Abstract
It has been proposed that high exercise loads increase the risk of infection, most frequently reported as upper respiratory tract infections, by suppressing the immune system. Most athletes will not train when experiencing sickness due to the fear of health complications. However, high training volumes are incompatible with high rates of non-training days, regardless of the cause. The purpose of this observational study was to examine the relationship between self-reported, exercise-constraining days of sickness (days when the athlete decided not to train due to symptoms of disease, either self-reported or by a physician) and the volumes of exercise training in elite endurance athletes by analyzing data from training logs kept for several years. The subjects included 11 elite endurance athletes (8 male, 3 female) competing at national and international levels in cross-country skiing, biathlon and long-distance running. Training logs available from these 11 subjects added to a total of 61 training years. The number of training hours per year (462, 79-856; median, range) was significantly and negatively correlated to the reported number of days not training due to sickness (15, 0-164) by a 3rd degree polynomial regression (R2 = 0.48, F ratio = 18, p < 0.0001). We conclude that elite endurance athletes can achieve high training volumes only if they also experience few sick-days.
Key points.
Top level performance demands high training volumes and intensities, which may compromise immune function.
Elite athletes must have an immune system capable of intact function also when under sever physiological and psychological stress.
Elite performance, especially in endurance sports, is therefore incompatible with a high rate of infections.
A negative correlation between infections and exercise training load among elite athletes is consequently observed – the less sick you are the more you can train.
Key words: Upper respiratory tract symptoms, infection, high volume training, immunosuppression
Introduction
High training intensities and volumes increase the risk of infection by impairing the immune function (Nieman, 2003; Nieman et al., 1989; 1990; Pedersen and Ullum, 1994; Peters and Bateman, 1983). Thus, elite athletes with high training intensities have a higher number of infectious episodes than recreational athletes and sedentary people (Gleeson and Walsh, 2012; Spence et al., 2007). However, in order to become an elite athlete absence of infections are important, and such findings may appear illogical (Malm, 2006). One issue in earlier studies has been that some conclusions regarding elite exercise training are based on non-elite athletes (Heath et al., 1991; Nieman et al., 1989; 1990) or on comparing athletes to non-athletes (Nieman et al., 2000). In addition, few studies have confirmed that pathogenic infections are present, but such studies have made statements that elite exercise training increases the odds ratio for an infection (Spence et al., 2007). Most athletes do not have the facilities required to carry out on-demand virus titers or establish bacterial cultures, and thus refrain from training based exclusively on self-diagnosis. The experience of these athletes thus makes the term Exercise Constrained Sick Days more appropriate. This can be defined as any day when the athlete chose not to train due to experienced symptoms of infections, self-reported or by a physician.
The relationship between the long term risk of URTI, immune function and exercise load is commonly modelled as a J-shaped curve with URTI on the y-axis and exercise load on the x-axis (Nieman, 1994a). This model suggests that sedentary individuals have a fixed risk of URTI, and that moderate exercise training decreases, while intense exercise training increases, the rate of URTI by a mechanism in which the immune system is modulated. Recently, support for this model was presented (Spence et al., 2007). The acute, repeated occurrence of impairment of immunity, the “open window” for infections to enter the body (Brines et al., 1996; Nieman, 1997; Pedersen and Bruunsgaard, 1995; Pedersen and Ullum, 1994) may result in a long-term increase in infection rates (the J-shaped curve).
We have previously shown that infection rates after a marathon increased only in subjects who had reported a pre-race infection (Ekblom et al., 2006). Consequently, we formed the hypothesis that the relationship between training and infection may form an S-curve when true elite athletes are included (Malm, 2006). Most studies have not differentiated between athletes with “high” and “elite” exercise loads, with the consequence that an incorrect definition of “elite” athletes has been used. We presented a pilot study data from one elite runner’s training log that covered 16 years (Malm, 2006), and concluded that an increased rate of infection is incompatible with a high training volume. These findings are in line with the recently published review article by Dhabhar (Dhabhar, 2014), where short term physical stress such as exercise, which is perceived as a positive event by the athlete, belongs to the immunoprotective response, enhancing survival and promoting enhanced physical performance.
The aim of this study was to test the hypothesis that exercise training loads are negatively correlated to the self-reported number of Exercise Constrained Sick Days.
Methods
Subjects
Male (N = 4) and female (N = 3) cross-country (XC) skiers, male biathletes (N = 2) and male long-distance runners (N = 2) completed the study. The inclusion criterion was that the athlete should have demonstrated “top national or international level performance in an endurance sports”. This does introduce a certain amount of subjectivity into whether the criterion was met, but all subjects were accepted as elite athletes to the School of Sports Science at Umeå University based on their competitive results from past years. Subjects were aged 17-24 years at the first year of reporting, and they reported a training period of 3-16 years. The number of observations of training years was 61 in all statistical calculations. A retrospective Power calculation was done (using the software G*power, version 3.1.3, www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3/) for Chi2 tests (goodness-of-fit for contingency tables) using an effect size of 0.3, p = 0.05, N = 61 and 2 degrees of freedom (between three levels of training volume) results in a Power of 0.54, while increasing the effect size to 0.5 gives a power of 0.95. Ethical permission (Ref. No. 2011-236-31M) was granted by the Regional Ethics Committee for northern Sweden, located at Umeå University. All subjects signed an informed consent form and the study was conducted in accordance with the WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects 2008. The study met also the ethical standards of IJSM (Harriss and Atkinson, 2011).
Procedure
Endurance athletes, who often keep rigorous records of their training, were asked to summarize their written training logbooks. Training volume (km or hours), the number of sick days and the number of days injured had to have been recorded for participation. Eleven endurance athletes’ training logs from the past 3-16 years (pending number of complete years recorded) met these criteria, and were summarized. Training logs are based on a daily subjective recordings, thus the definitions of “sick” and “injured” do not necessarily include examination by a physician, but always resulted in a no-training day. Consequently, the term self-reported Exercise Constrained Sick Days is used. Raw data from the training logs were summarized by the researchers in 12 month intervals as the sum of hours or kilometres of training, number of Exercise Constrained Sick Days due to sickness, and number of days injured (defined as trauma or over-use injuries) each year. Four subjects did not report the number of days injured in their training logs, without stating a reason for not reporting. A minimum of three years of reported training was required for inclusion. Two athletes (runners) summarized training in kilometres, which were transformed into training hours using an assumed average speed of 4 min 20 sec·km–1, for an elite distance runner or cross country skier, in which distance-training, interval-training and recovery running are averaged. Other variables, such as modes of training, diet, sleeping habits, travel schedules, medication, hygienic habits or other potential confounding factors were not taken into consideration. Dietary records and performance variables were not included. Subjects participated in the elite athletic program at the School of Sports Science, Umeå University, demanding at least a top national performance level. The authors have no conflicts of interest.
Statistical analysis
All statistical calculations were carried out in JMP 7.0.1 (SAS Institute Inc. Cary, NC, USA). We investigated correlations using third-degree polynomial regression fitting. The Exercise Constrained Sick Days data was not normally distributed, and thus the data was log-transformed before partition analysis. The 11 athletes had trained for a total of 61 years, with a span of 3-16 years. In order to investigate the correlation between training volume and the number of Exercise Constrained Sick Days, these 61 years were divided into three groups based on the number of Exercise Constrained Sick Days reported, using partition statistics (JMP 7.0.1). Partition was made to give 3 groups for which the differences between the groups was most significant (lowest p-value) when comparing number of training hours. We analysed the difference in number of training hours between the three groups using the non-parametric Kruskal-Wallis test. No adjustment for age was made. Due to the low number of subjects in each sport, and each sex, no further division of data, such as split between sports or sex, was done.
Results
The results demonstrate that the number of training days missed by an athlete due to self-reported sickness is negatively correlated to the volume of training in a mixed population of elite cross-country skiers, biathletes and long-distance runners.
Subjects reported a total of 61 training years, had trained an average of 462 (79-856) hours per year (median and range), were sick on 15 (0-164) days and injured on 21 (0-164) days. The number of training years reported was not significantly correlated to the number of self-reported Exercise Constrained Sick Days reported (R2 = 0.33, p = 0.16) (Table 1).
Table 1.
Group data on training volume and Exercise Constrained Sick Days in elite endurance athletes
| Training Group | #TY | MECSD | 10th and 90th percentile |
|---|---|---|---|
| < 266 h/year | 12 | 54 | 18 and 160 |
| 266 - 538 h/year | 27 | 17 | 6 and 57 |
| > 538 h/year | 22 | 8 | 0 and 27 |
#TY: Number of training years included. MECSD: Median Exercise Constrained Sick Days
Training years are ranked from 1-61 according to the number of training hours per year in Figure 1 (x-axis) and plotted against the number of Exercise Constrained Sick Days and the number of training hours in a dual y-axis graph. Figure 1 shows that the number of training hours per year is inversely correlated with the number and variation in Exercise Constrained Sick Days.
Figure 1.
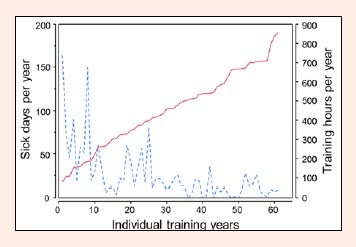
Sick days per year on left y-axis (solid line) and Training hours per year on right y-axis (dashed line) plotted against Individual training years on the x-axis. The variation in the number of sick days falls at approximately 400 training hours, indicating that, the number of sick days per year must be below 50 in order to train more than 400 hours per year.
A 3rd degree polynomial equation was derived (R2 = 0.48, p < 0.0001):
| S = 37.5 - 0.048 * T + 0.00027*(T-453)2 - 5.6*10–7*(T-453)3 |
where S is the number of sick days and T is the amount of training in hours.
This function is plotted in Figure 2 as a solid line, with the area between the 95% Confidence Intervals (CI) coloured grey and the 95% CI for individual data points shown as dashed lines (Figure 2).
Figure 2.
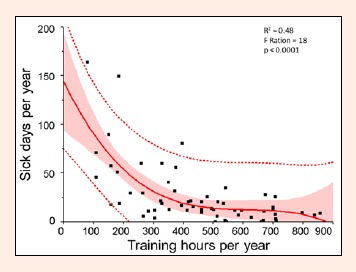
A third-degree polynomial bivariate fit (solid line) of Sick days per year (y-axis) and Training hours per year (x-axis) shows a significant (R2 = 0.48, F Ratio = 18, p < 0.0001, N = 61 training years from 11 subjects) decrease in the number of sick days reported as the number of hours of training increases. The shaded area indicates the 95% CI of the model and the dashed lines indicate the 95% CI for the individual data points.
The dataset of 61 individual training years was divided into three groups based on the number of completed hours of training using partition statistics to obtain the maximum significance of the differences in the number of ECDs between groups (Table 1). The skewness was 2.65, and thus it was necessary to carry out log-transformation of the ECD data. Loge (ECD) was then plotted along the y-axis for the three groups (plotted as x-variable). Partition using Log transformed sick-days data resulted in three groups; training less than 266 h/year (N = 12), training 266-538 h/year (N = 27) and training more than 538 h/year (N = 22). The non-parametric Kruskal-Wallis test on non-transformed data gave Chi2 = 27, p < 0.0001 when comparing number of sick days between the three training groups, with median ECDs at 54 (10th percentile = 18, 90th percentile = 160), 17 (6, 57) and 8 (0, 27), respectively.
Discussion
Our results demonstrate that a high training load is accompanied by a low incidence of days of training lost due to self-reported days of sickness, and is compatible with our previous suggestion (Malm, 2006).
Our findings agree with those of Moreira et al. (Moreira, Delgado, Moreira and Haahtela, 2009) in which a combination of the classic J-curve proposed by Nieman (1994a) and the S-curve proposed by Malm (2006) was presented. The combined model suggests that the risk of sickness in less-fit individuals can be displayed as a J-curve, while the curve tends to flatten as fitness increases. Moderate physical activity lowers the risk for infection in non-athletic adults from that of inactive adults, which is reflected in the J-curve nature of the results for such subjects (Nieman, 1994b; Nieman et al., 2011). It may be necessary to separate less-fit individuals from well-trained individuals when interpreting the effects of exercise on infection (Matthews et al., 2002), because of the demonstrated increased self-reported upper respiratory tract infection in elite, compared to recreational athletes (Gleeson et al., 2013)
Many studies have examined endurance running events such as marathons, and report that there is an increased risk of acquiring an infection in the weeks following such an event. However, Ilback et al. (1991) (in rats) and Ekblom et al. (2006) (in humans) have shown that pre-effort infection is the probable cause of the increase in post-effort infection rates, not the post-effort sensitivity to infections.
The present study did not investigate immune function, but others have reported a different immune response in elite compared to sedentary individuals (Walsh et al., 2011). Different inclusion criteria could therefore partly explain the difference in results between the present and previous (Nieman, 1994a; 1994b) studies.
It can be argued that an immune system capable of fighting infection also during and after repetitive, strenuous exercise is necessary in order to become a successful elite athlete. Thus, measurements of infection rates in elite athletes are biased due to positive selection, and this could explain the S-curve/flattened J-curve (Malm, 2006). Elite athletes, such as the participants in this study, have the ambition to train every healthy day, and thus more training hours can be completed in years with fewer infections. These arguments are not in contradiction to such findings as by Spence et al. (Spence et al., 2007), showing that elite athletes have higher reported episodes of infections than non-elite subjects. All athletes participating in the present study performed at an elite level in their sport, and had the ambition to reach high training volumes every year in order to compete on a national and international elite level; they were all accepted to the School of Sports Science at Umeå University. However, because of infections, they were not able to reach their goals every season, manifested as the data points at the low end of Training hours per year in Figure 2. Thus, the argument that infections caused low training volumes, may be equally valid as the opposite; that high training volumes will cause infections. The latter being practically and statistically impossible, as 500-800 training hours per year will demand very few sick days, regardless cause and pathology. Consequently, a large variation in the number of sick days will be present in any study including elite athletes, unless a biased selection of only health elite subjects is done.
The results in the present study do not by any means explain the cause, but are in line with our pilot study (Malm, 2006) as well as our conclusion regarding infection rates in marathon runners (Ekblom et al., 2006); In elite athletes, exercise load is negatively correlated with self-diagnosed Exercise Constrained Sick Days. A recent review by Moreira et al. (2009) also conclude that “among elite athletes, the relationship between exercise load and immune dysfunction tends to flat”. The demands associated with elite sports require an immune system that is capable of fighting off infections also in situations with extreme physical and mental challenges.
Because this study is based on retrospectively summarize training logs, self-reported sickness, and a relatively few athletes, future studies should include a much larger number of subjects, as well as pathogen identification to investigate the mechanisms that govern the immunological response and clinical outcome of exercise training and competition. Of interested would also be to correlate sick days and training volumes to diet, performance and other co-founding factors in a prospective approach. This could benefit our understanding not only of the mechanisms behind the function of the immune system, and its adaptation in elite athletes, but also the clinical application of exercise to optimize both immune function and performance.
Perspective
Elite athletes are individuals in pursuit of reaching their genetic limits of physical performance. They encounter numerous obstacles on this pathway, injuries and disease being two of the most common. This study makes a simple, but not scientifically published, observation that minimizing the number of Exercise Constrained Sick Days is a key issue for high training volumes in elite athletes, whose key to winning is maintained health.
Conclusion
In elite athletes, high training volumes are incompatible with a high number of non-training days, regardless of cause. Consequently, the correlation between the number of sick days and training hours was found to be negative.
Biographies

Sandra MÅRTENSSON
Employement
Sports Medicine Unit, Umeå University, Sweden
Degree
BSc
Research interest
Infection risk and elite athletes. Currently working with health maintenance, exercise training and diet.
E-mail: sandravm88@hotmail.com

Kristina NORDEBO
Employement
Sports Medicine Unit, Umeå University, Sweden
Degree
MS
Research interest
Infections and adaptations to exercise.
E-mail: k_nordebo@hotmail.com

Christer MALM
Employement
Assoc. Prof., Sports Medicine Unit, Umeå University, Sweden
Degree
PhD
Research interest
Muscle adaptation to exercise, immune function, physical performance and testing.
E-mail: christer.malm@umu.se
References
- Brines R., Hoffman-Goetz L., Pedersen B.K. (1996) Can you exercise to make your immune system fitter? Immunology Today 17(6), 252-254 [DOI] [PubMed] [Google Scholar]
- Dhabhar F.S. (2014) Effects of stress on immune function: the good, the bad, and the beautiful. Immunology Research 58(2-3), 193-210. [DOI] [PubMed] [Google Scholar]
- Ekblom B., Ekblom O., Malm C. (2006) Infectious episodes before and after a marathon race. Scandinavian Journal of Medicine and Science in Sports 16(4), 287-293. [DOI] [PubMed] [Google Scholar]
- Gleeson M. (2007) Immune function in sport and exercise. Journal of Applied Physiology 103(2), 693-699. [DOI] [PubMed] [Google Scholar]
- Gleeson M., Bishop N., Oliveira M., Tauler P. (2013) Influence of training load on upper respiratory tract infection incidence and antigen-stimulated cytokine production. Scandinavian Journal of Medicine and Science in Sports 23(4), 451-457. [DOI] [PubMed] [Google Scholar]
- Gleeson M., Walsh N.P. (2012) The BASES expert statement on exercise, immunity, and infection. Journal of Sports Science 30(3), 321-324. [DOI] [PubMed] [Google Scholar]
- Harriss D.J., Atkinson G. (2011) Update - ethical standards in sport and exercise science research. International Journal of Sports Medicine 32(11), 819-821. [DOI] [PubMed] [Google Scholar]
- Heath G.W., Ford E.S., Craven T.E., Macera C.A., Jackson K.L., Pate R.R. (1991) Exercise and the incidence of upper respiratory tract infections. Medicine and Science in Sports and Exercise 23(2), 152-157. [PubMed] [Google Scholar]
- Ilback N.G., Crawford D.J., Neufeld H.A., Friman G. (1991) Does exercise stress alter susceptibility to bacterial infections? Uppsala Journal of Medicine and Science 96(1), 63-68 [DOI] [PubMed] [Google Scholar]
- Malm C. (2006) Susceptibility to infections in elite athletes: the S-curve. Scandinavian Journal of Medicine and Science in Sports 16(1), 4-6. [DOI] [PubMed] [Google Scholar]
- Matthews C.E., Ockene I.S., Freedson P.S., Rosal M.C., Merriam P.A., Hebert J.R. (2002) Moderate to vigorous physical activity and risk of upper-respiratory tract infection. Medicine and Science in Sports and Exercise 34(8), 1242-1248. [DOI] [PubMed] [Google Scholar]
- Moreira A., Delgado L., Moreira P., Haahtela T. (2009) Does exercise increase the risk of upper respiratory tract infections? British Medical Bulletin 90, 111-131. [DOI] [PubMed] [Google Scholar]
- Nieman D.C. (1994a) Exercise, infection, and immunity. International Journal of Sports Medicine 15 (Suppl 3), S131-141. [DOI] [PubMed] [Google Scholar]
- Nieman D.C. (1994b) Exercise, upper respiratory tract infection, and the immune system. Medicine and Science in Sports and Exercise 26(2), 128-139. [DOI] [PubMed] [Google Scholar]
- Nieman D.C. (1997) Risk of upper respiratory tract infection in athletes: An epidemiologic and immunologic perspective. Journal of Athletic Training 32(4), 344-349. [PMC free article] [PubMed] [Google Scholar]
- Nieman D.C. (2003) Current perspective on exercise immunology. Current Sports Medicine Reports 2(5), 239-242. [DOI] [PubMed] [Google Scholar]
- Nieman D.C., Henson D.A., Austin M.D., Sha W. (2011) Upper respiratory tract infection is reduced in physically fit and active adults. British Journal of Sports Medicine 45(12), 987-992. [DOI] [PubMed] [Google Scholar]
- Nieman D.C., Johanssen L.M., Lee J.W. (1989) Infectious episodes in runners before and after a roadrace. Journal of Sports Medicine and Physical Fitness 29(3), 289-296. [PubMed] [Google Scholar]
- Nieman D.C., Johanssen L.M., Lee J.W., Arabatzis K. (1990) Infectious episodes in runners before and after the Los Angeles Marathon. Journal of Sports Medicine and Physical Fitness 30(3), 316-328. [PubMed] [Google Scholar]
- Nieman D.C., Nehlsen-Cannarella S.L., Fagoaga O.R., Henson D.A., Shannon M., Hjertman J.M., Schmitt R.L., Bolton M.R:, Austin M.D., Schling B.K., Thorpe R. (2000) Immune function in female elite rowers and non-athletes. British Journal of Sports Medicine 34(3), 181-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen B.K., Bruunsgaard H. (1995) How physical exercise influences the establishment of infections. Sports Medicine 19(6), 393-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen B.K., Ullum H. (1994) NK cell response to physical activity: possible mechanisms of action. Medicine and Science in Sports and Exercise 26(2), 140-146. [DOI] [PubMed] [Google Scholar]
- Peters E.M., Bateman E.D. (1983) Ultramarathon running and upper respiratory tract infections. An epidemiological survey. South African Medical Journal 64(15), 582-584. [PubMed] [Google Scholar]
- Spence L., Brown W.J., Pyne D.B., Nissen M.D., Sloots T.P., McCormack J.G., Locke A.S., Fricker P.A. (2007) Incidence, etiology, and symptomatology of upper respiratory illness in elite athletes. Medicine and Science in Sports and Exercise 39(4), 577-586. [DOI] [PubMed] [Google Scholar]
- Walsh N.P., Gleeson M., Pyne D.B., Nieman D.C., Dhabhar F.S., Shephard R.J., Oliver S.J., Bermon S., Kajeniene A. (2011) Position statement. Part two: Maintaining immune health. Exercise Immunology Review 17, 64-103. [PubMed] [Google Scholar]


