Abstract
As cesarean rates have climbed to almost one-third of all births in the United States, current research and professional organizations have identified letting labor begin on its own as one of the most important strategies for reducing the primary cesarean rate. At least equally important, letting labor begin on its own supports normal physiology, prevents iatrogenic prematurity, and prevents the cascade of interventions caused by labor induction. This article is an updated evidence-based review of the “Lamaze International Care Practices That Promote Normal Birth, Care Practice #1: Let Labor Begin on Its Own,” published in The Journal of Perinatal Education, 16(3), 2007.
Keywords: let labor begin on its own, labor induction, hormonal preparation for birth
It can be argued that the most powerful way in which we can support the normal physiology of labor and birth is to let labor begin on its own. Virtually, every definition and consensus statement on normal birth begins with “spontaneous onset of labor” (see Table 1).
TABLE 1. Normal Birth Definitions.
| Source | Definition or statement |
| American midwives (Supporting Healthy and Normal Physiologic Childbirth: A Consensus Statement by ACNM, MANA, and NACPM [American College of Nurse-Midwives, Midwives Alliance of North America, National Association of Certified Professional Midwives, 2012]) | Normal physiologic childbirth is characterized by spontaneous onset and progression of labor. |
| Canadian obstetricians, obstetric nurses, midwives, family physicians, and rural physicians (Joint Policy Statement on Normal Childbirth [Society of Obstetricians and Gynaecologists of Canada, Association of Women’s Health, Obstetric and Neonatal Nurses of Canada, Canadian Association of Midwives, College of Family Physicians of Canada, Society of Rural Physicians of Canada, 2008]) | A normal birth is spontaneous in onset. |
| English obstetricians, midwives, and childbirth educators (Making Normal Birth a Reality—Consensus Statement From the Maternity Care Working Party [National Childbirth Trust, Royal College of Midwives, Royal College of Obstetricians and Gynaecologists, 2007]) | The “normal delivery” group includes women whose labor starts spontaneously. |
| World Health Organization (Care in Normal Birth—A Practical Guide, 1996) | We define normal birth as: spontaneous in onset. |
This article is an updated evidence-based review of the “Lamaze International Care Practices That Promote Normal Birth, Care Practice #1: Let Labor Begin on Its Own,” published in The Journal of Perinatal Education, 16(3), 2007.
Yet in a recent survey of American women who gave birth in a 1-year period from July 2011 to June 2012, less than half of the women surveyed allowed labor to begin on its own (Declercq, Sakala, Corry, Applebaum, & Herrlich, 2013). Cesarean rates have increased in the United States from about 23% in 1990 to almost 33% in 2013 (Hamilton, Martin, Osterman, & Curtin, 2014). With the vaginal birth after cesarean rate at only about 10% (Osterman & Martin, 2014), most women with previous cesarean surgeries go on to have scheduled repeat cesarean births in subsequent pregnancies. The Centers for Disease Control and Prevention (CDC) also reports that the induction rate has more than doubled from less than 10% in 1990 to almost 23% in 2012 (Martin, Hamilton, Osterman, Curtin, & Mathews, 2013). A troubling concern for childbirth educators and other birth professionals is that the survey also revealed that American women do not have accurate information on which to make informed decisions. Almost 60% of the women surveyed wrongly believed that macrosomia is an appropriate indication for induction of labor, and almost 30% of the women wrongly thought that induction lowers the risk for cesarean surgery.
This article will review the importance of allowing labor to begin on its own for a safe and healthy birth and the risks associated with labor induction.
SUPPORTING NORMAL PHYSIOLOGY
The most compelling reason to let labor begin on its own may be to allow the birth hormones to regulate labor and birth, breastfeeding, and attachment as nature intends. Most childbirth educators and other birth professionals are familiar with the important roles which the four main birth hormones—oxytocin, endorphins, catecholamines, and prolactin—play in regulating labor and birth, breastfeeding, and attachment. But an important new report by Dr. Sarah Buckley (2014) also details the critical roles that these four hormones play in preparing both mother and baby for labor and birth.
Oxytocin
Both the blood levels of oxytocin and the number of oxytocin receptors throughout the mother’s body increase as pregnancy advances. However, final surges in oxytocin and oxytocin receptors may not occur until the final days before the spontaneous start of labor (Buckley, 2014). Letting labor begin on its own with the optimal number of oxytocin receptors and optimal levels of natural oxytocin on board increases the likelihood that labor and birth will progress successfully and that breastfeeding and attachment will get off to the best possible start.
In animal studies, there is a surge of maternal oxytocin in the 24 hr around the time of spontaneous labor (Ceanga, Spataru, & Zagrean, 2010). This surge of oxytocin is thought to transfer to the fetal brain via the placenta and the immature blood–brain barrier of the fetus. The oxytocin reduces oxygen requirements in the fetal brain, thus providing a neuroprotective effect for the fetal brain during labor. Animal studies also indicate that administration of high levels of synthetic oxytocin reduce this neuroprotective effect and may increase fetal vulnerability to low levels of oxygen. The increased vulnerability to hypoxia with the administration of synthetic oxytocin may be one piece of the puzzle in explaining the association between labor induction and increased cases of cerebral palsy reported in Norway (Elkamil et al., 2011) and the association between labor induction and autism reported in North Carolina (Gregory, Anthopolos, Osgood, Grotegut, & Miranda, 2013).
The most compelling reason to let labor begin on its own may be to allow the birth hormones to regulate labor and birth, breastfeeding, and attachment as nature intends.
The reduced amount of natural oxytocin and reduced number of oxytocin receptors in women who do not allow pregnancy to proceed until spontaneous labor begins, in addition to the effect of overloading oxytocin receptors caused by the administration of synthetic oxytocin, may help explain the increased incidence of postpartum hemorrhage in women who are induced or augmented with synthetic oxytocin (Belghiti et al., 2011; Grotegut et al., 2011; Rooks, 2009).
Endorphins
Like oxytocin and oxytocin receptors, levels of endorphins and the number of endorphin receptors also gradually increase during pregnancy. Research has shown that women who exercise regularly have higher levels of endorphins when they go into labor and report less labor pain than women who do not exercise regularly (Varrassi, Bazzano, & Edwards, 1989). Letting labor begin on its own and exercising regularly throughout pregnancy will allow women to begin labor with optimal levels of endorphins.
Catecholamines
Fetal catecholamines also increase a few days before the spontaneous start of labor. Catecholamines play a critical role in readying the fetal lungs for air breathing immediately after birth by reducing the amount of fluid in the lungs (Jain, 2006; Jain & Eaton, 2006). Newborns who do not have this advantage because of scheduled cesarean surgery or induction of labor are at higher risk for respiratory problems at birth and admission to the neonatal intensive care unit (NICU; Buckley, 2014).
Prolactin
In her report, The Hormonal Physiology of Childbearing, Dr. Buckley (2014) describes studies that show that prolactin levels, such as those of oxytocin and endorphins, increase throughout pregnancy, with steep increases at term. In animal studies, there is a large increase in prolactin receptors the day before the onset of spontaneous labor. Not only is prolactin critical in establishing breastfeeding, but it is also thought that late-gestation prolactin plays a role in helping fetal lungs to mature and in helping the baby to regulate his or her temperature after birth.
SUMMARY OF THE IMPORTANCE OF ALLOWING LABOR TO BEGIN ON ITS OWN ON BIRTH PHYSIOLOGY
With levels of endorphins gradually increasing throughout pregnancy and levels of oxytocin, catecholamines, and prolactin sharply increasing around the time of the spontaneous onset of labor, it is clear that waiting for labor to begin on its own will result in both the mother and the fetus having ideal levels of these critical birth hormones. With optimal levels of the birth hormones, the baby is physiologically ready for extrauterine life, labor is more likely to progress well, breastfeeding is easier and more successful, and attachment is enhanced.
WHAT ARE THE RISKS OR HARMS OF NOT LETTING LABOR BEGIN ON ITS OWN?
The three most important risks of not letting labor begin on its own are interfering with the hormones that regulate pregnancy, labor, birth, breastfeeding, and attachment (discussed earlier); iatrogenic prematurity; and initiating the cascade of interventions.
Iatrogenic Prematurity
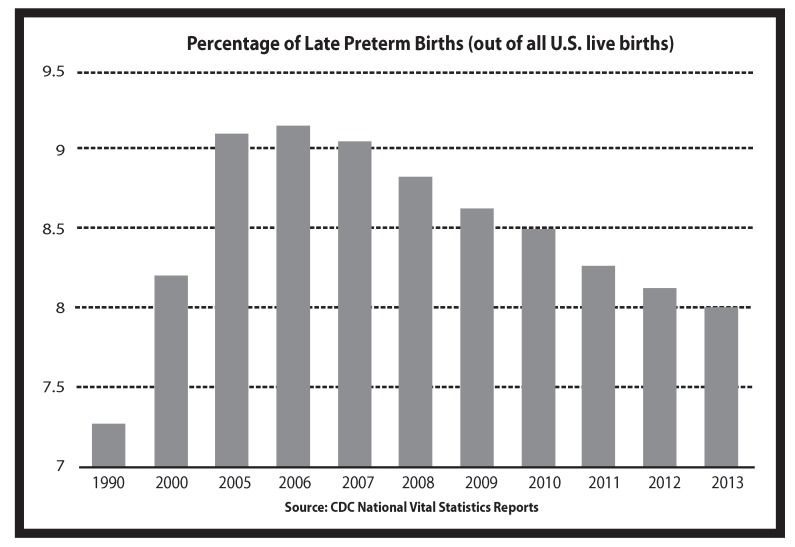
In an analysis of the dramatic increase in the percentage of late preterm births between 1990 and 2006 in the United States, epidemiologists for the National Center for Health Statistics stated that, “studies suggest that the increasing use of induction of labor and cesarean delivery at 34–36 weeks has influenced the upswing in the late preterm birth rate” (Martin, Kirmeyer, Osterman, & Shepherd, 2009, pp. 5–6). As evidence mounted of the increased risks to babies born late preterm (Tomashek, Shapiro-Mendoza, Davidoff, & Petrini, 2007), the Joint Commission in 2010 asked hospitals to voluntarily report the number of elective births before 39 weeks as one of the perinatal quality measures. The good news is that since 2006, the percentage of late preterm births has slowly decreased each year (see Figure 1). In 2013, the rate was 8% (Hamilton et al., 2014), better than the 2006 rate of 9.15% but still well higher than the 1990 rate of 7.3%. As of January 1, 2014, the Joint Commission perinatal quality measure to report elective births before 39 weeks is required for all hospitals with 1,100 births or more per year. Many hospitals have banned all elective births before 39 weeks.
FIGURE 1.
Late preterm birth rates.
There are two reasons why babies whose births are scheduled ahead of time may be born too early. One reason is that due dates are not exact. Engle (2006) found that prenatal methods for estimating gestational age have a margin of error of ± 2 weeks. Current guidelines report a consistent 8% margin of error for establishing gestational age based on ultrasound. This is calculated against the number of days of gestation so that at 8 weeks, the margin of error is ± 5 days; at 18 weeks, the margin of error is 10 days; and at 28 weeks, the margin of error increases to almost 16 days (Hunter, 2009). If the due date is estimated incorrectly and the birth is scheduled ahead of time, it is possible that the baby will be born late preterm or early term.
Many childbearing women in the United States do not understand how important it is for babies to be born full term. In the Listening to Mothers III survey, mothers were asked to identify the earliest week when it is safe for a baby to be born provided that there are no complications requiring early birth. Only 21% of the mothers chose the correct answer of 39 weeks or later. Thirty-five percent of the women chose 37–38 weeks, whereas 44% chose 34–36 weeks or less.
Risks for Late Preterm Babies
In a review of the literature published in 2010, researchers found that babies born “late preterm” (between 34 and 37 weeks) are at higher risk for respiratory distress, apnea, temperature instability, hypoglycemia, jaundice, and feeding difficulty (Loftin et al., 2010). A sobering statistic is that a baby born late preterm is three times more likely to die in the first year of life than a baby born full term (Mathews & MacDorman, 2013). In addition to increased morbidity and mortality, there is evidence that babies born late preterm are at increased risk for developmental delays and problems in school. Researchers in Florida looked at long-term effects of late preterm birth and found that even healthy late preterm infants compared with healthy term infants are at greater risk for developmental delay and school-related problems up to the first 5 years of life (Morse, Zheng, Tang, & Roth, 2009).
Risks for Early-Term Babies
Even babies born just a few weeks early are at higher risk for increased mortality and morbidity. CDC researchers found that babies born early-term (37–38 weeks) have mortality rates that were two-thirds higher than those born 39–41 weeks’ gestation (Mathews & MacDorman, 2013). According to the American College of Obstetricians and Gynecologists (ACOG; 2013b), babies born at 37–38 weeks’ gestation are at increased risk for respiratory distress syndrome, transient tachypnea, ventilator use, pneumonia, respiratory failure, NICU admission, hypoglycemia, 5-min Apgar scores lower than 7, and neonatal mortality.
In addition to estimating the due date incorrectly, the other reason that scheduling the baby’s birth ahead of time may result in a baby who is born “too early” is that there appears to be a wide variation in the length of human gestation. In a prospective cohort study published in Human Reproduction in 2013, researchers followed 221 healthy women with no known fertility problems who discontinued contraception to become pregnant (Jukic, Baird, Weinberg, McConnaughey, & Wilcox, 2013). The women kept diaries and collected daily first morning urine specimens for 6 months or through the eighth week past their last menstrual periods if they conceived. Researchers measured hormone levels in the urine specimens to determine the exact date of ovulation. There were 130 conceptions during the study that resulted in singleton live births. After exclusions, including for preterm births, researchers found that ovulation-based gestation ranged from 247 to 284 days—a span of 37 days or more than 5 weeks. Using the traditional method of dating pregnancies from the last menstrual cycle, the pregnancies lasted from a little more than 37 weeks to a little more than 42 1/2 weeks. Although researchers cautioned that results may not be generalizable to more diverse populations, they recommended that a pregnant woman be given a range of due dates rather than just one specific day.
Many scientists now believe that it is the baby who initiates the labor process. When all the baby’s organs are fully mature and the baby is ready for life outside the uterus, he releases a small amount of a protein that initiates labor in the mother (Condon, Pancharatnam, Faust, & Mendelson, 2004). This does not happen until critical growth and maturation take place in the baby’s brain and lungs during the last weeks of pregnancy.
When all the baby’s organs including the baby’s brain, which grows dramatically in the last weeks of pregnancy, and the late-maturing fetal lungs are fully mature and the baby is ready for life outside the uterus, the baby releases a small amount of a protein which initiates labor in the mother.
Thus, in most cases, the best way to know that the baby is fully mature is to wait for the baby to initiate the labor process. With a possible natural 5-week variation in the length of normal gestation, some babies may be fully mature at 38 weeks and ready for life outside the womb, whereas others need a few more weeks to become fully mature at 40 or even 42 weeks.
Initiating the Cascade of Interventions
There are risks associated with most methods of labor induction, and the induction routinely requires additional medical interventions.
Swiss researchers recently compared obstetrical and neonatal outcomes in elective and medically indicated labor inductions done at term (Baud, Rouiller, Hohlfeld, Tolsa, & Vial, 2013). Both groups were also compared to women with spontaneous onset of labor. They found no significant differences in outcomes between the elective and medically indicated induction groups. Compared to women with spontaneous onset of labor, women who were induced at term were at greater risk for cesarean surgery, instrumental birth, postpartum hemorrhage of more than 500 ml, and prolonged maternal hospitalization (more than 6 days). The babies of the mothers who were induced were at greater risk of arterial umbilical cord pH of lower than 7.1, admission to the NICU, and prolonged NICU hospitalization (more than 7 days).
Labor is often induced by administering intravenous (IV) synthetic oxytocin (known as Pitocin in the United States and Canada). IV Pitocin is one of only 10 specific medications named to the “high-alert” list by the Institute for Safe Medication Practices (ISMP; 2012). According to ISMP, high-alert medications are drugs that bear a heightened risk of causing significant patient harm when they are used in error. Indeed, approximately half of all paid obstetric litigation claims involve allegations of oxytocin misuse (Rooks, 2009).
At the 2013 ACOG Annual Clinical Meeting, Dr. Michael Tsimis presented a retrospective analysis of deliveries that were either induced or augmented with Pitocin. The study included more than 3,000 women giving birth to full-term infants from 2009 to 2011 at Beth Israel Hospital in New York City. Researchers found that induction and augmentation with Pitocin was an independent risk factor for full-term babies for unexpected admission to the NICU lasting more than 24 hr. Augmentation with Pitocin also correlated with Apgar scores of lower than 7 at 5 min. A press release from ACOG (2013c) notes that “the analysis suggests that oxytocin use may not be as safe as once thought and that proper indications for its use should be documented for further study” (para. 6).
IV fluids are required when labor is induced with IV Pitocin. Because there is an increased risk for uterine tachysystole and neonatal morbidity with the administration of Pitocin, continuous electronic fetal monitoring (EFM) is also required. The combination of IV fluids and continuous EFM limits the ability of the laboring woman to move and change positions and her choice of comfort measures. Pitocin-generated contractions may peak more quickly and last longer than natural contractions, increasing the likelihood that the laboring mother will request epidural analgesia for pain relief. With epidurals, there are increased risks for the need for urinary catheterization and instrumental birth. Epidurals are also associated with the development of maternal fever during labor, which can lead to separation of mother and baby after birth and testing and antibiotic administration for the baby (Greenwell et al., 2012; Leighton & Halpern, 2002; Lieberman & O’Donoghue, 2002; Wassen et al., 2014).
Although there is some controversy about the association of labor induction and the risk for cesarean surgery, numerous studies have concluded that induction increases the risk of cesarean surgery for first-time mothers (Burgos et al., 2012; Dunne, Da Silva, Schmidt, & Natale, 2009; Ehrenthal, Jiang, & Strobino, 2010; Levine, Hirshberg, & Srinivas, 2013; Rattigan, Atkinson, & Baum, 2013). In their 2009 practice bulletin on induction of labor, ACOG (2009) advises obstetricians that “nulliparous women undergoing induction of labor with unfavorable cervices should be counseled about a two-fold increased risk of cesarean delivery” (p. 389).
GUIDELINES FROM PROFESSIONAL ORGANIZATIONS
The Joint Commission, which accredits hospitals in the United States, now requires that all hospitals with more than 1,100 births per year report the number of elective births before 39 weeks, with a goal of eliminating such births.
Almost all professional organizations of health-care providers, both in the United States and worldwide, now recommend induction of labor only for medical reasons. In February 2014, the ACOG and the Society of Maternal-Fetal Medicine (SMFM) issued a consensus statement in which they said that inductions should generally only be done only for medical indications before 41 weeks’ gestation (ACOG, 2014).
WHEN SHOULD LABOR BE INDUCED?
According to the ACOG, the following are examples of medical indications for late preterm or early-term births:
-
•
Preeclampsia, eclampsia, gestational hypertension, or complicated chronic hypertension
-
•
Oligohydramnios
-
•
Prior classical cesarean birth or prior myomectomy
-
•
Placenta previa or placenta accreta
-
•
Multiple gestations
-
•
Fetal growth restriction
-
•
Pregestational diabetes with vascular disease
-
•
Pregestational or gestational diabetes—poorly controlled
-
•
Placental abruption
-
•
Chorioamnionitis
-
•
Premature rupture of membranes
-
•
Cholestasis of pregnancy
-
•
Alloimmunization of pregnancy with known or suspected fetal effects
-
•
Fetal congenital malformations
In the same committee opinion in which ACOG (2013b) published the preceding list, ACOG also states, “In contrast, suspected macrosomia, well-controlled gestational diabetes, and documented pulmonary maturity with no other indication are all examples of conditions that are not indications for early-term delivery” (p. 1). Yet, almost 60% of the women in the Listening to Mothers III survey believed that macrosomia is an appropriate reason for induction. Childbirth educators hear almost every day that women are scheduling inductions because the baby appears to be “too big.”
The Joint Commission, which accredits hospitals in the United States, now requires that all hospitals with more than 1,100 births per year report the number of elective births before 39 weeks, with a goal of eliminating such births.
There is controversy about whether oligohydramnios by itself, without other symptoms of fetal compromise, is an appropriate indication for labor induction. Experts do not agree about the best method of measuring amniotic fluid and do not agree about how much amniotic fluid is too little. According to Dr. Mary Munn (2011), who reviewed the literature on oligohydramnios in Obstetrics and Gynecology Clinics of North America, “The significance of oligohydramnios is unclear in high-risk and especially low-risk populations, and may lead to interventions that increase morbidity and mortality, especially in the mother” (p. 391).
When to Induce for Postterm Pregnancies?
Although some healthcare providers recommend routine induction for posterm pregnancies at 41 weeks, the weight of the evidence and professional consensus support routine induction for postterms at 42 weeks. In a 2014 practice bulletin, ACOG (2014a) reviewed the literature and made the following recommendations:
Induction of labor after 42 0/7 weeks and by 42 6/7 weeks of gestation is recommended, given evidence of an increase in perinatal morbidity and mortality. (Based on good and consistent scientific evidence (Level A) and
. . . Induction of labor between 41 0/7 weeks and 42 0/7 weeks of gestation can be considered. (Based on limited or inconsistent scientific evidence (Level B).
Although the researchers who wrote the 2012 Cochrane Review on induction on posterm pregnancies (Gulmezoglu, Crowther, Middleton, & Heatley, 2012) state that routine induction at 41 weeks is associated with fewer perinatal deaths than expectant management, they acknowledge that the absolute risk of death is small and encourage healthcare providers to allow women to make informed choices.
A policy of labour induction [generally at 41 completed weeks] compared with expectant management is associated with fewer perinatal deaths and fewer caesarean sections . . . However, the absolute risk of perinatal death is small. Women should be appropriately counselled in order to make an informed choice between scheduled induction for a post-term pregnancy or monitoring without induction (or delayed induction). (p. 2)
Although the current Cochrane review on induction at term or beyond was published in 2012, the reviewers did not use any studies published later than 2007 in their analysis. In 2009, Swedish researchers also published a systematic review looking at induction of labor versus expectant management for postterm pregnancies (Wennerholm, Hagberg, Brorsson, & Bergh, 2009, pp. 12, 15). Thirteen of the studies included in the Cochrane review were also included in the Swedish review. But Swedish reviewers excluded some additional studies included by Cochrane for predetermined reasons. The Swedish reviewers came to a different conclusion, stating,
Our results differ from that review [Cochrane] because of different selection criteria for the included trials. . . . These exclusions fulfilled our exclusion criteria determined in advance for this systematic review. In conclusion, the present meta-analysis did not demonstrate that there is a significant difference in perinatal mortality when comparing a strategy of elective induction with one of expectant management. (pp. 12, 15)
The authors of the prestigious medical textbook Williams Obstetrics agree with the Swedish systematic review rather than the current Cochrane review. They say,
. . . we consider 41-week pregnancies without other complications to be normal. Thus, no interventions are practiced solely based on fetal age until 42 completed weeks. (Cunningham et al., 2010, pp. 839–840)
The World Association for Perinatal Medicine also agrees with the Swedish systematic review (Wennerholm et al., 2009) in their guidelines for managing postterm pregnancy:
There is no conclusive evidence that this policy [routine induction before 42 weeks] improves fetal, maternal, and neonatal outcomes as compared to expectant management. . . it would seem appropriate to let women make an informed decision about which management they wish to undertake. (Mandruzzato et al., 2010, p. 111)
Goer and Romano (2012) in their excellent analysis of evidence-based maternity care, Optimal Care in Childbirth, also say, “Refrain from elective inductions prior to 42 completed weeks” (p. 157).
WHAT IF A WOMAN HAS TO SCHEDULE THE BIRTH FOR MEDICAL REASONS?
There are times when it is better for a baby to be born than to stay inside the uterus. In such cases, allowing the pregnancy to continue for as long as possible will help to increase the levels of the birth hormones and the numbers of receptors. If IV fluids and continuous EFM are required during labor, asking if it is possible to sit or stand next to the bed will give the laboring woman more positions with which to work. If telemetry is available, the laboring woman can walk and change positions, taking the IV pole with her. Having a doula to provide support and encouragement to both the laboring woman and her labor partner will enhance progress and comfort. Finally, placing the baby skin-to-skin on the mother’s chest immediately after birth and leaving the baby there until the first feeding is accomplished even in the event of a cesarean will increase substantially levels of oxytocin, endorphins, and prolactin. Keeping mother and baby together after the birth with skin-to-skin contact and frequent breastfeeding will help to compensate for the interference from synthetic oxytocin and other medical interventions and increase levels of the critical birth hormones to promote successful breastfeeding and attachment.
WHAT CAN CHILDBIRTH EDUCATION DO TO ENCOURAGE WOMEN TO LET LABOR BEGIN ON ITS OWN?
Several years ago, physicians and childbirth educators in a large midwestern hospital argued about who was responsible for the recent increase in the number of inductions. The physicians said, “Our patients are demanding to be induced. We are just giving them what they want.” The childbirth educators retorted, “The students in our classes tell us that it is the doctors who are suggesting induction” (G. Newman, personal communication, September 2010). To help resolve the argument, the doctors helped to fund a randomized controlled trial to look at whether childbirth education could decrease the number of inductions. First, researchers looked at induction rates for women who attended childbirth classes at the hospital versus women who did not attend class. The induction rates were similar in both groups. Then, the researchers created a special 45-min presentation on the risks of labor induction entitled Is Labor Induction Right for You? After several months of offering childbirth education classes with the added presentation, researchers again looked at the induction rates between those who attended classes and those who did not. This time, those who attended classes were significantly less likely to have their labors induced (Simpson, Newman, & Chirino, 2010a, 2010b).
Childbirth educators and doulas who meet with their clients prenatally can encourage students to think of a range for their due dates rather than a specific day. They can share the consumer information from Dr. Buckley’s (2014) report, The Hormonal Physiology of Childbearing, so that childbearing families understand the importance of having optimal levels of birth hormones “on board” for labor and birth, breastfeeding, and attachment. They can teach about the important growth and development that takes place in the baby’s brain and lungs in the last weeks and days of pregnancy. (The March of Dimes poster or card illustrating brain growth in the last weeks of pregnancy is a valuable resource.) They can present information on the risks of not letting labor begin on its own, quoting professional organizations such as ACOG who recommend against elective inductions before 41 weeks’ gestation. Most importantly, they can share positive stories and images of pregnancy, labor and birth, and breastfeeding so that pregnant women trust that their bodies know the perfect birth date for their baby and have confidence in their own body’s innate ability to give birth.
WHAT CAN OTHER BIRTH PROFESSIONALS DO TO ENCOURAGE WOMEN TO LET LABOR BEGIN ON ITS OWN?
Health-care providers can abide by current professional guidelines by not suggesting labor induction unless there are medical indications. In the randomized controlled trial cited earlier (Simpson et al., 2010a, 2010b), 75% of the women who completed the survey and had an elective induction indicated that the physician suggested the option, compared to only 25% who indicated that they asked the physician to perform an elective induction.
Labor nurses can participate on committees that establish guidelines for appropriate labor induction. For those pregnant women who require induction for medical reasons, nurses can support and promote comfort measures that promote labor progress and the flow of birth hormones such as immediate, uninterrupted skin-to-skin contact for the healthy mother and baby until the first feeding is accomplished.
WHAT CAN CHILDBEARING FAMILIES DO?
The childbearing woman can choose a provider and birth location that supports and promotes allowing labor to begin on its own. She and her support team can create a plan for birth based on the Lamaze International’s six healthy birth practices.
CONCLUSION
Current evidence overwhelmingly supports the wisdom of allowing labor to begin on its own for healthy women and their babies. With professional organizations such as ACOG actively promoting vaginal birth and discouraging elective inductions, childbirth educators and others in the birth community have new support to help women to desire, plan for, and achieve letting labor begin on its own.
Biography
DEBBY AMIS is the coauthor of Prepared Childbirth—The Family Way, Prepared Childbirth—The Educator’s Guide, and The Lamaze Toolkit. She is also codirector of The Family: Way Lamaze Childbirth Educator Program. She and her husband live close to their grandchildren in Houston, Texas.
REFERENCES
- American College of Nurse-Midwives. Midwives Alliance of North America. National Association of Certified Professional Midwives (2012). Supporting healthy and normal physiologic childbirth: A consensus statement by ACNM, MANA, and NACPM. Retrieved from http://mana.org/pdfs/Physiological-Birth-Consensus-Statement.pdf [DOI] [PubMed]
- American College of Obstetricians and Gynecologists (2009). ACOG Practice Bulletin no. 107: Induction of labor. Obstetrics and Gynecology, 114(2, 386–397. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists (2013a). ACOG Committee Opinion No. 579: Definition of term pregnancy. Retrieved from http://www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Obstetric_Practice/Definition_of_Term_Pregnancy [DOI] [PubMed]
- American College of Obstetricians and Gynecologists (2013b). ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Retrieved from http://www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Obstetric_Practice/Nonmedically_Indicated_Early-Term_Deliveries [DOI] [PubMed]
- American College of Obstetricians and Gynecologists (2013c, May 7). Study finds adverse effects of Pitocin in newborns. American College of Obstetricians and Gynecologists News Room. Retrieved from http://www.acog.org/About_ACOG/News_Room/News_Releases/2013/Study_Finds_Adverse_Effects_of_Pitocin_in_Newborns [Google Scholar]
- American College of Obstetricians and Gynecologists (2014). Practice bulletin #146: Management of late-term and postterm pregnancies. Obstetrics and Gynecology, 124(2, 390–396. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine (2014). Obstetric care consensus: Safe prevention of the primary cesarean delivery. Obstetrics and Gynecology, 123, 693–671. Retrieved from http://www.acog.org/Resources_And_Publications/Obstetric_Care_Consensus_Series/Safe_Prevention_of_the_Primary_Cesarean_Delivery [DOI] [PubMed] [Google Scholar]
- Baud D., Rouiller S., Hohlfeld P., Tolsa J. F., Vial Y. (2013). Adverse obstetrical and neonatal outcomes in elective and medically indicated inductions of labor at term. Journal of Maternal-Fetal & Neonatal Medicine, 26(16), 1595–1601. [DOI] [PubMed] [Google Scholar]
- Belghiti J., Kayem G., Dupont C., Rudigoz R. C., Bouvier-Colle M.-H., Deneux-Tharaux C. (2011). Oxytocin during labour and risk of severe postpartum haemorrhage: A population-based, cohort-nested case-control study. BMJ Open, 1(2), e000514. 10.1136/bmjopen-2011-000514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley S. (2014). The hormonal physiology of childbearing. New York, NY: Childbirth Connection. [Google Scholar]
- Burgos J., Rodríguez L., Otero B., Cobos P., Osuna C., Centeno Mdel M., Martínez-Astorquiza T. (2012). Induction at 41 weeks increases the risk of caesarean section in a hospital with a low rate of caesarean sections. Journal of Maternal-Fetal & Neonatal Medicine, 25(9), 1716–1718. [DOI] [PubMed] [Google Scholar]
- Ceanga M., Spataru A., Zagrean A. M. (2010). Oxytocin is neuroprotective against oxygen–glucose deprivation and reoxygenation in immature hippocampal cultures. Neuroscience Letters, 477(1), 15–18. [DOI] [PubMed] [Google Scholar]
- Condon J. C., Pancharatnam J., Faust J. M., Mendelson C. R. (2004). Surfactant protein secreted by the maturing mouse fetal lung acts as a hormone that signals the initiation of parturition. Proceedings of the National Academy of Sciences of the United States of America, 101(14), 4978–4983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham F. G., Leveno K. J., Bloom S. L., Hauth J. C., Rouse D. J., Spong C. Y. (2010). William’s obstetrics. New York, NY: McGraw Medical. [Google Scholar]
- Declercq E. R., Sakala C., Corry M. P., Applebaum S., Herrlich A. (2013). Listening to mothers III: Pregnancy and childbirth. New York, NY: Childbirth Connection. [Google Scholar]
- Dunne C., Da Silva O., Schmidt G., Natale R. (2009). Outcomes of elective labour induction and elective caesarean section in low-risk pregnancies between 37 and 41 weeks’ gestation. Journal of Obstetrics and Gynaecology Canada, 31(12), 1124–1130. [DOI] [PubMed] [Google Scholar]
- Ehrenthal B. B., Jiang X., Strobino D. M. (2010). Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstetrics and Gynecology, 116(1), 35–42. [DOI] [PubMed] [Google Scholar]
- Elkamil A. I., Anderson G. L., Salvesen K. A., Skranes J., Irgens L. M., Vik T. (2011). Induction of labor and cerebral palsy: A population-based study in Norway. Acta Obstetricia et Gynecologica Scandinavica, 90(1), 83–91. [DOI] [PubMed] [Google Scholar]
- Engle W. A. (2006). A recommendation for the definition of “late preterm” (near-term) and the birth weight-gestational age classification system. Seminars in Perinatology, 30(1), 2–7. [DOI] [PubMed] [Google Scholar]
- Goer H., Romano A. (2012). Optimal care in childbirth: The case of a physiologic approach. Seattle, WA: Classic Day. [Google Scholar]
- Greenwell E. A., Wyshak G., Ringer S. A., Johnson L. C., Rivkin M. J., Lieberman E. (2012). Intrapartum temperature elevation, epidural use, and adverse outcome in term infants. Pediatrics, 129(2), e477–e454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory S. G., Anthopolos R., Osgood C. E., Grotegut C. A., Miranda M. L. (2013). Association of autism with induced or augmented childbirth in North Carolina Birth Record (1990–1998) and Education Research (1997–2007) databases. JAMA Pediatrics, 167(10), 959–966. [DOI] [PubMed] [Google Scholar]
- Grotegut C. A., Paglia M. J., Johnson L. N. C., Thames B., James A. H. (2011). Oxytocin exposure during labor among women with postpartum hemorrhage secondary to uterine atony. American Journal of Obstetrics & Gynecology, 204(1), 56, e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gülmezoglu A. M., Crowther C. A., Middleton P., Heatley E. (2012). Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews, (6), CD004945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton B. E., Martin J. A., Osterman M. J. K., Curtin S. C. (2014). Births: Preliminary data for 2013. National Vital Statistics Reports, 63(2). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Hunter L. A. (2009). Issues in pregnancy dating: Revisiting the evidence. Journal of Midwifery & Women’s Health, 54(3), 184–190. [DOI] [PubMed] [Google Scholar]
- Institute for Safe Medication Practices (2012). ISMP’s list of high-alert medications. Retrieved from http://www.ismp.org/tools/highalertmedications.pdf
- Jain L. (2006). Implications of labor on neonatal outcomes. In NIH State-of-the-Science Conference: Cesarean delivery on maternal request. Retrieved from http://www.consensus.nih.gov/2006/cesareanabstracts.pdf [PubMed]
- Jain L., Eaton D. C. (2006). Physiology of fetal lung fluid clearance and the effect of labor. Seminars in Perinatology, 30(1), 34–43. [DOI] [PubMed] [Google Scholar]
- Jukic A. M., Baird D. D., Weinberg C. R., McConnaughey D. R., Wilcox A. J. (2013). Length of human pregnancy and contributors to its natural variation. Human Reproduction, 28(10), 2848–2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leighton B. L., Halpern S. H. (2002). The effects of epidural analgesia on labor, maternal, and neonatal outcomes: A systematic review. American Journal of Obstetrics and Gynecology, 186(5, Suppl. Nature), S69–S77. [DOI] [PubMed] [Google Scholar]
- Levine L. D., Hirshberg A., Srinivas S. K. (2013). Term induction of labor and risk of cesarean delivery by parity. Journal of Maternal, Fetal, and Neonatal Medicine, 27(12), 1232–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman E., O’Donoghue C. (2002). Unintended effects of epidural analgesia during labor: A systematic review. American Journal of Obstetrics and Gynecology, 186(5, Suppl.), S31–S68. [DOI] [PubMed] [Google Scholar]
- Loftin R. W., Habli M., Snyder C. C., Cormier C. M., Lewis D. F., DeFranco E. A. (2010). Late preterm birth. Reviews in Obstetrics and Gynecology, 39(1), 10–19. [PMC free article] [PubMed] [Google Scholar]
- Mandruzzato G., Alfirevic Z., Chervenak F., Gruenebaum A., Heimstad R., Thilaganathan B. (2010). Guidelines for the management of postterm pregnancy. Journal of Perinatal Medicine, 38(2), 111–119. [DOI] [PubMed] [Google Scholar]
- Martin J. A., Hamilton B. E., Osterman M. J. K., Curtin S. C., Mathews T. J. (2013). Births: Final data for 2012. National Vital Statistics Reports, 62(9). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Martin J. A., Kirmeyer S., Osterman M., Shepherd R. A. (2009). NCHS data brief #24: Born a bit too early: Recent trends in late preterm births. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [PubMed] [Google Scholar]
- Mathews T. J., MacDorman M. F. (2013). Infant mortality statistics from the 2010 period linked birth/infant death data set. Hyattsville, MD: National Center for Health Statistics; Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_08.pdf [PubMed] [Google Scholar]
- Morse S. B., Zheng H., Tang Y., Roth J. (2009). Early school-age outcomes of later preterm infants. Pediatrics, 123(4), e622–e629. [DOI] [PubMed] [Google Scholar]
- Munn M. B. (2011). Management of oligohydramnios in pregnancy. Obstetrics and Gynecology Clinics of North America, 38(2), 387–395. [DOI] [PubMed] [Google Scholar]
- National Childbirth Trust , Royal College of Midwives, Royal College of Obstetricians and Gynaecologists. (2007). Making normal birth a reality—Consensus statement from the Maternity Care Working Party. Retrieved from http://www.rcog.org.uk/files/rcog-corp/uploaded-files/JointStatementNormalBirth2007.pdf
- Osterman M. J. K., Martin J. A. (2014). Primary cesarean delivery rates, by state: Results from the revised birth certificate, 2006–2012. National Vital Statistics Reports, 63(1). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Rattigan M. I., Atkinson A. L., Baum J. D. (2013). Delivery route following elective induction of labor at term: Analysis of 807 patients. Journal of Clinical Medical Research, 5(4), 305–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooks J. (2009). Oxytocin as a “high alert medication”: A multilayered challenge to the status quo. Birth, 36(4), 345–358. [DOI] [PubMed] [Google Scholar]
- Simpson K. R., Newman G., Chirino O. R. (2010a). Patient education to reduce elective inductions. MCN. The American Journal of Maternal Child Nursing, 35(4), 188–194. [DOI] [PubMed] [Google Scholar]
- Simpson K. R., Newman G., Chirino O.R. (2010b). Patients’ perspectives on the role of prepared childbirth education in decision making regarding elective labor induction. The Journal of Perinatal Education, 19(3), 21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Society of Obstetricians and Gynaecologists of Canada , Association of Women’s Health, Obstetric and Neonatal Nurses of Canada, Canadian Association of Midwives, College of Family Physicians of Canada, Society of Rural Physicians of Canada. (2008). Joint policy statement on normal childbirth. Retrieved from http://www.cfpc.ca/uploadedFiles/Resources/Resource_Items/Health_Professionals/JointPolicyStatementonNormalChildbirth.pdf
- Tomashek K. M., Shapiro-Mendoza C. K., Davidoff M. J., Petrini J. R. (2007). Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. The Journal of Pediatrics, 151(5), 450–456. [DOI] [PubMed] [Google Scholar]
- Varrassi G., Bazzano C., Edwards W. T. (1989). Effects of physical activity on maternal beta-endorphin levels and perception of labor pain. American Journal of Obstetrics and Gynecology, 160(3), 707–712. [DOI] [PubMed] [Google Scholar]
- Wassen M. M., Winkens B., Dorssers E. M., Marcus M. A., Moonen R. M., Roumen F. J. (2014). Neonatal sepsis is mediated by maternal fever in labour epidural analgesia. Journal of Obstetrics and Gynaecology, 17, 1–5. [DOI] [PubMed] [Google Scholar]
- Wennerholm U. B., Hagberg H., Brorsson B., Bergh C. (2009). Induction of labor versus expectant management for post-date pregnancy: Is there sufficient evidence for a change in clinical practice? Acta Obstetricia et Gynecologica Scandinavica, 88(1), 6–17. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1996). Care in normal birth—A practical guide. Retrieved from http://www.who.int/maternal_child_adolescent/documents/who_frh_msm_9624/en/