Abstract
Paraquat (PQ) has known negative human health effects, but continues to be commonly used worldwide as a herbicide. Our clinical data shows that the main prognostic factor is the time required to achieve a negative urine dithionite test. Patient survival is a 100% when the area affected by ground glass opacity is <20% of the total lung volume on high-resolution computed tomography imaging 7 days post-PQ ingestion. The incidence of acute kidney injury is approximately 50%. The average serum creatinine level reaches its peak around 5 days post-ingestion, and usually normalizes within 3 weeks. We obtain two connecting lines from the highest PQ level for the survivors and the lowest PQ level among the non-survivors at a given time. Patients with a PQ level between these two lines are considered treatable. The following treatment modalities are recommended to preserve kidney function: 1) extracorporeal elimination, 2) intravenous antioxidant administration, 3) diuresis with a fluid, and 4) cytotoxic drugs. In conclusion, this review provides a general overview on the diagnostic procedure and treatment modality of acute PQ intoxication, while focusing on our clinical experience.
Keywords: Paraquat, Reactive Oxygen Species, Antioxidants, Hemoperfusion
INTRODUCTION
Paraquat (N, N'-dimethyl-4, 4'-bipyridinium dichloride; PQ) is one of the most widely used herbicides in the world (1), despite its ban in the European Union since 2007 for not meeting health standards (2). PQ intoxication is a serious public health problem, with an estimated annual incidence of 2000 toxic ingestions associated with a mortality rate of 60%-70%, in some Asian countries (3, 4, 5, 6, 7). PQ is a widely used suicide agent in developing countries due to its widespread availability, low toxic dose, and relatively low cost.
Several methods have been studied for modifying the toxicity of PQ (8, 9, 10, 11, 12) over the past 40 yr, but none have proven to be effective to date. Therefore, the clinical outcome of PQ intoxication is usually determined by the degree of exposure (13, 14).
Intentional ingestion of pesticide is a common way of committing suicide in Korea. Our pesticide intoxication institute therefore experiences a high incidence of acute PQ intoxication, with more than 10,000 cases during the past 30 yr.
In this article, we describe our clinical experience and propose a diagnostic and therapeutic approach for patients with acute PQ intoxication.
MECHANISM OF PARAQUAT (PQ) POISONING
Mechanisms of critical toxicity in the human body
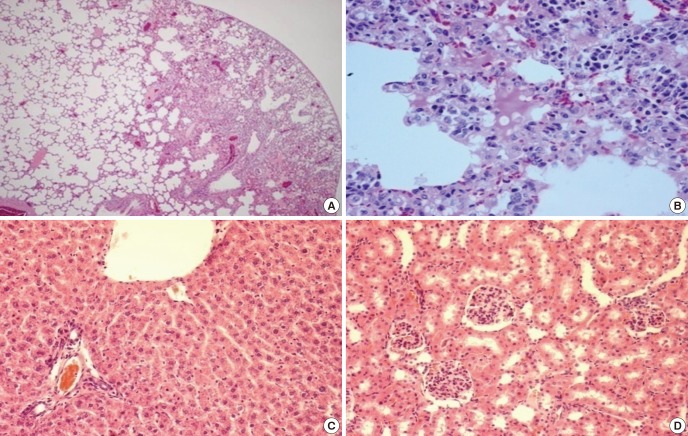
Several pathways are identified as causative factors of critical toxicity of PQ in the human body. Firstly, the lungs are vulnerable to PQ intoxication (Fig. 1). PQ concentration within the lungs increases continuously during the first several hours post-PQ ingestion despite decreasing plasma PQ levels. Many scientists attribute this phenomenon to high affinity of PQ to alveolar cells. Injury to pneumocytes is initiated by nicotinamide adenine dinucleotide (NADH)-dependent reduction of PQ to mono cation radicals (PQ+). Spontaneous reaction with molecular oxygen yields the superoxide radical (O2-) and reversibly forms PQ++, which can be reduced again. PQ intoxication thus frequently causes death due to respiratory failure (15, 16).
Fig. 1.
Lung is a vulnerable organ in acute paraquat intoxication. Lethal dose of paraquat (25 mg/kg) was injected intraperitoneally in mice and 3 days later, the mice were sacrificed. The lung, liver and kidney were obtained and examined by light microscopy. (A) The lung parenchyma show interstitial widening and inflammatory infiltrates predominantly in the sub-pleural area (H&E, ×40). (B) High power examination of the lung reveals dense infiltration of lymphoplasma cells (H&E, ×400). The liver (C) and kidney (D) are histologically unremarkable (H&E, ×100).
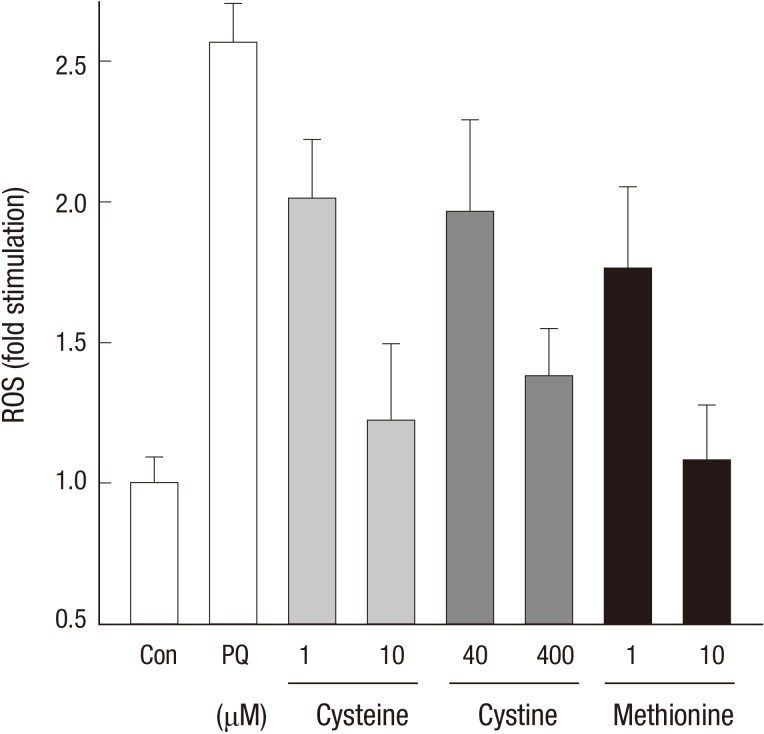
Secondly, reactive oxygen species (ROS) mediated cell signal transduction causes inflammation (17, 18). Consequently, the initial pathologic finding is characterized by inflammatory cell infiltration (Fig. 2). Many physicians thus attempt anti-inflammatory drugs as a treatment modality in patients with acute PQ intoxication. This topic is further addressed in the following paragraphs. Thirdly, mitochondria damage by PQ. Finally, PQ releases free form iron from ferritin, aggravating ROS production (19, 20, 21, 22).
Fig. 2.
ROS mediated signal transduction in inflammation. Free radicals stimulate protein complexes, such as PI3K, NF-κB, and Activator protein-1 which control transcription of DNA, involved in cellular functions such as cell growth, proliferation, and differentiation.
CLINICAL MANIFESTATIONS
Clinical characteristics of acute PQ intoxication
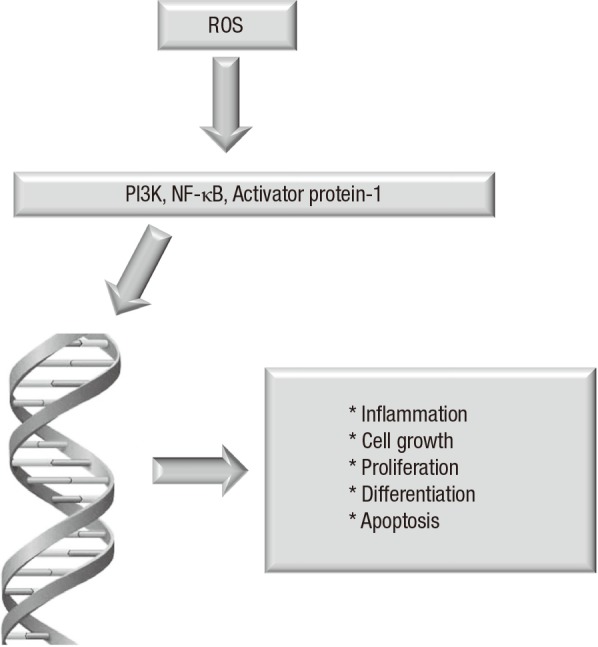
The clinical features of acute PQ intoxication are characterized by high mortality, rapid progression, and frequent injury to the lung and kidney. Acute PQ intoxication is usually asymptomatic in the early stage. Irritation and numbness of the tongue and oral mucosa are generally the only complaints noted in most cases, within the first few days. Table 1 summarizes the main symptoms reported according to severity of PQ intoxication.
Table 1.
Symptoms and signs of acute PQ intoxication, according to the severity of intoxication
*Hiccups generally occur when the ingestion amount is >100 mL and far ominous symptoms; †Confusion is usually accompanied by death within a few days.
Shortness of breath, an increased respiratory rate (tachypnea), lethargy, and confusion appear within 3 to 4 days post-PQ ingestion, as the lung injury (consolidation on imaging) progresses in cases of moderate to severe intoxication.
Clinical features of acute kidney injury in patients with acute PQ
The incidence of acute kidney injury (AKI) secondary to PQ intoxication is approximately 50% (23, 24, 25, 26). Non-oliguric renal failure is observed in >50% of AKI patients, especially when a large volume of fluid is administered in early management. Average serum creatinine level reaches its peak around the 5th day post-ingestion, and is usually normalized within 3 weeks. There is no report on permanent loss of renal function after PQ intoxication; however, the mortality risk is significantly higher in patients with renal failure.
Prognostic markers for PQ intoxication
Lee et al. (27) identified the following significant prognostic factors for PQ intoxication based on the initial blood and urine samples obtained in the emergency room and the patient demographics. Age, the amount of PQ ingested, plasma PQ concentration, leukocyte count, blood urea nitrogen, serum creatinine, uric acid, aspartate aminotransferase, alanine aminotransferase, and amylase were significant prognostic factors.
DIAGNOSIS
Detection and interpretation of PQ in a body fluid
The detection of PQ in a body fluid (e.g., serum, plasma, urine) is necessary and sufficient to confirm PQ intoxication. PQ levels are to be interpreted with reference to the time lag after PQ ingestion in keeping with the toxicokinetics of PQ. The kinetics of PQ distribution are best described by a 3-compartment model: 1) plasma, 2) a rapid uptake and removal compartment such as the kidney, and 3) a slow uptake compartment, reaching a maximum at approximately 4-5 hr, such as the lung (28). The plasma level peaks early, usually within 1 hr post-PQ ingestion, followed by a rapid and steep decline due to its rapid redistribution from the circulation to other compartments. During this period, plasma concentration shows substantial variation with slight changes at different time intervals after ingestion.
Interpretation of PQ concentration in urine
Seok et al. (29) described the diagnostic potential of a dithionite urine test, an indicator of the plasma PQ level, to determine the severity of PQ intoxication. The principle behind the dithionite test is that the absorbance of PQ changes as a result of the blue color produced on reacting with dithionite. This chemical reaction is facilitated in an alkaline environment. Therefore, the first step of the dithionite test is addition of dithionite to a fresh urine sample in a colorless container followed by alkalization with a weak alkalizing agent such as sodium bicarbonate. The lowest detection level of PQ by high-performance liquid chromatography (HPLC) is 0.01 µg/mL, and by the dithionite PQ detection test, approximately 1 µg/mL. Despite its lower sensitivity, the dithionite test is a useful bedside screening tool for PQ intoxication because of its convenience and reproducibility.
A Foley catheter should be placed and the bladder should be fully emptied on immediate arrival of a PQ intoxicated patient, at the emergency room. This urine sample represents urine production over the previous several hours. Dithionite urine test results from the first sample represent the average blood PQ levels during the previous several hours. A second urine sample is collected after the first urine collection. The result of the dithionite test from the second urine sample represents the current blood PQ level. An observation of higher levels in the first urine sample than the second urine sample can be interpreted as decreasing serum PQ levels from the initial levels prior to patient hospitalization.
Sequential dithionite urine tests are conducted every 3-4 hr after the second dithionite urine test, until the results are negative. The time to achieve a negative urine dithionite test is a reliable marker for predicting mortality and/or essential organ failure (29).The sensitivity and specificity for mortality are 71.4% and 75.0%, respectively with a cut-off value of 34.5 hr for the time to negative conversion of the urine dithionite test. The incidence of acute kidney injury and respiratory failure with a time>34.5 hr is 100% and 85.0%, respectively.
Evaluation of PQ-induced lung injury by imaging
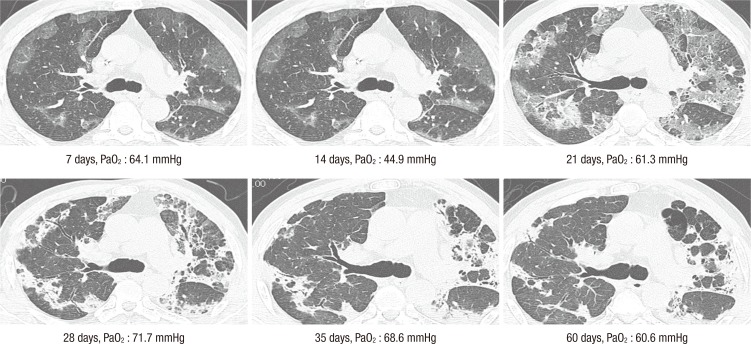
A simple chest radiograph has poor sensitivity and specificity for evaluating PQ-induced lung injury. We recommend high-resolution computed tomography (HRCT) of the lungs on day 7 post-PQ ingestion. We find HRCT as a best modality in fully evaluating the extent of acute PQ lung injury (Fig. 3) (30, 31, 32).
Fig. 3.
Sequential measures on HRCT of the lung. A forty-three old woman intentionally ingested on paraquat in a suicide attempt. She presented to the hospital within 3 hr of ingestion. Serum paraquat level was 2.63 µg/mL. Note that the area of the lung lesion was not expanded in the sequential HRCT. The process of lung fibrosis completes by one month.
The initial pathology of the lung is an inflammation of the alveoli, i.e. alveolitis, which presents as ground glass opacity (GGO) signal on HRCT imaging (30). The predilection site of GGO is the sub-pleural area. A GGO area >50% of the total lung volume is usually fatal, but all surviving patients have a GGO area <20% of the total lung volume on HRCT imaging at 7 days post-PQ ingestion (33).
When a patient hesitantly ingests a large amount of undiluted PQ (>100 mL of 20% PQ) with multiple sips, there is a high chance of developing esophageal rupture and pneumomediastinum, with fatal consequences. GOO lesions progress to fibrosis after 2-3 weeks. Fibrosis is a progressive process, usually stopped within one month (34).
Evaluation of PQ-induced lung injury by arterial blood gas analysis (aBGA)
Tachypnea with low PaCO2 indicates the progression of hypoxia. PaO2 decreases progressively as the PQ induced lung injury proceeds. Notably, in cases of PaO2 <60 mmHg, there is a significant rise in morality. Pulmonary fibrosis develops in the later stage of lung injury. A pulmonary function test after PQ induced lung injury can demonstrate the restriction of lung volume, but the diffusion capacity of the remnant lung remains intact (34).
TREATMENT
Treatment strategy of acute PQ intoxication
The guidelines for developing a new treatment modality for PQ intoxication are derived from well-designed and controlled clinical trials. However, because of the high mortality rate (80%-90%) and ethical problems, it is hard to perform a well controlled clinical trial with PQ. Based on our clinical experience and previous reports (35), we propose the following as a baseline to develop an effective treatment strategy:
1) There are some treatable sub-groups in which PQ lung injury progression can be halted by intensive treatment modalities, 2) Early initiation of treatment is the most important factor, and 3) Renal protection is the cornerstone of early treatment.
Identification of treatable cases of acute PQ intoxication
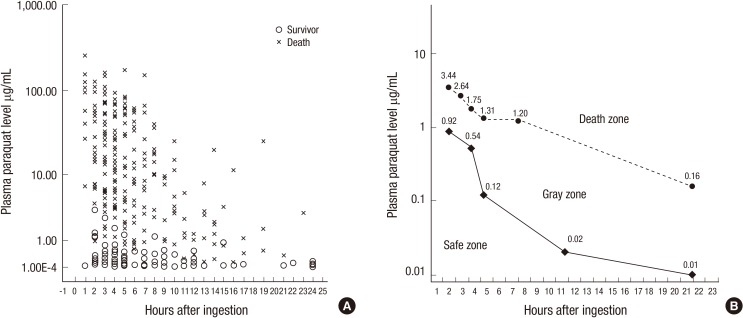
Proudfoot et al. (36) have reported that patients with plasma PQ levels <2.0, 0.6, 0.3, 0.16, and 0.1 µg/mL at 4, 6, 10, 16, and 24 hr post-PQ ingestion, respectively, are most likely to survive. However, even with these predictive guidelines, it is difficult to determine which patients will survive in a clinical setting, because some patients with low PQ levels nevertheless die.
When the plasma PQ levels of 375 patients are plotted against the time lag since PQ ingestion, the highest PQ level of survivors for a given time is 3.44 µg/mL at 2 hr, and then gradually decreases to 2.64 µg/mL at 3 hr, 1.75 µg/mL at 4 hr, 1.31 µg/mL at 5 hr, 1.2 µg/mL at 8 hr, and 0.16 µg/mL at 24 hr from an earlier report (37). For non-survivors, the lowest PQ level is 0.92 µg/mL at 2 hr, and then decreased to 0.54 µg/mL at 4 hr, 0.12 µg/mL at 5 hr, 0.02 µg/mL at 12 hr, and 0.01 µg/mL at 24 hr (Fig. 4) (37). We can obtain two connecting lines, connecting the highest PQ level for the survivors and the lowest PQ level among the non-survivors each at a given time. Patients whose PQ levels fall between these two lines at a given time (gray zone in Fig. 2) are indicated for intensive therapy. These are so-called "treatable patients".
Fig. 4.
Identification of cases with acute PQ intoxication those are treatable. The upper and lower limit of paraquat levels among survivors and non-survivors among 375 patients with acute paraquat intoxication. These levels can be divided into a dead zone (above the upper line, no survivors), gray zone (between the two lines; uncertain final outcome), and a safe zone (below the lower line, no deaths).
Extracorporeal elimination
The best modality on extra-corporeal elimination of PQ is hemoperfusion (HP). The reduction rate of plasma PQ levels by HP is higher than hemodialysis (HD) (9).
The efficacy of HP in clearing serum PQ depends on the function of the HP cartridge, blood flow, and plasma levels. The reduction rate of PQ by HP is 67%-83% in 3 hr, which shows high efficacy throughout the HP in all subjects, according to a report by Hong et al. (9). In light of an almost constant reduction rate and a fixed value for blood flow, the main factor contributing to the efficacy of HP for PQ elimination appears to be the PQ plasma level. A linear correlation exists between the amount of PQ eliminated and the plasma PQ levels, suggestive that the initiation of HP as early as the PQ level reaches its peak level, would be the most effective way to eliminate PQ from the body.
The high incidence of AKI after PQ intoxication is challenging to renal elimination of PQ. The kidney can remove more PQ than HP, and is very effective when renal function is normal. However, once renal function declines, so does the ability to clear PQ. Therefore, the efficacy of the kidneys and HP in elimination of serum PQ varies depending on a number of factors. The kidney is very effective in clearing PQ but is vulnerable to PQ injury. Deterioration of renal function is commonly observed at the early stage of intoxication especially when the PQ level is high. Therefore, renal protection is critical during the early treatment of PQ intoxication.
The elimination of PQ during HP is also limited by blood flow dynamics, which can be regulated by using a jugular venous catheter at a rate of 200-300 mL/min in adults. Keeping in mind both the large PQ distribution volume of 1.0-1.5 L/kg body weight and the very rapid progression of ROS injury on PQ intoxication, PQ elimination must be carried out as soon as possible with high blood flow. Early HP is a required lifesaving treatment in PQ intoxicated patients, especially in cases of early kidney failure or high PQ plasma levels. The clinical effect of HP is below the theoretical expectation; it is unfortunate that the HP clearance is inferior compared to the renal clearance and the volume of distribution of PQ is large.
Background for antioxidant therapy
There are neither true pharmacological antagonists, nor chelating agents against PQ to date. However since PQ induces its toxic effects via oxidative stress-mediated mechanisms, innovations in management of PQ poisoning are directed towards antioxidant administration.
Depletion of glutathione (GSH) enhances PQ toxicity as observed by Bus et al. (38). Hagen et al. (39) and Brown et al. (40) show that the addition of GSH to type-II alveolar cells protects against PQ toxicity. Furthermore, the evidence that GSH peroxidase plays a key role in protecting animals against PQ toxicity is demonstrated on transgenic mice in which deletion of this enzyme enhances toxicity while addition of it affords some protection (41).
GSH provides the reducing equivalent for the reduction of hydrogen peroxide to H2O, and is oxidized to its disulfide (GSSG). Most of the GSSG is immediately reduced back to GSH through a GSH reductase with the cofactor NADH.
N-acetyl-L-cysteine (NAC) is a precursor of GSH. Hoffer et al. (42) incubated NAC with type-II alveolar cells, and showed an enhanced GSH content and prevention of PQ induced cytotoxicity.
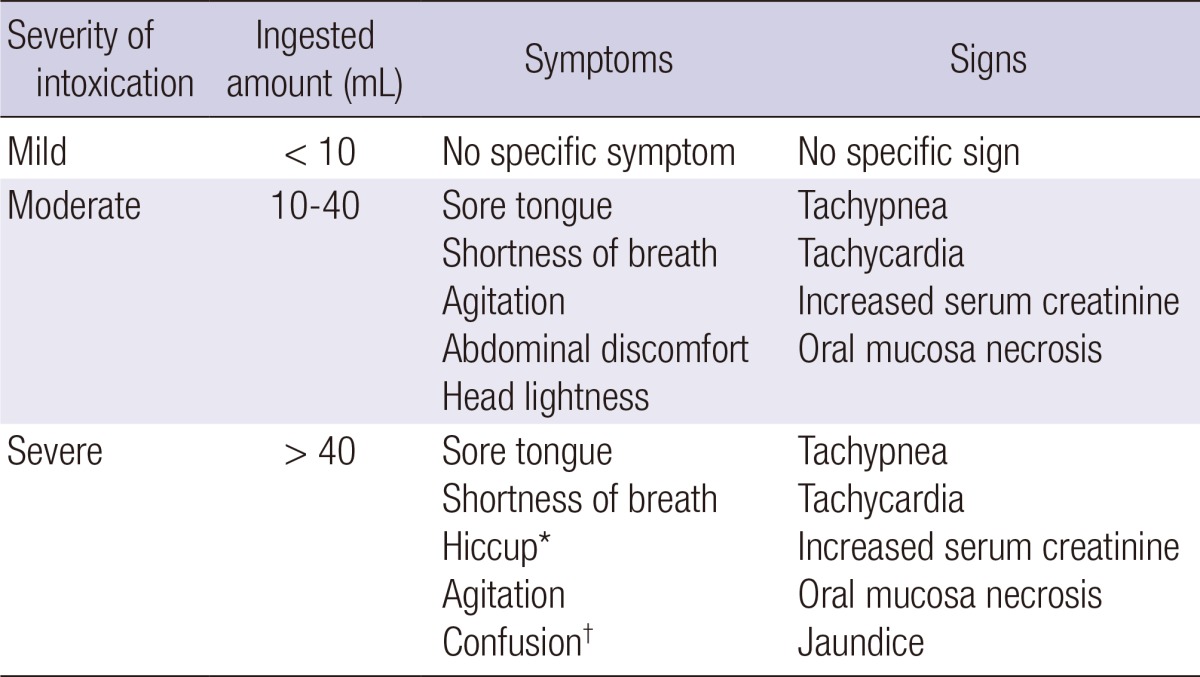
Optimal dose of anti-oxidants
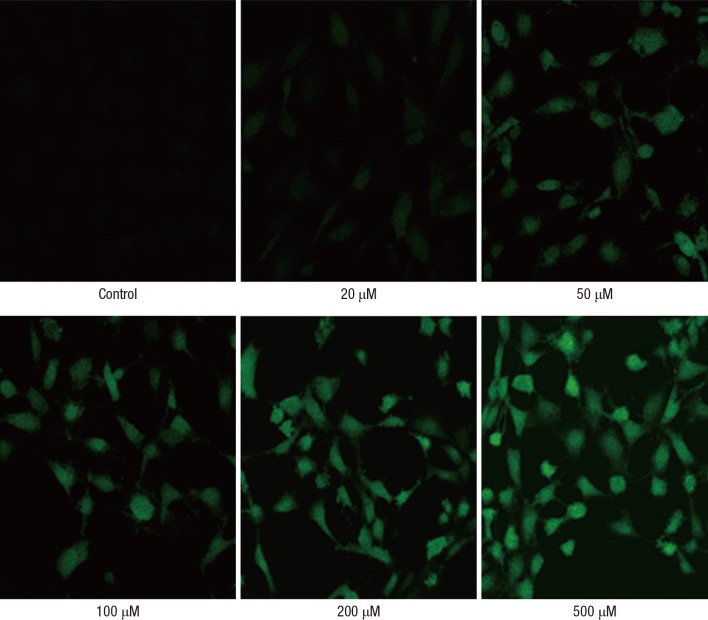
A tremendous amount of ROS is produced immediately after acute PQ intoxication (Fig. 5). Therefore, antioxidants should be administered intravenously. NAC (43, 44) and GSH (45) are commonly used antioxidants, which are safe even at high dosage. In vitro, NAC suppresses ROS in a dose-dependent manner; 10 µM NAC suppresses approximately 50% of the ROS produced by PQ (43). Owing to a lack of pharmacokinetic data, the optimal dose is unknown, but in our experience, 50-70 mg/kg of NAC can be safely administered intravenously.
Fig. 5.
Production of reactive oxygen species (ROS) by PQ treatment in a dose-dependent manner in Swiss 3T3. After 40 min incubation of the cells with 20-500 µM PQ, intracellular ROS generation was assessed with 2, 7-dichlorofluorescein and a laser scanning confocal microscope (×400).
The concentration required to suppress ROS levels by 50% is reported as 10 µM for cysteine and 50 µM for methionine. Based on metabolic kinetics analysis with the assumption that cysteine and methionine are metabolites of GSH, the expected concentrations of cysteine and methionine are estimated to be >20 µM and 50 µM, respectively, when GSH is administered at 50 mg/kg body weight (Fig. 6) (45).
Fig. 6.
Antioxidant effects of thiol-containing amino acid. Note that only 10 µM of both cysteine and methionine is enough to suppress ROS formation in PQ poisoning.
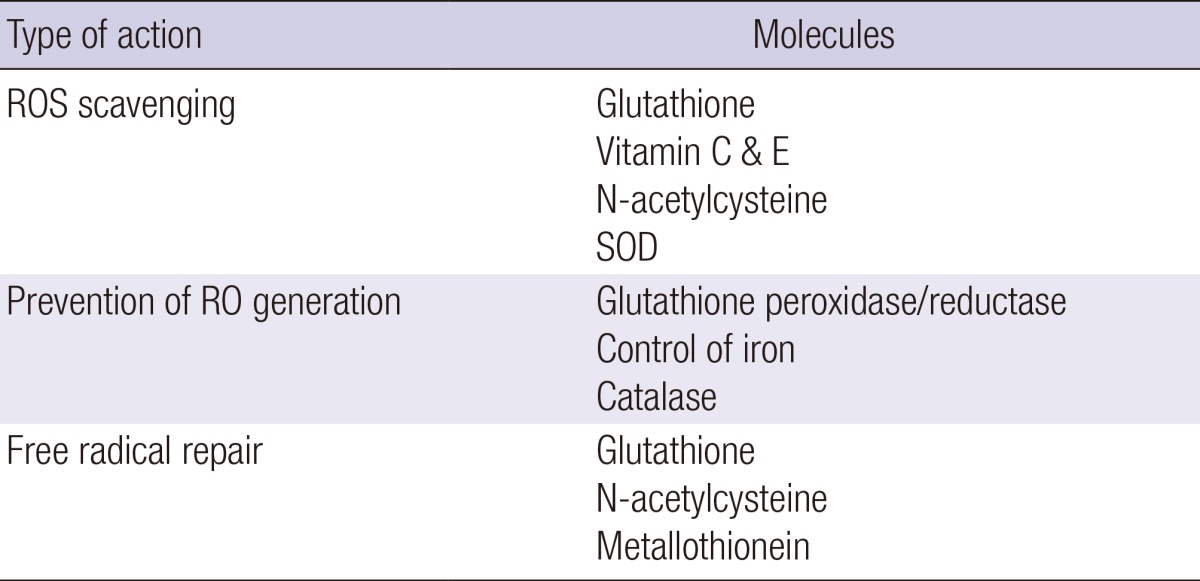
Limitation of anti-oxidants in acute PQ intoxication
Enzymatic antioxidant defense, provided by superoxide dismutase, catalase, and glutathione peroxidase, is the main cellular mechanism, but there is no way to increase the activity of these enzymes thus far (Table 2). PQ intoxication leads to ROS generation not in the extra-cellular space but in intra-cellular space, though we can observe some of the free radicals in the circulation; hydroxyl radical is initially formed in the intracellular environment but crosses the plasma membrane and diffuse out from the cell. Therefore, antioxidants that can enter the cells through the plasma membrane are ideal. It is unfortunate that most of the antioxidants, such as protein thiol, ascorbic acid, and α-tocopherol have low plasma membrane permeability. The process, known as the redox cycle, is sustained by the extensive supply of electrons and oxygen in the lungs (46). Antioxidants exert their antioxidant effect with free radicals, forming a complex with 1:1 stoichiometry. Therefore theoretically, optimal dose of anti-oxidants should be administered without cessation, until the redox cycle is interrupted. However, it is impossible to identify the optimal dose of antioxidant at the patients' bed side and it is difficult to administer high dose of antioxidants for several days without cessation.
Table 2.
Cellular antioxidant strategies
Back ground of cytotoxic drug use
The rationale for cytotoxic drug use in treatment of PQ intoxication is that PQ induces inflammatory cell infiltration in the lung (8, 47, 48, 49). Cyclophosphamide is recommended for a short period on the initial 3-4 days. This is because the cardinal pathologic changes are completed within the first few days of intoxication, and prolonged use of these drugs may be complicated by opportunistic infection. However, until now, cyclophosphamide has inconsistent treatment effects for PQ intoxication; some reports show a positive effect (8, 50), while others do a negative effect (48). We believe that cyclophosphamide administration is more or less effective in the suppression of the inflammatory cell infiltration in the PQ lung. However, to achieve this effect, early administration of cyclophosphamide, at least 2-3 hr after PQ exposure, is important because cyclophosphamide is not effective once cells have already infiltrated (from our animal experiment, data not published). In reality, most patients arrive several hours post-PQ ingestion, probably, leading to a limited clinical effect of cyclophosphamide.
Back ground of steroid therapy
Prednisone, a synthetic corticosteroid is particularly effective as an immunosuppressant drug and is used to treat certain inflammatory diseases. It has likewise become a treatment regimen for patients with acute PQ intoxication. In addition to this general anti-inflammatory effect, our recent in vitro experiment shows that methylprednisolone attenuates PQ-induced cell cytotoxicity via induction of efflux transporter, P-glycoprotein expression (51). However, as with cyclophosphamide, there is no current consensus on the effect of steroid therapy in PQ intoxication.
Iron chelating therapy
Iron chelating therapy is useful against the over-accumulation of iron and is expected to reduce oxidative stress, resulting from the Fenton reaction and Haber-Weiss reaction (52, 53).
The primary use of chelating has been via iron overload transfusion (54). However, coupled with advances in tissue iron quantitation (55, 56), there is tremendous promise of an individually tailored approach to chelating, and subsequent reduction in morbidity and mortality. With this background, appropriate iron chelating would be an effective treatment modality in patients with acute PQ intoxication. However, currently there is no randomized controlled study to prove the effect of iron chelating therapy in acute PQ intoxication.
PROGNOSIS
Proposed treatment modality and clinical outcome
As mentioned above, treatment of PQ intoxication is based on 3 main tenets: some patients are treatable; early treatment initiation is necessary; renal protection is the cornerstone of early treatment. We recommend the following treatment modality: Extracorporeal elimination (HP), Intravenous antioxidant administration (NAC, GSH), Diuresis with fluid, and Short-term cytotoxic drug treatment (steroid pulse therapy, cyclophosphamide).
We find the following clinical outcomes on using this treatment modality. The survival rate varies according to the ingestion amount: <10 mL, almost 100%; 10-20 mL, 80%-90%; 20-40 mL, 50%-60%; 40-50 mL, <10%; >60 mL, <1%. The cause of death also varies in accordance with the amount of PQ ingested. Individuals in the 'sudden death' group (death within the first 24 hr) ingest >100 mL, and cardiac arrest is the most frequent cause of death. Individuals in the 'rapid progress' group (death within 7 days) ingest 50-100 mL, and the most common cause of death is respiratory failure, with or without acute renal failure. Finally, individuals in the 'slow progress' group (death within 2-4 weeks) ingests 15-40 mL, and death occurs in all due to respiratory failure.
A patient is defined as a 'survivor' if he or she survives >3 months after PQ ingestion with stable vital signs and stable lung function. It is extremely rare for a patient to expire 3 months later, secondary to PQ related problems.
CONCLUSION
In conclusion, treatment of PQ intoxication is not well codified. To date, most of the studies are prevalently performed in vitro or in animal models. However, based on our rich clinical experience, we believe a treatable group exists on PQ intoxication. Further studies are required to focus on improved treatment efficiency and on an expanded range of treatment groups.
Footnotes
This work was supported by Soonchunhyang University Research Fund (20140003).
The authors declare no conflicts of interest, and the authors alone are responsible for the content and writing of the article.
References
- 1.Hart TB. Paraquat: a review of safety in agricultural and horticultural use. Hum Toxicol. 1987;6:13–18. doi: 10.1177/096032718700600103. [DOI] [PubMed] [Google Scholar]
- 2.Baltazar T, Dinis-Oliveira RJ, Duarte JA, de Lourdes Bastos M, Carvalho F. Paraquat research: do recent advances in limiting its toxicity make its use safer? Br J Pharmacol. 2013;168:44–45. doi: 10.1111/j.1476-5381.2012.02017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan CT. Suicidal poisoning deaths in Singapore 1975-1984. Ann Acad Med Singapore. 1987;16:300–302. [PubMed] [Google Scholar]
- 4.Yamashita M, Matsuo H, Tanaka J, Yamashita M. Analysis of 1,000 consecutive cases of acute poisoning in the suburb of Tokyo leading to hospitalization. Vet Hum Toxicol. 1996;38:34–35. [PubMed] [Google Scholar]
- 5.Seok SJ, Gil HW, Jeong DS, Yang JO, Lee EY, Hong SY. Paraquat intoxication in subjects who attempt suicide: why they chose paraquat. Korean J Intern Med. 2009;24:247–251. doi: 10.3904/kjim.2009.24.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilks MF, Fernando R, Ariyananda PL, Eddleston M, Berry DJ, Tomenson JA, Buckley NA, Jayamanne S, Gunnell D, Dawson A. Improvement in survival after paraquat ingestion following introduction of a new formulation in Sri Lanka. PLoS Med. 2008;5:e49. doi: 10.1371/journal.pmed.0050049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang SS, Lu TH, Eddleston M, Konradsen F, Sterne JA, Lin JJ, Gunnell D. Factors associated with the decline in suicide by pesticide poisoning in Taiwan: a time trend analysis, 1987-2010. Clin Toxicol (Phila) 2012;50:471–480. doi: 10.3109/15563650.2012.688835. [DOI] [PubMed] [Google Scholar]
- 8.Lin JL, Lin-Tan DT, Chen KH, Huang WH, Hsu CW, Hsu HH, Yen TH. Improved survival in severe paraquat poisoning with repeated pulse therapy of cyclophosphamide and steroids. Intensive Care Med. 2011;37:1006–1013. doi: 10.1007/s00134-010-2127-7. [DOI] [PubMed] [Google Scholar]
- 9.Hong SY, Yang JO, Lee EY, Kim SH. Effect of haemoperfusion on plasma paraquat concentration in vitro and in vivo. Toxicol Ind Health. 2003;19:17–23. doi: 10.1191/0748233703th171oa. [DOI] [PubMed] [Google Scholar]
- 10.Harley JB, Grinspan S, Root RK. Paraquat suicide in a young woman: results of therapy directed against the superoxide radical. Yale J Biol Med. 1977;50:481–488. [PMC free article] [PubMed] [Google Scholar]
- 11.Köppel C, von Wissmann C, Barckow D, Rossaint R, Falke K, Stoltenburg-Didinger G, Schnoy N. Inhaled nitric oxide in advanced paraquat intoxication. J Toxicol Clin Toxicol. 1994;32:205–214. doi: 10.3109/15563659409000452. [DOI] [PubMed] [Google Scholar]
- 12.Hong SY, Hwang KY, Lee EY, Eun SW, Cho SR, Han CS, Park YH, Chang SK. Effect of vitamin C on plasma total antioxidant status in patients with paraquat intoxication. Toxicol Lett. 2002;126:51–59. doi: 10.1016/s0378-4274(01)00431-3. [DOI] [PubMed] [Google Scholar]
- 13.Savy FP, Duval G, Her B, Canu P, Fintelz P. Failure of chemotherapy and radiotherapy in pulmonary fibrosis caused by paraquat. Ann Fr Anesth Reanim. 1988;7:159–161. doi: 10.1016/s0750-7658(88)80146-1. [DOI] [PubMed] [Google Scholar]
- 14.Hampson EC, Pond SM. Failure of haemoperfusion and haemodialysis to prevent death in paraquat poisoning. A retrospective review of 42 patients. Med Toxicol Adverse Drug Exp. 1988;3:64–71. doi: 10.1007/BF03259932. [DOI] [PubMed] [Google Scholar]
- 15.Matthew H, Logan A, Woodruff MF, Heard B. Paraquat poisoning--lung transplantation. Br Med J. 1968;3:759–763. doi: 10.1136/bmj.3.5621.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darke PG, Gibbs C, Kelly DF, Morgan DG, Pearson H, Weaver BM. Acute respiratory distress in the dog associated with paraquat poisoning. Vet Rec. 1977;100:275–277. doi: 10.1136/vr.100.14.275. [DOI] [PubMed] [Google Scholar]
- 17.Roebuck KA. Oxidant stress regulation of IL-8 and ICAM-1 gene expression: differential activation and binding of the transcription factors AP-1 and NF-kappaB (Review) Int J Mol Med. 1999;4:223–230. doi: 10.3892/ijmm.4.3.223. [DOI] [PubMed] [Google Scholar]
- 18.Hensley K, Robinson KA, Gabbita SP, Salsman S, Floyd RA. Reactive oxygen species, cell signaling, and cell injury. Free Radic Biol Med. 2000;28:1456–1462. doi: 10.1016/s0891-5849(00)00252-5. [DOI] [PubMed] [Google Scholar]
- 19.Monteiro HP, Vile GF, Winterbourn CC. Release of iron from ferritin by semiquinone, anthracycline, bipyridyl, and nitroaromatic radicals. Free Radic Biol Med. 1989;6:587–591. doi: 10.1016/0891-5849(89)90065-8. [DOI] [PubMed] [Google Scholar]
- 20.Koskenkorva-Frank TS, Weiss G, Koppenol WH, Burckhardt S. The complex interplay of iron metabolism, reactive oxygen species, and reactive nitrogen species: insights into the potential of various iron therapies to induce oxidative and nitrosative stress. Free Radic Biol Med. 2013;65:1174–1194. doi: 10.1016/j.freeradbiomed.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Rangel NA, Lin L, Rakariyatham K, Bach A, Trinh K, Clement MH, Srinivasan C. Unincorporated iron pool is linked to oxidative stress and iron levels in Caenorhabditis elegans. Biometals. 2012;25:971–985. doi: 10.1007/s10534-012-9563-5. [DOI] [PubMed] [Google Scholar]
- 22.Jomova K, Valko M. Advances in metal-induced oxidative stress and human disease. Toxicology. 2011;283:65–87. doi: 10.1016/j.tox.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 23.Kim SJ, Gil HW, Yang JO, Lee EY, Hong SY. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol Dial Transplant. 2009;24:1226–1232. doi: 10.1093/ndt/gfn615. [DOI] [PubMed] [Google Scholar]
- 24.Vaziri ND, Ness RL, Fairshter RD, Smith WR, Rosen SM. Nephrotoxicity of paraquat in man. Arch Intern Med. 1979;139:172–174. [PubMed] [Google Scholar]
- 25.Gil HW, Yang JO, Lee EY, Hong SY. Clinical implication of urinary neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 in patients with acute paraquat intoxication. Clin Toxicol (Phila) 2009;47:870–875. doi: 10.3109/15563650903306651. [DOI] [PubMed] [Google Scholar]
- 26.Roberts DM, Wilks MF, Roberts MS, Swaminathan R, Mohamed F, Dawson AH, Buckley NA. Changes in the concentrations of creatinine, cystatin C and NGAL in patients with acute paraquat self-poisoning. Toxicol Lett. 2011;202:69–74. doi: 10.1016/j.toxlet.2011.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee EY, Hwang KY, Yang JO, Hong SY. Predictors of survival after acute paraquat poisoning. Toxicol Ind Health. 2002;18:201–206. doi: 10.1191/0748233702th141oa. [DOI] [PubMed] [Google Scholar]
- 28.Baud FJ, Houze P, Bismuth C, Scherrmann JM, Jaeger A, Keyes C. Toxicokinetics of paraquat through the heart-lung block. Six cases of acute human poisoning. J Toxicol Clin Toxicol. 1988;26:35–50. doi: 10.3109/15563658808995396. [DOI] [PubMed] [Google Scholar]
- 29.Seok S, Kim YH, Gil HW, Song HY, Hong SY. The time between paraquat ingestion and a negative dithionite urine test in an independent risk factor for death and organ failure in acute paraquat intoxication. J Korean Med Sci. 2012;27:993–998. doi: 10.3346/jkms.2012.27.9.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee SH, Lee KS, Ahn JM, Kim SH, Hong SY. Paraquat poisoning of the lung: thin-section CT findings. Radiology. 1995;195:271–274. doi: 10.1148/radiology.195.1.7892484. [DOI] [PubMed] [Google Scholar]
- 31.Im JG, Lee KS, Han MC, Kim SJ, Kim IO. Paraquat poisoning: findings on chest radiography and CT in 42 patients. AJR Am J Roentgenol. 1991;157:697–701. doi: 10.2214/ajr.157.4.1892020. [DOI] [PubMed] [Google Scholar]
- 32.Zhang H, Liu P, Qiao P, Zhou J, Zhao Y, Xing X, Li G. CT imaging as a prognostic indicator for patients with pulmonary injury from acute paraquat poisoning. Br J Radiol. 2013;86:20130035. doi: 10.1259/bjr.20130035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim YT, Jou SS, Lee HS, Gil HW, Yang JO, Lee EY, Hong SY. The area of ground glass opacities of the lungs as a predictive factor in acute paraquat intoxication. J Korean Med Sci. 2009;24:636–640. doi: 10.3346/jkms.2009.24.4.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee KH, Gil HW, Kim YT, Yang JO, Lee EY, Hong SY. Marked recovery from paraquat-induced lung injury during long-term follow-up. Korean J Intern Med. 2009;24:95–100. doi: 10.3904/kjim.2009.24.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dawson A, Buckley N. Integrating approaches to paraquat poisoning. Ceylon Med J. 2007;52:45–47. doi: 10.4038/cmj.v52i2.1018. [DOI] [PubMed] [Google Scholar]
- 36.Proudfoot AT, Stewart MS, Levitt T, Widdop B. Paraquat poisoning: significance of plasma-paraquat concentrations. Lancet. 1979;2:330–332. doi: 10.1016/s0140-6736(79)90345-3. [DOI] [PubMed] [Google Scholar]
- 37.Gil HW, Kang MS, Yang JO, Lee EY, Hong SY. Association between plasma paraquat level and outcome of paraquat poisoning in 375 paraquat poisoning patients. Clin Toxicol (Phila) 2008;46:515–518. doi: 10.1080/15563650701549403. [DOI] [PubMed] [Google Scholar]
- 38.Bus JS, Cagen SZ, Olgaard M, Gibson JE. A mechanism of paraquat toxicity in mice and rats. Toxicol Appl Pharmacol. 1976;35:501–513. doi: 10.1016/0041-008x(76)90073-9. [DOI] [PubMed] [Google Scholar]
- 39.Hagen TM, Brown LA, Jones DP. Protection against paraquat-induced injury by exogenous GSH in pulmonary alveolar type II cells. Biochem Pharmacol. 1986;35:4537–4542. doi: 10.1016/0006-2952(86)90776-8. [DOI] [PubMed] [Google Scholar]
- 40.Brown LA, Bai C, Jones DP. Glutathione protection in alveolar type II cells from fetal and neonatal rabbits. Am J Physiol. 1992;262:L305–L312. doi: 10.1152/ajplung.1992.262.3.L305. [DOI] [PubMed] [Google Scholar]
- 41.Cheng WH, Ho YS, Valentine BA, Ross DA, Combs GF, Jr, Lei XG. Cellular glutathione peroxidase is the mediator of body selenium to protect against paraquat lethality in transgenic mice. J Nutr. 1998;128:1070–1076. doi: 10.1093/jn/128.7.1070. [DOI] [PubMed] [Google Scholar]
- 42.Hoffer E, Baum Y, Tabak A, Taitelman U. N-acetylcysteine increases the glutathione content and protects rat alveolar type II cells against paraquat-induced cytotoxicity. Toxicol Lett. 1996;84:7–12. doi: 10.1016/0378-4274(95)03446-3. [DOI] [PubMed] [Google Scholar]
- 43.Hong SY, Gil HW, Yang JO, Lee EY, Kim HK, Kim SH, Chung YH, Lee EM, Hwang SK. Effect of high-dose intravenous N-acetylcysteine on the concentration of plasma sulfur-containing amino acids. Korean J Intern Med. 2005;20:217–223. doi: 10.3904/kjim.2005.20.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hong SY, Yang JO, Lee EY, Lee ZW. Effects of N-acetyl-L-cysteine and glutathione on antioxidant status of human serum and 3T3 fibroblasts. J Korean Med Sci. 2003;18:649–654. doi: 10.3346/jkms.2003.18.5.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hong SY, Gil HW, Yang JO, Lee EY, Kim HK, Kim SH, Chung YH, Hwang SK, Lee ZW. Pharmacokinetics of glutathione and its metabolites in normal subjects. J Korean Med Sci. 2005;20:721–726. doi: 10.3346/jkms.2005.20.5.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bus JS, Gibson JE. Paraquat: model for oxidant-initiated toxicity. Environ Health Perspect. 1984;55:37–46. doi: 10.1289/ehp.845537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin JL, Lin-Tan DT, Chen KH, Huang WH. Repeated pulse of methylprednisolone and cyclophosphamide with continuous dexamethasone therapy for patients with severe paraquat poisoning. Crit Care Med. 2006;34:368–373. doi: 10.1097/01.ccm.0000195013.47004.a8. [DOI] [PubMed] [Google Scholar]
- 48.Perriëns JH, Benimadho S, Kiauw IL, Wisse J, Chee H. High-dose cyclophosphamide and dexamethasone in paraquat poisoning: a prospective study. Hum Exp Toxicol. 1992;11:129–134. doi: 10.1177/096032719201100212. [DOI] [PubMed] [Google Scholar]
- 49.Li LR, Sydenham E, Chaudhary B, You C. Glucocorticoid with cyclophosphamide for paraquat-induced lung fibrosis. Cochrane Database Syst Rev. 2012;7:Cd008084. doi: 10.1002/14651858.CD008084.pub3. [DOI] [PubMed] [Google Scholar]
- 50.Lin JL, Wei MC, Liu YC. Pulse therapy with cyclophosphamide and methylprednisolone in patients with moderate to severe paraquat poisoning: a preliminary report. Thorax. 1996;51:661–663. doi: 10.1136/thx.51.7.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zerin T, Kim YS, Hong SY, Song HY. Protective effect of methylprednisolone on paraquat-induced A549 cell cytotoxicity via induction of efflux transporter, P-glycoprotein expression. Toxicol Lett. 2012;208:101–107. doi: 10.1016/j.toxlet.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 52.Rival T, Page RM, Chandraratna DS, Sendall TJ, Ryder E, Liu B, Lewis H, Rosahl T, Hider R, Camargo LM, et al. Fenton chemistry and oxidative stress mediate the toxicity of the beta-amyloid peptide in a Drosophila model of Alzheimer's disease. Eur J Neurosci. 2009;29:1335–1347. doi: 10.1111/j.1460-9568.2009.06701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jomova K, Valko M. Importance of iron chelation in free radical-induced oxidative stress and human disease. Curr Pharm Des. 2011;17:3460–3473. doi: 10.2174/138161211798072463. [DOI] [PubMed] [Google Scholar]
- 54.Saigo K, Kono M, Takagi Y, Takenokuchi M, Hiramatsu Y, Tada H, Hishita T, Misawa M, Imoto S, Imashuku S. Deferasirox reduces oxidative stress in patients with transfusion dependency. J Clin Med Res. 2013;5:57–60. doi: 10.4021/jocmr1180w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shimizu Y, Matsuzaki S, Dobashi K, Yanagitani N, Satoh T, Koka M, Yokoyama A, Ohkubo T, Ishii Y, Kamiya T, et al. Elemental analysis of lung tissue particles and intracellular iron content of alveolar macrophages in pulmonary alveolar proteinosis. Respir Res. 2011;12:88. doi: 10.1186/1465-9921-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu W, Dahnke H, Rahmer J, Jordan EK, Frank JA. Ultrashort T2* relaxometry for quantitation of highly concentrated superparamagnetic iron oxide (SPIO) nanoparticle labeled cells. Magn Reson Med. 2009;61:761–766. doi: 10.1002/mrm.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]