the denture4, poor strength of the repair material4,16, as well as inherent stress on the denture base that happens over time16,29. Denture fractures occur outside and inside the mouth. Outside the mouth, they often occur as a consequence of impact (accidents), as a result of expelling the denture from the mouth while coughing, or simply of dropping the denture3,16,22. Inside, the causes of denture fracture can be excessive bite force, improper occlusal plane, high frenal attachment, lack of balanced occlusion, poor fit or limitations in denture base material1. When in function, midline fracture is the result of flexural fatigue failure caused by cyclic deformation of the base, and is more likely to occur because flexure of the denture base occurs along the midline21.
Denture repairs should have adequate strength, dimensional stability4,16,22,27, good color match4,10,15,16,22,27, are easily and quickly performed16,18,27, are relatively inexpensive10,15,27. Factors affecting adhesion and the mechanical properties of the repair material can influence the strength of the repaired denture. Attempts to improve the bond strength between the denture base resin and the repair material, through mechanical or chemical surface modification9,14,21,25,27, as well as the transverse strength, by metal wiring or fiber reinforcements10,11,14,18,25, have been described. The choice of denture base resin, as well as of the repair material may also influence the strength of the repaired denture5,6,15,19,23,24.
Heat-polymerized materials have been proven to have higher mechanical properties when compared with auto-polymerized materials4,6,17. However, laboratory packing and flasking procedures are time consuming and present risk of denture distortion by heat8.
Comparing the different repair techniques, was described that acrylic resins, when polymerized under pressure and then stored in water, were more resistant than those polymerized by trade polymerization method13. Accordingly, considering the variability of the repair materials and the different repairing techniques, herein we aimed at assessing the flexural strength of acrylic resin repairs using different processing techniques. It is expected that the different methods of polymerization of acrylic resins used to repair specimens allow flexural strength values similar to those of the non-repaired specimens.
MATERIAL AND METHODS
One control and three experimental groups (n=15) were formed according to the type of resin used for repairing specimens made of Lucitone 550 thermoactivated acrylic resin (Dentsply Trubite, York, PA, USA): 1) Control - no repair; 2) repair with Lucitone 550; 3) repair with Acron MC thermoactivated acrylic resin (GC Dental Ind. Corporation, Alsip, IL, USA); 4) repair with Simplex chemically activated acrylic resin (Artigos Odontológicos Clássicos, São Paulo, SP, Brazil).
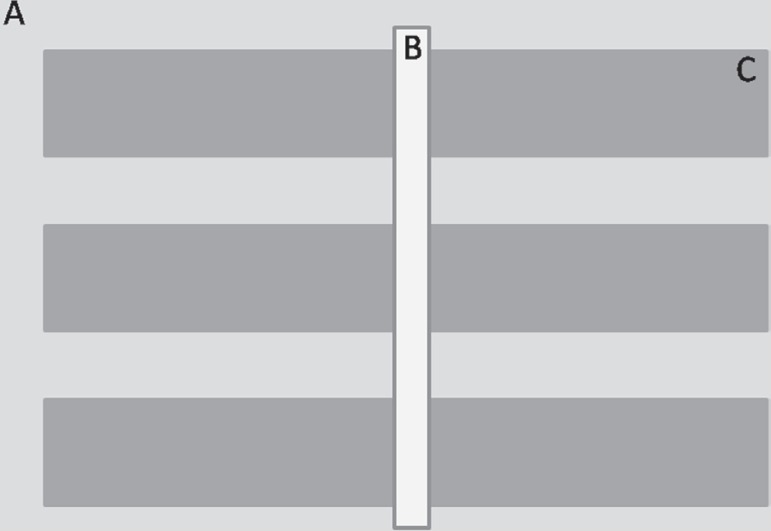
Metal master pattern with rectangular cavities associated to a metal spacer bar with 3.0x10.0x2.5 mm3 placed in the center of this pattern were used to make repaired specimens measuring 65.0x10.0x2.5 mm3, according to the Specification No.12 of the American Dental Association (Figure 1).
Figure 1.
A) Metal master pattern; B) Spacer Bar, and C) Rectangular cavities
Pattern was initially isolated with a thin layer of acrylic separating film (Cel-Lac, S.S. White, Rio de Janeiro, RJ, Brazil) and included in special flasks (Provecto Analítica, Jundiai, SP, Brazil) that can be used in the microwave oven reinforced with stone plaster type III Herodent (Cremer, São Paulo, SP, Brazil). With the plaster still fluid, one matrix was placed on each flask, maintaining its superior face exposed. After 60 min, each matrix compartment was filled with liquid wax (Kota Imports, São Paulo, SP, Brazil), and the counter flask was again filled with a new portion of stone plaster type III. The specimens of control group were made without use of the metal spacer bar.
After setting of the stone, the flask was opened and the wax was removed with hot water. The inner surface of the metal pattern was coated with acrylic separating film and the cavities were filled with acrylic resin (Lucitone 550), mixed according to the manufacturer's instructions, keeping the metal spacer bar placed only to groups 2, 3 and 4. The flask was closed to be pressed in a hydraulic press (Delta, Delta Máquinas Especiais, Vinhedo, SP, Brazil). A cellophane sheet was placed over acrylic resin before the flask was closed. The initial pressing was carried out with 800 kg to eliminate excess resin. Then, the flask was opened, the cellophane sheet was removed and a second pressing was carried out with 1,250 kg for 30 min. After this procedure, the flask was immersed in water at 74°C for 9 h in a polymerization unit (Termotron P-100, Termotron do Brasil Ltda, São Paulo, SP, Brazil). After being left at room temperature (26°C), the flasks were carefully opened and the metal spacer bar was removed. The acrylic specimens were also removed and abraded with 200-, 400-, 600-, 1000-, 1500-grit silicon carbide paper (Norton, Comercial e Técnica de Abrasivos Ltda., Campinas, SP, Brazil) in a decreasing sequence of abrasiveness, followed by final polishing with 1 µm diamond paste. All specimens were stored in distilled water at 37°C for 1 week before repair.
Each specimen was then replaced on the flaks in order to maintain a uniform space for the repair material and to determine the alignment of the specimens. For all groups butt joint surfaces without treatment was produced.
Upon removal of the space bar, the 2 sections of the specimens were repaired using the 3 different acrylic resins. In group 2, repairs were done with acrylic resin Lucitone 550, prepared according to the manufacturer's recommendations. Lucitone 550 resin was placed under compression (1250 kg) for 30 min at room temperature, and polymerized in short-cycle water bath (60 min under 100ºC degrees)26. Specimens of group 3 were repaired using acrylic resin Acron Mc, also under same compression for 30 min, at room temperature (23ºC) and polymerized in a domestic microwave (Sensor Crisp 38, Brastemp, Manaus, AM, Brazil) for 3 min at 500 W17. Finally, in group 4, repair materials were chemically polymerized and placed in the flask, under same compression, in water bath (55°C for 15 min)26. This method was conducted in order to improve their physical properties25 and standardize the amount of material to be used in the repair. Prior to the flexural strength tests, all specimens were stored again in distilled water at 37°C for 1 week.
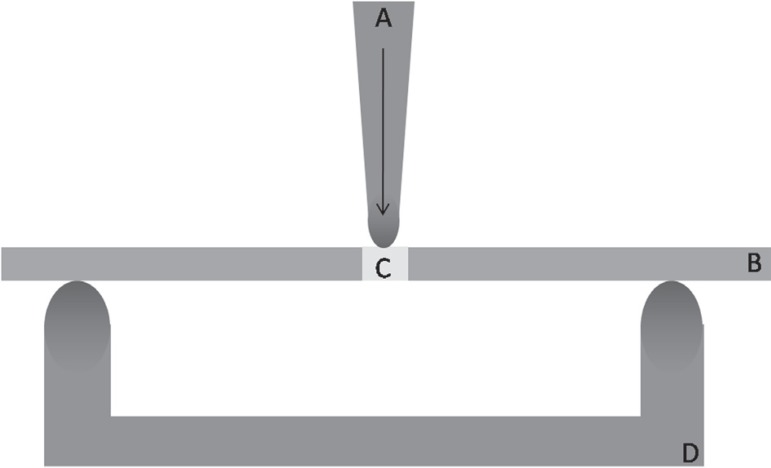
The three-point bending flexural strength test was conducted in a computerized device for mechanical assays (MTS-810 - MTS Systems Corporation, Eden Praire, MN-USA) with load cell of 100 kgf under constant speed of 5 mm/min6. Force was applied in the center of the specimens (repair area)4,25, in opposition to the supports, with a round-end point. Force was uniformly increased until fracture of the specimens (Figure 2). The maximum load applied was registered and calculated in N.
Figure 2.
Scheme of test in MTS 810: A) round-end point, B) resin specimen, C) resin repair, and D) support for specimen
The maximum load applied was used to calculate the flexural strength by means of the specimens' cross sectional area, according the following equation:
Where: S= transverse strength; W= load at fracture, L= distance between supporting wedges (50 mm); b= width of the specimen (10 mm); d= thickness of the specimen (2.5 mm).
Preliminary analysis of data showed a non-normal distribution. Thus, the Kruskal-Wallis non-parametric test was adopted to analyze the results (p<0.05) followed by Student-Newman-Keuls test for multiple comparisons. Statistical analysis was done using BioStat 5.0 software (AnalystSoft, Vancouver, BC, Canada).
RESULTS
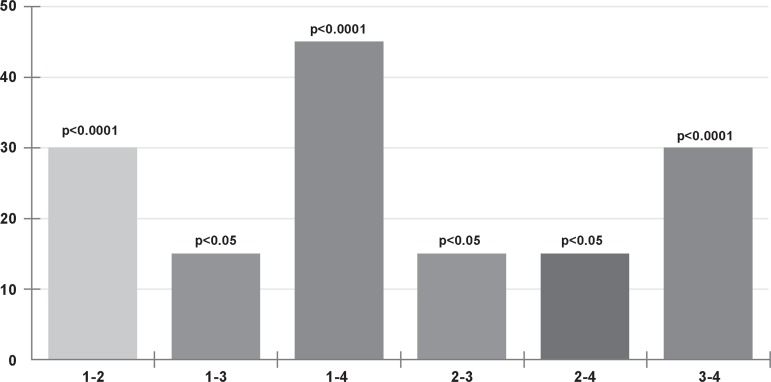
Table 1 presents flexural strength values of each group, standard deviation (SD), mean and median for the all groups. There was significant difference among groups (p<0.05), as demonstrated by Kruskal Wallis statistical test and Student-Newman-Keuls for statistical comparison Figure 3.
Table 1.
Measurements of rupture tension in the MPa, standard deviation (SD), mean and median
| Resins | ||||
|---|---|---|---|---|
| Specimens | Control | Lucitone 550 | Acron MC | Simplex |
| 1 | 158.008 | 37.536 | 41.822 | 7.215 |
| 2 | 153.408 | 35.285 | 46.700 | 7.543 |
| 3 | 153.510 | 38.629 | 44.772 | 6.845 |
| 4 | 157.037 | 34.171 | 44.747 | 8.694 |
| 5 | 157.328 | 36.416 | 42.266 | 6.014 |
| 6 | 158.937 | 35.648 | 45.746 | 7.598 |
| 7 | 155.552 | 36.149 | 42.716 | 5.780 |
| 8 | 154.768 | 34.422 | 40.839 | 6.903 |
| 9 | 156.347 | 35.645 | 39.896 | 5.841 |
| 10 | 154.301 | 36.470 | 41.956 | 5.527 |
| 11 | 154.647 | 37.457 | 45.532 | 6.478 |
| 12 | 155.496 | 35.698 | 40.562 | 7.210 |
| 13 | 157.903 | 36.531 | 39.587 | 5.987 |
| 14 | 154.838 | 37.469 | 44.329 | 6.432 |
| 15 | 158.607 | 35.699 | 43.872 | 7.025 |
| SD | 1.832 | 1.205 | 2.257 | 0.856 |
| Mean | 156.046 | 36.215 | 43.023 | 6.742 |
| Median | 155.552 | 36.149 | 42.716 | 6.845 |
Figure 3.
Intergroup comparisons (Kruskal-Wallis; p<0.05)
The best result was demonstrated by group 1 (control) followed by group 3 (microwave), 2 (warm water-bath) and 4 (chemical polymerization), in a decreasing order of strength. The flexural strength of group 3 was up to 27% of the intact specimens' strength. The types of failures of the specimens were not observed in this study.
DISCUSSION
This study assessed the flexural strength of 3 different types of acrylic resins, used in the repair of rectangular specimens produced with acrylic resins by different methods of polymerization. The repair material of choice depends on the following factors: length of time required for making the repair, transverse strength obtained with the repair material, and degree to which dimensional accuracy is maintained during the repair. Other important factor is that the increase in the temperature of polymerization improves mechanical and chemical properties of acrylic resins7.
All repaired groups demonstrated flexural values lower than that of the intact specimens in this study. The hypothesis tested in this study was thus rejected. It was found in test group that microwave-cured resin had the highest intact transverse strength with a mean value of 43.023 MPa, followed by warm water-bath-cured resin, with a mean value of 36.215 MPa and chemically polymerized resin with a mean value 6.742 MPa.
The increased transverse strength of microwave-cured resin (Acron MC) was probably due to the presence of less rubber in its composition as compared to conventional warm water-bathcured resin (Lucitone 550), which makes the last one behave more elastically, demonstrating low final strength values20. Moreover, some studies have shown that microwave-cured resins have decreased porosity because the heat necessary to break the benzoyl peroxide molecule into free radicals is created inside the resin once microwave radiations have greater penetrating capability15,20. This way, the heat is dispersed more efficiently and polymerization is rapid and decreases residual monomer content as compared to warm waterbath-cured resin.
On the other hand, in this study, chemical polymerizing showed the worst flexural strength values mean, when compared to the others groups, in agreement with other study25. This method is the most commonly used for denture repairs in daily practical. However, it has been shown that, not all the monomer is converted to polymer in denture repair, and the level of residual monomer has been demonstrated to affect other properties. It is possible that the repair strength could be improved by effecting further polymerization like microwave energy or warm water-bath28. A way to improve the performance of this type of polymerization is that dentures repaired with auto-polymerized acrylic resin should be stored in water for a time between 24 h and 1 week before being installed, allowing to the complete polymerization of the material9. However, it is important to consider that in clinical practice there is often urgency in repairing dentures, which make the time recommended by the authors unfeasible, in order to avoid embarrassing situations for the patients.
As all in vitro studies, the present research has limitations. Although this work compared different methods of polymerization, one of the limitations of this study is the use of resins of different commercial brands and compositions. However, the methods can be used safely for comparisons, once it agrees with the studies cited previously20,25,28. Further research is needed to evaluate these results under conditions that simulate a clinical situation like thermal cycling and/or cyclic loading.
CONCLUSIONS
Within the limitations of this in vitro study, the following conclusions were found:
1-The repaired specimens showed lower flexural strength, as compared to the intact specimens (control group);
2-Repairs with autopolymerized acrylic resins showed the lowest flexural strength;
3-Final results are influenced by the repair material.
REFERENCES
- 1.Agarwal M, Nayak A, Hallikerimath R. A study to evaluate the transverse strength of repaired acrylic denture resins with conventional heat-cured, autopolymerizing and microwave-cured resins: an in vitro study. The Journal of Indian Prosthodontic Society. 2008;8:36–41. [Google Scholar]
- 2.Andreopoulos AG, Polyzois GL, Demetriou PP. Repairs with visible light-curing denture base materials. Quintessence Int. 1991;22:703–706. [PubMed] [Google Scholar]
- 3.Beyli MS, Von Fraunhofer JA. An analysis of causes of fracture of acrylic resin dentures. J Prosthet Dent. 1981;46:238–241. doi: 10.1016/0022-3913(81)90206-7. [DOI] [PubMed] [Google Scholar]
- 4.Beyli MS, Von Fraunhofer JA. Repair of fractured acrylic resin. J Prosthet Dent. 1980;44:497–503. doi: 10.1016/0022-3913(80)90067-0. [DOI] [PubMed] [Google Scholar]
- 5.Darbar UR, Huggett R, Harrison A. Denture fracture - a survey. Br Dent J. 1994;176:342–345. doi: 10.1038/sj.bdj.4808449. [DOI] [PubMed] [Google Scholar]
- 6.Dar-Odeh NS, Harrison A, Abu-Hammad O. An evaluation of self- cured and visible light-cured denture base materials when used as a denture base repair material. J Oral Rehabil. 1997;24:755–760. doi: 10.1046/j.1365-2842.1997.00571.x. [DOI] [PubMed] [Google Scholar]
- 7.Dogan A, Bek B, Cevik NN, Usanmaz A. The effect of preparation conditions of acrylic denture base materials on the level of residual monomer, mechanical properties and water absorption. J Dent. 1995;23:313–318. doi: 10.1016/0300-5712(94)00002-w. [DOI] [PubMed] [Google Scholar]
- 8.Dyer RA, Howlett JA. Dimensional stability of denture bases following repair with microwave resin. J Dent. 1994;22:236–241. doi: 10.1016/0300-5712(94)90120-1. [DOI] [PubMed] [Google Scholar]
- 9.Harrison WM, Stansbury BE. The effect of joint surface contours on the transverse strength of repaired acrylic resin. J Prosthet Dent. 1970;23:464–472. doi: 10.1016/0022-3913(70)90014-4. [DOI] [PubMed] [Google Scholar]
- 10.John J, Gangadhar SA, Shah I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J Prosthet Dent. 2001;86:424–427. doi: 10.1067/mpr.2001.118564. [DOI] [PubMed] [Google Scholar]
- 11.Karacaer O, Dogan OM, Tinçer T, Dogan A. Reinforcement of maxillary dentures with silane-treated ultra high modulus polyethylene fibers. J Oral Sci. 2001;43:103–107. doi: 10.2334/josnusd.43.103. [DOI] [PubMed] [Google Scholar]
- 12.Keyf F, Uzun G. The effect of glass fibre-reinforcement on the transverse strength, deflection and modulus of elasticity of repaired acrylic resins. Int Dent J. 2000;50:93–97. doi: 10.1002/j.1875-595x.2000.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 13.Leong A, Grant AA. The transverse strength of repairs in polymethyl methacrylate. Aust Dent J. 1971;16:232–234. doi: 10.1111/j.1834-7819.1971.tb03412.x. [DOI] [PubMed] [Google Scholar]
- 14.Nagai E, Otani K, Satoh Y, Suzuki S. Repair of denture base resin using woven metal and glass fiber: effect of methylene chloride pretreatment. J Prosthet Dent. 2001;85:496–500. doi: 10.1067/mpr.2001.115183. [DOI] [PubMed] [Google Scholar]
- 15.Ng eT, Tan LH, Chew BS, Thean HP. Shear bond strength of microwaveable acrylic resin for denture repair. J Oral Rehabil. 2004;31:798–802. doi: 10.1111/j.1365-2842.2004.01295.x. [DOI] [PubMed] [Google Scholar]
- 16.Polyzois GL, Andreopoulos AG, Lagouvardos PE. Acrylic resin denture repair with adhesive resin and metal wires: effects on strength parameters. J Prosthet Dent. 1996;75:381–387. doi: 10.1016/s0022-3913(96)90029-3. [DOI] [PubMed] [Google Scholar]
- 17.Polyzois GL, Handley RW, Stafford GD. Repair strength of denture base resins using various methods. Eur J Prosthodont Restor Dent. 1995;3:183–186. [PubMed] [Google Scholar]
- 18.Polyzois GL, Tarantili PA, Frangou MJ, Andreopoulos AG. Fracture force, deflection at fracture, and toughness of repaired denture resin subjected to microwave polymerization or reinforced with wire or glass fiber. J Prosthet Dent. 2001;86:613–619. doi: 10.1067/mpr.2001.120069. [DOI] [PubMed] [Google Scholar]
- 19.Rached RN, Del-Bel Cury AA. Heat-cured acrylic resin repaired with microwave-cured one: bond strength and surface texture. J Oral Rehabil. 2001;28:370–375. doi: 10.1046/j.1365-2842.2001.00666.x. [DOI] [PubMed] [Google Scholar]
- 20.Rached RN, Powers JM, Del Bel Cury AA. Repair strength of autopolymerizing, microwave, and conventional heat-polymerized acrylic resins. J Prosthet Dent. 2004;92:79–82. doi: 10.1016/j.prosdent.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Shen C, Colaizzi FA, Birns B. Strength of denture repairs as influenced by surface treatment. J Prosthet Dent. 1984;52:844–848. doi: 10.1016/s0022-3913(84)80016-5. [DOI] [PubMed] [Google Scholar]
- 22.Stipho HD, Stipho AS. Effectiveness and durability of repaired acrylic resin joints. J Prosthet Dent. 1987;58:249–253. doi: 10.1016/0022-3913(87)90186-7. [DOI] [PubMed] [Google Scholar]
- 23.Stipho HD, Talic YF. Repair of denture base resins with visible light-polymerized reline material: effect on tensile and shear bond strengths. J Prosthet Dent. 2001;86:143–148. doi: 10.1067/mpr.2001.117055. [DOI] [PubMed] [Google Scholar]
- 24.Thean HP, Chew CL, Goh KI, Norman RD. An evaluation of bond strengths of denture repair resins by a torsional method. Aust Dent J. 1998;43:5–8. doi: 10.1111/j.1834-7819.1998.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 25.Vallittu PK, Lassila VP, Lappalainen R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat-polymerized resin. J Prosthet Dent. 1994;72:639–643. doi: 10.1016/0022-3913(94)90297-6. [DOI] [PubMed] [Google Scholar]
- 26.Vallittu PK, Ruyter IE. Swelling of poly(methyl methacrylate) resin at the repair joint. Int J Prosthodont. 1997;10:254–258. [PubMed] [Google Scholar]
- 27.Ward JE, Moon PC, Levine RA, Behrendt CL. Effect of repair surface design, repair material, and processing method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent. 1992;67:815–820. doi: 10.1016/0022-3913(92)90591-w. [DOI] [PubMed] [Google Scholar]
- 28.Yunus N, Harrison A, Huggett R. Effect of microwave irradiation on the flexural strength and residual monomer levels of an acrylic resin repair material. J Oral Rehabil. 1994;21:641–648. doi: 10.1111/j.1365-2842.1994.tb01179.x. [DOI] [PubMed] [Google Scholar]
- 29.Zappini G, Kammann A, Wachter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003;90:578–585. doi: 10.1016/j.prosdent.2003.09.008. [DOI] [PubMed] [Google Scholar]