Abstract
Falls are a major health problem for elderly populations worldwide. We analyzed data from the 2011 Korean Community Health Survey to identify potential risk factors for falls in a representative population-based sample of community-dwelling older Korean adults. Risk factors for falls were assessed by multivariate survey logistic regression models. The prevalence of falls was 36.5% in males and 63.5% in females. Age and female sex were associated with a higher risk of falls. Similarly, living alone, living in an urban area, poor self-rated health, and high stress were associated with a high risk of falls. Subjects with diabetes mellitus, stroke, osteoarthritis, osteoporosis, urinary incontinence, cataracts, or depression had a high risk of falls. However, subjects with hypertension were at low risk for falls. In conclusion, age, female sex, marital status, residence location, self-rated health, stress, and several chronic conditions were significantly associated with the risk for falls in the older Korean adults. Our findings suggest that these risk factors should be addressed in public health policies for preventing falls.
Graphical Abstract
Keywords: Accidental Falls, Elderly People, Risk Factors, Koreans
INTRODUCTION
Falls are a major health problem for elderly populations worldwide. At least one-third of elderly people experience one or more falls each year (1). Recent studies have shown that 25%-40% of people aged 65 yr and over experience falls at least once per year (2, 3, 4). Falls are a leading cause of injury in people aged 65 yr and older. The rate of hospitalization caused by falls in people aged 60 yr and older in Australia, Canada, and England ranges from 1.6 to 3.0 per 10,000 population (5).
Falls are caused by the interaction of multiple risk factors (6). Thus, the identification and removal of risk factors associated with falls is a high clinical priority. A previous meta-analysis revealed that a history of falls, instrumental disability, walking aid use, cognitive impairment, history of stroke, urinary incontinence, rheumatic disease, dizziness and vertigo, diabetes, pain, fear of falling, Parkinson's disease, a number of medications, use of sedatives, use of antiepileptics, and gait problems were associated with the risk of falls (7).
Although several studies have investigated the risk factors associated with falls in elderly people in various countries, few have been conducted on the Korean population (8, 9, 10), and of those, most had limitations such as small sample sizes (about 500) and highly selective populations. Furthermore, no previous study has investigated risk factors associated with falls in a nationally representative sample in Korea. The present study identified potential risk factors for falls in a representative population-based sample of community-dwelling older Korean adults.
MATERIALS AND METHODS
Subjects
Our study was based on data from the 2011 Korean Community Health Survey (KCHS) performed in Korea, between September and November 2011. The KCHS is an annual national health survey conducted since 2008 to provide country-level health indicators of adults aged 19 yr or older. The 2011 KCHS used a multistage sampling design to select representative households. A total of 229,226 subjects participated in the 2011 KCHS. Our analysis was restricted to 56,624 participants who were aged 65 yr or older. Of those, 13,257 subjects were excluded because of missing data. Thus, our study included 43,367 subjects aged 65 yr and older (19,592 males and 23,775 females).
Definition of falls
Falls were defined as one or more falls in the past 12 months. To assess the history of falls, participants were asked whether they had fallen during the past 12 months and, if yes, how often.
Covariates
Body mass index (BMI) was calculated using self-reported height and weight. Marital status was coded into two categories (married/partnered, never married/non-partnered). Household income was determined by each subject's reported monthly household income in Korean won and categorized as <one million and ≥1.01 million Korean won (1,100 KRW is approximately equal to one US dollar). Educational attainment was categorized as uneducated and higher than elementary school. Type of residence was categorized as detached house or other. Self-rated health was ascertained using the question 'In general, how is your health?' with choices of 'very good', 'good', 'ordinary', 'poor', or 'very poor', and was categorized as good health, ordinary, or poor health. Stress experienced was categorized as substantial, some, or little or no stress. Residence location was categorized as a rural or urban. Smoking status was classified as never smoker (smoked<100 cigarettes in their lifetime and not currently smoking) and current smoker (smoked≥100 cigarettes in their lifetime and currently a smoker). Current alcohol intake was defined as drinking alcohol at least once per month in the current year. Physical activity was categorized as absence versus presence of vigorous or moderate physical activity more than once per week. History of hypertension, diabetes mellitus, and dyslipidemia were defined as the use of medication for these diseases. History of stroke, coronary heart disease, osteoarthritis, osteoporosis, urinary incontinence, cataracts, and depression were assessed by self-report of a physician's diagnosis.
Statistical analysis
The data were analyzed to obtain descriptive statistics. Continuous variables were expressed as mean values±standard deviation. Categorical variables were analyzed using the chi-square test. Potential risk factors were selected based on review of literature. Multivariate survey logistic regression models were used to identify the risk factors for fallers and odds ratio (OR) and 95% confidence interval (CI) were calculated in the multivariate model that included all potential risk factors as independent variables. The statistical tests were conducted using the STATA software, version 12.0 SE (StataCorp, College Station, TX, USA), and P values<0.05 were considered to indicate statistical significance.
Ethics statement
The study protocol of 2011 KCHS was reviewed and approved by the institutional review board of Korean Centers for Disease Control and Prevention (2011-05CON-04-C). All participants provided informed consent.
RESULTS
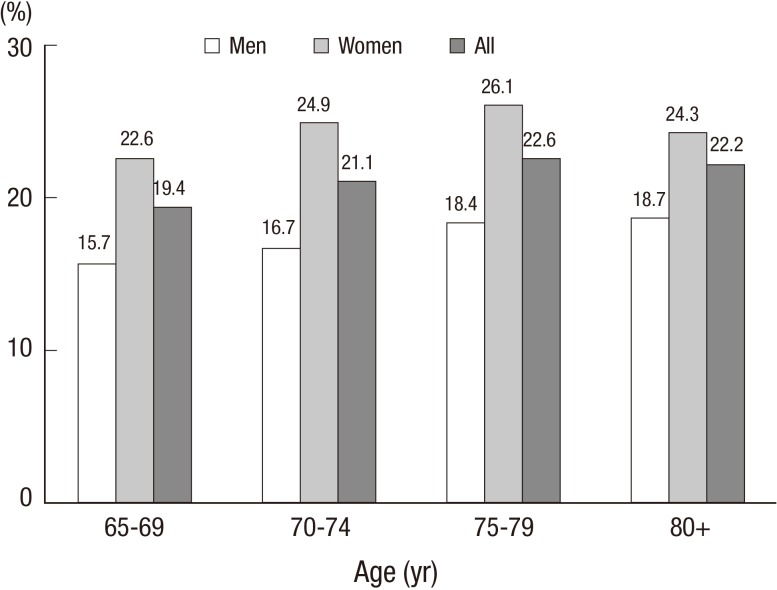
Table 1 shows the general characteristics of the study participants. The mean age of fallers was 73.2±5.8 yr and that of non-fallers was 72.8±5.8 yr. The prevalence of falls was 36.5% in males and 63.5% in females. Compared with non-fallers, fallers had a significantly higher proportion of never married or non-partnered, a low household income, no education, and lived in a residence other than a detached house, respectively. Furthermore, a higher proportion of fallers reported poor health and high stress than did non-fallers. However, non-fallers had a higher rate of current smoking, current alcohol intake, and physical activity. Compared with non-fallers, a higher percentage of fallers had hypertension, diabetes mellitus, dyslipidemia, stroke, coronary heart disease, osteoarthritis, osteoporosis, urinary incontinence, cataracts, and depression. Fig. 1 shows the prevalence of falls according to sex and age. The prevalence of falls was higher in females than in males and increased with age in both sexes.
Table 1.
General characteristics of study participants according to falls history
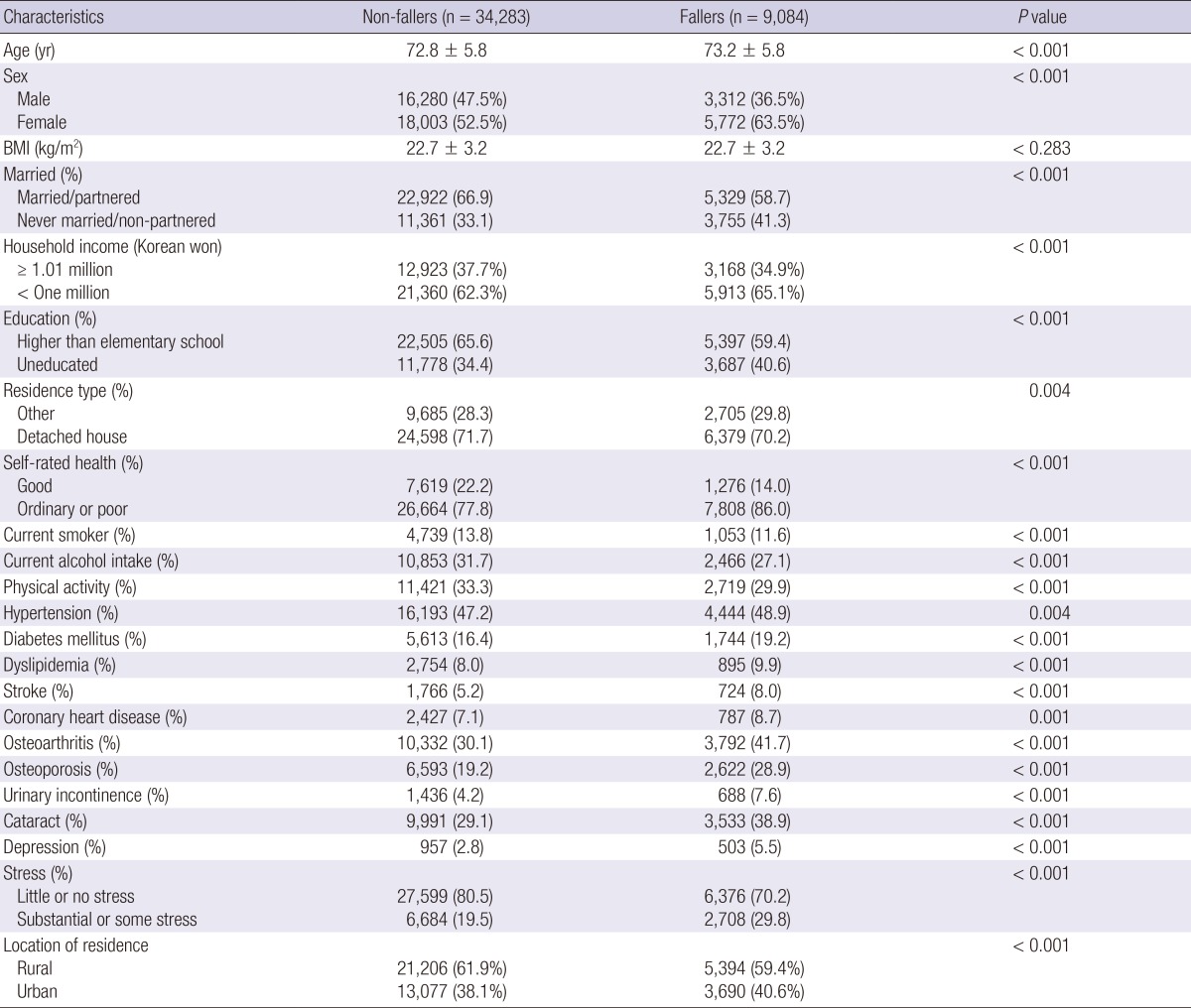
Fig. 1.
Prevalence of falling by sex and age groups.
Table 2 shows the multivariate logistic regression model for the risk of falls. Age (OR per 10 yr, 1.10; 95% CI, 1.04-1.17) and female sex (OR, 1.17; 95% CI, 1.08-1.27) were associated with a higher risk for falls. Living alone (OR, 1.13; 95% CI, 1.05-1.21), living in an urban area (OR, 1.10; 95% CI, 1.03-1.17), poor self-rated health (OR, 1.27; 95% CI, 1.16-1.38), and high stress (OR, 1.54; 95% CI, 1.44-1.65) were associated with a high risk of falls. Furthermore, subjects with diabetes mellitus (OR, 1.14; 95% CI, 1.05-1.23), stroke (OR, 1.44; 95% CI, 1.28-1.62), osteoarthritis (OR, 1.33; 95% CI, 1.24-1.42), osteoporosis (OR, 1.24; 95% CI, 1.15-1.34), urinary incontinence (OR, 1.22; 95% CI, 1.08 -1.37), cataracts (OR, 1.27; 95% CI, 1.19-1.35), and depression (OR, 1.47; 95% CI, 1.27-1.70) had a high risk of falls. However, subjects with hypertension were at low risk for falls (OR, 0.88; 95% CI, 0.83-0.94).
Table 2.
Multivariate logistic regression analysis of risk factors for falls
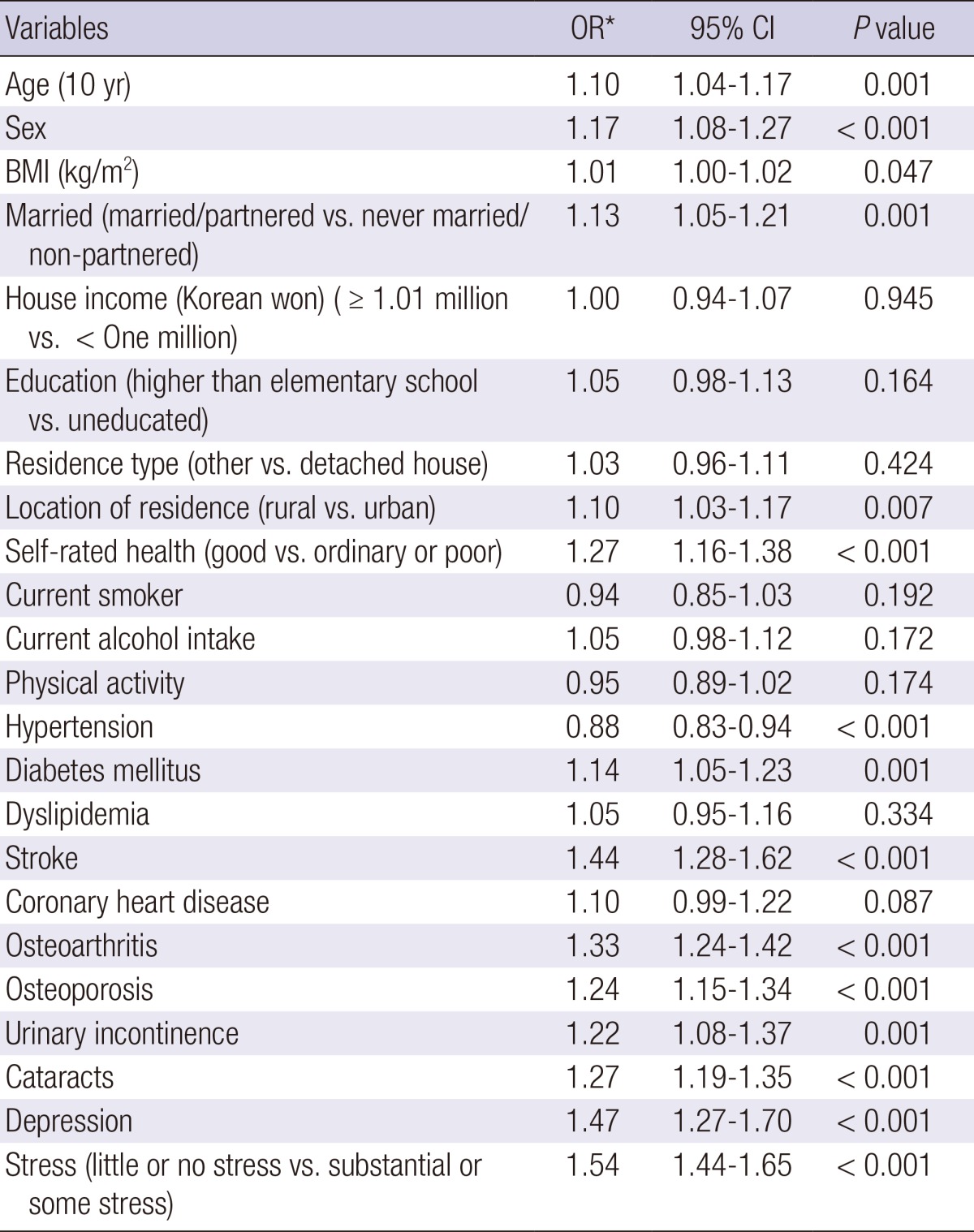
*Adjusted odds ratios were calculated in the multivariate logistic regression that included all variables in the Table as independent variables.
DISCUSSION
We identified potential risk factors for falls among older Korean adults. We found that advanced age, female sex, marital status, location of residence, poor self-rated health, diabetes mellitus, stroke, osteoarthritis, osteoporosis, urinary incontinence, cataracts, depression, and stress were associated with an increased risk of falls. To our knowledge, ours is the first study of a nationally representative sample of older Korean adults to identify risk factors for falls.
Age is a key risk factor for falls (11); and our finding that age was significantly associated with the risk of falls is consistent with previous studies and systematic reviews (7, 12, 13). Moreover, our finding that females were at higher risk for falls than males is consistent with several previous reports that female sex is a significant risk factor for falls (3, 4, 13, 14, 15). In contrast, one community-based study found that the risk of falls was comparable in males and females (16). The authors noted that the male participants in their study received more home care services and experienced more traumatic injuries caused by a falling than males in other studies, and suggested that this difference may explain the conflicting findings (16). Several factors may underlie the gender difference in the risk of falling, including the reluctance of males to report falling, sex differences in leg muscle strength (14), the result of variables not examined in our study (i.e., differences in gait, knee action) (17), and factors associated with being female, such as osteoporosis (18).
Previous investigations of the association between living alone and falls have reported inconsistent results. Australian researchers reported that participants who lived with someone had a low risk for falls (15); however, several previous studies found that living alone was not associated with falls (12, 19, 20). A community-based study found that living alone was inversely associated with falls (21). Living alone is often considered a proxy for social support. Elderly people who live alone may have lower social status and depression caused by isolation and loneliness (22). A community-based study found that the frequency of social interaction was inversely related to reported falls (23). Furthermore, a high level of social support provided by family and friends is associated with a low incidence of falls (24). We found that living alone was associated with an increased risk for falls.
In this study, participants who rated their health as 'ordinary' or 'poor' were at a high risk for falls, which is consistent with a previous report showing that respondents who rated their general health as 'fair or poor' had a high risk for falls (15). A Swedish study found that poor self-rated health was significantly associated with falls in males and females (25). Furthermore, a community-based study revealed that poor self-rated health was significantly associated with recurrent falls (16). These findings suggest that self-rated health status may be useful for identifying those at risk for falls, particularly when clinical assessments may be too expensive or difficult to implement (26).
The use of antihypertensive drugs may cause postural hypotension (27) leading to syncope and falls (28). A systematic review and meta-analysis conducted in Italy found that the use of antihypertensive drugs was significantly associated with the risk for falls (7). Moreover, a Chinese community-based study found that participants who experienced orthostatic hypotension and hypertension had an increased risk for falls (29). Conversely, we found that the risk for falls was decreased in participants who used antihypertensive medications. Similar to this study, a Canadian study based on data from the National Population Health Survey found that the use of antihypertensive medication was associated with a decreased risk for falls, with an odds ratio of 0.42 (13). Interestingly, in a review of drug treatment and falls, no certain association was found between antihypertensive drugs and an increased risk of falls (30). The inconsistency of these findings may be due to discrepancies in population and study design. In addition, the effect of antihypertensive on falls may be influenced by the type or time after initiation of antihypertensive drugs. A Canadian study revealed that initiation of antihypertensive drugs is associated with an increased risk of falls during the first 45 days of treatment (31). However, our study is limited by the lack of information about the type and time period of antihypertensive medication. Therefore, further studies are needed to clarify this issue.
We found that participants who had diabetes mellitus, stroke, osteoarthritis, osteoporosis, urinary incontinence, cataracts, and depression had an increased risk of falls. These results are consistent with those of two recent systematic reviews that found a number of chronic conditions, including visual impairment, depression, urinary incontinence, diabetes, and arthritis and history of stroke were associated with an increased risk for falls (7, 32). Similarly, a community-based study found that participants who had diabetes, stroke sequel, cataracts, osteoarthritis, or depression were at an increased risk for falls (29). A recent community-based study reported that osteoporosis may be associated with falls in older females (18). Overall, several previous studies have found that older people who have one or more chronic diseases are at a significantly increased risk of falls (4, 6, 16, 19, 21, 25, 29, 33).
We found that participants who reported having high levels of stress were at high risk for falls. A previous study found that emotional stress may trigger falls and contribute to injuries among autonomous elderly people (34). The authors suggested that a changing gaze strategy may explain the relationship between stress and injurious fall. In stressful situations, older people use a gaze strategy that is unfavorable for balance control, and as a result, premature gaze transfer contributes to an increased incidence in falls (35). Stress is not a common risk factor for falls; thus, it has not been widely investigated in this context.
We found that participants who lived in urban areas were at higher risk for falls than those living in rural areas. Differences in the distribution of known risk factors and environmental conditions may account for this finding. In contrast, a community-based study found that older people living in rural areas had a significantly higher number of falls than those living in urban areas (36). The authors suggested that the difference could be explained by the fact that older people who live in rural areas had poor health and greater physical impairment than those in urban communities may account for the difference. In our study, participants who lived in urban areas had more chronic conditions, such as diabetes, stroke, incontinence, and depression than those living in rural areas (data not shown); however, adjustment for these variables did not attenuate the association between residence in an urban area and the risk for falls. We found a significant difference between rural and urban areas in the site of falls, suggesting that the distribution of environmental risk factors may account for differences in the risk of falls between these locations.
Our study had several limitations. First, we used a cross-sectional design; thus, we were not able to establish causal relationships between the independent variables and the risk of falls. Second, we relied on self-reports for the incidence of falls, which may have resulted in underreporting. Finally, our study did not consider several known risk factors for falls such as gait problems, hypotension, dizziness, and use of a walking aid.
In conclusion, we found that age, female sex, marital status, location of residence, self-rated health, stress, and several chronic conditions were significantly associated with the risk for falls in older Korean adults. Our findings suggest that these risk factors should be addressed in public health policies to prevent falls.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981;10:264–270. doi: 10.1093/ageing/10.4.264. [DOI] [PubMed] [Google Scholar]
- 2.Milat AJ, Watson WL, Monger C, Barr M, Giffin M, Reid M. Prevalence, circumstances and consequences of falls among community-dwelling older people: results of the 2009 NSW Falls Prevention Baseline Survey. N S W Public Health Bull. 2011;22:43–48. doi: 10.1071/NB10065. [DOI] [PubMed] [Google Scholar]
- 3.Siqueira FV, Facchini LA, Silveira DS, Piccini RX, Tomasi E, Thumé E, Silva SM, Dilélio A. Prevalence of falls in elderly in Brazil: a countrywide analysis. Cad Saude Publica. 2011;27:1819–1826. doi: 10.1590/s0102-311x2011000900015. [DOI] [PubMed] [Google Scholar]
- 4.Orces CH. Prevalence and determinants of falls among older adults in ecuador: an analysis of the SABE I survey. Curr Gerontol Geriatr Res. 2013;2013:495468. doi: 10.1155/2013/495468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. WHO global report on falls prevention in older age. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 6.Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R. Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci. 2002;57:M722–M726. doi: 10.1093/gerona/57.11.m722. [DOI] [PubMed] [Google Scholar]
- 7.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 8.Cho JP, Paek KW, Song HJ, Jung YS, Moon HW. Prevalence and associated factors of falls in the elderly community. Korean J Prev Med. 2001;34:47–54. [Google Scholar]
- 9.Sohng KY, Moon JS, Song HH, Lee KS, Kim YS. Risk factors for falls among the community-dwelling elderly in Korea. J Korean Acad Nurs. 2004;34:1483–1490. doi: 10.4040/jkan.2004.34.8.1483. [DOI] [PubMed] [Google Scholar]
- 10.Yoo IY. Recurrent falls among community-dwelling older Koreans: prevalence and multivariate risk factors. J Gerontol Nurs. 2011;37:28–40. doi: 10.3928/00989134-20110503-01. [DOI] [PubMed] [Google Scholar]
- 11.Craven R, Bruno P. Teach the elderly to prevent falls. J Gerontol Nurs. 1986;12:27–33. doi: 10.3928/0098-9134-19860801-08. [DOI] [PubMed] [Google Scholar]
- 12.Sheahan SL, Coons SJ, Robbins CA, Martin SS, Hendricks J, Latimer M. Psychoactive medication, alcohol use, and falls among older adults. J Behav Med. 1995;18:127–140. doi: 10.1007/BF01857865. [DOI] [PubMed] [Google Scholar]
- 13.Fletcher PC, Hirdes JP. Risk factors for serious falls among community-based seniors: results from the national population health survey. Can J Aging. 2002;21:103–116. [Google Scholar]
- 14.de Rekeneire N, Visser M, Peila R, Nevitt MC, Cauley JA, Tylavsky FA, Simonsick EM, Harris TB. Is a fall just a fall: correlates of falling in healthy older persons. The Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:841–846. doi: 10.1046/j.1365-2389.2003.51267.x. [DOI] [PubMed] [Google Scholar]
- 15.Gill T, Taylor AW, Pengelly A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology. 2005;51:340–345. doi: 10.1159/000086372. [DOI] [PubMed] [Google Scholar]
- 16.Fletcher PC, Hirdes JP. Risk factors for falling among community-based seniors using home care services. J Gerontol A Biol Sci Med Sci. 2002;57:M504–M510. doi: 10.1093/gerona/57.8.m504. [DOI] [PubMed] [Google Scholar]
- 17.Campbell AJ, Spears GF, Borrie MJ. Examination by logistic regression modelling of the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43:1415–1420. doi: 10.1016/0895-4356(90)90110-b. [DOI] [PubMed] [Google Scholar]
- 18.Lin MR, Hwang HF, Lin PS, Chen CY. Relations of osteoporosis and follow-up duration to recurrent falls in older men and women. Osteoporos Int. 2014;25:863–871. doi: 10.1007/s00198-013-2549-5. [DOI] [PubMed] [Google Scholar]
- 19.Tromp AM, Smit JH, Deeg DJ, Bouter LM, Lips P. Predictors for falls and fractures in the Longitudinal Aging Study Amsterdam. J Bone Miner Res. 1998;13:1932–1939. doi: 10.1359/jbmr.1998.13.12.1932. [DOI] [PubMed] [Google Scholar]
- 20.Wu TY, Chie WC, Yang RS, Kuo KL, Wong WK, Liaw CK. Risk factors for single and recurrent falls: a prospective study of falls in community dwelling seniors without cognitive impairment. Prev Med. 2013;57:511–517. doi: 10.1016/j.ypmed.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 21.Leung A, Chi I, Lou VW, Chan KS. Psychosocial risk factors associated with falls among Chinese community-dwelling older adults in Hong Kong. Health Soc Care Community. 2010;18:272–281. doi: 10.1111/j.1365-2524.2009.00900.x. [DOI] [PubMed] [Google Scholar]
- 22.Xie LQ, Zhang JP, Peng F, Jiao NN. Prevalence and related influencing factors of depressive symptoms for empty-nest elderly living in the rural area of YongZhou, China. Arch Gerontol Geriatr. 2010;50:24–29. doi: 10.1016/j.archger.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Cwikel J. Falls among elderly people living at home: medical and social factors in a national sample. Isr J Med Sci. 1992;28:446–453. [PubMed] [Google Scholar]
- 24.Cwikel J, Fried AV, Galinsky D. Falls and psychosocial factors among community-dwelling elderly persons: a review and integration of findings from Israel. Public Health Rev. 1989;17:39–50. [PubMed] [Google Scholar]
- 25.Hedman AM, Fonad E, Sandmark H. Older people living at home: associations between falls and health complaints in men and women. J Clin Nurs. 2013;22:2945–2952. doi: 10.1111/jocn.12279. [DOI] [PubMed] [Google Scholar]
- 26.Vellas BJ, Wayne SJ, Garry PJ, Baumgartner RN. A two-year longitudinal study of falls in 482 community-dwelling elderly adults. J Gerontol A Biol Sci Med Sci. 1998;53:M264–M274. doi: 10.1093/gerona/53a.4.m264. [DOI] [PubMed] [Google Scholar]
- 27.Kwok T, Liddle J, Hastie IR. Postural hypotension and falls. Postgrad Med J. 1995;71:278–280. doi: 10.1136/pgmj.71.835.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Craig GM. Clinical presentation of orthostatic hypotension in the elderly. Postgrad Med J. 1994;70:638–642. doi: 10.1136/pgmj.70.827.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu PL, Qin ZH, Shi J, Zhang J, Xin MZ, Wu ZL, Sun ZQ. Prevalence and related factors of falls among the elderly in an urban community of Beijing. Biomed Environ Sci. 2009;22:179–187. doi: 10.1016/S0895-3988(09)60043-X. [DOI] [PubMed] [Google Scholar]
- 30.Campbell AJ. Drug treatment as a cause of falls in old age. A review of the offending agents. Drugs Aging. 1991;1:289–302. doi: 10.2165/00002512-199101040-00005. [DOI] [PubMed] [Google Scholar]
- 31.Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int. 2013;24:2649–2657. doi: 10.1007/s00198-013-2369-7. [DOI] [PubMed] [Google Scholar]
- 32.Tinetti ME, Kumar C. The patient who falls: "Its alway's a trade-off". JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sibley KM, Voth J, Munce SE, Straus SE, Jaglal SB. Chronic disease and falls in community-dwelling Canadians over 65 years old: a population-based study exploring associations with number and pattern of chronic conditions. BMC Geriatr. 2014;14:22. doi: 10.1186/1471-2318-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Möller J, Hallqvist J, Laflamme L, Mattsson F, Ponzer S, Sadigh S, Engström K. Emotional stress as a trigger of falls leading to hip or pelvic fracture. Results from the ToFa study - a case-crossover study among elderly people in Stockholm, Sweden. BMC Geriatr. 2009;9:7. doi: 10.1186/1471-2318-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chapman GJ, Hollands MA. Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait Posture. 2007;26:59–67. doi: 10.1016/j.gaitpost.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 36.Wojszel ZB, Bień B. Falls amongst older people living in the community. Rocz Akad Med Bialymst. 2004;49:280–284. [PubMed] [Google Scholar]