Abstract
Epiphrenic esophageal diverticula (EED) are rare. The estimated incidence is about 1:500,000/year. EED usually result from a combination of esophageal obstruction, functional or mechanical and a point of weakness of the muscularis propria. Most of the symptoms are unspecific, but dysphagia is most common. Chest radiograph, barium esophagogram, endoscopy and manometry are diagnostic tools. The treatment methods are conservative medical therapy, myotomy, diverticulectomy and fundoplication. In addition, endoscopic pneumatic dilation and botulinum toxin injection are a good alternative for symptomatic patients with motility disorders who are unfit for or unwilling to undergo surgery.
Keywords: Diverticulum, epiphrenic, esophageal
INTRODUCTION
Epiphrenic esophageal diverticula (EED) are out-pouching of the esophageal lumen, originating in the distal of the esophagus,[1] typically 4-8 cm above the cardia and usually projecting from the right posterior wall.[2]
EED are rare,[3,4,5,6,7] and account for <10% of all esophageal diverticula.[8,9] The prevalence of EED is 0.06-4% based on radiologic and endoscopic findings.[3] The actual incidence of EED is unknown,[1,10] but, the estimated incidence is about 1:500,000/year.[1]
We present a case with a long history of symptoms which caused by epiphrenic diverticulum.
CASE REPORT
The present case report is about a 48-year-old male patient who was admitted in the clinic of internal medicine at Amir-ul-Momenin hospital, Zabol, Iran on June 2013 with a body mass index of 42.6. He has been complained of heartburn, retrosternal pain and occasional regurgitation. Symptoms had started since 20 years ago, but worsened during the last 6 months, especially after meals. The pain sometimes radiated to the lower-left side of the chest and the upper quadrants of the abdomen, which aggravated after eating a big meal. Besides antacids and H2 receptor antagonists such as cimetidine, the pain often alleviated after eructation and regurgitation. A barium swallow demonstrated an epiphrenic driverticulum of 42 mm at the right side of sternum [Figure 1]. In addition, he complained of a severe constipation and rectal bleeding after barium esophagography. The complete blood count test revealed a hematocrit of 47.4% and hemoglobin of 16.3 g/dl. A panendoscopy showed a hiatus hernia and erythematous mucosa in the body of the stomach. A biopsy of gastric antral erythematous mucosa showed a moderate chronic active superficial gastritis and mild atrophy. However, there was no evidence of dysplasia and metaplasia in the biopsy. Treatment team was not consent whether the patient must undergo for an early diverticulectomy due to the size of diverticulum and the moderate-severe symptoms. The patient was unwilling to be operated as well. The symptoms were improved after 2 weeks of prescription of pantaprazole sodium 80 mg bid and teaching to change the food habits such as chewing food thoroughly and drinking plenty of water after meals.
Figure 1.
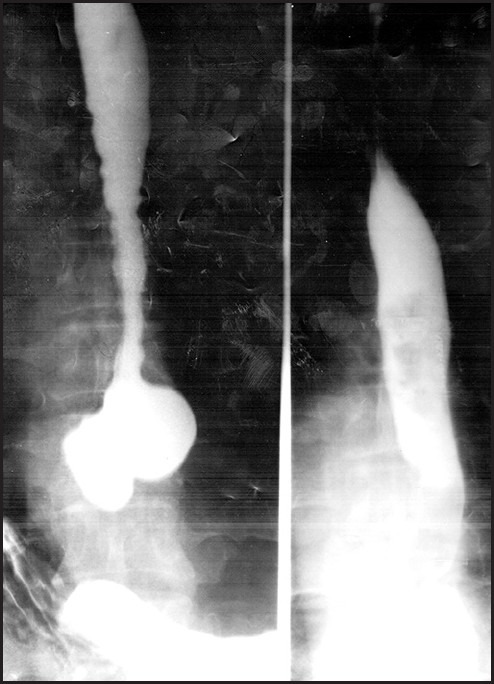
Barium view of epiphrenic esophageal diverticulum
DISCUSSION
EED usually result from a combination of esophageal obstruction, functional or mechanical and a point of weakness of the muscularis propria.[11] All or only the mucosa and submucosal layers of the esophagus may involve as well.[4,12] The functional obstruction is associated with motility disorders e.g., achalacia, diffuse spasm,[1,2,3] hypertensive lower esophageal sphincter (LES), non-specific motility disorders,[2,13] uncoordinated and poorly relaxing LES with very high-pressure peristaltic waves.[2] The mechanical obstruction is associated with a prior Nissen fundoplication,[7,9,10] peptic stricture and leiomyoma or gastroesophageal junction tumor.[7,10] In some patients functional obstruction coincides with mechanical obstruction.[7]
Clinical manifestations of the EED vary in type, severity and frequency.[8] The most common symptom is dysphagia. The other symptoms are regurgitation, weight loss, chest pain, halitosis, aspiration,[3] anorexia, hematemesis, heartburn, melena, nocturnal cough and odynophagia.[12] Symptoms usually progress with time[8] and the size of the diverticula. Patients with a diverticulum larger than 5 cm are usually symptomatic.[10] However, most of patients with EED are asymptomatic.[2,4,11,12]
As the symptoms are common and unspecific, EED are diagnosed late. Late diagnosis can cause more severe and potentially life-threatening illnesses e.g., aspiration pneumonia and cancer.[12] The incidence of cancer is 0.6% in EED[3] and often advanced at diagnosis.[12] The warning symptoms are progressive dysphagia, unintentional weight loss, blood in the regurgitated material, regurgitation of a piece of the tumor, odynophagia, melena, hematemesis and hemoptysis. Risk factors for malignancy are old age, men, long-standing history and larger diverticula.[3] However, some of the researchers did not find esophageal carcinoma arising within a diverticulum.[1]
The EED are diagnosed using chest radiograph, barium esophagogram, endoscopy and manometry.[8] Barium swallow is a brilliant,[3,12] safe, simple and effective[12] test to diagnose and determine the size and location of EED.[3] However, Barium is associated with constipation and barium impaction.[14] Drinking plenty of water and using a stool softener or laxative promote evacuation of barium.[15] Upper digestive endoscopy confirms the presence of diverticula,[3] and rules out malignancy and associated diseases.[3,4,12] Esophageal manometry is the other excellent test for diagnosing the esophageal motor disorders. In symptomatic patients, pH monitoring diagnoses gastroesophageal reflux disease and guides medical treatments. However, some authors obviate manometry[3,12] or ambulatory pH monitoring because they believe motor disorder is always present in patient with EED and the results usually do not affect the planned procedures.[4]
No specific treatment needs for asymptomatic small and mildly symptomatic medium-sized diverticula, but symptoms of reflux or gastritis should be managed using proton pump inhibitors or H2-blockers. Endoscopic pneumatic dilation[1] and botulinum toxin injection are a good alternative for symptomatic patients with motility disorders who are unfit for or unwilling to undergo surgery.[2]
Patients with EED should not have blind gastric intubation even by experienced care providers.[5,15] Catheters must be inserted under fluoroscopic guidance or under endoscopy.[5]
The presence of diverticulum, per se and its size are not indications for surgery in the patient with EED. Surgery should be for patients with large diverticula, severe dysphagia, regurgitation, food retention and the actual or potential risk of aspiration pneumonia.[1,5]
Treatment strategies, surgical or laparoscopic, in patient with symptomatic EED involve esophageal myotomy, diverticulectomy and fundoplication.[1,2,9,10] Myotomy decreases the incidence of diverticulum recurrence[13] and partial fundoplication has been proposed as the most appropriate antireflux method.[6,7,9]
Laparoscopy is the best approach[3,4] for diverticulectomy, esophageal myotomy and fundoplication,[3,9,10] when diverticula are <4 cm across the base and closer to the esophageal hiatus.[4] Surgical access has traditionally been through a left thoracotomy.[3,11] This approach offers better exposure of the esophagus in patients with midesophageal diverticula, previous abdominal surgery and morbid obesity.[11] Thoracotomy permits a longer myotomy, which may reduce the risk of diverticula recurrence.[9] Proton pump inhibitors are maintained indefinitely and all medications are prescribed in crushed or liquid form, avoiding pills.[4]
CONCLUSIONS
The current case not only adds to the collective clinical knowledge of this rare esophageal disorder, but also reveals a considerable perspective on relieving symptoms through conservative treatments. Patient was symptomatic despite having a diverticulum <5 cm and there was no evidence for malignancy regardless of having risk factors i.e., old age, men, long-standing history and delayed diagnosis. The conservative treatments and changing food habits were effective in alleviating the symptoms. Therefore, this kind of treatment should always be the first line management even for the symptomatic patients. The patient with EED must consume plenty of water after the meal to wash out the food remnants from esophageal diverticula. They should not allow blind esophageal intubation. Although chest pain is unspecific, patients must be oriented that it might be a critical symptom of myocardial infarction and must seriously be assessed and managed in referral centers. To prevent the complications of barium esophagography such as constipation and barium impaction, the patient should consume plenty of water and use stool softener or laxative. Finally, if symptoms persist and the risk of aspiration pneumonia presents, operation becomes the alternative treatment method.
AUTHORS’ CONTRIBUTION
All authors have contributed in designing and conducting the study. All authors have assisted in preparation of the first draft of the manuscript or revising it critically for important intellectual content. All authors have read and approved the content of the manuscript and confirmed the accuracy or integrity of any part of the work.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zaninotto G, Portale G, Costantini M, Zanatta L, Salvador R, Ruol A. Therapeutic strategies for epiphrenic diverticula: Systematic review. World J Surg. 2011;35:1447–53. doi: 10.1007/s00268-011-1065-z. [DOI] [PubMed] [Google Scholar]
- 2.Katsinelos P, Chatzimavroudis G, Zavos C, Pilpilidis I, Paroutoglou G, Kountouras J. Long-term botulinum toxin treatment for dysphagia due to large epiphrenic diverticulum in elderly patients: A report of two cases. Dysphagia. 2009;24:109–13. doi: 10.1007/s00455-008-9159-y. [DOI] [PubMed] [Google Scholar]
- 3.Herbella FA, Patti MG. Modern pathophysiology and treatment of esophageal diverticula. Langenbecks Arch Surg. 2012;397:29–35. doi: 10.1007/s00423-011-0843-2. [DOI] [PubMed] [Google Scholar]
- 4.Magee MJ, Sonett JR. Management of epiphrenic esophageal diverticula. Oper Tech Thorac Cardiovasc Surg. 2011;16:18–29. [Google Scholar]
- 5.Vicentine FP, Herbella FA, Silva LC, Patti MG. High resolution manometry findings in patients with esophageal epiphrenic diverticula. Am Surg. 2011;77:1661–4. [PubMed] [Google Scholar]
- 6.D’Journo XB, Ferraro P, Martin J, Chen LQ, Duranceau A. Lower oesophageal sphincter dysfunction is part of the functional abnormality in epiphrenic diverticulum. Br J Surg. 2009;96:892–900. doi: 10.1002/bjs.6652. [DOI] [PubMed] [Google Scholar]
- 7.Reznik SI, Rice TW, Murthy SC, Mason DP, Apperson-Hansen C, Blackstone EH. Assessment of a pathophysiology-directed treatment for symptomatic epiphrenic diverticulum. Dis Esophagus. 2007;20:320–7. doi: 10.1111/j.1442-2050.2007.00716.x. [DOI] [PubMed] [Google Scholar]
- 8.Usküdar O, Dağli U, Asil M, Yol S, Saşmaz N. Epiphrenic diverticulum with abnormal manometry: A case report. Turk J Gastroenterol. 2004;15:108–11. [PubMed] [Google Scholar]
- 9.Plackett TP, Meghoo CA, Febinger DL. Recurrent epiphrenic diverticulum after transabdominal diverticulectomy: Report of a case and review of the literature. Image. 2009;68:13–5. [PubMed] [Google Scholar]
- 10.Melman L, Quinlan J, Robertson B, Brunt LM, Halpin VJ, Eagon JC, et al. Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myotomy, and partial fundoplication for epiphrenic diverticula. Surg Endosc. 2009;23:1337–41. doi: 10.1007/s00464-008-0165-9. [DOI] [PubMed] [Google Scholar]
- 11.Soares RV, Montenovo M, Pellegrini CA, Oelschlager BK. Laparoscopy as the initial approach for epiphrenic diverticula. Surg Endosc. 2011;25:3740–6. doi: 10.1007/s00464-011-1779-x. [DOI] [PubMed] [Google Scholar]
- 12.Conklin JH, Singh D, Katlic MR. Epiphrenic esophageal diverticula: Spectrum of symptoms and consequences. J Am Osteopath Assoc. 2009;109:543–5. [PubMed] [Google Scholar]
- 13.Valentini M, Pera M, Vidal O, Lacima G, Belda J, de Lacy AM. Incomplete esophageal myotomy and early recurrence of an epiphrenic diverticulum. Dis Esophagus. 2005;18:64–6. doi: 10.1111/j.1442-2050.2005.00450.x. [DOI] [PubMed] [Google Scholar]
- 14.Smeltzer S. China: Lippincott Williams & Wilkins; 2012. Brunner and Suddarth's Handbook of Laboratory and Diagnostic Tests. [Google Scholar]
- 15.Brunner LS, Smeltzer SCOC, Bare BG, Hinkle JL, Cheever KH. China: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. [Google Scholar]


