Abstract
Background and Aims:
Admission to an intensive care unit (ICU) is considered as an objective marker of severe maternal morbidity. The aim was to assess the incidence and possible risk factors of obstetric patient admissions in the multidisciplinary ICU of a tertiary care center with emphasis on standardized mortality ratio (SMR).
Material and Methods:
A retrospective five year ICU record analysis was done for all pregnant women, who were admitted to multidisciplinary ICU of a tertiary care hospital during June 2007-12.
Results:
During this 5-year period, 21,943 deliveries took place and 164 women required ICU admission. Out of these, the data of 151 patients were analyzed. Maternal mortality rate was 31.1% (47 deaths) for patients admitted to ICU. The simplified acute physiologic score (SAPS) II was 62 (55-68) in nonsurvivor versus 34.00 (28-46) in survivor group (P value < 0.001). The receiver operated characteristic curve was plotted using SAPS II scores and the area under the curve was 0.93 with 95% confidence interval (0.89-0.96). The calculated SMR was 0.97.
Conclusions:
Women admitted to ICU with diagnosis of puerperal sepsis and intrauterine death (IUD) with coexisting sepsis had higher mortality as compared to women with hypertensive disease of pregnancy and hemorrhage. The calculated SMR was less than one which is a predictor of good ICU care.
Keywords: Developing countries, ICU, IUD, obstetric, obstetric hemorrhage, preeclampsia, pregnancy, puerperal sepsis, SAPS II
Introduction
Developing countries account for 99% of global maternal deaths. According to the data of world health organization 2010, the incidence of global maternal mortality ratio (MMR) was 210 maternal deaths per 100,000 live births. India accounts for 19% (56,000) of global maternal deaths. Despite some progress in providing improved healthcare to pregnant women in the last decade an alarmingly high MMR still remains a challenge in developing countries. The major causes of pregnancy-related complications are severe bleeding after childbirth, infections, pregnancy-induced hypertension, and unsafe abortion.[1,2,3,4,5] The incidence of pregnant women admitted to intensive care unit (ICU) in developed countries is 2-4 per 1,000 deliveries as compared with 2-13.5 per 1,000 deliveries in developing countries.[6]
Admission of pregnant women to an ICU is considered as an objective marker of severe maternal morbidity.[7] The present study was conducted to identify the causes and possible risk factors of obstetric patient admission to ICU of a tertiary care center with emphasis on standardized mortality ratio (SMR).
Materials and Methods
After institutional approval, a retrospective record analysis of all obstetric admissions during 5-year period from June 2007- to 2012 was done. The tertiary care hospital is a 650-bedded facility with a multidisciplinary closed 14-bedded ICU and is managed by a team of two anesthesia consultants, five ICU residents, attending obstetric consultant, and a senior/junior obstetric resident. The nurse:patient ratio is 1:2.
The ICU records of all pregnant women or women admitted within 6 weeks of delivery admitted to the multidisciplinary ICU over this period were evaluated. The variables included were age, diagnosis, antepartum, or postpartum admission, time from onset of symptoms from other health facilities and transfer to hospital, time taken after admission of patient in hospital and her transfer to ICU, blood transfusions, inotropes, intrauterine death (IUD), method of delivery on admission (cesarean or normal vaginal delivery), hysterectomy, and medical or obstetric disorders developing during pregnancy. On admission to ICU simplified acute physiologic score (SAPS) II was calculated for assessment of severity of illness and for predicted mortality rate.[8] The receiver operated characteristic (ROC) curve was plotted for different SAPS II score points and cut off was obtained which predicted the sensitivity and specificity. The SMR was calculated using ratio of actual mortality/predicted mortality.
The acute reasons for ICU admission were classified into obstetric, if admission in ICU was a direct consequence of the pregnant or postpartum state (e.g., preeclampsia, postpartum hemorrhage), and medical, if it could have occurred due nonobstetric causes (e.g., community-acquired pneumonia, rheumatic heart disease). Chronic medical disorders that preceded the pregnancy were also recorded. Organ dysfunctions on admission were assessed for individual organs. The assessment for respiratory dysfunction was done using the criteria of PaO2 <60 mmHg on FiO2 of 0.21 or need for ventilator support or both. Hemodynamic instability was defined as systolic blood pressure (SBP) <90 mm Hg even after fluid resuscitation and central venous pressure of 8-12 cm H2O or continuous infusion of inotrope agents to maintain SBP >90 mm Hg or both. Patients with heart diseases were managed according to the echocardiography findings. Renal dysfunction was defined as presence of one or more than one of the following criteria: Serum creatinine >300 μmol/L, urine output <500 mL/24 h or 180 mL/8 h or need for hemodialysis or peritoneal dialysis. Neurological dysfunction was defined as presence of Glasgow coma scale <6 (absence of sedation at any one point in day) or sudden onset of confusion or psychosis or both. Hepatic dysfunction was defined as presence of either serum bilirubin >100 μmol/L or serum alkaline phosphatase >3 × normal or both. Coagulation dysfunction was defined in the presence of platelet count <40 000/mm3 or presence of increased (>1.5 times normal) prothrombin time or partial thromboplastin time or in combination. IUD was defined as fetal death at admission. Uterine and pelvic infection occurring prior to delivery was considered as chorioamnionitis, whereas that occurring after delivery or abortion was considered as puerperal sepsis. Outcome measures included days of mechanical ventilation, packed red cell transfusion, inotropes, length of ICU stay, maternal survival, and total length of hospital stay.
The collected data were analyzed using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 15.0 for Windows). Parametric data were represented as mean and standard deviations, nonparametric data as median and interquartrile range (IQR) and categorical data were presented as percentage. Student's t-test was used for demographic data; Mann-Whitney U-test was used for SAPS II score, predicted mortality, ventilator days, length of ICU stay, and length of hospital stay. Chi-square test or Fisher's exact test was used for use of inotropes, mode of delivery, duration of admission to hospital, and transfer to ICU <24 h which ever was applicable according to the type of data. P value of < 0.05 was considered statistically significant.
Results
During the 5-year study period (June 2007-12), 164 pregnant women were admitted to ICU, out of these four patients had readmissions and data of nine patients could not be retrieved. We analyzed data of 151 patients which was 6.0% of all obstetric admissions to our ICU. During this period, 21,943 deliveries took place at our hospital and out of 151 obstetric ICU patients; seven patients had noninstitutional delivery. The mean age of the patients admitted to ICU was 25.3 ± 4.2 years with mean gestational age of 33 weeks; 12 (7.9%) patients were admitted antepartum, while majority of them 139 (92.1%) were admitted to ICU in the postpartum period. Out of all admissions, 82 (54.3%) women were primigravida. Maternal deaths occurred in 31.1% (47 deaths) of all obstetric patients admitted to ICU and out of these five patients had delivered outside resulting in calculated MMR of 191 per 100,000 deliveries. Fetal mortality rate was 21.19% (32 fetal deaths). The mean length of ICU stay for 151 patients was 5.0 days (IQR, 3-9.75 days) [Table 1].
Table 1.
Variables of 151 obstetric patients admitted to intensive care unit of a tertiary care hospital during 5-year-period
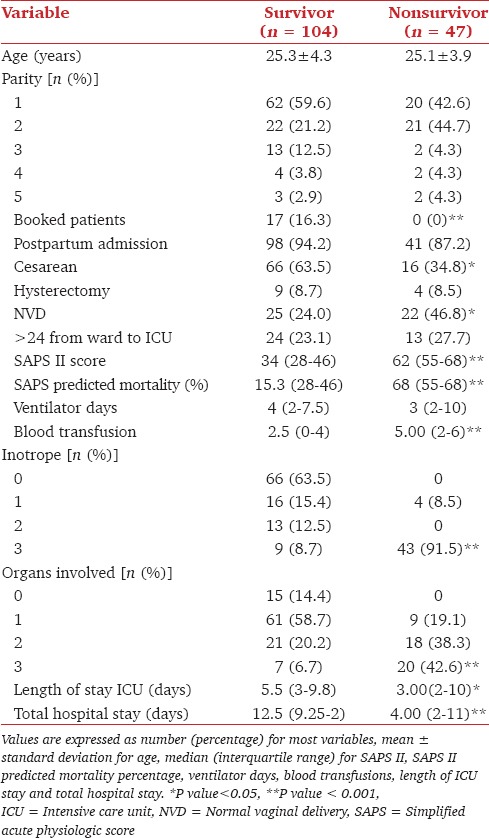
Patients were further divided into two groups: Survivor (n = 104) and nonsurvivor (n = 47) groups. Mean age of women was comparable in both the groups. Unbooked patients, women who delivered vaginally prior to ICU and/or hospital admission had higher mortality (P < 0.05), while patients who had undergone caesarean delivery prior to ICU admission had better survival rate (P value < 0.001).
SAPS II score was 62 (55-68) versus 34.00 (28-46) in nonsurvivor and survivor women, respectively (P value < 0.001). The predicted mortality percentage was 68 (55-68) in nonsurvivors and 15.30 (28-46) in survivor group (P value < 0.0001). We plotted the ROC curve using SAPS II scores. The area under the ROC curve was 0.93, with 95% confidence interval (0.89-0.96) which again shows a good fit [Figure 1]. The best cut off on ROC curve was 44 with 100.00% sensitivity and 60.00% specificity. The predicted mortality was 48 and the calculated SMR was 0.97.
Figure 1.
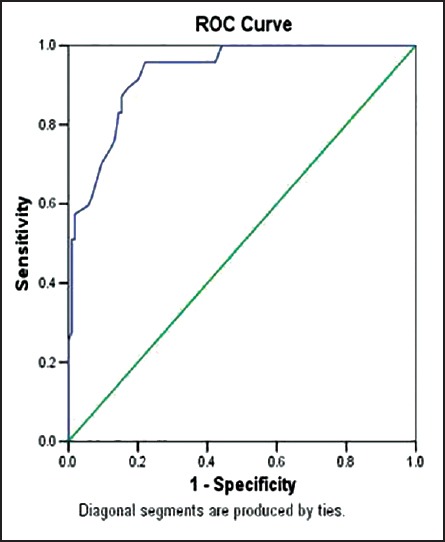
Receiver operated curve plotted using simplified acute physiologic score II scores of 151 obstetric patients admitted in intensive care unit of a tertiary care hospital over 5-year-period
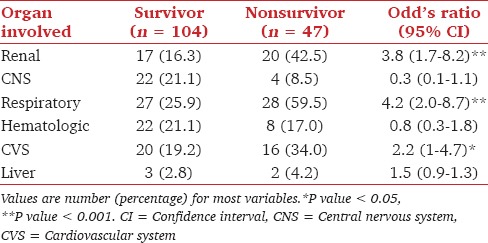
On comparing the nonsurvivor group with survivor group [Table 1], a higher number of patients had multiorgan involvement and were receiving inotropes on admission to ICU (P <0.001). A detailed analysis of individual organ system failure revealed that failure of respiratory, renal, and cardiovascular were associated with high mortality rate (P value <0.05) [Table 2].
Table 2.
Organ involvement on admission in 151 obstetric patients admitted to intensive care unit of a tertiary care hospital during 5-year-period
A few patients had more than one diagnosis on admission, hence; the indications of patient's admission in each group were higher than the number of admissions [Table 3]. Patients with puerperal sepsis and IUD with coexisting sepsis (P < 0.001) had higher mortality. In subgroup analysis of nonsurvivor group, 23 women had puerperal sepsis, out of these 10 patients had coexisting multiorgan dysfunction syndrome (MODS), seven patients had acute respiratory syndrome (ARDS), three patients had acute renal failure (ARF) and five patients were admitted following noninstitutional delivery. There were 12 women in the nonsurvivor group admitted with IUD with sepsis and coexisting involvement of MODS in three patients, ARF in three patients, ARDS in two patients, encephalitis in one patient, intracerebral bleed in one patient, bleeding diathesis in one patient, and severe anaemia in one patient on admission.
Table 3.
Chronic and acute disorders in 151 obstetric patients admitted to intensive care unit of a tertiary care hospital during 5-year period (2007-2012)
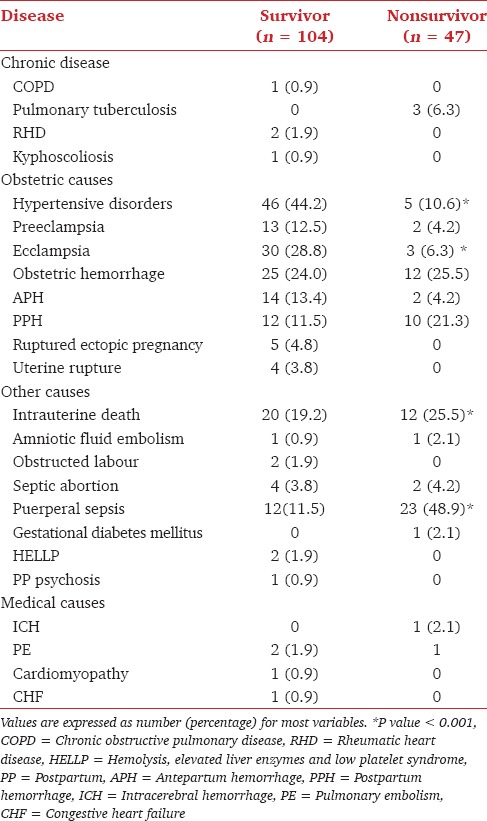
The obstetric patients who did not survive in ICU were further analyzed according to acute illness. Out of all 151 obstetric patients’ admitted to ICU, 47 patients did not survive, out of these 10 patients (6.62%) had medical disorders and 37 patients (24.50%) had obstetric cause of admission to ICU.
Discussion
The present study is one of the few studies in recent years that have analyzed obstetric patients admissions to ICU over a 5 years span.[6,9,10,11,12,13] During this period, 151 obstetric patients were admitted to the ICU (seven had noninstitutional delivery) with an incidence of 6.5 per 1000 deliveries which was higher as compared to recently published studies from developing countries [Table 4].[6,9,10,11,12,13,14,15,16] Only 17(16.34%) patients of survivor group received antenatal care which was an important factor for pregnant patients who survived.[11,13,14,15,16]
Table 4.
A comparison of present study with studies reporting intensive care unit admissions for pregnant and postpartum women
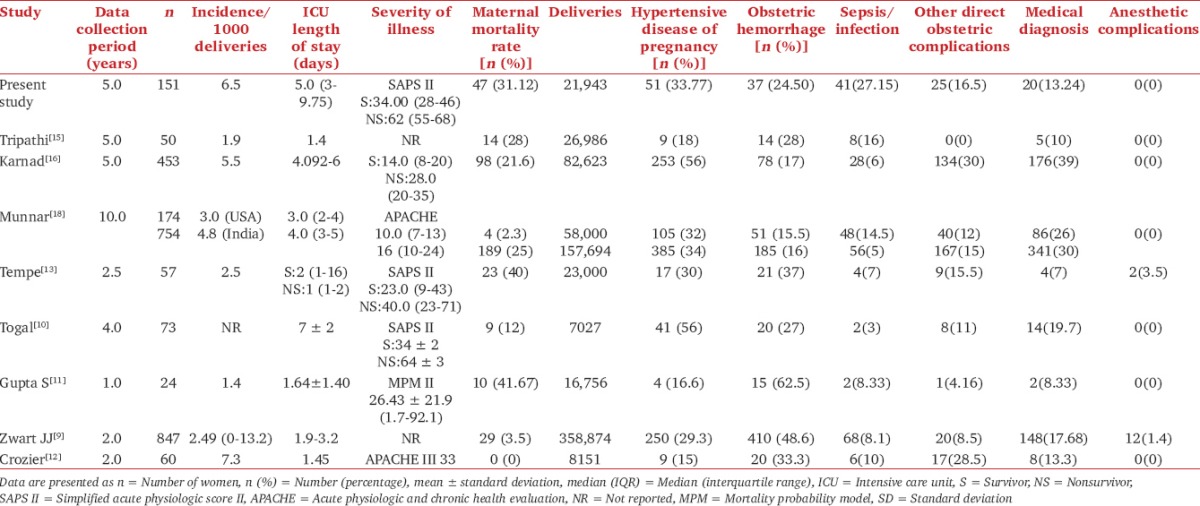
The length of ICU stay in present study was comparable with most of the recently published studies [Table 4]. In an earlier study, Tempe et al., reported shorter ICU stay but observed higher mortality rate,[13] indicating that the patients were unstable. In the present study, the time interval between the hospital admissions to ICU admission was lesser than 24 h in majority of patients, hence, depicting good care in hospital and priority of admission of obstetric patients in ICU.
SAPS II score was used for ICU scoring on admission as it provides estimate of risk of death without having to specify a primary diagnosis. Our patients on admission had SAPS II score of 34.00 (28-46) in survivor group and 62 (55-68) in the nonsurvivor group. This was higher as compared to Tempe et al.,[13] but were comparable with patients studied by Togal et al.[10] SAPS II score system accurately predicted data of ICU admissions with almost 100% sensitivity as the average SAPS II score was 44.56 ± 16.88. This was probably because SAPS II score underestimated mortality at low score and accurately predicted mortality with higher score. In an earlier study, no improvement was observed after modification of standard severity of illness scores of SAPS II and acute physiologic and chronic health evaluation (APACHE) II according to altered maternal physiology in pregnancy rather, APACHE II was observed to overestimate mortality and SAPS II was found to be a good discriminator of illness severity.[17] Crozier and Wallace[12] used APACHE III score and suggested that the APACHE III scoring system is not validated for obstetric population. The mortality predicting scores like APACHE II/III are not as reliable in obstetric patients; however, the SAPS II score does seem to have some degree of validity in obstetric ICU.[13] Hence, we preferred SAPS II over APACHE II and III.
We plotted the ROC curve which showed a good fit, emphasizing good validation of SAPS II score with ICU obstetric population. The calculated SMR value was <1 in the present study which indicated good ICU care.
Majority of women admitted to ICU were postpartum and are comparable with the published literature.[9,10,16,17] The common indications of ICU admissions were hypertensive disease of pregnancy 51 (33.77%), sepsis 41 (27.15%), and hemorrhage during pregnancy 37 (24.50%). However, ICU admission of 41 (27.15%) women with puerperal sepsis and/or infection on admission with coexisting conditions was much higher than the recent studies from developed and developing countries [Table 4].[6,9,10,11,12,13,14,15,16,18] There were 47 maternal deaths (31.1%) which was comparable with the data from developing countries. We observed a higher mortality in patients who were admitted in ICU with sepsis as ours is a tertiary care center hence, patients that were admitted were referred and not booked. Such patients had higher SAPS II score at the time of admission probably due to lack of protocoled care for sepsis in non institutional setups. Low socioeconomic status, suboptimal medical care, lack of education, and myths regarding antenatal check up may contribute to increased maternal morbidity and mortality in developing countries.[18,19] The present study had limitations in being retrospective, and hence, intellectual and socioeconomic aspects could not be evaluated.
In a recently published study, hemorrhage was the commonest cause of death (52.5%), followed by sepsis (13.75%) and pregnancy-induced hypertension (10%).[20] Sepsis is now a major preventable cause of maternal mortality and morbidity worldwide.[21] Under reporting of sepsis undermines its role in maternal mortality.[22] There is an urgent need of measures for early detection, effective treatment strategies, protocol based management of sepsis, and data reporting in our country.
In the near future, sepsis may become a major cause of maternal mortality in developing countries and even surpass hypertensive disease of pregnancy and obstetric hemorrhage if adequate measures are not taken. Measures regarding maternal awareness, curbing suboptimal medical care, and early referral is required to safeguard these women who are otherwise healthy individuals. Multicentric prospective studies in this regard are required to further validate the findings of our study and also provide more authenticated data for formulating evidence-based national guidelines.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.UN Population Fund (UNFPA), World Health Organization, UN Children's Fund and the World Bank (2012) Maternal Deaths Halved in 20 Years, but Faster Progress Needed. [Last accessed on 2012 Nov 7]. Available from http://www.unfpa.org/public/home/news/pid/10730 .
- 2.Lassi ZS, Haider BA, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and improving neonatal outcomes. Cochrane Database Syst Rev. 2010:CD007754. doi: 10.1002/14651858.CD007754.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Ensor T, Cooper S. Overcoming barriers to health service access: Influencing the demand side. Health Policy Plan. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 4.Singh P, Pandey A, Aggarwal A. House-to-house survey vs. snowball technique for capturing maternal deaths in India: A search for cost-effective method. Indian J Med Res. 2007;125:550–6. [PubMed] [Google Scholar]
- 5.Bhardwaj N, Hasan SB, Zaheer M. Maternal care receptivity and its relation to perinatal and neonatal mortality. A rural study. Indian Pediatr. 1995;32:416–23. [PubMed] [Google Scholar]
- 6.Pollock W, Rose L, Dennis CL. Pregnant and postpartum admissions to the intensive care unit: A systematic review. Intensive Care Med. 2010;36:1465–74. doi: 10.1007/s00134-010-1951-0. [DOI] [PubMed] [Google Scholar]
- 7.Gilbert TT, Smulian JC, Martin AA, Ananth CV, Scorza W, Scardella AT Critical Care Obstetric Team. Obstetric admissions to the intensive care unit: Outcomes and severity of illness. Obstet Gynecol. 2003;102:897–903. doi: 10.1016/s0029-7844(03)00767-1. [DOI] [PubMed] [Google Scholar]
- 8.Aegerter P, Boumendil A, Retbi A, Minvielle E, Dervaux B, Guidet B. SAPS II revisited. Intensive Care Med. 2005;31:416–23. doi: 10.1007/s00134-005-2557-9. [DOI] [PubMed] [Google Scholar]
- 9.Zwart JJ, Dupuis JR, Richters A, Ory F, van Roosmalen J. Obstetric intensive care unit admission: A 2-year nationwide population-based cohort study. Intensive Care Med. 2010;36:256–63. doi: 10.1007/s00134-009-1707-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Togal T, Yucel N, Gedik E, Gulhas N, Toprak HI, Ersoy MO. Obstetric admissions to the intensive care unit in a tertiary referral hospital. J Crit Care. 2010;25:628–33. doi: 10.1016/j.jcrc.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S, Naithani U, Doshi V, Bhargava V, Vijay BS. Obstetric critical care: A prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian J Anaesth. 2011;55:146–53. doi: 10.4103/0019-5049.79895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crozier TM, Wallace EM. Obstetric admissions to an integrated general intensive care unit in a quaternary maternity facility. Aust N Z J Obstet Gynaecol. 2011;51:233–8. doi: 10.1111/j.1479-828X.2011.01303.x. [DOI] [PubMed] [Google Scholar]
- 13.Tempe A, Wadhwa L, Gupta S, Bansal S, Satyanarayana L. Prediction of mortality and morbidity by simplified acute physiology score II in obstetric intensive care unit admissions. Indian J Med Sci. 2007;61:179–85. [PubMed] [Google Scholar]
- 14.Olarra J, Longarela AM, Suarez L, Palacio FJ. Critically ill obstetric patients treated in an ICU. Chest. 2002;121:2077. doi: 10.1378/chest.121.6.2077. [DOI] [PubMed] [Google Scholar]
- 15.Tripathi R, Rathore AM, Saran S. Intensive care for critically ill obstetric patients. Int J Gynaecol Obstet. 2000;68:257–8. doi: 10.1016/s0020-7292(99)00200-3. [DOI] [PubMed] [Google Scholar]
- 16.Karnad DR, Lapsia V, Krishnan A, Salvi VS. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med. 2004;32:1294–9. doi: 10.1097/01.ccm.0000128549.72276.00. [DOI] [PubMed] [Google Scholar]
- 17.Lapinsky SE, Hallett D, Collop N, Drover J, Lavercombe P, Leeman M, et al. Evaluation of standard and modified severity of illness scores in the obstetric patient. J Crit Care. 2011;26:535.e1–7. doi: 10.1016/j.jcrc.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Munnar U, Karnad DR, Bandi VD, Lapsia V, Suresh MS, Ramshesh P, et al. Critically ill obstetrics patients in an American and an Indian public hospital: Comparison of case-mix, organ dysfunction, intensive care requirements, and outcomes. Intensive Care Med. 2005;31:1087–94. doi: 10.1007/s00134-005-2710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martey JO, Djan JO, Twum S, Browne EN, Opoku SA. Maternal mortality and related factors in Ejisu District, Ghana. East Afr Med J. 1994;71:656–60. [PubMed] [Google Scholar]
- 20.Khumanthem PD, Chanam MS, Samjetshabam RD. Maternal mortality and its causes in a tertiary center. J Obstet Gynecol India. 2012;62:168–71. doi: 10.1007/s13224-012-0169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bamfo JE. Managing the risks of sepsis in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2013;27:583–95. doi: 10.1016/j.bpobgyn.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Acosta CD, Knight M. Sepsis and maternal mortality. Curr Opin Obstet Gynecol. 2013;25:109–16. doi: 10.1097/GCO.0b013e32835e0e82. [DOI] [PubMed] [Google Scholar]


