Abstract
Background and Aims:
This prospective, randomized, double-blind study was undertaken to establish the effect of addition of magnesium or dexmedetomidine, as an adjuvant, to epidural bupivacaine in lower limb surgeries.
Materials and Methods:
One hundred and twenty ASA (American Society of Anesthesiologists) class I and II patients undergoing lower limb surgeries were enrolled to receive either magnesium sulfate (Group M) or dexmedetomidine (Group D) along with epidural bupivacaine for surgical anesthesia. All the study subjects received an epidural anesthesia with 14 ml of 0.5% bupivacaine along with either MgSO4 50 mg (Group M) or dexmedetomidine 0.5 μg/kg (Group D) or saline (Group C). The onset of motor and sensory block, duration of block, hemodynamic parameters, and any adverse events were monitored.
Results:
Analgesia in the postoperative period was better in Group D, duration of sensory and motor blockade was significantly prolonged in Group D and incidence of sedation was more in Group D.
Conclusion:
Hence, addition of dexemedetomidine to epidural bupivacaine can be advantageous with respect to increased duration of motor and sensory blockade and arousable sedation.
Keywords: Dexmedetomidine, epidural block, magnesium
Introduction
Pain is an unpleasant sensation that originates from ongoing and impending tissue damage. Epidural placement is the safe, effective means of providing surgical anesthesia and postoperative analgesia. No drug has yet been identified that specifically inhibits nociception without associated side effects.[1]
Recent studies suggest the role of magnesium sulfate as an adjuvant to local anesthetics in spinal anesthesia.[2] The biological basis for potential antinociceptive effect of magnesium is its voltage-dependent regulation of calcium influx into the cell, and noncompetitive antagonism of N-methyl-D-aspartate (NMDA) receptors.[1]
Dexmedetomidine is agonist of alpha-2 adrenergic receptors. Alpha-2 agonists (clonidine) have been used as adjuvants in epidural to increase the analgesic duration.[3] Dexmedetomidine is indicated for sedation[4] of critically ill or injured patients in an intensive care unit setting. It has also been used intravenously for postoperative pain relief as adjunct to epidural bupivacaine.[5] Intrathecal and epidural characteristics of dexmedetomidine have been studied in animals.[6,7]
The present study was conceived to evaluate the efficacy of dexmedetomidine and magnesium as an adjuvant to epidural bupivacaine.
Materials and Methods
This randomized, double blind study was approved by the institutional ethics committee. All adult, ASA grade I and II patients scheduled for lower limb surgery who gave informed consent were eligible for the study. Exclusion criteria were patients with history of adverse reaction to any study medication, history of analgesic use, and chronic pain syndrome, where communication difficulties preventing reliable assessment and patients for whom central neuraxial block is contraindicated. Of the 144 subjects, 120 were selected and randomized.
All the patients enrolled in the study had standard monitoring of their heart rate and blood pressure. An intravenous (i.v.) cannula was inserted and lactated Ringer's solution was infused at 20 ml/kg prior to the siting of the epidural. Under aseptic conditions and infiltration of the skin with local anesthetic, an 18G Tuohy needle was used to identify the epidural space, by loss of resistance technique, at L2-3 or L3-4 space. A multiorifice, epidural catheter was then advanced to 5 cm in the epidural space. Correct placement of epidural catheter was verified with a test dose of 3 ml epidural lignocaine 2% with adrenaline (1:200,000).
Subjects were randomized into Groups M, D, and C by randomization using a sealed envelope technique and received medications by epidural route as follows:
Group M: Bupivacaine 0.5% (14 ml) + magnesium sulfate 50 mg (in 1 ml 0.9% saline)
Group D: Bupivacaine 0.5% (14 ml) + dexmedetomidine 0.5 μg/kg (in 1 ml 0.9% saline)
Group C: Bupivacaine 0.5% (14 ml) + saline 0.9% (1 ml)
Motor blockade was assessed by using Modified Bromage Scale:
-
0.
No motor block;
-
1.
Inability to raise extended leg; able to move knees and feet,
-
2.
Inability to raise extended leg or move knee but able to move feet, and
-
3.
Complete motor block of limb).[8]
The sensory block was assessed using a short beveled sterile 26G hypodermic needle along the midclavicular line, bilaterally. The time to achieve anesthesia up to T10 level was noted.
Monitoring consisted of heart rate and noninvasive blood pressure in three groups. The hemodynamic parameters were monitored continuously during the perioperative period and any changes greater than 20% from the baseline value were treated. Hypotension was defined as mean arterial blood pressure >20% decrease in baseline values, treated with inj. mephentermine 6 mg i.v. in bolus dose.
Tachycardia was defined as heart rate >100/min and bradycardia was defined as heart rate <60/min. or >25% decrease in baseline values; it was treated with inj. atropine 0.3 mg i.v. in bolus dose.
The patients were asked to evaluate their pain on standard 100 point visual analogue pain scale (VAS 0 = no pain, VAS 100 = worst possible pain). In the event of pain, (VAS ≥40), both intraoperatively as well as postoperatively, a bolus of epidural bupivacaine 0.125% (12 ml) was administered by the anesthesiologist inside the operation theatre and the nursing staff in the recovery room.
Time to this first epidural top up requirement was recorded.
Any side effects including hypotension, bradycardia, nausea and vomiting, sedation, and shivering were noted. Nausea and vomiting was treated with inj. ondansetron 6 mg. Sedation was graded by five point scale (1-alert and wide awake, 2-arousable to verbal command, 3-arousable with gentle tactile stimulation, 4-arousable with vigorous shaking, and 5-unarousable).[9]
Statistical analysis
Data were expressed as mean ± standard deviation (SD). Group comparisons have been performed using “Microsoft Excel 2007” analysis of variance (ANOVA): Single factor.
Results
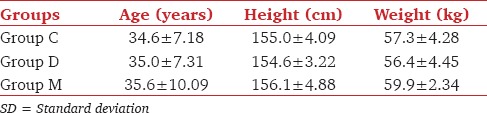
There were no statistical differences in age, height, and body weight between the groups [Table 1].
Table 1.
Age, height, and weight of patients in different groups (mean ± SD)
These groups were similar in the maximal dermatome height achieved. All the subjects underwent orthopedic surgery of the lower limb.
The pulse rate of the patients was recorded at various time intervals, that is, preoperatively, at the time of drug delivery, at 5 min intervals for first 20 min then 10 min and 15 min intervals up to 60 min [Figure 1].
Figure 1.
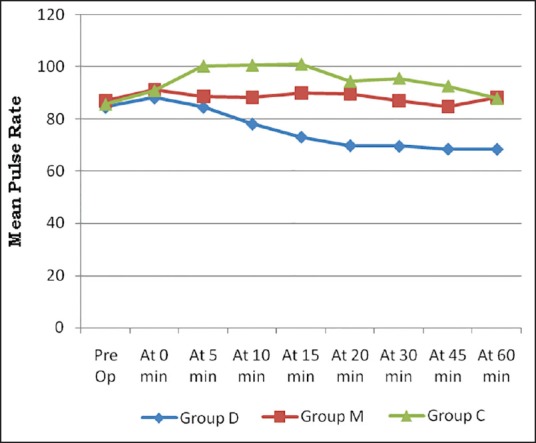
Diagram showing mean pulse rate (PR) at various time intervals in three groups
There was statistically significant difference (P < 0.001) in the mean pulse rate of the three groups. There was fall in the mean pulse rate in Group D.
The mean arterial pressure (MAP) of the patients was recorded at various time intervals, that is, preoperatively, at the time of drug delivery, at 5 min intervals for first 20 min then 10 min and 15 min intervals up to 60 min [Figure 2[.
Figure 2.
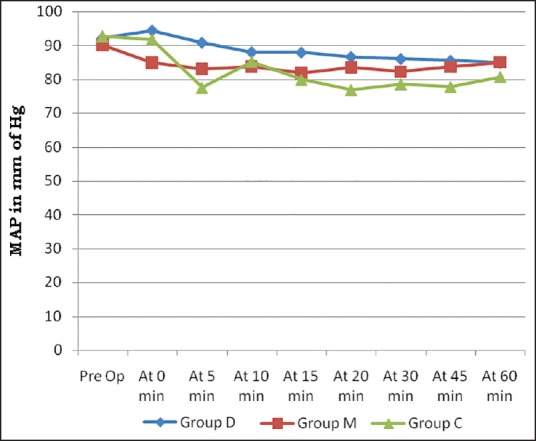
Diagram showing mean arterial pressure (MAP) at various time intervals in three groups
There was no statistically significant difference (P > 0.05) in the MAP of the three groups.
The time to achieve sensory block to T10 level was 14.6 ± 1.9, 15.4 ± 2.1, and 19.7 ± 2.1 min for Groups D, M, and C, respectively. The duration in Group C was significantly longer than the other two groups (P < 0.05), but the difference between Groups D and M was not significant [Table 2].
Table 2.
Time in minutes (mean ± SD) to achieve various landmarks
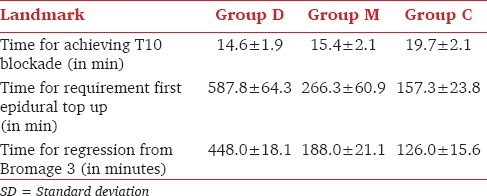
The time from epidural medication to first epidural top up was longest (587.8 ± 64.3 min) in dexmedetomidine group followed by magnesium group (266.3 ± 60.9 min) and with a shortest (157.3 ± 23.8 min) in control group of patients. The differences among groups were highly significant (P < 0.001).
The time from epidural medication for regression from Bromage 3 (i.e., the time when some power was regained in the limb or regression from complete motor block of lower limb) was 126.0 ± 15.6 min for control group and 448.0 ± 18.1 min for dexmedetomidine group, and 188.0 ± 21.1 min in magnesium group. These differences were statistically significant (P < 0.001).
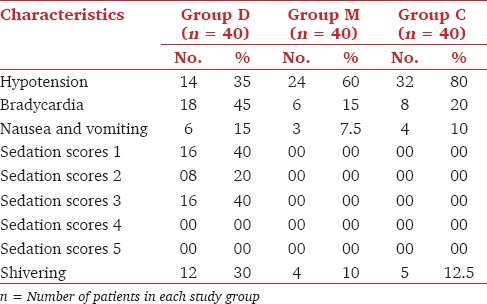
The adverse effects [Table 3] were noted during the first 1-2 h of the drug administration in all three groups.
Table 3.
Side effects
Discussion
In humans, the dose of epidural dexmedetomidine reported is in the range of 1.5-2 μg/kg. Fukushima, et al.,[10] administered 2 μg/kg epidural dexmedetomidine for postoperative analgesia in humans without any reports of neurological deficits. Moreover, Maroof, et al.,[11] used epidural dexmedetomidine, approximately 1.5 μg/kg, to decrease the incidence of postoperative shivering, without any reports of neurological deficits. The results of our study reveal that the combination of 14 ml of 0.5% epidural bupivacaine with a smaller dose of 0.5 μg/kg of dexmedetomidine significantly prolonged both motor and sensory block when compared with 0.5% epidural bupivacaine alone or in combination with magnesium sulfate (MgSO4). We preferred lower dose of dexmedetomidine as higher doses results in more side effects such as bradycardia.[12]
Kalso, et al.,[6] studied the antinociceptive effects of intrathecal dexmedetomidine in rats and observed good antinociception lasting upto 6 h.
The mechanisms by which α2-adrenoceptor agonists prolong the motor and sensory block of local anesthetics is not well understood. It is not a result of altered systemic absorption, as the plasma level of bupivacaine was not altered after the addition of intrathecal clonidine to bupivacaine spinal injection.[13] It may be an additive or synergistic effect secondary to the different mechanisms of action of the local anesthetic and the α2-adrenoceptor agonist. The local anesthetic acts by blocking sodium channels, whereas the α2-adrenoceptor agonist acts by binding to presynaptic C fibers and postsynaptic dorsal horn neurons. The α2-adrenoceptor agonists produce analgesia by depressing the release of C-fiber transmitters and by hyperpolarization of postsynaptic dorsal horn neurons.[14,15,16,17,18] This antinociceptive effect may explain the prolongation of the sensory block when added to spinal or epidural anesthetics. On the other hand, Yaksh[19] has shown that intrathecal α2-adrenoceptor agonists can cause a dose-dependent decrease in motor strength in animals. The prolongation of the motor block of spinal anesthetics may result from the binding of α2-adrenoceptor agonists to motor neurons in the dorsal horn.[20]
Arcioni, et al.,[21] observed that intrathecal and epidural magnesium sulfate potentiated and prolonged motor block.[21] They concluded that patients undergoing orthopedic surgery, supplementation of spinal anesthesia with combined intrathecal and epidural MgSO4 significantly reduces patients’ post-operative analgesic requirements. Magnesium blocks NMDA channels in a voltage-dependent way and produces a dramatic reduction of NMDA-induced currents.[22]
Noxious stimulation leads to the release of glutamate and aspartate neurotransmitters, which bind to the NMDA receptor. Activation of these receptors leads to calcium entry into the cell and initiates a series of central sensitization such as wind-up and long-term potentiation in the spinal cord in the response of cells to prolonged stimuli.[23] NMDA receptor signaling may be important in determining the duration of acute pain.[24] Magnesium blocks calcium influx and noncompetitively antagonizes NMDA receptor channels.[25]
Supplementation of epidural dexmedetomidine seems to be a good alternative to epidural magnesium since it produces significantly prolonged duration of sensory and motor block and arousable sedation (grades 2 and 3 and grade 4 as per five point sedation scale. Sedation was graded as per the study by Bajwa, et al.[9]
Shivering was seen in all the three groups, but was more common in Group D. The probable mechanism could be due to hypothermia caused by local epidural anesthetic injection and partially resulting from thermal redistribution from the central to the peripheral region,[26] among other causes.
Although the prolonged duration of sensory blockade with dexmedetomidine can improve postoperative pain management, the delayed recovery of motor function may have its disadvantages and may be inappropriate in day care surgeries.
Our study establishes the role of dexmedetomidine as an adjunct to bupivacaine in comparison to magnesium. In conclusion, 0.5 μg/kg epidural dexmedetomidine seems to be an attractive alternative as adjuvant to epidural bupivacaine for prolonged surgeries, with minimal side effects and excellent postoperative analgesia. Noncompetitive NMDA antagonist magnesium sulfate, administered epidurally, also prolongs the duration of analgesia, but less than epidural dexmedetomidine. Further studies are required to determine whether larger doses of epidural magnesium sulfate can produce greater potentiation of analgesia and reduce opioid requirements.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sirvinskas E, Laurinaitis R. Use of magnesium sulphate in anesthesiology. Med. 2002;38:147–50. [PubMed] [Google Scholar]
- 2.Ozalevli M, Cetin TO, Unlugenc H, Guler T, Isik G. The effect of adding intrathecal magnesium sulphate to bupivacaine-fentanyl spinal anaesthesia. Acta Anaesthesiol Scand. 2005;49:1514–9. doi: 10.1111/j.1399-6576.2005.00793.x. [DOI] [PubMed] [Google Scholar]
- 3.Parker RK, Connelly NR, Lucas T, Serban S, Pristas R, Berman E, et al. Epidural clonidine added to a bupivacaine infusion increases analgesic duration in labor without adverse maternal or fetal effects. J Anesth. 2007;21:142–7. doi: 10.1007/s00540-006-0476-8. [DOI] [PubMed] [Google Scholar]
- 4.Szumita PM, Baroletti SA, Anger KE, Wechsler ME. Sedation and analgesia in the intensive care unit: Evaluating the role of dexmedetomidine. Am J Health Syst Pharm. 2007;64:37–44. doi: 10.2146/ajhp050508. [DOI] [PubMed] [Google Scholar]
- 5.Sule A, Anis A, Gulnaz A. Dexmedetomidine as an adjunct to epidural analgesia after abdominal surgery in elderly intensive care patients: A prospective, double-blind, clinical trial. Curr Therap Res. 2008;69:16–28. doi: 10.1016/j.curtheres.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalso EA, Pöyhiä R, Rosenberg PH. Spinal antinociceptive by dexmedetomidine, a highly selective 2-adrenergic agonist. Pharmacol Toxicol. 1991;68:140–3. doi: 10.1111/j.1600-0773.1991.tb02052.x. [DOI] [PubMed] [Google Scholar]
- 7.Savola M, Woodley J, Kending J, Maze M. Alpha2B adrenoreceptor activation inhibits nociceptor response in the spinal cord of the neonatal rat. Eur J Pharmacol. 1990;183:740. [Google Scholar]
- 8.Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Aneaesthesiol Scand Suppl. 1965;75:193–200. doi: 10.1111/j.1399-6576.1965.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 9.Bajwa SJ, Bajwa SK, Kaur J, Singh G, Arora V, Gupta S, et al. Dexmedetomidine and clonidine in epidural anaesthesia: A comparative evaluation. Indian J Anaesth. 2011;55:116–21. doi: 10.4103/0019-5049.79883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fukushima K, Nishimi Y, Mori K, Takeda J. Effect of epidurally administered dexmedetomidine on sympathetic activity and postoperative pain in man. Anesth Analg. 1996;82:S121. [Google Scholar]
- 11.Maroof M, Khan SA, Jain D, Khan RM, Maroof SM. Evaluation of effect of dexmedetomidine in reducing shivering following epidural anesthesia. Anesthesiology. 2004;101:A495. [Google Scholar]
- 12.Oriol-López SA, Maldonado-Sanchez, Hernandez-Bernal CE, Castelazo-Arredondo JA, L Moctezuma R. Epidural dexmedetomidine in regional anesthesia to reduce anxiety. Revista Mexicana de Anestesiología. 2008;31:271–7. [Google Scholar]
- 13.Boico O, Bonnet F, Mazoit JX. Effects of epinephrine and clonidine on plasma concentrations of spinal bupivacaine. Acta Anaesthesiol Scand. 1992;36:684–8. doi: 10.1111/j.1399-6576.1992.tb03544.x. [DOI] [PubMed] [Google Scholar]
- 14.Eisenach JC, De Kock M, Klimscha W. Alpha(2)-adrenergic agonists for regional anesthesia. A clinical review of clonidine (1984-1995) Anesthesiology. 1996;85:655–74. doi: 10.1097/00000542-199609000-00026. [DOI] [PubMed] [Google Scholar]
- 15.Lawhead RG, Blaxall HS, Bylund DB. Alpha-2A is the predominant a-2 adrenergic receptor subtype in human spinal cord. Anesthesiology. 1992;77:983–91. doi: 10.1097/00000542-199211000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Smith MS, Schumbra UB, Wilson KH, Page SO, Hulette C, Light AR, et al. Alpha 2-Adrenergic receptor in human spinal cord: Specific localized expression of mRNA encoding alpha-2 adrenergic receptor subtypes at four distinct levels. Brain Res Mol Brain Res. 1995;34:109–17. doi: 10.1016/0169-328x(95)00148-l. [DOI] [PubMed] [Google Scholar]
- 17.Yaksh TL, Jage J, Takano Y. Pharmacokinetics and pharmacodynamics of medullar agents. The spinal actions of a-2 adrenergic agonists as analgesics. In: Atikenhead AR, Benad G, Brown BR, et al., editors. Baillieres Clinical Anaesthesiology. Vol. 7. London: Bailliere Tindall; 1993. pp. 597–614. [Google Scholar]
- 18.Fairbanks CA, Wilcox GL. Spinal antinociceptive synergism between morphine and clonidine persists in mice made acutely or chronically tolerant to morphine. J Pharmacol Exp Ther. 1999;288:1107–16. [PubMed] [Google Scholar]
- 19.Yaksh TL. Pharmacology of spinal adrenergic systems which modulate spinal nociceptive processing. Pharmacol Biochem Behav. 1985;22:845–58. doi: 10.1016/0091-3057(85)90537-4. [DOI] [PubMed] [Google Scholar]
- 20.Smith C, Birnbaum G, Carter JL, Greenstein J, Lublin FD. Tizanidine treatment of spasticity caused by multiple sclerosis: Results of a double-blind, placebo-controlled trial. US Tizanidine Study Group. Neurology. 1994;44:S34–43. [PubMed] [Google Scholar]
- 21.Arcioni R, Palmisani S, Santorsola C, Sauli V, Romano S, Mercieri M, et al. Combined intrathecal and epidural magnesium sulfate supplementation of spinal anesthesia to reduce post-operative analgesic requirements: A prospective, randomized, double-blind, controlled trial in patients undergoing major orthopedic surgery. Acta Anaesthesiol Scand. 2007;51:482–9. doi: 10.1111/j.1399-6576.2007.01263.x. [DOI] [PubMed] [Google Scholar]
- 22.Liu HT, Hollmann MW, Liu WH, Hoenemann CW, Durieux ME. Modulation of NMDA receptor function by ketamin and magnesium: Part 1. Anesth Analg. 2001;92:1173–81. doi: 10.1097/00000539-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Pockett S. Spinal cord synaptic plasticity and chronic pain. Anesth Analg. 1995;80:173–9. doi: 10.1097/00000539-199501000-00026. [DOI] [PubMed] [Google Scholar]
- 24.Woolf CJ, Thompson SW. The induction and maintenance of central sensitization is dependent on N-methyl-o-aspartic acid receptor activation; Implications for the treatment of post-injury pain hypersensitivity states. Pain. 1991;44:293–9. doi: 10.1016/0304-3959(91)90100-C. [DOI] [PubMed] [Google Scholar]
- 25.Fawcett WJ, Haxby EJ, Male DA. Magnesium: Physiology and pharmacology. Br J Anaesth. 1999;83:302–20. doi: 10.1093/bja/83.2.302. [DOI] [PubMed] [Google Scholar]
- 26.Sessler DI, Ponte J. Shivering during epidural anesthesia. Anesthesiology. 1990;72:816–21. doi: 10.1097/00000542-199005000-00008. [DOI] [PubMed] [Google Scholar]


