Abstract
Background & Aims:
Video-guided laryngoscopy, though unproven in achieving better success rates of laryngoscopy outcome and intubation, seems to provide better glottic visualization compared with direct laryngoscopy. The objective of this study was to compare the efficacy of video-guided laryngoscope (VGL) in the airway management skills of medical students.
Materials and Methods:
Medical students throughout their anesthesiology rotations were enrolled in this study. All students received standard training in the airway management during their course and were randomly allocated into two 20 person groups. In Group D, airway management was performed by direct laryngoscopy via Macintosh blade and in Group G intubation was performed via VGL. Time to intubation, number of laryngoscopy attempts and success rate were noted. Successful intubation was considered as the primary outcome.
Statistical Analysis:
All data were analyzed using SPSS 16 software. Chi-square and Fisher's exact test were used for analysis of categorical variables. For analyzing continuous variables independent t-test was used. P < 0.05 was considered as statistically significant.
Results:
Number of laryngoscopy attempts was less in Group G in comparison to Group D; this, however, was statistically insignificant (P: 0.18). Time to intubation was significantly less in Group G as compared to Group D (P: 0.02). Successful intubation in Group G was less frequently when compared to Group D (P: 0.66). Need for attending intervention, esophageal intubation and hypoxemic events during laryngoscopy were less in Group G; this, however, was statistically insignificant.
Conclusions:
The use of video-guided laryngoscopy improved the first attempt success rate, time to intubation, laryngoscopy attempts and airway management ability of medical students compared to direct laryngoscopy.
Keywords: Airway management, education, medical students, video-guided laryngoscope
Introduction
Airway management has always been a priority for the physicians of all eras.[1] Every physician must have skill for appropriate airway management. Difficult laryngoscopy has been reported to occur in 6-10% of intubations.[2,3] Consequently, every intervention which could improve successful intubation may be warranted in these situations.[4] There has been much research for development of new devices, which were designed for difficult airway management. Video-guided laryngoscope (VGL) is a device for airway management which is designed to allow a good exposure of glottis without aligning oral, pharyngeal and tracheal axes.[5] It increases first attempt success rate for endotracheal intubation.[6,7,8,9] Several studies have demonstrated its glottic exposure to be equal or better than direct laryngoscopy[10,11,12] most of which agree that future trials are required to show the exact efficacy of VGL in difficult airway management.[13,14] It is yet unclear whether use of glidescope results in improved glottic exposure and consequent increased intubation success in comparison to the use of conventional direct laryngoscopy.[15,16]
Our training program for medical students for airway management traditionally focused on direct laryngoscopy as the primary intervention until 2011 when we started using VGL in our airway management practice for medical students. We hypothesized that airway management and intubation with VGL has more success rate than direct laryngoscopy and based on this hypothesis we performed this study to evaluate the efficacy of VGL in intubation skills of medical students.
Materials and Methods
After approval of our local ethics committee, this study was performed from September 2012 to September 2013. Written informed consent was obtained from all patients during the study. Inclusion criteria were adult patients aged 18-55 years old and American Society of Anesthesiologists physical Status of 1 and 2 who were scheduled to undergo elective surgeries. All patients had Mallampati Class 1 or 2. Intubation was performed by medical students who had already passed the required airway management course. Exclusion criteria were anatomical and dental disorders and patients at the risk of increased intracranial pressure. Medical students who were transferred from other universities or had airway management education prior to the study period were enrolled in this study. All students received standard training in the airway management during their course. Anesthesiology education rotation for our university students is a 4 weeks course. During the 1st week, theoretical course on anatomy and physiology of airway, bag/mask ventilation, difficult airway management and preoperative airway evaluation was performed for medical students and later, students conducted airway management and intubation with the assistance of an attending anesthesiologist. Each student had to perform 50 intubations before entering the study. During this period, medical students were randomly allocated into two 20 person groups based on previous studies.[17] In Group D, airway management was performed by direct laryngoscopy using Macintosh blade and in Group G, intubation was performed using VGL. Throughout the study, intubation was performed by medical students under supervision of an attending anesthesiologist. All patients were premedicated with 1 mg midazolam before induction of anesthesia. Monitoring consisted of capnography, noninvasive blood pressure monitoring, electrocardiography, and pulse oximetry. Premedication was performed with fentanyl 2 μg/kg and induction of anesthesia was performed with propofol 2 mg/kg, atracurium 0.5 mg/kg, lidocaine 1 mg/kg. The glidescope blade size selected was similar to the Macintosh blade size.
Data collection
For all intubations, time to intubation, number of laryngoscopy attempts and success rate were noted. In addition, number of attending interventions and complications were noted. Time to intubation was measured from the time device entered the mouth until the detection of end tidal CO2. If >1 attempt was required, the patient received mask ventilation between the attempts. Time to intubation included the time between the attempts. Failed intubation was defined as three unsuccessful attempts for intubation. Successful intubation was considered as the primary outcome. All data were analyzed using SPSS 16 software SPSS Inc., 233 South Wacker Drive, 11th Floor, Chicago, IL 60606-6412. Patent No. 7,023,453. Chi-square and Fisher's exact test were used for analysis of categorical variables. For analyzing continuous variables independent t-test was used. P < 0.05 was considered as statistically significant.
Results
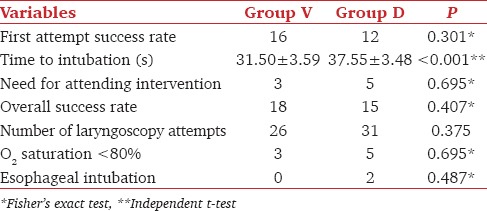
No significant difference could be observed between two groups regarding demographic characteristics [Table 1]. Mallampati Grades 1 and 2 were observed in 31 and 9 patients, respectively. Successful and failed intubation occurred in 34 (85%) and 6 (15%) patients, respectively. Laryngoscopy was less attempted in Group G in comparison to Group D; however, the difference was not statistically significant (P = 0.18). Time to intubation was significantly less in Group G compared to Group D (P = 0.02). Successful intubation was observed less frequently in Group G as compared to Group D (P = 0.66). Attending intervention, esophageal intubation and hypoxemic events during laryngoscopy were less frequent in Group G; however, the difference was not statistically significant [Table 2].
Table 1.
Demographic characteristics of patients
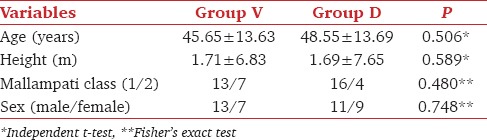
Table 2.
Assessed variables during study
Discussion
Results obtained from this study showed that VGL was associated with less intubation time, fewer numbers of laryngoscopy attempts and increased successful intubation rate compared to direct laryngoscopy. These results are mostly due to the improved glottic visualization which is similar to the previous studies.[18,19] Considering this fact, the importance of difficult airway management[20,21] and VGL not requiring alignment of oral, tracheal and pharyngeal axes,[5,22] clinicians usually use VGL when difficulty with endotracheal intubation is anticipated.[23] One of the most important results obtained from our study is the decrease in laryngoscopy attempts with VGL which might be due to medical students being inexpert operators in performing laryngoscopy; similar previous studies also mentioned that there is no benefit in airway management using VGL by skilled operators.[18] Kory et al. suggest that VGL should be used as the primary device when urgent intubations are performed by less experienced operators.[24] As first successful attempt might be of more value in the airway management of infants and multiple attempts endanger these patients, Kaufmann et al. in their study, recommended VGL as a suitable approach in airway management in younger children.[25] Our study showed that esophageal intubation and hypoxemia during intubation was less in VGL group. Although this difference was not statistically significant, it was clinically important and might have been statistically significant with larger sample sizes. As there were some studies suggesting difficult or failed intubation in association with VGL due to problems related to positioning the tube in the trachea despite a good glottic view,[10,26] we used intubation time and other rates of successful intubation, which were better in VGL, yet statistically insignificant. Less intubation time in VGL group in this study might be due to unskilled operators, as skilled operators usually perform direct laryngoscopy faster. Educational courses throughout the anesthesiology curriculums are reported to be associated with desirable educational outcomes.[27,28]
Each intervention, which could improve the success rate of airway management, especially in unskilled persons is of great value for future studies. No important complication was reported in association with VGL in this study; however, there are few reports on its complications including perforation of palatopharyngeal arch.[14] Therefore, everyone should take precautionary measurements, while using this device for airway management especially in emergency situations.
Our study was a single-centered study with 40 persons; therefore, future studies with larger sample sizes comparing the skilled with unskilled persons for laryngoscopy is recommended. Another limitation of study was the possibility that medical students had different skills or training levels between direct laryngoscopy and VGL. However, we suppose this is variation would be less as they all received the same education with the same attending professors during their study course. However a study determining the same outcome measures using a structured curriculum of training in both groups would be helpful in overcoming these variations. We believe that the change in complication rates between both groups was related to the changes from the Direct Laryngoscopy to the VGL, as other variables were constant. Furthermore, it was impossible to blind intubators to study group assignment.
In summary, VGL can be used as an appropriate device for airway management in anticipated difficult airway or following failed direct laryngoscopy.
Acknowledgment
The authors would like to thank all those who helped throughout the different stages of this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Golzari SE, Khan ZH, Ghabili K, Hosseinzadeh H, Soleimanpour H, Azarfarin R, et al. Contributions of medieval Islamic physicians to the history of tracheostomy. Anesth Analg. 2013;116:1123–32. doi: 10.1213/ANE.0b013e3182884313. [DOI] [PubMed] [Google Scholar]
- 2.Ezri T, Weisenberg M, Khazin V, Zabeeda D, Sasson L, Shachner A, et al. Difficult laryngoscopy: Incidence and predictors in patients undergoing coronary artery bypass surgery versus general surgery patients. J Cardiothorac Vasc Anesth. 2003;17:321–4. doi: 10.1016/s1053-0770(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 3.el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–204. doi: 10.1097/00000539-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Parish M, Panahi JR, Afhami MR, Pour AM. Role for the second anesthesiologist in failed intubations. Anesth Analg. 2006;102:971. doi: 10.1213/01.ANE.0000190879.76048.2D. [DOI] [PubMed] [Google Scholar]
- 5.Kim JT, Na HS, Bae JY, Kim DW, Kim HS, Kim CS, et al. GlideScope video laryngoscope: A randomized clinical trial in 203 paediatric patients. Br J Anaesth. 2008;101:531–4. doi: 10.1093/bja/aen234. [DOI] [PubMed] [Google Scholar]
- 6.Hirabayashi Y, Otsuka Y, Seo N. GlideScope videolaryngoscope reduces the incidence of erroneous esophageal intubation by novice laryngoscopists. J Anesth. 2010;24:303–5. doi: 10.1007/s00540-010-0872-y. [DOI] [PubMed] [Google Scholar]
- 7.Hsiao WT, Lin YH, Wu HS, Chen CL. Does a new videolaryngoscope (glidescope) provide better glottic exposure? Acta Anaesthesiol Taiwan. 2005;43:147–51. [PubMed] [Google Scholar]
- 8.Malik MA, Subramaniam R, Maharaj CH, Harte BH, Laffey JG. Randomized controlled trial of the Pentax AWS, Glidescope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–8. doi: 10.1093/bja/aep266. [DOI] [PubMed] [Google Scholar]
- 9.Narang AT, Oldeg PF, Medzon R, Mahmood AR, Spector JA, Robinett DA. Comparison of intubation success of video laryngoscopy versus direct laryngoscopy in the difficult airway using high-fidelity simulation. Simul Healthc. 2009;4:160–5. doi: 10.1097/SIH.0b013e318197d2e5. [DOI] [PubMed] [Google Scholar]
- 10.Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–8. doi: 10.1007/BF03027728. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan MB, Hagberg CA, Ward DS, Brambrink A, Chhibber AK, Heidegger T, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–62. doi: 10.1016/j.jclinane.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope video laryngoscope: Randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–4. doi: 10.1093/bja/aei041. [DOI] [PubMed] [Google Scholar]
- 13.Rai MR, Dering A, Verghese C. The Glidescope system: A clinical assessment of performance. Anaesthesia. 2005;60:60–4. doi: 10.1111/j.1365-2044.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 14.Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007;54:54–7. doi: 10.1007/BF03021900. [DOI] [PubMed] [Google Scholar]
- 15.Nouruzi-Sedeh P, Schumann M, Groeben H. Laryngoscopy via Macintosh blade versus GlideScope: Success rate and time for endotracheal intubation in untrained medical personnel. Anesthesiology. 2009;110:32–7. doi: 10.1097/ALN.0b013e318190b6a7. [DOI] [PubMed] [Google Scholar]
- 16.Jones PM, Armstrong KP, Armstrong PM, Cherry RA, Harle CC, Hoogstra J, et al. A comparison of glidescope videolaryngoscopy to direct laryngoscopy for nasotracheal intubation. Anesth Analg. 2008;107:144–8. doi: 10.1213/ane.0b013e31816d15c9. [DOI] [PubMed] [Google Scholar]
- 17.Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: A fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910–5. doi: 10.1213/01.ane.0000166975.38649.27. [DOI] [PubMed] [Google Scholar]
- 18.Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can J Anaesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008;63:745–60. doi: 10.1111/j.1365-2044.2008.05489.x. [DOI] [PubMed] [Google Scholar]
- 20.Lai HY, Chen IH, Chen A, Hwang FY, Lee Y. The use of the GlideScope for tracheal intubation in patients with ankylosing spondylitis. Br J Anaesth. 2006;97:419–22. doi: 10.1093/bja/ael133. [DOI] [PubMed] [Google Scholar]
- 21.Lim TJ, Lim Y, Liu EH. Evaluation of ease of intubation with the GlideScope or Macintosh laryngoscope by anaesthetists in simulated easy and difficult laryngoscopy. Anaesthesia. 2005;60:180–3. doi: 10.1111/j.1365-2044.2004.04038.x. [DOI] [PubMed] [Google Scholar]
- 22.Agrò F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90:705–6. doi: 10.1093/bja/aeg560. [DOI] [PubMed] [Google Scholar]
- 23.Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: An analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41. doi: 10.1097/ALN.0b013e3182023eb7. [DOI] [PubMed] [Google Scholar]
- 24.Kory P, Guevarra K, Mathew JP, Hegde A, Mayo PH. The impact of video laryngoscopy use during urgent endotracheal intubation in the critically ill. Anesth Analg. 2013;117:144–9. doi: 10.1213/ANE.0b013e3182917f2a. [DOI] [PubMed] [Google Scholar]
- 25.Kaufmann J, Laschat M, Hellmich M, Wappler F. A randomized controlled comparison of the Bonfils fiberscope and the GlideScope Cobalt AVL video laryngoscope for visualization of the larynx and intubation of the trachea in infants and small children with normal airways. Paediatr Anaesth. 2013;23:913–9. doi: 10.1111/pan.12137. [DOI] [PubMed] [Google Scholar]
- 26.Serocki G, Bein B, Scholz J, Dörges V. Management of the predicted difficult airway: A comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol. 2010;27:24–30. doi: 10.1097/EJA.0b013e32832d328d. [DOI] [PubMed] [Google Scholar]
- 27.Soleimanpour H, Gholipouri C, Panahi JR, Afhami MR, Ghafouri RR, Golzari SE, et al. Role of anesthesiology curriculum in improving bag-mask ventilation and intubation success rates of emergency medicine residents: A prospective descriptive study. BMC Emerg Med. 2011;11:8. doi: 10.1186/1471-227X-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soleimanpour H, Shams Vahdati S, Mahmoodpoor A, Rahimi Panahi J, Afhami MR, Pouraghaei M, et al. Modified cricothyroidotomy in skill laboratory. J Cardiovasc Thorac Res. 2012;4:73–6. doi: 10.5681/jcvtr.2012.018. [DOI] [PMC free article] [PubMed] [Google Scholar]


