Significance
Brain metastases represent the most common intracranial tumors in adults. Adequate chemotherapy delivery to the CNS is hindered by the blood–brain barrier. Efforts in intracranial chemotherapy delivery aim to maximize CNS levels while minimizing systemic toxicity; however, the success has been limited thus far. In this work, intracranial implanted doxorubicin and temozolomide microcapsules are compared with systemic administration in a novel rodent model of breast adenocarcinoma brain metastases. These microcapsules are versatile and efficacious, but that efficacy may depend on the ability of the chemotherapy to diffuse in brain tissue. These insights apply to other non-CNS applications of local drug delivery, and drugs should be evaluated based on their ability to penetrate the targeted tissue as well as their inherent efficacy.
Keywords: microcapsule, intracranial, chemotherapy, brain, metastases
Abstract
Metastases represent the most common brain tumors in adults. Surgical resection alone results in 45% recurrence and is usually accompanied by radiation and chemotherapy. Adequate chemotherapy delivery to the CNS is hindered by the blood–brain barrier. Efforts at delivering chemotherapy locally to gliomas have shown modest increases in survival, likely limited by the infiltrative nature of the tumor. Temozolomide (TMZ) is first-line treatment for gliomas and recurrent brain metastases. Doxorubicin (DOX) is used in treating many types of breast cancer, although its use is limited by severe cardiac toxicity. Intracranially implanted DOX and TMZ microcapsules are compared with systemic administration of the same treatments in a rodent model of breast adenocarcinoma brain metastases. Outcomes were animal survival, quantified drug exposure, and distribution of cleaved caspase 3. Intracranial delivery of TMZ and systemic DOX administration prolong survival more than intracranial DOX or systemic TMZ. Intracranial TMZ generates the more robust induction of apoptotic pathways. We postulate that these differences may be explained by distribution profiles of each drug when administered intracranially: TMZ displays a broader distribution profile than DOX. These microcapsule devices provide a safe, reliable vehicle for intracranial chemotherapy delivery and have the capacity to be efficacious and superior to systemic delivery of chemotherapy. Future work should include strategies to improve the distribution profile. These findings also have broader implications in localized drug delivery to all tissue, because the efficacy of a drug will always be limited by its ability to diffuse into surrounding tissue past its delivery source.
The rationale behind localized drug delivery is that high concentrations of drug may be reached in target tissue while minimizing systemic exposure to the large quantities of drug that might otherwise be necessary to achieve the desired biologic effect. Localized drug delivery has been used, such as in drug-eluting stents for coronary artery disease, metered dose inhalers for the treatment of asthma, and intracranial chemotherapy wafers for brain tumors. This premise is particularly applicable to conditions affecting tissue that is sequestered from systemic circulation, such as conditions affecting the CNS.
Adequate and efficacious drug delivery to the CNS has proved challenging. Systemic delivery methods are hindered by low permeability at the blood–brain barrier (BBB) to nonlipophilic drugs, which requires high systemic doses to be administered, thereby increasing systemic toxicity (1, 2). One method of circumventing the BBB is to place polymers that can release drug in a time-controlled manner at the site of tumor resection (3–6). Localized drug delivery devices provide high drug concentrations to the tumor site while preventing drug degradation and clearance until its release (7, 8). The efficacy of current intracranial drug delivery, such as Carmustine wafers, has promise, with a doubling of median survival from 9 to 20 mo in the case of Carmustine wafers (6, 9, 10). Phase III trial data indicated a 2-to 3-mo survival advantage in Carmustine wafers-treated patients (11), and Carmustine wafers continue to have a role combined with radiation and oral temozolomide (TMZ). However, nearly all patients still succumb to tumor progression.
The clinical focus of CNS drug delivery has been high-grade glioma (12). The modest increases in survival seen with such strategies have been attributed, in part, to the limited efficacy of the chemotherapies used and the disease target itself, because these tumors are among the most infiltrative and aggressive tumors studied (6, 8). It has also been postulated that the chemotherapy that has been used (Carmustine) does not diffuse well through brain tissue to produce tissue effects away from the implantation site. Such strategies have not been widely tested in more focal, noninfiltrative lesions of the brain, such as brain metastases. Several experiments have been conducted with polymer-based vehicles, which locally delivery chemotherapy, that suggest their efficacy in brain metastases (13). The microcapsules described here were studied in a rodent glioma model and showed tunable release kinetics and efficacy (12). These vehicles have, however, not been tested in brain metastases.
Metastases to the brain are the most commonly encountered tumors in the brain (14–17). It is estimated that 100,000–200,000 new cases are identified in the United States each year. Furthermore, 20% of patients with disseminated cancer have evidence of CNS involvement at autopsy (14). Certain tumors have a predilection to metastasize to the brain with nonsmall cell lung cancer, breast carcinoma, small cell lung carcinoma, malignant melanoma, renal cell carcinoma, gastrointestinal carcinoma, uterine carcinoma, and unknown primary carcinoma in decreasing frequency (14, 15). Cell surface markers seem to predict metastatic potential; for example, human epidermal growth factor receptor 2-positive breast carcinoma is more likely to present with CNS lesions (16). Metastases are focal in nature, with no true invasion of brain tissue in contrast to high-grade gliomas.
The treatment of brain metastases is often multimodal, with surgery, whole-brain radiotherapy (WBRT), stereotactic radiosurgery, and chemotherapy all playing a role (18, 19). The selection of specific modalities of treatment is dependent on patient-specific factors, such as number, size, and location of metastases, patient’s overall health and prognosis, and degree of symptoms attributable to these metastases. Surgery remains a standard treatment for metastatic lesions, particularly those that are symptomatic for patients with good functional status and well-controlled extracranial disease (19). Metastases tend to be noninfiltrative histologically, suggesting that surgical treatment should reduce or eliminate tumor burden and be beneficial. Multiple retrospective analyses have shown survival benefit from resection of single brain metastases, particularly combined with WBRT (19–22). More recent data from 2005 suggest that patients with two or three metastases also show increases in overall survival when the dominant symptomatic lesion is surgically resected (23). The most promising trial of combination chemotherapy showed response rates of 40–59% in breast cancer metastases to the brain (24), although more recent studies show a wide range of response from 10% to 45%, with variability based on the primary tumor (19). Systemic chemotherapy delivery has played a limited role in the treatment of brain metastases, in part because of the poor penetration through the BBB (19). More recent studies suggest that chemotherapeutic agents that have better penetration of the BBB, such as TMZ, may have a role in newly diagnosed metastases, not just as salvage therapy (25, 26). The agents that have shown promise include cyclophosphamide, 5-fluorouracil, methotrextate and vincristine combined, and TMZ, although the use of TMZ has been restricted to recurrent breast metastases (19, 27, 28). The use of TMZ in recurrent breast cancer brain metastases has shown modest increases in survival, although this patient population represents a selection of the most aggressive and refractory cancers that have withstood surgery, WBRT, and multiple other systemic chemotherapies.
Doxorubicin (DOX) has been used to treat early-stage, node-positive breast cancer, particularly HER2-positive tumors, although it is more commonly used for treatment of non-Hodgkins lymphoma and certain leukemias (29). Its clinical use in breast metastases to the brain has largely been limited by the resistance of the tumor to the chemotherapy as well as its poor penetration of the BBB and its dose-related adverse effects. The risk of developing potentially lethal cardiotoxicity increased significantly when doses of DOX reach 500 mg/m2 (30).
Microcapsules loaded with DOX or TMZ were administered intracranially in an experimental model of metastases to the brain in the following set of experiments. The CRL1666 cell line has been used in a metastatic spine model. This body of work represents the first time that it has been successfully used in a brain metastasis model to the best of our knowledge (31). Their efficacy was compared with systemic administration of DOX and TMZ. Tissue harvested from these animals was then processed for evidence of induction of apoptosis, and the distribution of drug released from the devices was also examined to test the relationship between drug distribution and biologic activity and efficacy.
Results
TMZ Liquid Crystal Polymer Devices.
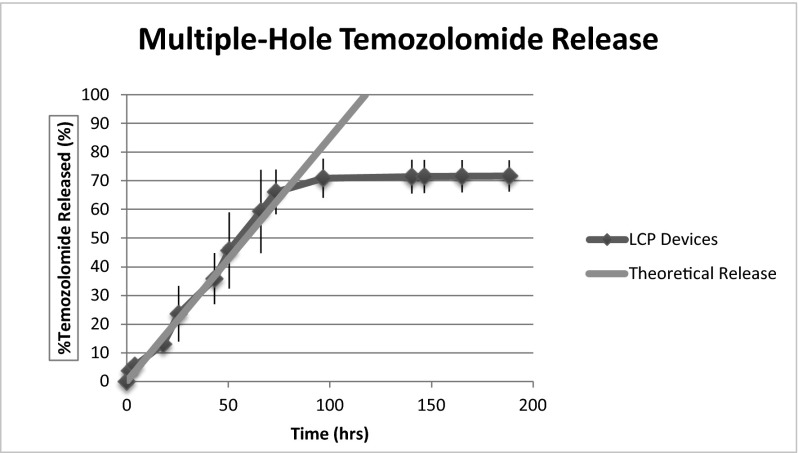
Liquid crystal polymer (LCP) is nonbiodegradable but biocompatible and inert, and its liquid crystal structure along with polymer chain rigidity do not allow drug partitioning through its membrane, which has been an issue with other polymer compounds used (such as polylactic acid). Fick’s Law of Diffusion was used to estimate the rate of drug delivery from microcapsule devices for the device prototype. Release kinetics were controlled by the diameter of device orifices, the number of orifices, and the solubility of the drug. The inner volume of the reservoir measured 1.5 mL, which allowed for higher drug loading per device volume compared with previous drug delivery devices (10, 32). One important innovation in this work was the use of the injection molding process for high-precision device production, which gave reliable and consistent results, including very small tolerances in volume. These devices can be engineered to achieve desired release kinetics. These devices are not biodegradable and were intact on retrieval from brain tissue at the time of animal euthanasia without evidence of biofouling. Multiple-orifice microcapsules were fabricated to increase the release rate of TMZ. These devices were manufactured with a total of five orifices for drug release: one 889-μm-diameter orifice in the cap and four 403-μm-diameter orifices around the circumference of the microcapsule reservoir. The theoretical release rate of TMZ from a single 889-μm-diameter orifice microcapsule was calculated by calculation of the flux (J) and the area (A) over which drug release occurs. The release rate of TMZ from these devices was found to be 2.5 × 10−5 mg/s or 2.16 mg/d (Fig. 1).
Fig. 1.
TMZ LCP device in vitro release.
In Vitro TMZ Drug Release Kinetics.
The in vitro release of TMZ from the LCP microcapsules into HPLC-grade water was assayed by HPLC. Control devices with sealed orifices were fabricated to test the hermeticity of the UV-curable epoxy and polymer housing. A theoretical release curve based on Fick’s Law was constructed for comparison with experimental drug release data. The calculated mass flow rate was 90 mg/h. The experiment was completed in triplicate. Results were reported as average values with SDs. The experimental release curves were in agreement with the theoretical release curve. The experimental TMZ release rate during the first 100 h of release was 88 mg/h ± 6.75 μg. At this time, 67% of the total 12-mg payload was released. The release rate decreased after 100 h, with 71% after 190 h. The devices fabricated for drug leak tests showed that the epoxy sealed the devices, preventing leakage. No drug partitioning through the polymer housing was detected, suggesting that LCP is capable of storing TMZ throughout the length of therapy.
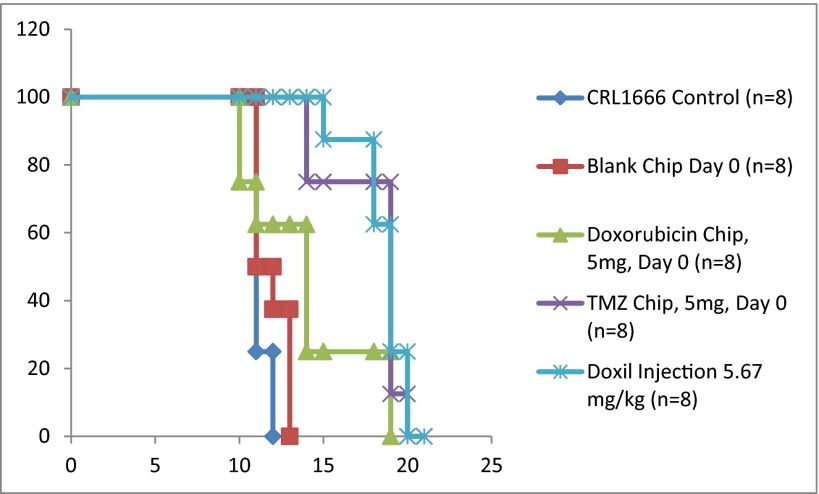
In Vitro DOX Drug Release Kinetics.
The in vitro release of DOX from LCP microcapsules was assayed using spectroscopy. A theoretical release curve was again constructed for comparison with experimental release data. The calculated mass flow rate for single-orifice devices was 1.21 mg/d. The calculated rate for multiple-hole devices was 2.16 mg/d (Fig. 2). The experiment was completed in triplicate. Results were reported as average values with SDs. At 300 h, nearly 70% of the 1-mg payload was released from single-orifice devices. Multiple-hole devices released 70% of the payload from multiple-hole devices over a shorter time period (Fig. 2). The experimental and theoretical release curves were in agreement.
Fig. 2.
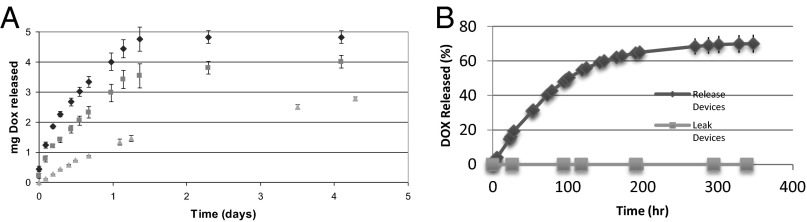
(A) In vitro release of DOX from one- (green), three- (red), and five-hole (blue) microcapsule devices loaded with 5 mg DOX. (B) DOX LCP single-orifice device in vitro release compared with leak devices.
In Vivo Efficacy Experiments.
Efficacy of locally delivered DOX and TMZ.
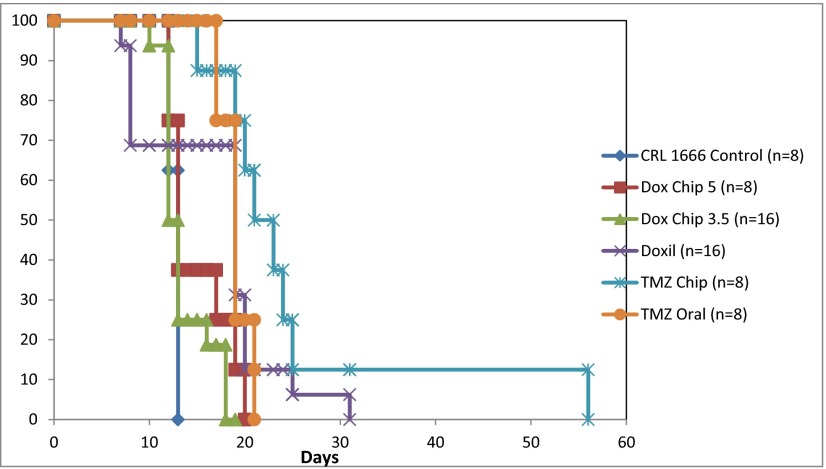
The primary efficacy outcome was animal survival (Fig. 3). The median survival of untreated control animals was 11 d, with mean of 10 d. Animals with unfilled (blank) LCP-implanted devices had mean and median survival of 12 d. Animals with DOX-loaded LCP devices (payload = 5 mg) had mean and median survival of 14 d. Rats from the systemic DOX and intracranial TMZ microcapsule groups exhibited longer survival rates. TMZ LCP device-treated animals had median and mean survival of 19 and 18 d, respectively, with all dying at 21 d. DOX-treated animals had mean and median survival of 19 d, with all animals dying by 25 d. Statistical analyses of the survival data were performed, and significant differences were observed between the control/DOX (P < 0.05), control/TMZ (P < 0.05), blank/DOX (P < 0.05), and blank/TMZ (P < 0.05) groups. There was no statistical significance shown between the control and DOX microcapsule groups.
Fig. 3.
Efficacy of locally delivered DOX and TMZ in breast metastasis model.
The second in vivo experiment tested the efficacy of DOX microcapsules loaded with lower payload (3.5 and 5 mg) against other groups. Animal survival was the primary outcome measure (Fig. 4). Untreated control animals experienced a median survival of 13 d. Those animals treated with DOX LCP microcapsules (payload = 5 mg) had median survival of 13 d and mean survival of 15 d. Animals treated with DOX LCP devices (payload = 3.5 mg) had median and mean survival of 12 and 13 d, respectively. DOX animals had median survival of 18 d, with mean survival of 13 d. Animals treated with oral TMZ had mean and median survival of 19 d, with all animals dying by 21 d. Animals with TMZ microcapsules had median and mean survival of 21 and 25 d, respectively, with all dying by 56 d. Significant differences were observed between control/oral TMZ (P < 0.05), control/TMZ LCP (P = 0.01), DOX LCP (5 mg)/TMZ LCP (P = 0.02), DOX LCP (3.5 mg)/TMZ LCP (P = 0.02), and DOX/TMZ LCP (P = 0.01). Increased survival in TMZ LCP microcapsules was not statistically significant compared with oral TMZ administration (P = 0.09).
Fig. 4.
Efficacy of locally delivered DOX and TMZ in second breast metastasis experiment.
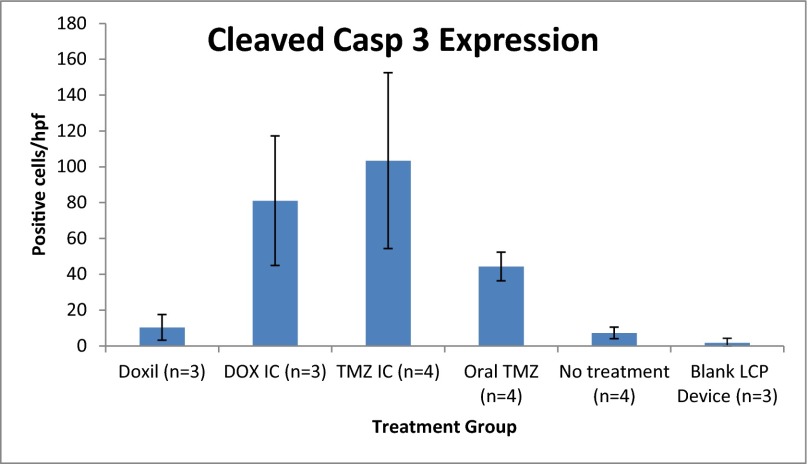
Cleaved caspase 3 expression on immunohistochemistry.
Brain tissue harvested from the in vivo efficacy studies was formalin-fixed and paraffin-embedded for immunohistochemistry. Coronal sections were obtained from each treatment group. Cells expressing the cleaved caspase 3 protein were counted per high-power field (hpf) in all sections and compared between treatment groups (Fig. 5). Untreated control animals had an average of 12 cells/hpf. DOX animal tissue had, on average, 10 cells/hpf. DOX LCP (5 mg) animal tissue had 81 cells/hpf. Blank LCP tissue had an average of 2 cells/hpf. TMZ LCP animal tissue had 103 cells/hpf. Using the unpaired t test, significant differences were observed between control/DOX microcapsule (P < 0.05), control/TMZ microcapsule (P < 0.05), control/oral TMZ (P = 0.001), DOX/DOX microcapsule (P < 0.05), and oral TMZ/TMZ microcapsule (P = 0.003).
Fig. 5.
Cleaved caspase 3 (cleaved casp 3) expression. IC, intracranial.
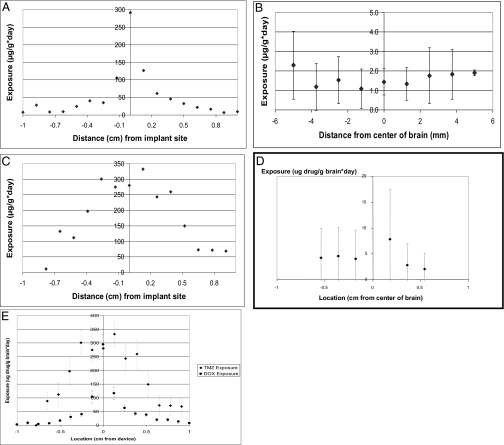
Drug distribution after release from microcapsules.
Healthy rodent brain tissues exposed to microcapsules filled with DOX or TMZ were examined for the spatial distribution of drug released over time (Fig. 6). Microcapsules loaded with DOX achieved narrow distribution, with a large peak seen at the sight of implantation and a steep drop out of drug level within 0.25 cm. Rodent tissue exposed systemically to DOX showed low but uniform levels of DOX. Microcapsules loaded with TMZ achieved broader distribution, with more uniform levels of drug seen within 0.5 cm, and a dropout was seen around 0.7 cm. Systemic TMZ achieved a similar distribution profile but with lower exposure levels than TMZ delivered through microcapsule.
Fig. 6.
(A) DOX distribution in rodent tissue when released from the microcapsule. (B) DOX distribution in rodent tissue when delivered systemically. (C) TMZ distribution in rodent tissue when released from the microcapsule. (D) TMZ distribution in rodent tissue when delivered systemically. (E) Comparison of drug distribution profiles when TMZ and DOX were delivered through the microcapsule.
Discussion
A growing trend in pharmacology is designing targeted therapies that minimize indiscriminate delivery and maximize delivery to the desired end organ. Multiple strategies have been used, including nanoparticle-driven delivery, liposomal formulation, and local delivery. Each strategy aims to minimize systemic toxicity. In these experiments, intracranial drug delivery was explored in metastatic breast tumors to the brain. The findings suggest that local chemotherapy delivery may be more efficacious than its systemic delivery, and this efficacy may hinge on drug diffusion. The broader implication for delivery outside the CNS is that successful local delivery depends on the efficacy and distribution of the drug. For those drugs that show strong biologic efficacy but with narrow distribution, strategies to improve distribution, such as chemical modification, should be deployed to improve their tissue penetration.
In Vitro Drug Release.
The rates of microcapsule devices exhibited close agreement with theoretical rates for the first 100 h of release. The release from single- and multiple-hole microcapsules plateaus after this time as chemical driving force decreases for diffusion. This plateau results in slower drug diffusion than theoretically predicted. The stability of TMZ also has a profound impact on the in vitro release kinetics. TMZ is a prodrug that quickly degrades into the bioactive MTIC (3-methyl-(triazen-1-yl)imidazole-4-carboxamide) molecule under basic conditions and in high-ionic strength solvents (32). This instability does not seem to be the case for DOX, because it is not a prodrug. In vitro release into water differs from in vivo conditions. The half-life of TMZ in water is considerably greater than its half-life in PBS, in FBS, and in vivo (32). This difference accounts for the close agreement with theory that is seen during the first 100 h of the TMZ water release profiles. Degradation of TMZ because of its instability in solution may account for the observed plateau and may explain why 100% drug is not released experimentally.
The microcapsule was designed for delivery of a large payload from a device small enough for rodent intracranial implantation. The tight dimensional tolerances between the rodent skull and the microcapsule device along with the introduction of a growing tumor could cause brain damage because of increased intracranial pressure (mass effect). This mass effect is pronounced in metastases patients and the primary indication for tumor resection surgery. The consequence of mass effect is shown in the short survival of blank microcapsule groups.
The microcapsule represents an improvement over prior intracranial delivery. As a reservoir-based vehicle, it maximizes payload delivered per unit volume compared with other local delivery strategies, such as polymer-composite wafers. Microcapsules are capable of delivering solid or liquid drug formulations, an ability that polymer-composite wafers do not currently possess. Such devices may house multiple classes of therapeutics: not just chemotherapy but macromolecules or tumor-directed viral particles. Release kinetics may be reliably tuned without the need for polymer degradation to occur for drug release, because the microcapsule is made from LCP, which does not permit drug partitioning. These properties allow for highly versatile and tunable drug delivery with the possibility of delivering a wide range of therapeutic compounds to brain tumors as well as other human diseases.
In Vivo Experiments.
The in vivo efficacy of localized TMZ and DOX therapy was investigated in a rodent breast metastasis model. TMZ microcapsules most effectively prolonged animal survival rates, and these results reached statistical significance in both experiments. Systemic DOX also showed prolonged survival compared with controls. Interestingly, DOX microcapsules did not show prolonged survival, regardless of payload chosen, suggesting that intracranial delivery is not always the most efficacious delivery route. Locally delivered TMZ is equivalent or superior to systemic TMZ. However, locally delivered DOX does not perform as well as systemic DOX. Systemic DOX is delivered in a liposomal formulation, which aides in its ability to evade the recticuloendothelial system, circulating longer. The differences in survival may be explained by distribution profiles seen in these experiments. Intracranial TMZ and systemic DOX do achieve more uniform distributions compared with intracranial DOX delivery, which seems to be quite narrow. Oral TMZ was administered 5 d after tumor implantation to mimic the peak release of TMZ from our device.
Intracranial DOX had narrow distribution, with levels dropping significantly at 2.5 mm, compared with the broader profile of intracranial TMZ, with drop off first seen at 5–7 mm. Strasser et al. (33) found that drug delivered from a biodegradable polymer implant was seen to diffuse only 1–2 mm from the site of implantation (33, 34). The reasons for the differences observed could be twofold: the polymer composite delivery vehicle may impact drug distribution itself, or the chemical properties of the agent delivered [BCNU (bis-chloroethylnitrosourea), DOX, or TMZ] are the larger determinant of the ability to diffuse in tissue. Given our experiments that used the same delivery vehicle for DOX and TMZ but yielded different profiles, results suggest that the chemical properties are likely the larger factor in determining depth of drug distribution. We suspect that prolonged survival in the systemic DOX is because of a low uniform level of DOX, which may be more ideal in treating cancer cells beyond the site of release.
One important caveat to our findings is that the distribution profiles were conducted in healthy rodents and not diseased animals. The relatively hypoxic environment of cancer coupled with the effect of tumor edema on diffusion may have a bearing here. These studies were a proof of principle of chemotherapy diffusion in brain tissue; they highlight the stark differences in intracranial distribution for different agents. These differences may explain limitations in efficacy of intracranial delivery, even in circumstances where the chemotherapy is potent and induces a robust apoptotic response (such as in intracranial DOX). Certainly, additional studies in diseased animals, where 3D models of drug distribution may be compared with the spatial distribution of biologic activity (such as cleaved caspase 3 expression), would be enlightening.
The histological analysis of each experimental group was also interesting. Intracranial delivery of chemotherapy led to more robust expression of apoptotic markers for both TMZ and DOX. However, the tissue evidence of cleaved caspase 3 did not explain or follow survival data; that is, intracranial (IC) DOX animals actually displayed poor survival compared with systemic DOX animals. The local activity of a drug may not adequately increase survival, because the drug must also act at some distance away from the implantation site. The ability of microcapsular TMZ to induce apoptosis more robustly than any other modality tested coupled with its wide distribution profile support the improved survival observed in the intracranial TMZ group.
The CRL1666 cell line has been used in a model of breast metastases to the spine. This body of work represents its first use in a brain metastasis model. Metastases are noninfiltrative tumors, and this cell line represents an appropriate histological model. In sharp contrast, primary brain cancer models should ideally model the infiltrative nature of these tumors. We believe that this body of work represents the potential to use local intracranial drug delivery for a different indication: to treat brain metastases. Their histologic nature may render them a better suited target by lessening the burden of broad drug distribution, because chemotherapies may only need to diffuse centimeters away from their delivery site to be efficacious.
TMZ was chosen based on the experience of certain groups with its use as a salvage treatment in breast metastases to the brain. In vitro cytotoxicity experiments against this cell line supported the choice to test its efficacy in vivo. Our results suggest that TMZ may play a clinical role in treatment of breast metastases to the brain. We feel that these results bear additional investigation. Currently, it is only used in a rescue setting but may have a role in first-line treatment of breast metastases to the brain, particularly when whole-brain radiation therapy may not be attractive given its long-term effects on cognition. This body of work is not meant to suggest that intracranial TMZ therapy alone may cure metastatic breast cancer; however, these studies represent a proof of concept that a chemotherapy-like TMZ, which until now, has been used with limited success, may be more beneficial when delivered intracranially in a device with tunable release kinetics.
Intracranial chemotherapy delivery has largely focused on high-grade gliomas, which are infiltrative by nature and quite different from metastatic lesions (13, 35). The limited efficacy of current intracranial delivery schema, including Carmustine wafers, may be attributed to the inability of chemotherapy to penetrate brain tissue well. Our experiments support the notion that differences in chemotherapeutic drug distribution seem to correlate to tissue response to chemotherapy and length of survival. Therefore, efforts in exploring intracranial drug delivery should focus, in part, on strategies to improve and broaden the distribution of the drug through tissue.
Conclusion
This work has shown that polymer microcapsules are capable of achieving tunable rates of release of various chemotherapies. TMZ microcapsules and systemic DOX seem to show promising efficacy against breast metastases to the brain. We have also shown that the tissues harvested from these experiments indicate that TMZ microcapsules induce apoptosis at higher levels than DOX microcapsules or systemic DOX. Finally, we have shown that the drug distribution profiles for intracranial and systemic DOX are quite different from that of intracranial TMZ and may explain the differences observed in survival. Microcapsules offer versatile targeted delivery without the requirement for intensive drug formulation necessary for liposomal, nanoparticle, or solvent drug-loading methods. These devices also have the unique ability to simultaneously deliver multiple therapies and may be used to deliver a variety of treatments beyond chemotherapy, including nanoparticles and small molecules. The ability of a drug to penetrate tissue requires additional investigation; drugs that show improved distribution profiles are likely to show more promise in treating lesions of the brain. Finally, the limitations of prior efforts at intracranial chemotherapy delivery may be overcome with focus on new therapeutic targets and strategies to improve the ability of a given chemotherapy to diffuse through CNS tissue. These insights apply to non-CNS applications of local drug delivery, where drug diffusion and inherent efficacy should be analyzed in target tissue. In cases where tissue penetration is poor, drug formulation strategies, although cumbersome, should improve the drug’s overall effect. When this two-pronged strategy is used, many new applications of localized drug delivery may be identified and further studied.
Materials and Methods
In Vitro Drug Release Kinetics of TMZ.
Twelve milligrams TMZ was loaded into LCP single- and multiple-hole devices. TMZ quantification was done using HPLC with acetonitrile (92:8) mobile phase and UV absorption at 316 nm. Interpolation of the readings with a standard curve was used to quantify the amount of drug released.
In Vitro Drug Release Kinetics of DOX.
DOX (3.5 and 5 mg) was loaded into LCP single- and multiple-hole polymer microcapsules for in vitro drug release characterization. DOX was quantified using the UV spectrophotometer at 481 nm. Interpolation of readings with a standard curve was used to quantify the amount of drug released.
In Vitro Cytotoxicity.
CRL1666 mammary adenocarcinoma cells were exposed to TMZ and DOX at varying concentrations to determine cytotoxicity. Cell proliferation was quantified using the MTT assay (Invitrogen).
In Vivo Experiments.
Tumor and device implantation.
Briefly, animals were anesthetized, and the dura was exposed. Stereotactic injection consisted of 75,000 tumor cells in 2.5 µL that were placed into the brain at a depth of 3.5 mm and delivered over 2 min. Devices were implanted at the time of tumor injection.
Efficacy of locally delivered TMZ and DOX.
Two experiments were conducted to determine the efficacy of locally delivered TMZ and DOX in tumor-bearing rats. All TMZ microcapsules used in this experiment had a total TMZ payload of 12 mg with a single 889-μm-diameter orifice cap. All DOX microcapsule devices used in this experiment had a total payload of 5 mg with a single 180-μm-diameter orifice cap and one 430-μm-diameter orifice on the reservoir. The first experiment included five experimental groups and 40 F344 rats: (i) no treatment (n = 8), (ii) i.p. DOX (Doxil; Johnson & Johnson) on days 0, 6, and 13 after tumor implantation (n = 8), (iii) empty devices (n = 8), (iv) TMZ-filled devices (n = 8), and (v) DOX-filled devices (n = 8). The second study included 80 F344 rats divided into seven experimental groups: (i) no treatment control (n = 16), (ii) oral TMZ by gavage on days 5–9 after tumor implantation (n = 8), (iii) TMZ-filled LCP microcapsule (n = 8), (iv) DOX-filled LCP microcapsule with 5 mg DOX payload (n = 8), (v) DOX-filled LCP microcapsule with 3.5 mg DOX payload (n = 16), (vi) i.p. DOX on days 0, 6, and 13 (n = 16), and (vii) empty device controls (n = 8). Overall, animal survival was compared with that of untreated controls. Death was the primary end point for efficacy studies. Kaplan–Meier survival curves were constructed.
Immunohistochemical staining.
Cleaved caspase 3 staining was developed by Cell Signaling Technology. The whole brain was sectioned and counted in aggregate, including tumor as well as peritumoral tissue.
Spatial drug distribution.
Nondiseased F344 rats underwent implantation of LCP devices with DOX or C13-radiolabeled TMZ. DOX LCP device animals were killed on days 2, 4, 6, 8, and 10 (n = 4). Radiolabeled TMZ animals were killed on days 2, 4, 6, 8, and 10 (n = 5). Rodent brain tissue was homogenized and processed for quantification of radiolabeled TMZ or DOX.
Western blotting.
Anti-cleaved caspase 3 Western blotting was done on rat brain tissue homogenates obtained from efficacy trials. Cleaved caspase 3 rabbit mAb was obtained from Cell Signaling Technology.
Supplementary Material
Acknowledgments
The authors thank Dr. Nancy Lin, a breast cancer oncologist at Dana–Farber Cancer Institute, who advised us on the clinical aspects of metastatic breast cancer treatment. This work was funded partially by National Institutes of Health Grant R01 EB006365-06 and Brain Science Foundation Private Grant 106708.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1313420110/-/DCSupplemental.
References
- 1.DeAngelis LM. Brain tumors. N Engl J Med. 2001;344(2):114–123. doi: 10.1056/NEJM200101113440207. [DOI] [PubMed] [Google Scholar]
- 2.Raghavan R, et al. Convection-enhanced delivery of therapeutics for brain disease, and its optimization. Neurosurg Focus. 2006;20(4):E12. doi: 10.3171/foc.2006.20.4.7. [DOI] [PubMed] [Google Scholar]
- 3.Brem H, Langer R. Polymer-based drug delivery to the brain. Sci Med (Phila) 1996;3:52–61. [Google Scholar]
- 4.Lesniak MS, Brem H. Targeted therapy for brain tumours. Nat Rev Drug Discov. 2004;3(6):499–508. doi: 10.1038/nrd1414. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer AJ, Piepmeier JM, Saltzman WM. New methods for direct delivery of chemotherapy for treating brain tumors. Yale J Biol Med. 2006;79(3-4):141–152. [PMC free article] [PubMed] [Google Scholar]
- 6.Brem H, et al. The Polymer-brain Tumor Treatment Group Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. Lancet. 1995;345:1008–1012. doi: 10.1016/s0140-6736(95)90755-6. [DOI] [PubMed] [Google Scholar]
- 7.Santini JT, Jr, Cima MJ, Langer R. A controlled-release microchip. Nature. 1999;397(6717):335–338. doi: 10.1038/16898. [DOI] [PubMed] [Google Scholar]
- 8.Santini J, Jr, Richards AC, Scheidt R, Cima MJ, Langer R. Microchips as controlled drug-delivery devices. Angew Chem Int Ed Engl. 2000;39(14):2396–2407. [PubMed] [Google Scholar]
- 9.McGirt MJ, et al. Gliadel (BCNU) wafer plus concomitant temozolomide therapy after primary resection of glioblastoma multiforme. J Neurosurg. 2009;110(3):583–588. doi: 10.3171/2008.5.17557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lechapt-Zalcman E, et al. O(6) -methylguanine-DNA methyltransferase (MGMT) promoter methylation and low MGMT-encoded protein expression as prognostic markers in glioblastoma patients treated with biodegradable carmustine wafer implants after initial surgery followed by radiotherapy with concomitant and adjuvant temozolomide. Cancer. 2012;118(18):4545–4554. doi: 10.1002/cncr.27441. [DOI] [PubMed] [Google Scholar]
- 11.Westphal M, et al. A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Gliadel wafers) in patients with primary malignant glioma. Neuro-oncol. 2003;5(2):79–88. doi: 10.1215/S1522-8517-02-00023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott AW, et al. Intracranial microcapsule drug delivery device for the treatment of an experimental gliosarcoma model. Biomaterials. 2011;32(10):2532–2539. doi: 10.1016/j.biomaterials.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 13.Ewend MG, Sampath P, Williams JA, Tyler BM, Brem H. Local delivery of chemotherapy prolongs survival in experimental brain metastases from breast carcinoma. Neurosurgery. 1998;43(5):1185–1193. doi: 10.1097/00006123-199811000-00093. [DOI] [PubMed] [Google Scholar]
- 14.Nussbaum ES, Djalilian HR, Cho KH, Hall WA. Brain metastases. Histology, multiplicity, surgery, and survival. Cancer. 1996;78(8):1781–1788. [PubMed] [Google Scholar]
- 15.Rusciano D, Burger MM. Mechanisms of metastases. In: Levine AJ, Schmidek HH, editors. Molecular Genetics of Nervous System Tumors. Wiley; New York: 1993. [Google Scholar]
- 16.Debinski W, Tatter SB. Convection-enhanced delivery for the treatment of brain tumors. Expert Rev Neurother. 2009;9(10):1519–1527. doi: 10.1586/ern.09.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bindal RK, Sawaya R, Leavens ME, Lee JJ. Surgical treatment of multiple brain metastases. J Neurosurg. 1993;79(2):210–216. doi: 10.3171/jns.1993.79.2.0210. [DOI] [PubMed] [Google Scholar]
- 18.Bindal AK, et al. Surgery versus radiosurgery in the treatment of brain metastasis. J Neurosurg. 1996;84(5):748–754. doi: 10.3171/jns.1996.84.5.0748. [DOI] [PubMed] [Google Scholar]
- 19.Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. Oncologist. 2007;12(7):884–898. doi: 10.1634/theoncologist.12-7-884. [DOI] [PubMed] [Google Scholar]
- 20.Patchell RA, et al. Radiosurgery plus whole-brain radiation therapy for brain metastases. JAMA. 2006;296(17):2089–2090. doi: 10.1001/jama.296.17.2089. [DOI] [PubMed] [Google Scholar]
- 21.Patchell RA, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500. doi: 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]
- 22.Pirzkall A, et al. Radiosurgery alone or in combination with whole-brain radiotherapy for brain metastases. J Clin Oncol. 1998;16(11):3563–3569. doi: 10.1200/JCO.1998.16.11.3563. [DOI] [PubMed] [Google Scholar]
- 23.Paek SH, Audu PB, Sperling MR, Cho J, Andrews DW. Reevaluation of surgery for the treatment of brain metastases: Review of 208 patients with single or multiple brain metastases treated at one institution with modern neurosurgical techniques. Neurosurgery. 2005;56(5):1021–1034. [PubMed] [Google Scholar]
- 24.Rosner D, Nemoto T, Lane WW. Chemotherapy induces regression of brain metastases in breast carcinoma. Cancer. 1986;58(4):832–839. doi: 10.1002/1097-0142(19860815)58:4<832::aid-cncr2820580404>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 25.Stark AM. Neurosurgical treatment of breast cancer metastases to the neurocranium. Patholog Res Int. 2010;2011(2010):549847. doi: 10.4061/2011/549847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang JE, Robins HI, Mehta MP. Therapeutic advances in the treatment of brain metastases. Clin Adv Hematol Oncol. 2007;5(1):54–64. [PubMed] [Google Scholar]
- 27.Abrey LE, et al. A phase II trial of temozolomide for patients with recurrent or progressive brain metastases. J Neurooncol. 2001;53(3):259–265. doi: 10.1023/a:1012226718323. [DOI] [PubMed] [Google Scholar]
- 28.Christodoulou C, et al. Hellenic Cooperative Oncology Group Phase II study of temozolomide in heavily pretreated cancer patients with brain metastases. Ann Oncol. 2001;12(2):249–254. doi: 10.1023/a:1008354323167. [DOI] [PubMed] [Google Scholar]
- 29.Laginha KM, Verwoert S, Charrois GJ, Allen TM. Determination of doxorubicin levels in whole tumor and tumor nuclei in murine breast cancer tumors. Clin Cancer Res. 2005;11(19 Pt 1):6944–6949. doi: 10.1158/1078-0432.CCR-05-0343. [DOI] [PubMed] [Google Scholar]
- 30.Ortho Biotech Products, LP 2007. DOXIL Product Information. Available at stage.doxil.com/shared/product/doxil/prescribing-information.pdf. Accessed April 19, 2007.
- 31.Mantha A, et al. A novel rat model for the study of intraosseous metastatic spine cancer. J Neurosurg Spine. 2005;2(3):303–307. doi: 10.3171/spi.2005.2.3.0303. [DOI] [PubMed] [Google Scholar]
- 32.Newlands ES, Stevens MF, Wedge SR, Wheelhouse RT, Brock C. Temozolomide: A review of its discovery, chemical properties, pre-clinical development and clinical trials. Cancer Treat Rev. 1997;23(1):35–61. doi: 10.1016/s0305-7372(97)90019-0. [DOI] [PubMed] [Google Scholar]
- 33.Strasser JF, Fung LK, Eller S, Grossman SA, Saltzman WM. Distribution of 1,3-bis(2-chloroethyl)-1-nitrosourea and tracers in the rabbit brain after interstitial delivery by biodegradable polymer implants. J Pharmacol Exp Ther. 1995;275(3):1647–1655. [PubMed] [Google Scholar]
- 34.Fung LK, et al. Pharmacokinetics of interstitial delivery of carmustine, 4-hydroperoxycyclophosphamide, and paclitaxel from a biodegradable polymer implant in the monkey brain. Cancer Res. 1998;58(4):672–684. [PubMed] [Google Scholar]
- 35.Ewend MG, et al. Local delivery of chemotherapy and concurrent external beam radiotherapy prolongs survival in metastatic brain tumor models. Cancer Res. 1996;56(22):5217–5223. [PubMed] [Google Scholar]