Abstract
Background and Aims:
Critical illness may complicate any pregnancy. Timely intensive care management of critically ill obstetric patients has better outcomes than expected from the initial severity of illness. The aim was to study the indications of transfer of post-cesarean section patients to post-anesthesia intensive care unit (PACU). (PACU transfer indicated that the patient required intensive care).
Materials and Methods:
This was a prospective observational study carried out in the PACU of a tertiary care teaching public hospital over a period of 2 years. Sixty-one postoperative lower segment cesarean section (LSCS) females admitted consecutively in PACU were studied. The study included obstetric PACU utilization rate, intensive care unit interventions, outcome of mother, Acute Physiology and Chronic Health Evaluation (APACHE II) score, and its correlation with mortality.
Results:
Postanesthesia intensive care unit admission rate was 2.8% and obstetric PACU utilization rate was 3.22%. Of 61 patients, four had expired. Obstetric indications (67.2%) were the most common cause of admission to PACU. Among the obstetric indications hemorrhage (36.1%) was found to be a statistically significant indication for PACU admission followed by hypertensive disorder of pregnancy (29.5%). Cardiovascular disease (16.4%) was the most common nonobstetric indication for PACU transfer and was associated with high mortality. The observed mortality was 6.557%, which was lower than predicted mortality by APACHE II Score.
Conclusion:
Obstetric hemorrhage, hypertensive disorders of pregnancy and cardiovascular diseases are the leading causes of PACU admission in post LSCS patients. Prompt provision of intensive care to critically ill obstetric patients can lead to a significant drop in maternal morbidity and mortality.
Keywords: Acute Physiology and Chronic Health Evaluation II, caesarean section, postanesthesia intensive care unit
Introduction
According to World Health Organization “There is a story behind every maternal death and life-threatening complication.” Understanding the lessons to be learnt can help to avoid such outcomes.[1] The pregnant woman is usually young and in good health before she becomes critically ill; hence, her prognosis will be better if she receives timely intensive care intervention. Obstetric patients requiring intensive care unit (ICU) admission may reflect near-miss maternal mortality and is now considered as maternal morbidity.[2,3,4] Maternal near-miss case is defined as “a woman who nearly died but survived a complication that occurred during pregnancy, childbirth, or within 42 days of termination of pregnancy.”[4] Maternal mortality rates are improving worldwide hence attention is switching to morbidity and as a marker of this obstetrics admission to ICU is scrutinized.[3,4] As ICU utilization rates are increasing worldwide separate intensive care units have been developed for cardiac, burns, respiratory, neurosurgery, pediatric, and neonatal care, but an ICU only for obstetric patients is not yet widely available in our country.[2] General illness severity scores are widely used in the ICU to characterize disease severity and degree of organ dysfunction, predict outcome and assess resource use. All the scores were developed to be used in mixed groups of ICU patients and their accuracy in subgroups of patients can be questioned. Acute Physiology and Chronic Health Evaluation (APACHE II), the world's most widely used severity of illness score is best fit for obstetric patients and has better calibration.[5]
With this background, we aimed to prospectively study the indications of transfer of post lower segment caesarean section (LSCS) patients to postanesthesia intensive care unit (PACU). Our secondary objective was to analyze all, consecutive critically ill obstetric patients admitted to PACU after LSCS with respect to the obstetric PACU utilization rate, their clinical course, treatment, ICU interventions, prediction of maternal mortality by APACHE II score, and outcome of mother.
Materials and Methods
This study was conducted in the PACU attached to a tertiary care teaching public hospital during the period January 1, 2011 to December 31, 2012. Study protocol was approved by institutional ethics committee. PACU is well-equipped with 10 ICU beds located near operation theatre complex where postoperative patients from all surgical specialties who need intensive care management are admitted and is not exclusive for obstetrics. PACU is postanesthesia/postoperative ICU; only patients needing Intensive care management in the postoperative period are admitted to PACU, while all other postoperative patients are observed in the recovery room outside each operation theatre. Apart from PACU separate ICUs are available for neonate, cardiac, medical and trauma patients.
This study included all consecutive post LSCS patients admitted to PACU. Obstetric critical care management strategies regarding mechanical ventilation, nutrition, antibiotic therapy, sepsis management and transfusion strategies were suitably modified on the basis of physiological changes seen during pregnancy, puerperium and the associated medical diseases. Obstetric patients developing complications antepartum or after vaginal delivery were transferred to medical ICU and were not included in this study.
Postanesthesia intensive care unit is managed by anesthesiologists. Medical, surgical and other expert opinions are sought for assuring coordinated care of patients. The data collected included obstetric and medical history, indication for PACU transfer, PACU course, duration of stay, treatment, the specific interventions like mechanical ventilation, blood and blood products transfusion and inotropic support. Maternal outcome was classified as survivors and nonsurvivors and cause of death in nonsurvivors was noted. APACHE II score at the time of admission was calculated to assess the outcome in terms of predicted death rate. Data of total PACU admissions and total LSCS during the 2-year period was also noted.
Statistical analysis
Qualitative data were represented in the form of frequency and percentage. Association between qualitative variables was assessed by Chi-square test with continuity correction for all 2 × 2 tables and Fisher's exact test for all 2 × 2 tables where P value of Chi-square test was not valid due to small counts. Adjacent row data of more than 2 × 2 tables was pooled and Chi-square test reapplied in case >20.0% cells having expected count <5. Quantitative data were represented using mean ± standard deviation and median and interquartile range. Analysis of quantitative data between survivors and nonsurvivors was done using unpaired t-test if data passes “normality test” and by Mann-Whitney test if data fails “normality test.” Data were analyzed using the Statistical Package for Social Sciences (version 13, SPSS, Chicago, IL).
Results
In the 2-year period, a total of 2120 women were operated for LSCS in our hospital and out of them 61 (2.8%) were admitted consecutively to PACU. Total admissions in the PACU from all surgical specialties were 1890 patients over the same period and 61 were post LSCS; thus, PACU utilization rate for these patients was 3.22%. Out of 61 patients 57 were survivors (93.4%) and 4 were nonsurvivors (6.6%). The mean age of the patients was 28 ± 5.206 years.
Obstetric indications (n = 41, 67.2%) were the most common cause of PACU admission as compared to nonobstetric indications (n = 20, 32.8%). Among obstetric causes hemorrhage (n = 22, 36.1%) was found to be a significant indication for PACU admission (P = 0.035) and hypertensive disorder of pregnancy (n = 18, 29.5%) was the next common cause. Nonobstetric conditions needing PACU admissions included cardiovascular diseases (n = 10, 16.4%), endocrinal disease (n = 5, 8.2), neurological disease (n = 3, 4.9%), aplastic anemia (n = 1, 1.6%), acute promyelocytic leukemia (PML) (n = 1, 1.6%) and sepsis (n = 1, 1.6%) [Figure 1].
Figure 1.
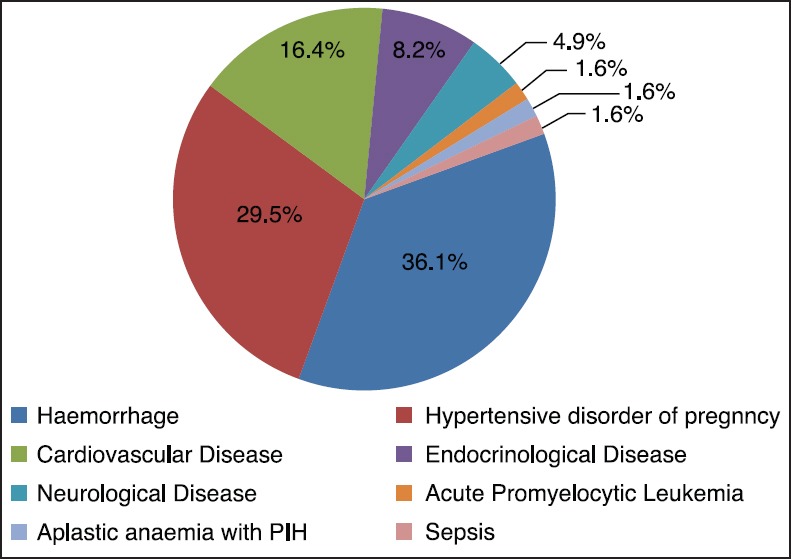
Indications of intensive care unit transfer
Admissions were higher in multipara (n = 40, 65.5%) when compared to primipara (n = 21, 34.5%). However, mortality was higher in primipara (n = 3, 14.3%) when compared to multipara (n = 1, 2.5%), but it was not statistically significant (P = 0.113). Thirty one (50.8%) patients required packed red blood cells (packed cells [PC]) and fresh frozen plasma (FFP) transfusion and 13 patients required platelet transfusion (21.3%) and the difference in total transfusions between survivors and nonsurvivors was not significant (P = 0.674, 0.179, 0.108 respectively for PC, FFP and platelets). Four patients required inotropic support (6.6%) and 26 patients required ventilatory support (42.6%) [Figures 2 and 3].
Figure 2.
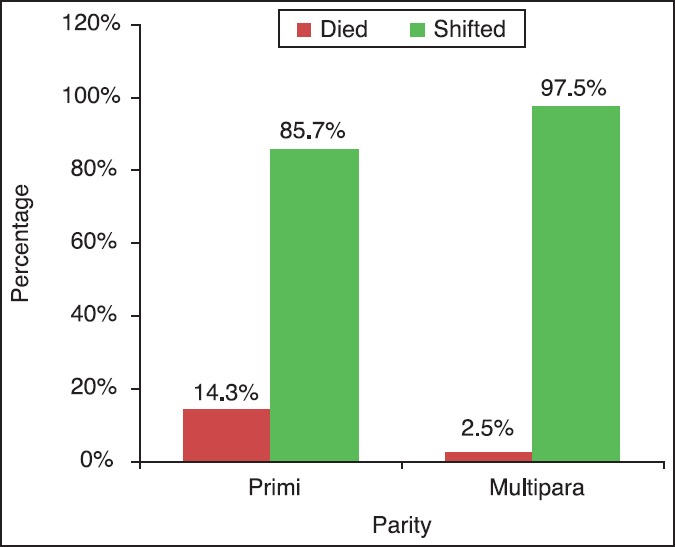
Maternal outcome and parity
Figure 3.
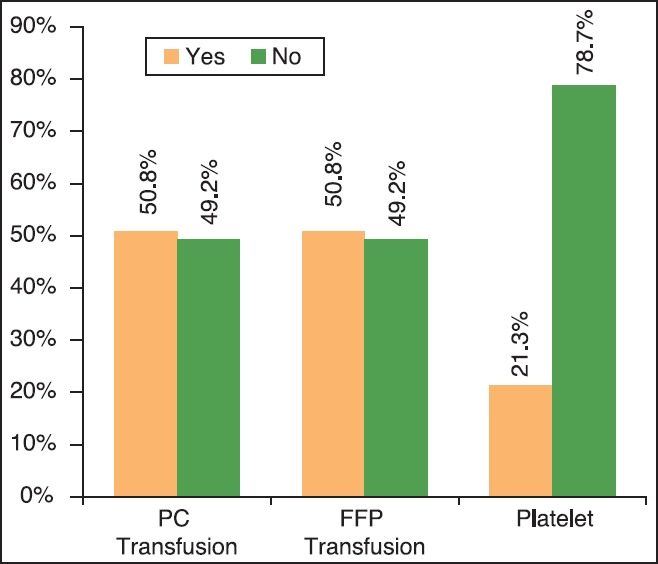
Total utilization of blood products in the study population
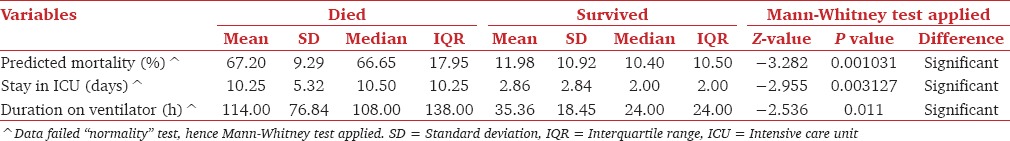
The mean duration of stay in the PACU was 3.34 (±3.511) days (range: 1-18 days). Duration of stay (10.25 ± 5.315 days), (P = 0.00313), duration on ventilator 114.00 (±76.83 h), (P = 0.029) and inotropic support (P = 0.00044 using Fisher's Exact test) in nonsurvivors were statistically significantly different from that among survivors. Predicted mortality was statistically significantly higher for nonsurvivors (67.20%) when compared to survivors (11.98%) (P = 0.00103) [Tables 1 and 2]. Observed mortality was 6.557%, which was lower than predicted mortality (15.6%) by APACHE II score.
Table 1.
Variables among the nonsurvivors in the study population
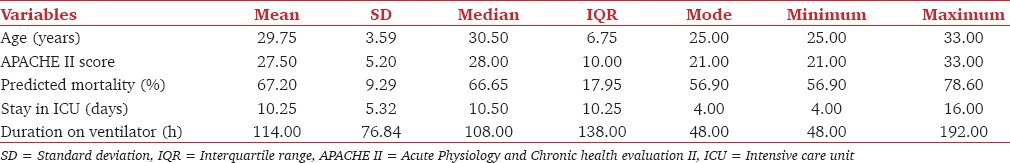
Table 2.
Comparison of various variables between died and survived cases
Causes of death included obstetric hemorrhage leading to disseminated intravascular coagulation (DIC) in one, peripartum cadiomyopathy (PCCM) leading to cardiac failure in two and PML in one. In all of them the terminal cause of death was multi-organ dysfunction syndrome (MODS).
Discussion
Though pregnancy and labor are considered a physiological process the potential for catastrophic complications is constant and may develop in a matter of minutes. There are approximately 118 life-threatening events of “near-miss mortality” or “severe acute maternal morbidity” (SAMM) for each maternal death.[3,4] Global prevalence of SAMM (defined as severe life-threatening obstetric complication necessitating urgent medical intervention in order to prevent likely death of the mother) varies from 0.015 to 8.23%.[3] Clinical recognition of the unique needs of the critically ill obstetric patients have received much attention in an attempt to assess the need for dedicated critical care facilities.[2] The provision of maternal intensive care varies considerably worldwide with very few obstetric units having an ICU located within the labor and maternity ward.[2,3]
Reasons for ICU admission of obstetric patients can be categorized into one of the following groups:[6] Conditions related to pregnancy-hypertensive disorders of pregnancy, hemorrhage, aspiration syndromes, amniotic fluid embolus, acute fatty liver, infections etc; Medical diseases that may be aggravated during pregnancy-congenital heart diseases, rheumatic and nonrheumatic valvular diseases, cardiomyopathy, pulmonary hypertension, anemia, renal failure etc. In the 2 years study period, total 2120 women were operated for LSCS in our hospital and out of them 61 (2.8%) were admitted to PACU. According to various studies it is estimated that 0.1% to 15% of parturients have complications requiring ICU admission.[2,7,8,9,10] In this study total admissions during 2 year study period in the PACU were 1890 patients and of these post LSCS admissions were 61. Thus, PACU utilization rate by obstetric patients was 3.22%. In their study Osinaike et al. they found 4.6% of the total ICU admissions, which is consistent with our study.[11] However, higher utilization of ICU services (1-14%) has been observed in the developed countries.[10,12] The major causes for underutilization of the ICU could be a delay in identification of critically ill obstetric patients, unavailability of dedicated obstetric ICU and limited beds available in PACU for obstetric patients. Out of 61 patients, 4 expired; mortality was thus 6.6% in the present study. In various studies done worldwide reported mortality rates of critically ill obstetric patients admitted to the ICU is in the range from 0 to 40%.[5,6]
Age is one of the important prognostic factors. Mean age of the patients in this study, was 28 ± 5.206 years, which is comparable to studies done by Bhadade et al. and Cleary-Goldman et al. who observed that advanced maternal age is associated with an increased incidence of obstetric complications, including LSCS, hypertensive disorders of pregnancy, eclampsia, placental problems and maternal mortality.[7,13]
In the current study, 40 patients were multipara when compared to 21 primipara patients. Multiparas were mainly admitted to PACU for obstetric indications, whereas primiparas were admitted for nonobstetric causes. Mortality was associated more with nonobstetric causes hence our observed mortality was higher in primipara (3) as compared to multipara (1). However these results are contrasting to other studies where multipara showed a steep rise in mortality.[7,9]
Our study group revealed a higher rate of obstetric indications (67.2%) for PACU transfer rather than nonobstetric (32.8%) indications. Of the obstetric indications hemorrhage and hypertensive disorder of pregnancy were found to be leading indications for PACU admission, which is comparable to literature from Indian and Western studies.[2,3,4,6,7,8,9,10,12,13,14,15,16] Although obstetric hemorrhage is the significant cause for ICU admission, early surgical intervention, systemic use of oxytocin, appropriate fluid replacement, blood transfusions, and correction of coagulopathies possibly contributed to a better outcome. Despite these measures, out of 22 patients of obstetric hemorrhage, hysterectomy was necessary in 8 patients and 1 patient succumbed after developing DIC and MODS. A total of 18 patients were admitted with uncontrolled hypertension and associated complications. They were treated with intravenous (hydralazine, nitroglycerine) antihypertensives and anticonvulsive therapy with magnesium sulfate as per the existing protocol, while care was taken for preventing complications. Nonobstetric indication for PACU transfer included cardiovascular disease (10) endocrinal disease (5) neurological disease (4) aplastic anemia (1), acute promyelocytic leukemia (1) and sepsis (1). Complications of the above conditions can be life threatening, and early detection and resuscitation is the key to successful management and optimal outcomes. Similar observations were echoed in studies by Karnad et al. Cunningham and Zeeman.[9,15,16]
Specific unique diagnoses, such as peripartum cardiomyopathy, require specialized skills and knowledge as they have potentially devastating consequences. Four of our patients had PCCM and out of them 2 patients expired. PCCM is defined as cardiomyopathy that develops in the last month of gestation or in the first 5 months in the postpartum period without any identifiable cause. Clinical presentation includes the signs and symptoms of heart failure and left ventricular systolic dysfunction. Management comprises sodium restriction, loop diuretics, afterload reducing agents (hydralazine, nitrates), and digoxin, β-blockers, anticoagulants, and peripartum cardiomyopathy-targeted therapies (such as intravenous immunoglobulin, pentoxifylline and bromocriptine). Mechanical support and cardiac transplant might be necessary in severe cases. Mortality rate may be as high as 10-50% and there is a high-risk of relapse in subsequent pregnancies.[17,18]
In this study during the course of treatment, 26 patients required ventilatory support and 4 patients required inotropic support. Ventilatory assistance may be required for varying reasons including eclampsia, acute respiratory distress syndrome (due to aspiration, amniotic fluid embolism, etc.) pulmonary edema, congestive cardiac failure and exacerbation of an underlying respiratory disease.[6,7,14] In addition, many patients with complex cardiac lesions are admitted to an ICU after an emergency or elective LSCS for supportive ventilation.[3,15] Longer duration of ventilation and inotropic support were significantly associated with poor outcome. Our observations were consistent with the study done by Gupta et al. in a dedicated obstetric ICU and Bhadade et al.[2,7] Total transfusion requirement was as follows; 31 patients required PC and FFP and 13 patients required platelet transfusion. Karnad et al. and Munnur et al. showed that prompt treatment with blood and blood products in patients with obstetric hemorrhage helped in reducing mortality in these patients.[9,17]
In the current study, the mean duration of stay in the PACU was 3.34 ± 3.511 days (range: 1-18 days) however duration of stay in nonsurvivors (10.25 ± 5.315 days) was longer. This is comparable to the average duration of critical care required in the majority of the patients which was around 5-10 days in the studies by Bhadade et al. and Basket and Sternadel.[7,8] Factors that may predict poor outcome are need for ventilatory support, longer duration of ventilation, inotropic support and prolonged ICU stay. MODS was found to be terminal cause of death in our study. These findings were consistent with the results of many studies.[1,2,3,4,7,8,9,10,15,16]
Accurate predictive scores in the PACU guide in providing aggressive management in those predicted for a poor outcome and also lead to better productive utilization of the limited resources. APACHE II, the world's most widely used severity of illness score is best fit for obstetric patients.[5,19] In APACHE II, there are just 12 physiological variables the reason for ICU admission is, therefore an important variable in predicting mortality, even when previous health status and the degree of acute physiological dysfunction are similar.[5,19]
In this study, we found that observed mortality was 6.557%, which was lower than predicted mortality (15.6%) by APACHE II score. Findings in the current study were comparable to studies done by Karnad et al., who showed that the APACHE II score, over-predicts the mortality in obstetric patients.[9] However, in a study by Bhadade et al. observed mortality was comparable to the predicted mortality, ascertaining the fact that the APACHE II score is a good predictor of mortality in critically ill obstetric patients.[7] It has been observed that when obstetric patients are admitted for medical disorders, the predicted mortality rate (PMR) correlates with the observed mortality rate (OMR). However, in patients with obstetric disorders, the OMR is much lower than the PMR. This overestimation of the risk could be attributed to reversibility of certain obstetric pathologies like preeclampsia and hemorrhage if there is effective and timely management.
The conditions requiring intensive care tend to mirror the causes of maternal deaths and are similar in all of the studies reviewed. Any obstetric unit must be able to provide initial critical care for obstetric emergencies which will be best done if there is dedicated obstetric ICU or high dependency unit (HDU). Full adoption of safe motherhood initiative that is close observation of pregnancy, improvement in antenatal care, early identification of complications, outlining protocols for admission to ICU as well as for management of severe hypertension, hemorrhage and common comorbid conditions and prompt intensive care will be a major step to decrease maternal morbidity as well as mortality. It is preferable to closely monitor for a few hours a high-risk obstetric patient with an uneventful delivery rather than manage complications that could have been prevented.
The limitation of our study was that the study involved only the patients course in the PACU and intraoperative parameters were not included in the protocol. Furthermore, only post LSCS patients were included but patients who developed complications in antepartum period or after vaginal delivery were not included as the study was confined to PACU. Hence, future research should be directed at by including all these obstetric patients, which would be possible if we set up a dedicated obstetric ICU in future. Future studies should also focus on elucidating the best score for predicting mortality in obstetric patients and on developing preventive strategies.
Conclusions
From the experience of the present study, we put forth the following: In the present study PACU utilization rate for obstetric patients was 3.22%. Obstetric hemorrhage and hypertensive disorders of pregnancy with its associated complications were the leading causes of PACU admission. Among nonobstetric indications cardiovascular disease was commonest for morbidity as well as mortality. Blood product transfusion, ventilatory and inotropic supports were the main interventions provided in the PACU and the need for prolonged ventilatory or inotropic support may predict poor outcome. Though predicted mortality by APACHE II score was significantly higher for non-survivors, it over-predicted the mortality in obstetric patients highlighting the importance of a continued search for better scoring system in the critically ill obstetric patients.
Care of the critically ill parturient is a unique challenge in obstetrics. It is these “near-misses” or “SAMM” which require immediate ICU care to minimize the prevalence of multiple organ failure and mortality in critically ill obstetric patients. We hope that this review will serve as an impetus for the formalization of dedicated obstetric critical care unit or HDU and will be the major stepping stone on the road to maternal safety. No efforts should be spared in the management of critically ill obstetric patients because their outcomes are often much better than expected from the initial severity of illness.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Leung NY, Lau AC, Chan KK, Yan WW. Clinical characteristics and outcomes of obstetric patients admitted to the intensive care unit: A 10-year retrospective review. Hong Kong Med J. 2010;16:18–25. [PubMed] [Google Scholar]
- 2.Gupta S, Naithani U, Doshi V, Bhargava V, Vijay BS. Obstetric critical care: A prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian J Anaesth. 2011;55:146–53. doi: 10.4103/0019-5049.79895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dattaray C, Mandal D, Shankar U, Bhattacharya P, Mandal S. Obstetric patients requiring high-dependency unit admission in a tertiary referral centre. Int J Crit Illn Inj Sci. 2013;3:31–5. doi: 10.4103/2229-5151.109416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ps R, Verma S, Rai L, Kumar P, Pai MV, Shetty J. “Near miss” obstetric events and maternal deaths in a tertiary care hospital: An audit. J Pregnancy 2013. 2013 doi: 10.1155/2013/393758. 393758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vincent JL, Moreno R. Clinical review: Scoring systems in the critically ill. Crit Care. 2010;14:207. doi: 10.1186/cc8204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trikha A, Singh P. The critically ill obstetric patient-recent concepts. Indian J Anaesth. 2010;54:421–7. doi: 10.4103/0019-5049.71041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhadade R, De’ Souza R, More A, Harde M. Maternal outcomes in critically ill obstetrics patients: A unique challenge. Indian J Crit Care Med. 2012;16:8–16. doi: 10.4103/0972-5229.94416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baskett TF, Sternadel J. Maternal intensive care and near-miss mortality in obstetrics. Br J Obstet Gynaecol. 1998;105:981–4. doi: 10.1111/j.1471-0528.1998.tb10261.x. [DOI] [PubMed] [Google Scholar]
- 9.Karnad DR, Lapsia V, Krishnan A, Salvi VS. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med. 2004;32:1294–9. doi: 10.1097/01.ccm.0000128549.72276.00. [DOI] [PubMed] [Google Scholar]
- 10.Naylor DF, Jr, Olson MM. Critical care obstetrics and gynecology. Crit Care Clin. 2003;19:127–49. doi: 10.1016/s0749-0704(02)00059-3. [DOI] [PubMed] [Google Scholar]
- 11.Osinaike B, Amanor-Boadu S, Sanusi A. Obstetric intensive care: A developing country experience. The Internet Journal of Anesthesiology. 2006;10(Number 2) Accessed at http://ispub.com/IJA/10/2/10463 . [Google Scholar]
- 12.Sriram S, Robertson MS. Critically ill obstetric patients in Australia: A retrospective audit of 8 years’ experience in a tertiary intensive care unit. Crit Care Resusc. 2008;10:124. [PubMed] [Google Scholar]
- 13.Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105:983–90. doi: 10.1097/01.AOG.0000158118.75532.51. [DOI] [PubMed] [Google Scholar]
- 14.Kostopanagiotou G, Kalimeris K, Pandazi A, Salamalekis G, Chrelias C, Matsota P. The role of the post-anaesthesia care unit in the management of high-risk obstetric patients. Arch Med Sci. 2011;7:123–6. doi: 10.5114/aoms.2011.20616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cunningham FG. Obstetrics complications. In: Leveno KJ, Steven BL, Hauth JC, Rouse DJ, editors. Williams Obstetrics. 23rd ed. New-York: McGraw Hill; 2011. pp. 706–841. [Google Scholar]
- 16.Zeeman GG. Obstetric critical care: A blueprint for improved outcomes. Crit Care Med. 2006;34:S208–14. doi: 10.1097/01.CCM.0000231884.99763.69. [DOI] [PubMed] [Google Scholar]
- 17.Munnur U, Bandi V, Guntupalli KK. Management principles of the critically ill obstetric patient. Clin Chest Med. 2011;32:53–60. doi: 10.1016/j.ccm.2010.10.003. vii. [DOI] [PubMed] [Google Scholar]
- 18.Bhattacharyya A, Basra SS, Sen P, Kar B. Peripartum cardiomyopathy: A review. Tex Heart Inst J. 2012;39:8–16. [PMC free article] [PubMed] [Google Scholar]
- 19.Strand K, Flaatten H. Severity scoring in the ICU: A review. Acta Anaesthesiol Scand. 2008;52:467–78. doi: 10.1111/j.1399-6576.2008.01586.x. [DOI] [PubMed] [Google Scholar]


