Abstract
We investigated the association of depressive symptoms with carotid intima-media thickness (IMT) and plaques in the general Korean population. A total of 7,554 Korean males and females aged 45-74 yr who were free from cardiovascular diseases were included in the analyses. Depressive symptoms were assessed by the Center for Epidemiologic Studies Depression Scale (CES-D). Subjects with a score of ≥16 were classified as having clinically significant depressive symptoms. Carotid ultrasonography was used to measure mean carotid IMT (C-IMT) and to determine the presence of plaques. A significant association between depressive symptoms and C-IMT was observed only in females. After adjustment for established cardiovascular risk factors, females with depressive symptoms had significantly greater C-IMT than females without depressive symptoms (mean difference 0.011±0.004 mm; 95% confidence interval, 0.003-0.019 mm). Compared with controls, the fully adjusted risk of females with depressive symptoms for abnormal C-IMT (≥1.0 mm) was significant (odds ratio, 1.63; 95% confidence interval, 1.16-2.30). No significant association between depressive symptoms and carotid plaques was observed in either gender. This study shows a significant association between depressive symptoms and C-IMT in middle-aged and older females.
Graphical Abstract
Keywords: Depression, Atherosclerosis, Carotid Intima-Media Thickness, Carotid Plaque Formation
INTRODUCTION
Depression is a common mental disorder globally, characterized by depressed mood, loss of interest, disturbed sleep or appetite, and poor concentration. Depression is the leading cause of disability and the fourth leading contributor to the global disease burden (1). A number of epidemiological studies have demonstrated that diagnosed depression and depressive symptoms are important risk factors for the development of coronary heart disease and cerebrovascular disease and related death (2, 3, 4, 5). To date, a number of non-invasive measures of subclinical atherosclerosis have been developed. Among them, intima-media thickness (IMT) and plaques of the carotid arteries, a marker of systemic atherosclerosis, is practically considered the surrogate end point of cardiovascular disease such as myocardial infarction and stroke (6, 7, 8, 9).
Recent epidemiological studies have reported an association between depressive symptoms and subclinical atherosclerosis, including carotid IMT and carotid plaques, but the results were inconsistent across studies (10, 11, 12, 13, 14, 15, 16). To our knowledge, few studies have investigated the association between depressive symptoms and carotid atherosclerosis in Asian populations. Moreover, whether depressive symptoms are significantly associated with subclinical carotid atherosclerosis in healthy subjects free of clinical cardiovascular disease remains unclear.
We investigated the association between clinically significant depressive symptoms and subclinical carotid atherosclerosis among healthy community-dwelling Korean adults aged 45 yr and older. In addition, we examined whether there are gender differences between depressive symptoms and carotid atherosclerosis. To evaluate if depressive symptoms contribute to carotid atherosclerosis independently of established cardiovascular risk factors, we considered the effects of established cardiovascular risk factors.
MATERIALS AND METHODS
Study population
The present study was conducted between 2004 and 2007 as the baseline survey of the Namwon Study, an ongoing population-based prospective study designed to investigate chronic disease in community-dwelling adults aged 45-74 yr (17). The Namwon study participants are residents of Namwon city, a representative rural area in Jeonbuk Province, Korea with approximately 90,000 inhabitants, the majority of whom are engaged in agriculture. The 2005 census reported 33,068 residents (14,960 men and 18,108 women) aged 45-74 yr in Namwon city. A total of 10,667 participants (4,201 men and 6,466 women) were recruited in the baseline survey between January 2004 and February 2007 (total participation rate=32.3%, 28.1% for men and 35.7% for women). All medical checkups and questionnaire surveys were performed at the Namwon Medical Center. The Namwon study is scheduled to be followed up by repeated examinations at 4-yr intervals.
Of the total 10,667 subjects who participated in this survey, depressive symptoms were assessed in 8,711 participants between 2005 and 2007. Among subjects in the analyses, we excluded 668 subjects with a self-reported history of cerebrovascular disease or coronary heart disease. We further excluded 228 subjects without information based on the Center for Epidemiologic Studies Depression (CES-D) Scale, 235 subjects without information regarding carotid ultrasonography, and 26 subjects with missing demographic data. In total, 7,554 subjects were included in the final analyses.
Depressive symptoms
Depressive symptoms were assessed by the CES-D Scale (18). The CES-D, a 20-item self-report questionnaire designed to measure depressive symptomatology in the general population, asks participants to report the frequency of being bothered by depressive symptoms experienced during the previous week on a 4-point scale (0 to 3 points). The total CES-D score ranged between 0 and 60, with higher scores indicating greater depressive symptoms. In this study, subjects with a total score of ≥16 were classified as having clinically significant depressive symptoms, and the remaining subjects served as controls (18).
Subclinical atherosclerosis
We measured carotid IMT and plaques using ultrasonography. The methods for carotid ultrasonography, image analysis and their reproducibility have been described previously (17). Briefly, two well-trained physicians used a high-resolution B-mode ultrasound (SONOACE 9900; Medison, Seoul, Korea) equipped with a 7.5-MHz linear array transducer. Using SigmaScan Pro, version 5.0.0 (SPSS Inc., Chicago, IL, USA), s single trained reader analyzed the still images according to a standardized protocol. In the longitudinal view, IMT was determined as the distance from the media-adventitia interface to the intima-lumen interface on the far wall in a plaque-free region. In the present study, the average of the maximum IMT of both common carotid artery and carotid bulb was defined as mean carotid IMT (C-IMT). The C-IMT above 1.0 mm was defined as abnormal C-IMT (19, 20). The presence of carotid plaques, defined as focal structures that encroached into the lumen by at least 100% of the surrounding IMT value, was determined from the scans of all carotid artery segments. The presence of carotid plaques was recorded if at least one lesion was detected in any segment in both carotid arteries. The correlation coefficients for between- and within-examiner variability of IMT were 0.86 and 0.90, respectively. The kappa coefficients were 0.76 for between-examiner agreement and 0.85 for within-examiner agreement for carotid plaques.
Covariates
Cigarette smoking, alcohol intake, self-reported medical history and medication use of each subject were assessed with a standardized questionnaire. Smoking status was classified into never a smoker, former smoker, and current smoker. Alcohol intake was assessed as the amount of ethanol consumed per day, which was calculated from the average number of alcoholic beverages consumed. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Blood pressure was measured on the right upper arm by using a mercury sphygmomanometer, with the subjects in the sitting position after a 5-min rest. Three consecutive readings of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded at a 1-min interval, and the average was used in the analysis. After a 12-hr overnight fast, venous blood samples were collected. Serum total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, fasting blood glucose (FBG) and uric acid (UA) levels were measured using the enzymatic method and were analyzed using an automatic analyzer (Hitachi 7600, Hitachi Ltd., Tokyo, Japan). High-sensitive C-reactive protein (hs-CRP) was measured by latex-enhanced nephelometry using a high-sensitivity assay analyzer (Behring Nephelometer II; Dade-Behring Diagnostics, Marburg, Germany).
Statistical analyses
All analyses were performed separately for males and females. Characteristics of the subjects with and without depressive symptoms were compared using the chi-square test for categorical variables and the Student's t-test for continuous variables. Correlation coefficients between C-IMT, carotid plaques, and CES-D score were evaluated. General linear model analyses were used to evaluate differences in C-IMT between subjects with and without depressive symptoms.
To examine the relationship between depressive symptoms and C-IMT, we dichotomized C-IMT as normal (<1.0 mm) or abnormal C-IMT (≥1.0 mm). Multiple logistic regression was used to evaluate the association between depressive symptoms and carotid atherosclerosis. Adjusted odds ratio (OR) and 95% confidence interval (CI) for carotid atherosclerosis according to dichotomous classification based on the CES-D cutoff score of 16 were compared. Logistic regression analysis was performed unadjusted (model 1); after adjustment for age, educational level, and marital status (model 2); after further adjustment for smoking status, alcohol intake, BMI, SBP, FBG, total/HDL cholesterol ratio, triglycerides, UA, hs-CRP, and antihypertensive and antidiabetic medications (model 3). All statistical analyses were performed using the PASW statistics 18.0 software package (SPSS Inc., Chicago, IL, USA).
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki guidelines. The study protocol was approved by the institutional review board of Chonnam National University Hospital (I-2007-07-062), and informed consent was obtained from each subject.
RESULTS
Baseline characteristics of the study population
The study population consisted of 3,019 males (40.0%) and 4,535 females (60.0%). The prevalence of current depressive symptoms (CES-D score≥16) was 7.9% for males and 18.7% for females. Characteristics of the study population according to depressive symptoms are shown in Table 1. Significant differences were found in the educational level, marital status and smoking status between subjects with and without depressive symptoms of both genders. BMI was significantly lower in subjects with depressive symptoms than subjects without depressive symptoms in both genders. Females with depressive symptoms were more likely to be older. While hs-CRP was significantly higher in males with depressive symptoms than in males without depressive symptoms, UA was significantly lower in females with depressive symptoms than in females without depressive symptoms.
Table 1.
Characteristics of the study population according to the presence of depressive symptoms
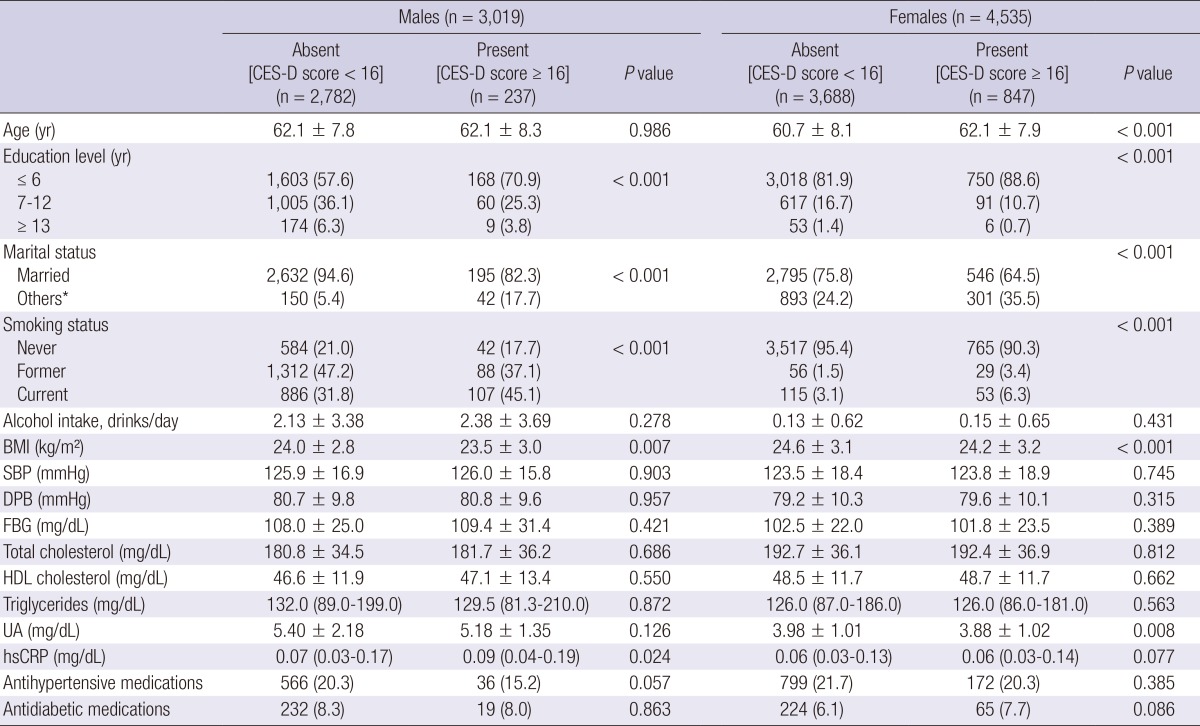
Data are expressed as means±standard deviation, medians (interquartile range) for skewed variables, or No.(%). *Unmarried, divorced, separated, or widowed. CES-D, the Center for Epidemiologic Studies Depression; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; HDL, high-density lipoprotein; UA, uric acid; hsCRP, high-sensitivity C-reactive protein.
Parameters of carotid atherosclerosis and depressive symptoms
The CES-D score was weakly and positively correlated with C-IMT in females (r=0.053) and borderline significantly correlated with C-IMT in males (r=0.035). No correlations between CES-D and carotid plaques were found in either gender. Weak-to-moderate correlations between C-IMT and carotid plaques were observed in males and females (r=0.128 and 0.122, respectively). Correlation analyses were performed after adjusting for age (Table 2).
Table 2.
Partial correlations between C-IMT, carotid plaques and CES-D score
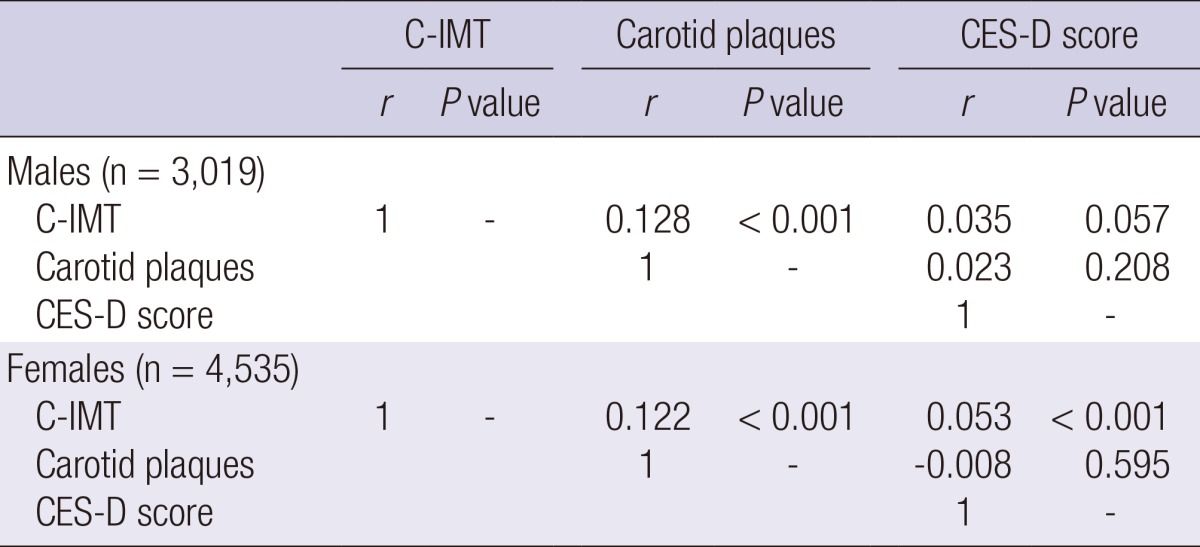
Adjusted for age. C-IMT, carotid intima-media thickness; CES-D, the Center for Epidemiologic Studies Depression.
Females with depressive symptoms had significantly greater C-IMT than females without depressive symptoms in the unadjusted model. The mean±standard deviation of C-IMT was 0.784±0.130 mm for females with depressive symptoms and 0.762±0.119 mm for females without depressive symptoms (P<0.001). After adjustment for established cardiovascular risk factors, the differences in C-IMT in females remained significant in models 2 and 3 (P=0.003 and 0.006, respectively). The mean difference in the C-IMT value in females was 0.011±0.004 mm (95% CI, 0.003-0.019 mm) after full adjustment.
In the unadjusted model, the mean±standard deviation of C-IMT was 0.822±0.139 mm for males with depressive symptoms and 0.814±0.127 mm for males without depressive symptoms (P=0.365). No significant difference in C-IMT was found between males with depressive symptoms and males without depressive symptoms in models 2 and 3 (P=0.314 and 0.421, respectively) (Table 3).
Table 3.
Differences in C-IMT between subjects with and without depressive symptoms
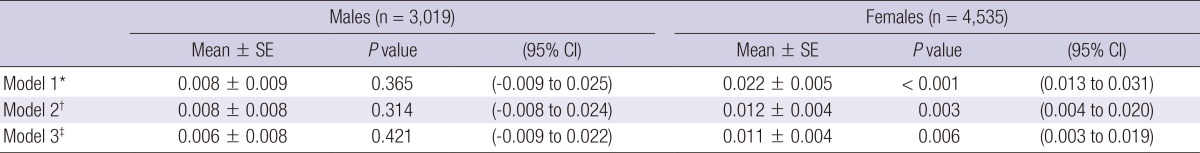
The mean difference between two groups (subjects of CES-D score≥16 minus subjects of CES-D score<16) was calculated using ANCOVA. *Unadjusted; †Adjusted for age, educational level, and marital status; ‡Further adjusted for smoking status, alcohol intake, body mass index, systolic blood pressure, fasting blood glucose, total/high-density lipoprotein cholesterol ratio, triglycerides, uric acid high-sensitive C-reactive protein, and antihypertensive and antidiabetic medications plus model 2. C-IMT, carotid intima-media thickness; CES-D, the Center for Epidemiologic Studies Depression.
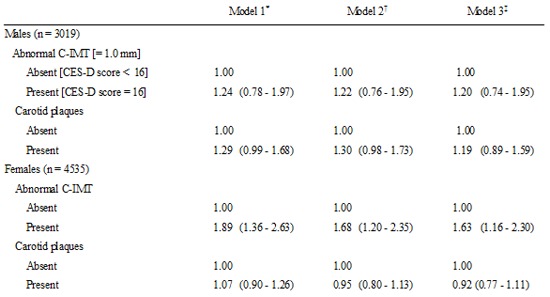
Relationship between depressive symptoms and carotid atherosclerosis
The relationship between depressive symptoms and subclinical carotid atherosclerosis is shown in Table 4. Compared with controls, the unadjusted risks (OR, 95% CI) of females with depressive symptoms for abnormal C-IMT (1.89, 1.36-2.63) was significant. Although additional adjustment for established cardiovascular risk factors slightly attenuated this relationship, depressive symptoms still remained as independent associations for abnormal C-IMT in females (1.68, 1.20-2.35 in model 2 and 1.63, 1.16-2.30 in model 3). Further adjustment for menopause and postmenopausal hormone therapy did not affect the significant association between depressive symptoms and C-IMT (data not shown). Conversely, no significant association between depressive symptoms and C-IMT was found in males (1.22, 0.76-1.95 in model 2 and 1.20, 0.74-1.95 in model 3). The association between depressive symptoms and carotid plaques was not statistically significant in either gender (Table 4).
Table 4.
Relationship between depressive symptoms and subclinical carotid atherosclerosis
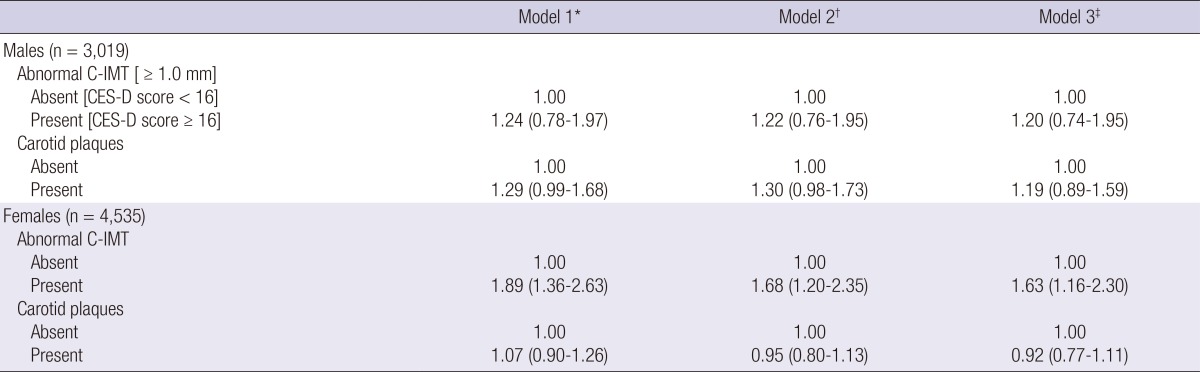
Data are presented as odds ratio (95% CI). *Unadjusted; †Adjusted for age, educational level, and marital status; ‡Further adjusted for smoking status, alcohol intake, body mass index, systolic blood pressure, fasting blood glucose, total/high-density lipoprotein cholesterol ratio, triglycerides, uric acid high-sensitive C-reactive protein, and antihypertensive and antidiabetic medications plus model 2. C-IMT, carotid intima-media thickness; CES-D, the Center for Epidemiologic Studies Depression.
DISCUSSION
This population-based cross-sectional study examined the association between clinically relevant depressive symptoms and subclinical carotid atherosclerosis among healthy community-dwelling Korean adults aged 45-74 yr. After adjustment for established cardiovascular risk factors, a high level of depressive symptoms as defined by a score of ≥16 on the CES-D scale was positively associated with C-IMT only in females. No significant association between depressive symptoms and carotid plaques was observed in either gender. Our findings suggest that a significant association between a high level of depressive symptoms and carotid atherosclerosis may exist, especially in females. These results support an underlying link between depression and subclinical carotid atherosclerosis.
Previous epidemiological studies have clearly demonstrated that depressive symptoms are related to the development of coronary heart disease, cerebrovascular disease and subsequent death (2, 3, 4, 5). Several pathophysiological, psychosocial, and behavioral mechanisms may explain the link between depressive symptoms and cardiovascular morbidity and mortality. The mechanisms include antidepressant cardiotoxicity, lower heart rate variability reflecting altered cardiac autonomic tone, increased platelet aggregation, inflammatory processes, unfavorable lifestyles and poor adherence to prevention and treatment regimens (21, 22).
In this study we measured established atherosclerotic indices, including C-IMT and carotid plaques, representing structural modifications of the vasculature in atherosclerosis. C-IMT and plaques reflect the development of systemic atherosclerosis. A number of epidemiological studies have demonstrated that these indices assessing extra-coronary atherosclerosis at different sites in the body are strong predictors of future cerebrovascular and cardiovascular events (8, 9).
Previous studies have evaluated the association of depression or depressive symptoms with C-IMT and plaques, although evidence is controversial. Tiemeier et al. showed that depressive disorders, not depressive symptoms, were associated with carotid IMT (10). Hamer et al. (11) observed that subjects with severe depressive symptoms had higher carotid IMT than did subjects with no symptoms. Another cross-sectional study of young adults showed that a significant relationship between depressive symptoms and carotid IMT was observed in males, but not in females (12). In contrast to the above study, we found a significant difference of C-IMT values only in females, after adjustment for known cardiovascular risk factors. Three longitudinal studies assessed the relationship of depressive symptoms and C-IMT. Haas et al. (13) reported that baseline depressive symptoms were independently predictive of carotid plaque among healthy employees in a 10-yr follow-up. Faramawi et al. (14) examined a significant association between depressive symptoms and the development of C-IMT in subjects aged 65 yr and older. Conversely, a longitudinal study of healthy community-dwelling participants showed no relationship between depressive symptoms and future C-IMT before or after adjustment for covariates (15).
In a cross-sectional study of middle-aged females, carotid plaque was associated with major depression, but not with current depressive symptoms (CES-D score ≥16) (23). No significant association of carotid plaque with depressive disorders or depressive symptoms was observed in another cross-sectional study of adults aged 60 yr and older (10). In agreement with previous research, our results showed no significant association between the presence of depressive symptoms and carotid plaques.
Although several studies have examined the gender difference in depressive symptoms and carotid atherosclerosis, whether a gender difference exists remains unclear. We observed a significant association between depressive symptoms and C-IMT only in females, suggesting a gender difference by association. Depressive symptoms are assumed to be significantly associated with carotid atherosclerosis in males, but not in females, because the protective effect of estrogen until menopause might delay the development of atherosclerosis (12). In our study, the significant association between depressive symptoms and C-IMT persisted after further adjustment for menopause and postmenopausal hormone therapy, suggesting that another mechanism is responsible for the link. More evidence is needed to confirm the gender-specific relationship between depressive symptoms and carotid IMT.
The mechanisms underlying the association between depressive symptoms and carotid atherosclerosis have not been established. However, several lines of evidence suggested that depression has both behavioral and pathophysiological effects that may increase the risk of cardiovascular disease in depressed individuals. Depressive subjects tend to have poor adherence to medical therapy and adverse health behaviors such as smoking, alcohol use, substance abuse, poor diet and low physical activity (24).
Our study has several strengths. First, a large number of community-dwelling elderly people participated in this study. Although atherosclerosis begins in childhood and progresses in subsequent decades (25), distinctive subclinical atherosclerotic changes to the arterial structure can be found in middle-aged and older adults. Therefore, the present study population being aged 45 yr and older may help to detect an association between depressive symptoms and subclinical carotid atherosclerosis. Second, this study showed the relationship between depressive symptoms and two non-invasive atherosclerotic indices simultaneously. Because each atherosclerotic index reflects a different aspect of atherosclerosis, overall consideration of atherosclerosis allowed clarification of the association between depressive symptoms and carotid atherosclerosis.
Several limitations of the present study exist. First, the cross-sectional design limited the ability to make causal inferences between depressive symptoms and atherosclerosis. Second, CES-D was measured at a single time point. Because the relationship between depressive symptoms and subclinical atherosclerosis is unlikely to be static, additional prospective studies examining the relationship between change in depressive symptoms and change in atherosclerotic parameters are needed to establish a temporal relationship. Because the Namwon Study is an ongoing population-based prospective study, repeat measurements can be performed at a later date. Third, we failed to evaluate the antidepressant medications, clinical diagnosis of depression, or the psychiatric history of participants. Additionally, no further psychiatric evaluations or interviews by psychologists or psychiatrists were performed in subjects with severe depressive symptoms. The relationship between clinical depressive disorder and atherosclerosis may actually be stronger than the relationship between depressive symptoms and carotid atherosclerosis observed in our study.
This study demonstrated a significant relationship between depressive symptoms and subclinical carotid atherosclerosis in middle-aged and older females, independent of known cardiovascular risk factors. Further cross-sectional and longitudinal research is needed to confirm the relationship between depressive symptoms and various subclinical atherosclerosis.
Footnotes
This study was supported by Wonkwang University in 2014.
There are no conflicts of interest to report.
References
- 1.World Health Organization. The world health report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization; 2002. [Google Scholar]
- 2.Yamanaka G, Otsuka K, Hotta N, Murakami S, Kubo Y, Matsuoka O, Takasugi E, Yamanaka T, Shinagawa M, Nunoda S, et al. Depressive mood is independently related to stroke and cardiovascular events in a community. Biomed Pharmacother. 2005;59:S31–S39. doi: 10.1016/s0753-3322(05)80007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66:305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 4.Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT, van Tilburg W. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58:221–227. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 6.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 7.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 8.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 9.Prati P, Tosetto A, Vanuzzo D, Bader G, Casaroli M, Canciani L, Castellani S, Touboul PJ. Carotid intima media thickness and plaques can predict the occurrence of ischemic cerebrovascular events. Stroke. 2008;39:2470–2476. doi: 10.1161/STROKEAHA.107.511584. [DOI] [PubMed] [Google Scholar]
- 10.Tiemeier H, van Dijck W, Hofman A, Witteman JC, Stijnen T, Breteler MM. Relationship between atherosclerosis and late-life depression: the Rotterdam Study. Arch Gen Psychiatry. 2004;61:369–376. doi: 10.1001/archpsyc.61.4.369. [DOI] [PubMed] [Google Scholar]
- 11.Hamer M, Malan NT, Harvey BH, Malan L. Depressive symptoms and sub-clinical atherosclerosis in Africans: role of metabolic syndrome, inflammation and sympathoadrenal function. Physiol Behav. 2011;104:744–748. doi: 10.1016/j.physbeh.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 12.Elovainio M, Keltikangas-Järvinen L, Kivimäki M, Pulkki L, Puttonen S, Heponiemi T, Juonala M, Viikari JS, Raitakari OT. Depressive symptoms and carotid artery intima-media thickness in young adults: the Cardiovascular Risk in Young Finns Study. Psychosom Med. 2005;67:561–567. doi: 10.1097/01.psy.0000170340.74035.23. [DOI] [PubMed] [Google Scholar]
- 13.Haas DC, Davidson KW, Schwartz DJ, Rieckmann N, Roman MJ, Pickering TG, Gerin W, Schwartz JE. Depressive symptoms are independently predictive of carotid atherosclerosis. Am J Cardiol. 2005;95:547–550. doi: 10.1016/j.amjcard.2004.10.032. [DOI] [PubMed] [Google Scholar]
- 14.Faramawi MF, Gustat J, Wildman RP, Rice J, Johnson E, Sherwin R. Relation between depressive symptoms and common carotid artery atherosclerosis in American persons > or =65 years of age. Am J Cardiol. 2007;99:1610–1613. doi: 10.1016/j.amjcard.2006.12.090. [DOI] [PubMed] [Google Scholar]
- 15.Rice SC, Zonderman AB, Metter EJ, Najjar SS, Waldstein SR. Absence of relation between depressive symptoms and carotid intimal medial thickness in the Baltimore Longitudinal Study of Aging. Psychosom Med. 2009;71:70–76. doi: 10.1097/PSY.0b013e3181865f73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whipple MO, Lewis TT, Sutton-Tyrrell K, Matthews KA, Barinas-Mitchell E, Powell LH, Everson-Rose SA. Hopelessness, depressive symptoms, and carotid atherosclerosis in women: the Study of Women's Health Across the Nation (SWAN) heart study. Stroke. 2009;40:3166–3172. doi: 10.1161/STROKEAHA.109.554519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kweon SS, Shin MH, Jeong SK, Nam HS, Lee YH, Park KS, Ryu SY, Choi SW, Kim BH, Rhee JA, et al. Cohort profile: the Namwon study and the Dong-gu study. Int J Epidemiol. 2014;43:558–567. doi: 10.1093/ije/dys244. [DOI] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 19.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. 1997;146:483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 20.Casella IB, Presti C, Porta RM, Sabbag CR, Bosch MA, Yamazaki Y. A practical protocol to measure common carotid artery intima-media thickness. Clinics (Sao Paulo) 2008;63:515–520. doi: 10.1590/S1807-59322008000400017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 22.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 23.Jones DJ, Bromberger JT, Sutton-Tyrrell K, Matthews KA. Lifetime history of depression and carotid atherosclerosis in middle-aged women. Arch Gen Psychiatry. 2003;60:153–160. doi: 10.1001/archpsyc.60.2.153. [DOI] [PubMed] [Google Scholar]
- 24.Kilbourne AM, Reynolds CF, 3rd, Good CB, Sereika SM, Justice AC, Fine MJ. How does depression influence diabetes medication adherence in older patients? Am J Geriatr Psychiatry. 2005;13:202–210. doi: 10.1176/appi.ajgp.13.3.202. [DOI] [PubMed] [Google Scholar]
- 25.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Ronnemaa T, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]


