Abstract
IMPORTANCE
Mothers and children living in adverse contexts are at risk of premature death.
OBJECTIVE
To determine the effect of prenatal and infant/toddler nurse home visiting on maternal and child mortality during a 2-decade period (1990–2011).
DESIGN, SETTING, AND PARTICIPANTS
A randomized clinical trial was designed originally to assess the home visiting program’s effect on pregnancy outcomes and maternal and child health through child age 2 years. The study was conducted in a public system of obstetric and pediatric care in Memphis, Tennessee. Participants included primarily African American women and their first live-born children living in highly disadvantaged urban neighborhoods, who were assigned to 1 of 4 treatment groups: treatment 1 (transportation for prenatal care [n = 166]), treatment 2 (transportation plus developmental screening for infants and toddlers [n = 514]), treatment 3 (transportation plus prenatal/postpartum home visiting [n = 230]), and treatment 4 (transportation, screening, and prenatal, postpartum, and infant/toddler home visiting [n = 228]). Treatments 1 and 3 were included originally to increase statistical power for testing pregnancy outcomes. For determining mortality, background information was available for all 1138 mothers assigned to all 4 treatments and all but 2 live-born children in treatments 2 and 4 (n = 704). Inclusion of children in treatments 1 and 3 was not possible because background information was missing on too many children.
INTERVENTIONS
Nurses sought to improve the outcomes of pregnancy, children’s health and development, and mothers’ health and life-course with home visits beginning during pregnancy and continuing through child age 2 years.
MAIN OUTCOMES AND MEASURES
All-cause mortality in mothers and preventable-cause mortality in children (sudden infant death syndrome, unintentional injury, and homicide) derived from the National Death Index.
RESULTS
The mean (SE) 21-year maternal all-cause mortality rate was 3.7% (0.74%) in the combined control group (treatments 1 and 2), 0.4% (0.43%) in treatment 3, and 2.2% (0.97%) in treatment 4. The survival contrast of treatments 1 and 2 combined with treatment 3 was significant (P = .007); the contrast of treatments 1 and 2 combined with treatment 4 was not significant (P = .19), and the contrast of treatments 1 and 2 combined with treatments 3 and 4 combined was significant (post hoc P = .008). At child age 20 years, the preventable-cause child mortality rate was 1.6% (0.57%) in treatment 2 and 0.0% (SE not calculable) in treatment 4; the survival contrast was significant (P = .04).
CONCLUSIONS AND RELEVANCE
Prenatal and infant/toddler home visitation by nurses is a promising means of reducing all-cause mortality among mothers and preventable-cause mortality in their first-born children living in highly disadvantaged settings.
Racial and economic disparities in adult mortality are substantial1–5 and increasing in the United States,5 with the risk of death increasing in a nonlinear fashion as income declines.2 In recent decades, the disproportionately high mortality associated with low income is applying to larger portions of the US population.2 Between 1992 and 2006, female mortality increased in 43% of US counties6; variations in county-level female mortality changes over time were accounted for by the percentage of residents with a college degree, who were of Hispanic heritage, and who did not smoke but were not explained by medical care conditions, such as proportions of primary care providers or uninsured within counties.6 Access to care is important,7 but more fully reducing mortality associated with low income is likely to depend on improving damaging behaviors and toxic contexts.8,9
Mortality among US children and youth has declined significantly over many decades,10,11 yet substantial disparities persist for children and youth living in poorer communities and for African Americans.10–14 A large portion of these disparities is explained by higher rates of death due to sudden infant death syndrome,14,15 unintentional injuries,11,13 and homicide.11,13 These causes of death are prime candidates for prevention because they are thought to be influenced by the degree to which the developing fetus is protected from adversity, the child is well cared for,15–17 home environments are safe,17 and children’s and youths’ behavior is well regulated.18 As far as we know, there have been no randomized clinical trials of early interventions that have found reductions in mortality for these causes.
Since 1990, we have been conducting, in Memphis, Tennessee, a randomized clinical trial of a program of prenatal and infancy/toddler home visiting by nurses for very low-income mothers, primarily African American, bearing their first children. The program is known today as the Nurse-Family Partnership (NFP).19–24 Nurses in the NFP are charged with improving maternal and child health during pregnancy and the first 2 years of the child’s life.25 The Memphis trial is the second in a series of 3 conducted with different populations.25–33 The first trial of the NFP, begun in 1977, was conducted with a primarily white sample with mixed sociodemographic risk living in a semi-rural community in upstate New York (Elmira).29–33 We focused the Memphis trial on women with higher concentrations of sociodemographic risk because the results of the Elmira trial indicated that the functional and economic benefits of the NFP were more pronounced in these higher risk segments of the sample.29–33 Earlier findings from the Memphis trial included treatment-control differences in children’s injuries revealed in the medical record,19 problems with behavioral regulation at school entry,21 and use of substances and internalizing disorders at age 12 years.23 For mothers in the Memphis trial, enduring differences have been found in the timing of subsequent pregnancies; use of welfare, food stamps, and Medicaid; and behavioral impairment resulting from substance use.19–24
As part of an 18-year follow-up of the mothers and children in Memphis, we monitored the rates of maternal and child death as we traced the sample. We had not hypothesized program effects on maternal and child mortality because we assumed that rates among mothers and children in these age ranges would be too low to discern the effect of the program. We report here, nevertheless, treatment-control maternal and child mortality differences, given their public health importance. The current study was approved by the University of Rochester Institutional Review Board. Participants were provided financial compensation for completing assessments.
Methods
We conducted a randomized clinical trial of the NFP in a public system of obstetric and pediatric care in Memphis, Tennessee, designed originally to assess the program’s effects on pregnancy outcomes and maternal and child health through child age 2 years.19
Participants
A total of 1138 of 1289 eligible women (88.3%) completed written informed consent and were randomized from June 1, 1990, through August 31, 1991. We primarily enrolled African American women at less than 29 weeks of gestation, with no previous live births, and with at least 2 of the following sociodemographic risk characteristics: unmarried, having less than 12 years of education, and unemployed. Of the women enrolled, 92.1% were African American, 98.1% were unmarried, 64.1% were 18 years or younger at registration, and 85.1% came from households with annual incomes below the US federal poverty guidelines. After completing informed consent and baseline interviews, women were randomly assigned to 1 of 4 treatment conditions described below.19
Treatment Conditions
As shown in eTable 1 in the Supplement, women in treatment 1 (n = 166) were provided free transportation for prenatal care appointments. Women in treatment 2 (n = 514) were provided the transportation for prenatal care and developmental screening and referral services for their children at ages 6, 12, and24 months. Those in treatment 3 (n = 230) were provided the free transportation and nurse home visits during pregnancy plus 2 postpartum visits. Women in treatment 4 (n = 228) were provided the same services as those in treatment 3, plus home visits through child age 2 years as well as developmental screening and referrals for their children. To maximize statistical power and minimize costs, participants were disproportionally assigned among treatments. Treatments 1 and 2 were combined to form a control group, and treatments 3 and 4 were combined to form a group visited during pregnancy for assessment of the program’s effect on pregnancy outcomes. To reduce research costs, participants in treatments 1 and 3 were not monitored originally for postnatal assessments.19
Randomization
Random assignment was conducted by means of a computer program based on methods that are extensions of those of Soares and Wu.34 This procedure concealed randomization from data gatherers directly involved with participants in Memphis. We used slightly different assignment ratios and treatment allocation schemes during 3 time frames in the 15-month sample recruitment period.19 This procedure was used to accommodate shifting expectations about completed sample size (because of competition with other studies that sampled the same population) and to manage a relatively large number of women enrolled during the first 2 months of recruitment when only 10 of the 12 project nurses had been hired. Treatment 1 was added to the design during the second and third allocation periods to reduce the number of families assigned to the 2 nurse-visited conditions.
Home Visiting Intervention
Women in treatments 3 and 4 received a mean of 7 prenatal visits, and those in treatment 4 received a mean of 26 visits after delivery. The NFP nurses are charged with (1) improving the outcomes of pregnancy by helping women improve their prenatal health, (2) improving children’s subsequent health and development by helping mothers provide more competent care of their babies, and (3) improving women’s health and development by helping them develop self-care practices, plan subsequent pregnancies, complete their educations, and find employment. The program guidelines include specific activities to support women’s protection of their health including eating balanced diets; avoiding substance use, unsafe sexual practices, and risky social relationships; engaging in exercise and hygiene; and advocating for themselves with providers of office-based care.25,35,36 The program guidelines provide extensive support to caregivers in their efforts to care well for their children, including promoting safe sleep practices (eg, placing babies on their backs during nap time and at night), ensuring safe sleep environments, reducing hazards in the home, and supporting regulated, responsive care of the child.25,35,36
Mortality Outcomes
For the analysis of maternal mortality, we matched all women randomized in each of the 4 treatment conditions with National Death Index (NDI) records using the mothers’ names, birthdates, sex, and Social Security Numbers. The NDI is the criterion standard for ascertainment of mortality and cause of death in the United States.37 For the study of child mortality, we had identifying information for all but 2 live-born children in treatments 2 and 4. Inclusion of children in treatments 1 and 3 was not possible because background information was missing on too many children. The NDI records were available through December 31, 2011.
We categorized causes of maternal deaths into natural and external categories using standard cause-of-death categories from the International Classification of Diseases, Ninth Revision (ICD-9) and International Statistical Classification of Diseases, 10th Revision (ICD-10) (ICD-9 for deaths before 1999 and ICD-10 for deaths 1999–2011).38,39 Natural causes in this sample included neoplasms, human immunodeficiency virus infection, sickle cell anemia, diabetes mellitus, endocarditis, stroke, renal disease, acidosis, aortic dissection, and pulmonary embolism. External causes included drug overdose, suicide, unintentional injuries, and homicide.
We classified the following causes of children’s deaths as preventable: sudden infant death syndrome, unintentional injuries, and homicide. There were no suicides. Natural causes of child death in this sample included multiple congenital malformations, conditions due to an anomaly of an unspecified chromosome, malignant neoplasms of the brain, extreme immaturity, chronic respiratory disease developing during the perinatal period, and infectious colitis, enteritis, and gastroenteritis.
Table 1 reports the number of mothers randomized to treatment conditions, the number of mothers in each condition interviewed after December 31, 2011, the number of cases sent to NDI for abstraction of mortality data, and the number of maternal and child cases for which we were able to ascertain survival status. We determined maternal survival status for all 1138 women randomized and child survival status for 706 of the 708 children in treatment groups 2 and 4 born alive. Across treatment groups, participants studied for mortality status were essentially equivalent on background characteristics at the time of randomization (eTable 2 in the Supplement for mothers and eTable 3 in the Supplement for children).19
Table 1.
Sample Composition Through Birth by Treatment
| Participant Status, No. | Treatment | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Mothers allocated to each treatment | 166 | 514a | 230 | 228 |
| Mothers interviewed after December 31, 2011 | 19 | 10 | ||
| Data on mother sent to NDI | 166 | 495 | 230 | 218 |
| Mothers included in mortality analyses | 166 | 514 | 230 | 228 |
| Miscarriages | 19 | 8 | ||
| Stillbirths | 5 | 2 | ||
| Children born alive | 490 | 218 | ||
| Missing identifiers | 1 | 1 | ||
| Children interviewed after December 31, 2011 | 21 | 9 | ||
| Child identifier data sent to NDI | 468 | 208 | ||
| Children included in mortality analyses | 489 | 217 | ||
Abbreviation: NDI, National Death Index.
One person was randomized a second time following a miscarriage and was subsequently excluded. Earlier reports20 of sample size showed 1139 participants and noted the exclusion of this case.
Mothers who had not died had a mean (SD) duration of follow-up of 20.9 (0.4) years and a mean age of 39.4 (3.1) years at this follow-up (range, 33.4–54.8 years). Children who had not died had a mean age (follow-up time) of 20.6 (0.4) years (range of 19.7–22.1 years).
Statistical Analysis
The Kaplan-Meier method was used to estimate survival functions for all-cause mortality outcomes.40 The log-rank test was used for comparing differences in survival functions. For external-cause mortality (for mothers) and preventable-cause mortality (for children) we used competing risk analysis to estimate cumulative probabilities of failure.41 The Gray test was used to compare differences in cumulative probability functions.42 For mothers, survival was assessed from their date of randomization until the date of death or, if alive, until December 31, 2011, or the last time that we interviewed them. For live-born children, survival started from their date of birth until the date of death or, if alive, until December 31, 2011, or the last time we interviewed them.
For the analysis of maternal mortality, we conducted 3 treatment contrasts: control (treatments 1 and 2 combined) vs (1) prenatal and postpartum home visiting (treatment 3); (2) prenatal, postpartum, and infant/toddler home visiting (treatment 4); and (3) the combination of treatments 3 plus 4 (a post hoc test). For the assessment of child mortality, we contrasted treatment 2 with treatment 4. We made no adjustments for multiple comparisons.
Results
Maternal Mortality
Table 2 reports the number of maternal deaths from natural and external causes. There were 27 deaths for all causes in treatments 1 and 2 combined, 1 in treatment 3, and 5 in treatment 4. There were 11 deaths in treatments 1 and 2 combined due to external causes, none in treatment 3, and 1 in treatment 4.
Table 2.
Deaths and Cause-of-Death Categories by Treatment Condition
| Cause of Death | Treatment | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Maternal deaths, No. | ||||||
| Natural (disease related) | 5 | 11 | 1 | 4 | ||
| External (unintentional injuries, suicide, drug overdose, homicide) | 0 | 11 | 0 | 1 | ||
| Total | ||||||
| Deaths | 5 | 22 | 1 | 5 | ||
| Sample sizea | 166 | 514 | 230 | 228 | ||
| Child deaths, No. | ||||||
| Natural (disease related) | 5 | 2 | ||||
| Preventable (SIDS, unintentional injuries, homicide) | 9 | 0 | ||||
| Total | ||||||
| Deathsb | 14 | 2 | ||||
| Sample sizec | 489 | 217 | ||||
Abbreviation: SIDS, sudden infant death syndrome.
Includes all cases randomized to all 4 treatment groups.
We did not assess child deaths in treatments 1 and 3 because we had unacceptably high rates of missing data for purposes of matching children in these two conditions. We had not conducted prior postnatal assessments of women and children in these groups.
Includes all but 2 cases born alive in treatments 2 and 4.
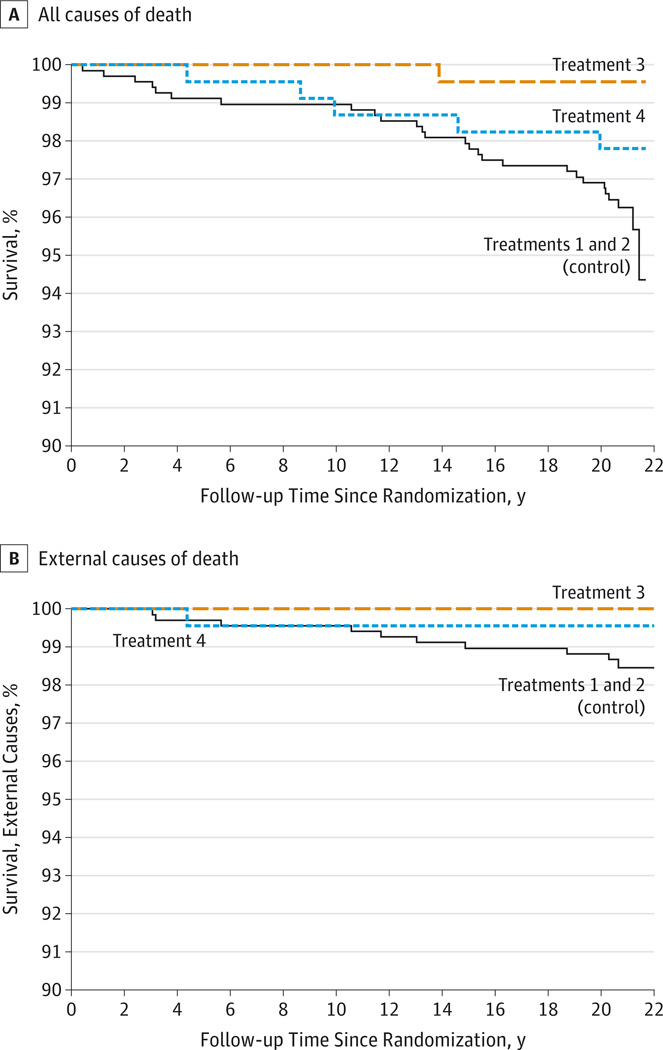
Figure 1A shows the all-cause survival curves for mothers in the 3 treatment conditions, with treatments 1 and 2 combined as the control group. At 21 years following randomization, the mean (SE) all-cause mortality rate was 3.7% (0.74%) in treatments 1 and 2 combined, 0.4% (0.43%) in treatment 3, and 2.2% (0.97%) in treatment 4. The survival contrast of treatments 1 and 2 with treatment 3 was significant (P = .007), the contrast of treatments 1 and 2 combined with treatment 4 was not significant (P = .19), and the contrast of treatments 1 and 2 combined with treatments 3 and 4 combined was significant (post hoc P = .008).
Figure 1. Survival Curves for Mothers in the Nurse-Family Partnership Trial.
A, All causes of death. B, External causes of death. All 1105 mothers who survived had at least 20.2 years of follow-up after randomization. The numbers at risk of dying at 20.5, 21.0, 21.5, and 22.0 years after randomization were 898, 437, 65, and 1, respectively.
Figure 1B shows the survival curves for external causes of mortality. At 21 years after randomization, the external-cause mortality rate was 1.7% (0.51%) in treatments 1 and 2 combined, 0.0% (SE not calculable) in treatment 3, and 0.4% (0.44%) in treatment 4. The external-cause survival analysis contrast of treatments 1 and 2 combined with treatment 3 was marginally significant (P = .053); with treatment 4 was not significant (P = .18); and with treatments 3 and 4 combined was significant (post hoc P = .02).
Child Mortality
Table 2 reports the number of child deaths for natural and preventable causes. There were 14 deaths for all causes in treatment 2 and 2 deaths in treatment 4. Five of the deaths in treatment 2 and 2 in treatment 4 were due to natural causes. Nine of the deaths in treatment 2 were due to preventable causes, whereas there were no deaths associated with preventable causes in treatment 4.
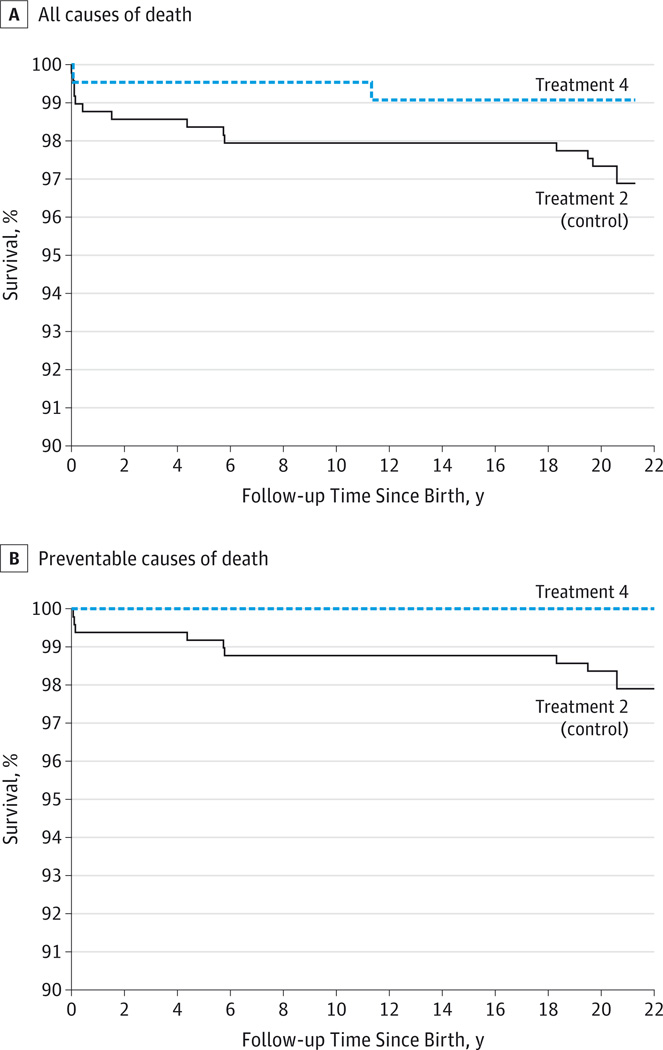
Figure 2A shows the survival curves for children in treatments 2 and 4, examining all causes of mortality. At child age 20 years, the all-cause mortality rate was 2.7% (0.73%) in treatment 2 and 0.9% (0.65%) in treatment 4. The nurse-control survival contrast was not significant (P = .11).
Figure 2. Survival Curves for Children in the Nurse-Family Partnership Trial.
A, All causes of death. B, Preventable causes of death. All 690 children who survived had at least 19.7 years of follow-up after birth. The numbers at risk of dying at 20.0, 20.5, 21.0, 21.5, and 22.0 years after randomization were 620, 369, 132, 4, and 1, respectively.
At child age 20 years, the preventable-cause mortality death rate was 1.6% (0.57%) in treatment 2 and 0.0% (SE not calculable) in treatment 4. The preventable-cause survival contrast of treatment 2 with treatment 4, shown in Figure 2B, was significant (P = .04).
Discussion
During the 2-decade period following registration in this trial, women enrolled in the 2 nurse-visited groups were less likely to have died than women assigned to the control group, and by age 20 years, children whose mothers received home visits during pregnancy and through child age 2 years were less likely to have died from preventable causes compared with their counterparts in the control group.
Although highly promising, these findings need to be understood in light of their limitations. First, the effect of the program on mortality was not hypothesized because of the infrequency of death among most groups in this age range.1 Second, the sparseness of the data and limited sample size for a study of mortality mean that the findings are sensitive to relatively small changes in the numbers of deaths in the intervention and control conditions. Third, had we formulated hypotheses at the start of this trial, we would have expected a linear ordering of home-visiting effects on maternal mortality, with the strongest effect being present for treatment 4, the group that received home visits through child age 2 years. Apparent differences between treatments 3 and 4 in maternal mortality are likely sampling artifacts.
Notwithstanding these limitations, the findings are noteworthy because mortality is an unequivocal outcome and its prevention aligns with the goals of the program and earlier program effects. Nurses are charged with improving maternal and child health by helping activate and support women’s motivations to protect their children and themselves.25,35,36 The program’s effect on maternal mortality from prenatal and postpartum visitation alone is plausible because pregnancy and the birth of first children activate mothers’ highly conserved brain based systems needed for children’s protection and development.43–45 Nurses’ support of mothers’ efforts to protect themselves and their offspring46 is likely to buffer the damaging effects of toxic stress on mothers’ rapidly changing neural circuitry and behavior during pregnancy and the puerperium.43–48
The reduction in external-cause maternal mortality in the 2 visited groups is thus noteworthy. A significant portion of the variance in these causes of maternal mortality is likely explained by maternal behaviors that require anticipation of risk and regulated behavior (eg, wearing seat belts and avoiding criminally involved individuals). Research47 with nulliparous pregnant rats emphasizes that gestation is a period of particular vulnerability for the developing fetus and mother, with mild stress affecting both maternal behavior and microRNA expression in the frontal cortex, a region involved in decision-making and maternal care. Moreover, structural changes inhuman brain regions involved in maternal motivation and behavior occur immediately following delivery.49
Given that the NFP is designed to help mothers anticipate risks and build skills to accomplish their goals,25,35,36 it is important that nurse-visited mothers in the Memphis trial reported a greater sense of mastery after randomization than did their counterparts in the control group19,23 and that self-efficacy and uplifting experiences in other studies have been found to attenuate pregnant women’s stress responses.50 Moreover, prenatal visitation produced positive changes before birth: women visited during pregnancy were more likely to use other community services and to have lower rates of yeast infection and pregnancy-induced hypertension than were women in the control group.19 Although the earlier Elmira trial found that the full program usually produced larger effects on maternal and child health than did prenatal visitation,29–33 adolescents whose mothers were visited during pregnancy alone, like those who underwent the entire program, had fewer arrests and convictions compared with adolescents in the control group.33
The reduction in child mortality due to preventable causes is consistent with earlier program effects on children’s duration of hospitalization for injuries,19 home environments,19 mothers’ beliefs associated with child abuse,19 mothers’ behavioral impairments resulting from substance use,24 children’s behavioral dysregulation,21 and children’s depression, anxiety, and use of substances.23 Moreover, we chose not to classify the following causes of infant mortality originating during pregnancy and the newborn period as preventable: extreme immaturity, chronic respiratory disease arising in the perinatal period, and infectious colitis, enteritis, and gastroenteritis. These causes of mortality were present only in the control group, so treating them as preventable would have increased the significance of differences.
Five features of these findings make them noteworthy. First, the findings are based on a randomized clinical trial with more than 2 decades of follow-up. Second, unlike many other outcomes, death is an unequivocal outcome measured validly. Third, survival was measured for all women randomized and all but 2 of the children born alive, nearly eliminating possible attrition bias. Fourth, this study is close to a population-based effectiveness trial because it enrolled a very large portion (88%) of the population invited to participate through a public system of care, and the program was delivered through the Memphis/Shelby County Health Department, where it was buffeted by many of the challenges found in public health delivery settings. Fifth, the effects of the program on both maternal and child mortality and their consistency with the program’s goals, objectives, and earlier effects increase the validity of each outcome. These findings should be replicated in well-powered trials with populations at very high levels of familial and neighborhood risk.
Conclusions
The relatively lower rates of death found among nurse-visited mothers and children compared with those in the control group are consistent with the effect of the program on earlier aspects of maternal and child health. These findings suggest that this intervention may have longer-term effects on health and mortality as the mothers and their children grow older.
Supplementary Material
Acknowledgments
The Prevention Research Center for Family and Child Health, directed by Dr Olds at the University of Colorado School of Medicine, has a contract with the NFP to conduct research to improve the NFP program and its implementation. Dr Olds and Mr Knudtson were employed by this center at the time the study was conducted. Dr Olds is the founder of the NFP.
Funding/Support: The current phase of this research was supported with funding from the National Institute of Drug Abuse (grant 1R01DA021624).
Role of the Sponsor: The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: Cheryl Loston-Williams (University of Colorado) helped to prepare this manuscript, Wendy Gehring (University of Colorado) assisted with data management, and Jamie McGregor, MD (University of Colorado), provided comments on the analysis. Mss Loston-Williams and Gehring received compensation from research grants for their work.
Footnotes
Author Contributions: Drs Olds and Knudtson had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Olds, Kitzman, Cole.
Acquisition, analysis, or interpretation of data: Kitzman, Knudtson, Anson, Smith, Cole.
Drafting of the manuscript: Olds, Kitzman.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Knudtson, Cole.
Obtained funding: Olds, Kitzman.
Administrative, technical, or material support: Kitzman, Anson, Smith.
Study supervision: Kitzman.
Conflict of Interest Disclosures: No other disclosures are reported.
REFERENCES
- 1.Murphy SL, Xu J, Kochabek KD. National Vital Statistics Reports. Deaths: final data for 2010. [Accessed May 23, 2014];National Vital Statistics Systems. 2013 61(4) http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf. [PubMed] [Google Scholar]
- 2.Dowd JB, Albright J, Raghunathan TE, Schoeni RF, Leclere F, Kaplan GA. Deeper and wider: income and mortality in the USA over three decades. Int J Epidemiol. 2011;40(1):183–188. doi: 10.1093/ije/dyq189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma J, Xu J, Anderson RN, Jemal A. Widening educational disparities in premature death rates in twenty six states in the United States, 1993–2007. PLoS One. 2012;7(7):e41560. doi: 10.1371/journal.pone.0041560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cullen MR, Cummins C, Fuchs VR. Geographic and racial variation in premature mortality in the U.S.: analyzing the disparities. PLoS One. 2012;7(4):e32930. doi: 10.1371/journal.pone.0032930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jemal A, Ward E, Anderson RN, Murray T, Thun MJ. Widening of socioeconomic inequalities in U.S. death rates, 1993–2001. PLoS One. 2008;3(5):e2181. doi: 10.1371/journal.pone.0002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kindig DA, Cheng ER. Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood) 2013;32(3):451–458. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- 7.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Health insurance and mortality in US adults. Am J Public Health. 2009;99(12):2289–2295. doi: 10.2105/AJPH.2008.157685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 9.Shonkoff JP, Garner AS Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 10.Powers DA, Song S. Absolute change in cause-specific infant mortality for blacks and whites in the US: 1983–2002. Popul Res Policy Rev. 2009;28:817–851. [Google Scholar]
- 11.Singh GK. Youth Mortality in the United States, 1935–2007: Large and Persistent Disparities in Injury and Violent Deaths: A 75th Anniversary Publication. Rockville, MD: Health Resources and Services Administration, Maternal and Child Health Bureau, US Dept of Health and Human Services; 2010. [Google Scholar]
- 12.Howell E, Decker S, Hogan S, Yemane A, Foster J. Declining child mortality and continuing racial disparities in the era of the Medicaid and SCHIP insurance coverage expansions. Am J Public Health. 2010;100(12):2500–2506. doi: 10.2105/AJPH.2009.184622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh GK, Kogan MD. Widening socioeconomic disparities in US childhood mortality, 1969–2000. Am J Public Health. 2007;97(9):1658–1665. doi: 10.2105/AJPH.2006.087320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matthews TJ, MacDorman MF. Infant mortality statistics from the 2009 period linked birth/infant death data set. NVSS. 2013;61(8):1–28. [PubMed] [Google Scholar]
- 15.Moon RY Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):e1341–e1367. doi: 10.1542/peds.2011-2285. [DOI] [PubMed] [Google Scholar]
- 16.Schnitzer PG, Covington TM, Dykstra HK. Sudden unexpected infant deaths: sleep environment and circumstances. Am J Public Health. 2012;102(6):1204–1212. doi: 10.2105/AJPH.2011.300613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kendrick D, Mulvaney CA, Ye L, Stevens T, Mytton JA, Stewart-Brown S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD006020.pub3. CD006020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olds D, Pettitt LM, Robinson J, et al. Reducing risks for antisocial behavior with a program of prenatal and early childhood home visitation. J Community Psychol. 1998;26:65–83. [Google Scholar]
- 19.Kitzman H, Olds DL, Henderson CR, Jr, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: a randomized controlled trial. JAMA. 1997;278(8):644–652. [PubMed] [Google Scholar]
- 20.Kitzman H, Olds DL, Sidora K, et al. Enduring effects of nurse home visitation on maternal life course: a 3-year follow-up of a randomized trial. JAMA. 2000;283(15):1983–1989. doi: 10.1001/jama.283.15.1983. [DOI] [PubMed] [Google Scholar]
- 21.Olds DL, Kitzman H, Cole R, et al. Effects of nurse home-visiting on maternal life course and child development: age 6 follow-up results of a randomized trial. Pediatrics. 2004;114(6):1550–1559. doi: 10.1542/peds.2004-0962. [DOI] [PubMed] [Google Scholar]
- 22.Olds DL, Kitzman H, Hanks C, et al. Effects of nurse home visiting on maternal and child functioning: age-9 follow-up of a randomized trial. Pediatrics. 2007;120(4):e832–e845. doi: 10.1542/peds.2006-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kitzman H, Olds DL, Cole R, et al. Enduring effects of prenatal and infancy home visiting by nurses on children: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):412–418. doi: 10.1001/archpediatrics.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olds DL, Kitzman H, Cole R, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life-course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):419–424. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olds DL. Prenatal and infancy home visiting by nurses: from randomized trials to community replication. Prev Sci. 2002;3(3):153–172. doi: 10.1023/a:1019990432161. [DOI] [PubMed] [Google Scholar]
- 26.Olds DL, Robinson J, O’Brien R, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110(3):486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- 27.Olds DL, Robinson J, Pettitt L, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics. 2004;114(6):1560–1568. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- 28.Olds DL, Holmberg JR, Donelan-McCall N, Luckey DW, Knudtson MD, Robinson J. Effects of home visits by paraprofessionals and by nurses on children: follow-up of a randomized trial at ages 6 and 9 years. JAMA Pediatr. 2014;168(2):114–121. doi: 10.1001/jamapediatrics.2013.3817. 24296904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the delivery of prenatal care and outcomes of pregnancy: a randomized trial of nurse home visitation. Pediatrics. 1986;77(1):16–28. [PubMed] [Google Scholar]
- 30.Olds DL, Henderson CR, Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]
- 31.Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged parents: a randomized trial of nurse home visitation. Am J Public Health. 1988;78(11):1436–1445. doi: 10.2105/ajph.78.11.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olds DL, Eckenrode J, Henderson CR, Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643. [PubMed] [Google Scholar]
- 33.Olds D, Henderson CR, Jr, Cole R, et al. Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. JAMA. 1998;280(14):1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- 34.Soares JF, Wu CF. Some restricted randomization rules in sequential designs. Comm Stat Theory Methods. 1983;12(17):2017–2034. [Google Scholar]
- 35.Olds D, Kitzman H, Cole R, Robinson J. Theoretical and empirical foundations of a program of home visitation for pregnant women and parents of young children. J Comm Psychol. 1997;25:9–25. [Google Scholar]
- 36.Olds DL. The prenatal/early infancy project. In: Price R, Cowen E, Lorion R, Ramos-McKay J, editors. Fourteen Ounces of Prevention: A Casebook for Practitioners. Washington, DC: American Psychological Association; 1988. pp. 9–23. [Google Scholar]
- 37.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12(7):462–468. doi: 10.1016/s1047-2797(01)00285-x. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Classification of Diseases and Injuries. [Accessed March 4, 2014]; http://ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD-9/ucod.txt.
- 39.Centers for Disease Control and Prevention. National 13 Center for Health Statistics. [Accessed March 4, 2014];International Classification of Diseases, Tenth Revision (ICD-10) http://www.cdc.gov/nchs/icd/icd10.htm.
- 40.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 41.Klein JP. Competing risks. WIREs Comp Stat. 2010;2(3):333–339. [Google Scholar]
- 42.Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16(3):1141–1154. [Google Scholar]
- 43.Clutton-Brock TH. The Evolution of Parental Care. Princeton, NJ: Princeton University Press; 1991. [Google Scholar]
- 44.Mayes LC, Swain JE, Leckman J. Parental attachment systems: neural circuits, genes and experiential contributions to parental engagement. Clin Neurosci Res. 2005;4(5):301–313. [Google Scholar]
- 45.Leckman JF, Feldman R, Swain JE, Eicher V, Thompson N, Mayes LC. Primary parental preoccupation: circuits, genes, and the crucial role of the environment. J Neural Transm. 2004;111(7):753–771. doi: 10.1007/s00702-003-0067-x. [DOI] [PubMed] [Google Scholar]
- 46.Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. J Child Psychol Psychiatry. 2007;48(3–4):355–391. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- 47.Zucchi FC, Yao Y, Ward ID, et al. Maternal stress induces epigenetic signatures of psychiatric and neurological diseases in the offspring. PLoS One. 2013;8(2):e56967. doi: 10.1371/journal.pone.0056967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leuner B, Glasper ER, Gould E. Parenting and plasticity. Trends Neurosci. 2010;33(10):465–473. doi: 10.1016/j.tins.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim P, Leckman JF, Mayes LC, Feldman R, Wang X, Swain JE. The plasticity of human maternal brain: longitudinal changes in brain anatomy during the early postpartum period. Behav Neurosci. 2010;124(5):695–700. doi: 10.1037/a0020884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nierop A, Wirtz PH, Bratsikas A, Zimmermann R, Ehlert U. Stress-buffering effects of psychosocial resources on physiological and psychological stress response in pregnant women. Biol Psychol. 2008;78(3):261–268. doi: 10.1016/j.biopsycho.2008.03.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.