Abstract
The authors present a model of interactive social psychological and relational feedback processes leading to human immunodeficiency virus (HIV) risk reduction behavior change among active drug users trained as Peer Health Advocates (PHAs). The model is supported by data from qualitative interviews with PHAs and members of their drug-using networks in the Risk Avoidance Partnership (RAP) project. Results suggest three mutually reinforcing social psychological processes that motivate PHAs to provide HIV prevention intervention to their peers and to reduce their own risk behaviors: development of a prosocial identity, positive social reinforcement from drug users and community members, and cognitive dissonance associated with continued risk behavior while engaging in health advocacy. These processes directly influence peer interventionists’ motivation and efficacy to continue giving intervention to their peers, and to reduce their HIV risk behaviors. The authors discuss implications of the model for continued research on effective HIV prevention in high-risk groups.
Peer-delivered interventions increasingly have been advocated to reduce human immunodeficiency virus (HIV) risk among hard to reach populations, such as active drug users, men who have sex with men (MSM), and youth (Broadhead, Heckathorn, Grund, Stern, & Anthony, 1995; Latkin, Sherman, & Knowlton, 2003; Sikkema et al., 1996; Weeks et al., 2009). Such interventions are thought to provide many advantages to other intervention strategies, such as small group or individual cognitive–behavioral interventions because of their ability to reach hidden populations and their relative cost-effectiveness (Broadhead et al., 1995; Dickson-Gomez, Weeks, Martinez, & Convey, 2006). In addition, peer-delivered interventions may be more acceptable to marginalized populations such as drug users, who are often mistrustful of health care professionals because they are delivered by individuals who are behaviorally and ethnically similar and draw on people’s intrinsic motivations to help others in their same circumstances (Broadhead et al., 1995; Friedman et al., 2004; Kelley, Murphy, & Lune, 2001; Latkin, 1998; Latkin, Hua, & Tobin, 2003; Weeks, Dickson-Gomez, Mosack et al., 2006). Indeed, many studies have found peer interventionists to be extremely effective at reaching hidden populations, and delivering prevention materials and messages (Amirkhanian, Kelly, Kabakchieva, McAuliffe, & Vassileva, 2003; Dickson-Gomez et al., 2006; French, Power, & Mitchell, 2000; Ross, Harzke, Scott, McCann, & Kelley, 2006; Simons et al., 1996; Van Khoat, West, Valdiserri, & Phan, 2003; Weeks et al., 2009).
Although peer-delivered interventions are based on the assumptions that social norms, group processes, and peer pressure are key factors in individual behavioral decision making and practices (Broadhead et al., 1995; Kelly et al., 1992; Latkin, 1998; Sikkema et al., 2000; Trotter, Bowen, & Potter 1995), the ways that these are conceptualized and put into practice differ significantly among interventions that fit under the “peer-delivered” umbrella. Peer-delivered interventions at the most basic level utilize a small number of individuals who belong to the target population to deliver HIV prevention intervention (Elford, Bolding, & Sherr, 2001; Elford, Hart, Sherr, Williamson, & Bolding, 2002; Flowers, Hart, Williamson, Frankis, & Der, 2002). These often are not theory-based, the intensity of intervention with the peer leaders is not sufficient to train leaders to meaningfully address psychosocial factors associated with risk and protective behaviors with peers, and the number of individuals recruited as educators is often insufficient to meet the critical mass needed to effectively change social network norms (Kelly, 2004). Other interventions have addressed the critical mass issue by using respondent-driven sampling (RDS) to efficiently reach large numbers of hidden and at-risk populations, such as injection drug users (Broadhead et al., 1995). In these interventions, initial “seeds” are recruited and given a very brief HIV prevention intervention. They are then asked to give the intervention to their peers and recruit peers using coupons to respond to a survey that assesses whether they have received accurate HIV information from their recruiter. These recruited individuals then receive the intervention and are trained to give the intervention to their own peers and recruit others in a similar fashion. However, the intervention received by those recruited by RDS is of necessity rather shallow. In addition, the lack of pre- and posttest design makes it difficult to ascertain whether the intervention achieves risk reduction behavior. Another approach is to recruit and deliver interventions to personal networks of friends who then support one another in putting risk reduction behaviors into practice (Trotter et al., 1995). While using the rules of etiquette and social support common in friendship groups, these interventions are unlikely to move beyond the social network level. Finally, other peer-delivered social network interventions offer opportunities for change at multiple levels including individual behavior change, social network change, and larger community level as actions by a large cadre of trained peer interventionists and support from their peers create a social movement to improve the health of the targeted population (Kelly, 2004; Weeks et al., 2009). These train large numbers of the target population to be peer educators to others in their networks and among crack users in the community (Kelly, 2004; Latkin, Sherman et al., 2003; Weeks et al., 2009). Some interventions such as the Popular Opinion Leader (POL) carefully select members who are well-respected in their networks to deliver prevention messages to their peers (Kelly et al., 1992; Sikkema et al., 2000), whereas others train any member of the target population willing and able to attend training sessions (Latkin, 1998; Weeks et al., 2006). Training is intensive and occurs over several sessions with ample opportunity to address psychosocial barriers and motivations to encourage peers to reduce their risk behavior, and time to practice the intervention and receive feedback and encouragement from facilitators to sustain peer intervention over time. While POL focuses on training individuals in particular venues (e.g. gay bars or low-income housing projects), other peer-delivered interventions, like RAP evaluated here, use larger sociometric networks to deliver interventions to hidden populations of drug users who may not frequent particular venues.
This latter group of peer-delivered interventions has been found to lead to significant risk reduction among peer interventionists themselves, often to a greater degree and longer term than in those who simply receive small group or individual level interventions (Kelly et al., 1997; Latkin, Sherman et al., 2003; Sikkema et al., 1996). In fact, randomized controlled trials of peer-delivered interventions have found significantly greater reductions in risk behavior than among equal-attention control conditions, including small group or individual cognitive behavioral interventions (Sikkema et al., 1996). Further, these improvements were not attributable to improvements in self-efficacy (Kelly et al., 1997). Clearly, the greater risk reduction among those who advocate risk reduction among their peers cannot be fully explained by individual-level cognitive changes such as their attitudes, intentions, and motivations. Although social influence processes have been proposed as the major mechanism influencing HIV risk reduction among outreach contacts, less is understood about social psychological processes causing peer health interventionists to reduce their own risk (Coyle, Needle, & Normand, 1998; Latkin, Sherman et al., 2003).
Here we present a model of interactive social psychological and relational mechanisms, intensified through feedback processes, which we propose as an explanation of the significant HIV risk-reduction behavior change among high-risk individuals who become interventionists among their peers. This model draws from social psychological theories combined with an inductive theory building process following iterative, systematic analysis of qualitative evaluation data from the Risk Avoidance Partnership (RAP) peer intervention study. These qualitative data, including in-depth interviews of active drug users participating as Peer Health Advocates (PHAs) and their peers who received the intervention, and observations of PHAs’ intervention encounters, provided extensive information on social processes, experiences, and personal factors that affected these PHAs in the course of their implementation of peer intervention. These data shed light on the meaning of peer health advocacy for peer interventionists and illustrate the processes by which participating in delivery of HIV prevention intervention leads to significant and sustained behavior change among those engaged in delivery.
MODELING SOCIAL PSYCHOLOGICAL FACTORS AFFECTING RISK REDUCTION AMONG PEER INTERVENTIONISTS
Three major social psychological theories have been hypothesized by researchers to explain risk reduction among Peer Interventionists, including cognitive dissonance, social identity theory and social reinforcement (Latkin, Sherman et al., 2003). In fact, the mutlilevel peer delivered interventions described above are based on these theories (Latkin, Sherman et al., 2003; Weeks et al., 2009). Further, in describing their reasons for participating as Peer Interventionists and their motivations for changing their own behavior in in-depth interviews, participants described processes that are consistent with these theories. We model these key social psychological mechanisms, their relationship with individual-level cognitive behaviors, and the ways they may be mutually reinforcing in Figure 1. Below, we briefly present the theories and their implications for peer interventionists in general. We will then present qualitative data from our study that illustrate each mechanism. Finally, we will discuss the implications of qualitative results for intervention refinement and suggest areas for further research.
Figure 1.
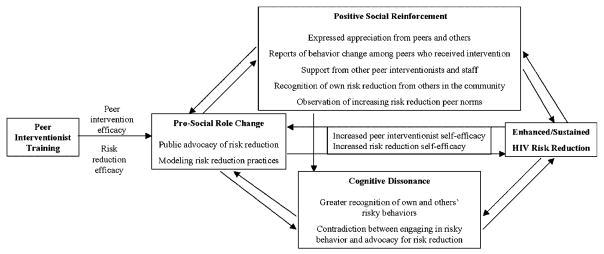
Social psychological dynamics of enhanced human immunodeficiency virus (HIV) risk reduction among peer interventionists.
Prosocial identity change among peer intervention providers is the first theme reported by peer interventionists as causing them to change their own behavior. The Peer Interventionist role consists of two activities: public advocacy for HIV risk reduction with a group of peers also engaged as Peer Interventionists and modeling risk reduction behaviors among their peers in community settings. Modeling risk reduction can also occur in two ways, including demonstrating proper harm reduction practices in outreach encounters (e.g. condom use, or cleaning used syringes with bleach) and practicing these behaviors in the presence of peers or sex partners. Social identity theory posits that when individuals identify with a group, the collective group concept becomes part of their self-concepts (Tajfel, 1981; Turner, 1978). In this process, a redefinition of self occurs and individuals’ behaviors tend to become congruent with the group’s goals and actions. Therefore, social identity theory would predict that Peer Interventionists would develop prosocial identities as they identify with a larger group of peers engaged in health promotion in their communities. This prosocial identity may be particularly salient to participants with stigmatized identities as drug users. In addition, changed identity may stem from the empowering effect of engagement in health advocacy (Brown, 1991). Further, the role of peer interventionist may be meaningful to participants and motivate them to practice risk reduction themselves and acquire new skills to fulfill the role of advocating behavior change among their peers and thereby increase their risk reduction self- efficacy (Latkin, Sherman et al., 2003; Purcell et al., 2004). Successfully implementing peer intervention may sustain and increase their peer interventionist self-efficacy, that is, their sense of competency in fulfilling this new role (Weeks, Convey, Dickson-Gomez et al., 2009).
Positive social reinforcement for HIV prevention outreach is a second mechanism that may influence peer interventionists to reduce their own HIV risk. Social reinforcement includes expressions of appreciation from peers and other community residents, observed or reported risk reduction among peers as a result of peer interventionist influence or prevention materials received from those interventionists, recognition of peer interventionists’ own risk reduction by their peers, increasing evidence of risk reduction norms among peers, and support and praise from other peer interventionists and project staff. Recognition of and social approval for the peer interventionists’ role may increase their commitment, motivation, and self-efficacy to continue in this role. Social reinforcement may also contribute to further role change (Latkin & Knowlton, 2005; Ramirez-Valles, 2002). Support to continue the peer-interventionist role by their peers and other members of the community may encourage them to expand their role and see themselves in a new light. The reward of social recognition might also, in turn, lead them to directly reduce their own risk behavior to model risk reduction practices to other drug users in their community. Recognized behavior change among peer interventionists and their peers reinforces social norms supporting risk reduction and penalizing risky behavior.
Cognitive dissonance is a third mechanism that may explain the greater than expected risk reduction among peer interventionists. It has long been observed in social psychology that inconsistencies between behavior and attitudes can lead to changes in attitudes to conform to behaviors, or the reverse (Bem & McConnell, 1970; Festinger, 1957). In the case of peer interventionists, inconsistencies between health promotion behaviors (advocating risk reduction among their peers) and engaging in risk behaviors themselves may lead them to reduce their own risky practices. Providing some support for this hypothesis are results of peer-delivered interventions that indicate that injection drug users who talked to their peers about HIV were less likely to practice injection risk themselves (Davey-Rothwell & Latkin, 2007). In addition, laboratory experiments have shown that cognitive dissonance, created by making participants aware of their past failure to use condoms consistently and persuade others to use condoms, increased condom use intentions (Aronson, Fried, & Stone, 1991). Although in classic cognitive dissonance experiments, participants’ are unaware of their attitude shift (Bem & McConnell, 1970; Festinger, 1957), this may be related to the task they are asked to perform (e.g., rating how interesting a tedious task is under different levels of incentives). In the case of risk reduction among drug users, participants may be more aware of inconsistencies between risk reduction behaviors and their own continued risk, particularly when advocating risk reduction to people with whom they have engaged in risk behavior such as people with whom they have shared drugs.
The second source of cognitive dissonance is through an increased recognition and awareness of the risks of their own behavior by observing others’ risky practices. Social reinforcement may increase cognitive dissonance if public recognition of behavior change and expressions of appreciation do not match peer interventionists’ private behaviors. Changes in social norms among peers to support risk reduction practices may also increase cognitive dissonance if behavior conflicts with newly established group norms. Further, feelings of cognitive dissonance may reinforce peer interventionists’ desire to model risk reduction practices.
Little research, however, has examined how these hypothesized social psychological processes (prosocial role change, positive social reinforcement, and cognitive dissonance) help to account for behavior change among peer interventionists. Individual-level cognitive (attitudinal, motivational, and efficacy) processes may, in fact, be reinforced by the social psychological processes that are in themselves mutually reinforcing. This interactive process may explain not only the observed greater risk reduction outcomes in peer interventionists themselves, but also suggests a greater probability of sustained risk reduction if the cycle of peer intervention delivery continues.
METHOD
The Risk Avoidance Partnership (RAP) was a 4-year project that began in December 2001. The RAP project was multitheoretical and incorporated social learning theory (Bandura, 1977, 1994), stages of change models (Prochaska, Redding, Harlow, Rossi, & Velicer, 1994), diffusion of innovations theory (Rogers, 1995), and social empowerment theory (Brown, 1991). Through the peer-delivered intervention, RAP utilized social networks and teachable moments to popularize risk reduction practices and establish HIV preventive norms (French, Power, & Mitchell, 2000; Kelly et al., 1992; Neaigus, 1998; Trautmann, 1995) based on the assumption that social influences, peer norms, and peer pressure are key factors in individual behavioral decision-making and practices. The RAP project drew on diffusion of innovations theory (Rogers, 1995) by training active drug users to deliver HIV prevention intervention materials, messages, and models to their drug-using peers in community settings. Although some peer intervention models emphasize careful selection of peers (Kelly et al., 1992), others allow any member of the target population who is able and willing to take on the new role to become a peer interventionist (Latkin, Sherman et al., 2003). In RAP, we used a combination of these two approaches. In the first months of the project, we selected active drug users who were “central” to drug-using networks, defined as those with a large number of members in their personal networks, or those who were gatekeepers of a drug use site. Later, we opened the project to any drug users who expressed interest in and willingness to become peer interventionists. Baseline comparisons with candidates from the first months of recruitment with those recruited after it was opened to any drug user found no statistical differences in gender, ethnicity, drug network size, retention rate, and self-reported number of peers with whom they gave prevention information, materials or demonstration during the 6 months before their training cycle began (Weeks, Li, Dickson-Gomez et al., 2009).
We initiated training with 129 active drug users to become Peer Health Advocates (PHAs) to provide peer-delivered HIV prevention and harm reduction intervention to other drug users in their networks and communities. The training curriculum consisted of both a four-session in-office program and one to six additional staff-partnered field sessions designed to support PHAs’ delivery of the RAP peer-led intervention. The latter included delivery of prevention materials, health promotion advocacy, information and slogans, and demonstration of preventive practices to their peers. Training was provided in 28 cycles to groups of three to eight trainees; 112 completed sessions one through five to become fully trained PHAs. These trained PHAs were invited to attend monthly community advocacy group (CAG) meetings to reinforce risk reduction practices and methods for talking to peers, to restock with prevention materials, and to learn about other advocacy and prevention opportunities in the city.
The evaluation design of the RAP PHA training curriculum and RAP peer-led intervention included a prospective study with pre- and post-assessments (baseline and 6 months) of risks and prevention efforts of the PHAs and two of their direct Contact Referrals (CRs), who were members of their drug-using networks. Peer Health Advocates who completed the RAP training were more likely to be African American than those who did not complete training. There were no ethnic differences between recruited PHAs or the CRs. Peer Health Advocates and CRs also did not differ significantly by their level of education, employment status, income, homeless status, or having received drug treatment in the last 6 months (Weeks, Li et al., 2009). This suggests that despite the initial recruitment strategy, PHAs did not differ significantly from the target population of drug users.
Peer Health Advocates who completed five sessions of the training also received a qualitative assessment 3 months after baseline of their responses and reactions to the PHA training program and their initial self-reported effectiveness in delivering intervention to their peers. Diffusion of the RAP intervention from PHAs to other drug users in the city was assessed through measuring RAP intervention recognition and effects within participants’ personal networks. The project also included in-depth interviews with PHAs and their peers and observations of intervention trainings and PHAs in the field to shed further light on how and in what ways the intervention worked, and processes that may explain observed behavior change. We drew primarily from these qualitative data to develop and illustrate our model of the social psychological mechanisms we hypothesize affect PHA risk reduction and interventionist changes.
Qualitative Data
Two ethnographic researchers experienced in conducting qualitative research with active drug users collected the qualitative data. One ethnographer (JDG) had a doctorate degree in anthropology; the other (MC) had a master’s degree in anthropology. The ethnographers attended PHA training to collect process data for the project. They were able to observe in-office training and field sessions, came to know PHAs throughout the length of the participation in the project, in many cases for several years, and gained significant rapport with participants, which facilitated in-depth interviews.
Observations
The project ethnographers attended training sessions and CAG meetings, and accompanied PHAs in their staff-partnered field sessions. Ethnographers documented observations in detailed field notes. They conducted observations of 98 project activities including 26 in-office training sessions, 64 staff-partnered field sessions, and 8 CAG meetings. Field notes of in-office training sessions focused on PHAs’ reactions to training components. Partnered session observations focused on where the outreach was conducted, with whom, what information or materials PHAs provided, and peers’ reactions to PHAs’ attempts to engage them in HIV prevention discussions. Community advocacy group meeting observations focused on who was present and the topics discussed, including problems encountered in continuing PHA work and structural barriers to risk reduction among active drug users.
In-depth interviews
The same ethnographers who observed training and partnered field sessions conducted in-depth interviews with 32 PHAs and 24 CRs. This purposive sample was designed to reflect the diversity of the larger sample of RAP PHAs and their CRs in terms of gender, ethnicity, and drug of choice. We also selected PHAs who remained active as peer interventionists and those who dropped out after finishing their in-office training sessions. Interviews with PHAs focused on their positive and negative experiences conducting PHA outreach, the meaning they gave to these experiences, their experiences with monthly CAG meetings, problems in their community that were addressed or not addressed by RAP, their assessment of risk and harm reduction behaviors in drug users they know, and their own changes in behavior as a result of participating in RAP. Participants received $25 for completing in-depth interviews. Demographics of PHAs who completed their training, those who recruited but did not complete training, CRs, and the in-depth interview sample are included in Table 1.
Table 1.
Baseline Demographics of Fully Trained Peer Health Advocates (PHAs), Recruited but Untrained PHAs, Contact Referrals (CRs), and PHAs and CRs Who Completed In-Depth Interviews
| Trained PHAs (N = 110) % | Untrained PHAs (N = 64) % | CRs (N = 223) % | In-depth PHAs (N = 32) % | In-depth CRs (N = 24) % | |
|---|---|---|---|---|---|
| Female Ethnicity | 37.5 | 29.7 | 22.5 | 43 | 46.4 |
| Puerto Rican | 40.2 | 48.4 | 39.6 | 43.8 | 25 |
| African American | 55.4 | 32.8 | 51.4 | 43.8 | 46.4 |
| White | 4 | 18.8 | 9.0 | 9.4 | 32.0 |
| Less than high school | 58.1 | 45.3 | 48.7 | ||
| Unemployed | 78.6 | 82.6 | 75.7 | ||
| Homeless | 48.2 | 49.2 | 48.6 |
Analysis of Qualitative Data
All in-depth interviews were transcribed verbatim. Transcripts and field notes were entered into Atlas.ti (Muhr, 1997–2004) for analysis. Data analysis proceeded using an iterative and multistep process (Emerson, Fretz, & Shaw, 1995). Interviews were first sorted and labeled by participant demographic characteristics, participant type (PHA, CR), type of data (observation, interview), and for observations, as well as type of event (in-office training session, staff-partnered field session, CAG). We then coded text data content. Twenty-four codes were generated both deductively, from our theoretical framework, and inductively, from themes identified in patterns of responses and observations in the data. Deductively derived codes included the meaning of PHA work for participants, others’ reactions to PHAs’ outreach work, and motivations and barriers to participating in the RAP project. Inductive analysis using these preliminary codes revealed additional themes, in particular those that contributed to the model presented here. We then applied these new codes to the data. For example, under the code for experiences as PHAs, participants reported expressions of gratitude from drug-using peers and other community members, behavior change among drug-using peers, recognition by peers of their own behavior changes, and support from other PHAs and staff. Although other themes were identified that acted as barriers to engaging in PHA work (e.g., homelessness, prison, illness, morning withdrawal symptoms), many of which also acted as barriers to PHAs’ reducing their own HIV risk (e.g., homelessness), we focus on the factors that contributed both to continuing in the PHA role and reducing HIV risk in this article.
We ran reports (output), maintained memos (researcher comments and interpretations) and revised our conceptual model as the third step in the qualitative analytical process. In this stage, we examined the relationships among codes and the processes that may explain them. In particular, we discovered the mutually reinforcing processes of many of the concepts during this phase of analysis. Coding occurred collaboratively between the two ethnographers, the principal investigator, and other members of the research team until consensus was reached regarding the content of coding, the application of codes to particular text segments, and the model to explain processes relating the codes to each other.
RESULTS
Previous Results and Unanswered Questions
Outcome analyses for the RAP intervention for the pre- and post-surveys are published elsewhere. In brief, all participants in the RAP project (both PHAs and CRs) reported significant reductions in a number of drug and sexual risk behaviors between baseline and 6-month interviews, indicating significant dissemination of the intervention and changes in social norms supporting risk reduction. Peer Health Advocates showed greater risk reduction on almost all outcome measures than CRs although these differences were not statistically significant. In addition, PHAs were significantly more likely to have given HIV prevention information or materials to their personal network members than CRs (p < .001) (Weeks, Li et al., 2009).
More germane to this article, for PHAs, having other PHAs in their social networks and being close to a PHA in their personal network who was actively involved in promoting intervention among peers was strongly associated with engaging in peer intervention among PHAs. Additionally, engaging in giving peer intervention was associated with reduced HIV risk. For PHAs who were injection drug users, giving HIV prevention intervention to peers was significantly associated with reduced injection frequency, whereas for all PHAs giving HIV prevention intervention to peers was associated with reduced sexual risk (Weeks, Li et al., 2009). These results suggest that actively engaging in peer intervention work was associated with reduced risk among PHAs, although the social psychological mechanisms for this association have not yet been fully explored.
Interestingly, CRs reported that PHAs provided them with HIV prevention materials, information, and demonstrations of risk reduction practices significantly more often than PHAs reported delivering such interventions to their peers (Weeks, Li et al., 2009). This suggests that although ethnographers were present during training and observing PHAs’ outreach with peers, social desirability bias was minimal and lends further support to our qualitative findings. Qualitative process and outcome data, illustrated through participant quotes, provide evidence of the processes and key factors that may account for PHA efficacy as peer interventionists and their greater risk reduction, as indicated in our model (Fig. 1).
Prosocial Identity Change
Many PHAs initially expressed nervousness in fulfilling their role as PHA, particularly before their first partnered session with staff. They feared negative reactions from their drug-using peers because they themselves still used drugs. However, most were pleasantly surprised by the positive reactions they received from their peers, and said that they enjoyed their new role as a PHA.
Like during the training class, I was like wow, you know, I don’t know how I’m gonna approach people…How they gonna look at me, especially people I get high [with], you know, and know that I get high. But it was nothing like that though…It was just the utmost respect. (Puerto Rican Man)
Although PHAs also reported negative reactions from peers, facilitators prepared them for situations in which negative reactions might arise, for example, when drug users were sick with withdrawal symptoms or in the presence of people who might not know they use drugs. Peer Health Advocates, thus tended to avoid these situations. However, some negative reactions were inevitable. Training facilitators, all of whom were experienced outreach workers, shared their experiences with negative reactions with PHAs during in-office training and field sessions. They assured PHAs that some people just are not ready to listen to prevention messages, but that some people who may be initially resistant change their behaviors over time. Thus, these relatively rare negative reactions seldom led to frustration among the majority of PHAs interviewed.
For most PHAs, just a few partnered sessions were enough to make them feel like they could be successful in this role (i.e. their sense of self-efficacy as peer interventionists increased). Indeed, prior analyses showed that PHA self-efficacy improved significantly 3 months postintervention (Weeks et al., 2006). Most PHAs began by talking to drug users they knew on the streets in their own neighborhood. Over time, many also incorporated PHA work into their daily activities by carrying prevention materials with them to the places they spent time and used drugs (Dickson-Gomez et al., 2006).
Peer Health Advocates reported that their enjoyment of the PHA role increased over time. They liked talking to people who needed help and serving as a positive role model for others in the community. These rewards may be especially important for drug users who suffer from multiple marginalizations. The vast majority of participants did not have regular employment. Most had criminal histories. In addition, the majority had also lost their parental responsibilities as a result of their drug use. PHA work, therefore, was a way for them to feel like they mattered and could contribute something to society.
So I like it ’cause I get to go out, talk to people. And I feel like somebody. It makes me feel good. I feel like somebody today… Some people are just taking it [the money as incentive] to do it, you know. But everybody’s different. But some people are serious about this. They like it. And I like it because I get to talk to them and they teach me out there, the guys that are out there, or the girls, and they ask me [questions]. And if I know, I’ll tell them. I tell you, when we put that pack thing [backpack with prevention materials] on the back, we feel like we’re doing a special job. And it’s good. I love it. (Puerto Rican woman)
Most PHAs we interviewed admitted to being initially motivated by the incentive payments received for attending training and field sessions. Almost all, however, expressed genuine surprise that their motivation changed as they started to enjoy their new role. In other words, the PHA role, advocating risk reduction and serving as a role model, was intrinsically rewarding to them. In the quote above, the participant mentions the materials given by the project, including backpack, t-shirts, and project materials that helped identify them to others as PHAs. As the participant mentions, she and others began to feel that they were doing a “special job” and “felt like somebody.” The social support of other PHAs may also have contributed to their motivation to continue in this role, and the positive feedback they received from peers reinforced this changed identity.
Social Reinforcement
All PHAs reported that other drug users and family members recognized and approved of the work the PHA was doing. Peer Health Advocates reported that people close to them congratulated them on doing something positive and helping to reduce HIV. For many, this public recognition reinforced their commitment to PHA work.
But you know, it felt good…Because people look up to you. Even though they know you may use, but they saw you doing something positive, you know, within the community, so they would like, “God, you know, that’s kinda nice what you’re doing.” (Puerto Rican Man)
My mom has been proud of me because like I said, I was out of control… She said, “That is what you need to do. Do something positive for society. Don’t be doing things to hurt yourself and other people.” (Puerto Rican woman)
Peer Health Advocates reported that drug users in their community and family members favorably contrasted this new role with their former actions and behaviors that were often centered on obtaining and using drugs.
You’re focusing on something other than just the streets, or on getting high and going out and copping [acquiring] drugs, you know. And it’s just, when you’re caught out like that, it’s all you think about. You don’t think about eating. You don’t think about your family. (Puerto Rican man)
Being a PHA gave participants a way to interact with other drug users in their community without using drugs themselves. Many drug treatment programs admonish drug users to avoid “people, places and things” that they associate with getting high. For inner-city drug users, this admonition is difficult to follow, as drug use is ubiquitous in their neighborhoods, and many of their childhood friends and even family members may also use drugs. As mentioned, the majority of PHAs were unemployed. Providing peer intervention, therefore, gave drug users attempting to cut down or abstain from drug use something to fill the time that was previously filled with obtaining and using drugs.
Other PHAs were motivated to continue in their role after seeing behavior change in one or more of their drug-using peers. Some said that helping one person reduce their risk for HIV was enough to make them feel they were successful in their role.
A friend of mine…came to my house because at the time I used to let people fix themselves [inject] and they give me $5 or $10… I [had] just kind of finished the program [RAP]… so I explained to him what was going on. He realized what he was doing was wrong. I guess he was embarrassed that I told him. That it came from a woman. Then after that I didn’t see him. Then three days later he came here and then started the [RAP] program. Then after that he got himself to an inpatient [drug treatment program]. He is doing real good. It makes me feel good because since that day I guess I opened his eyes on what was going on. It showed me that at least somebody is listening to me. I’m not just talking and there is not action…That makes me fight for more and help more people. (Puerto Rican woman)
For many PHAs, ultimate success was defined as getting a heavy drug user into treatment so that he or she might abstain from drug use altogether.
Others felt successful by supporting those who needed help and were socially marginalized, for example, female sex workers or homeless drug injectors.
My heart was for the women that worked the streets because they want to please. They want to do whatever it takes to get whatever they are going to get, regardless of the danger of their own self. By me being out there and being in that predicament and knowing how, “Oh, I won’t use a condom because if I use a condom he won’t give the money.” I would say [to them] “Put this condom in your mouth and they would never, never know. Use the condom always. That is the best part about the female condom. He never even has to know”…They aren’t going to be looking down there anyway. All they want to do is get their thing off (African American woman)
Both of the PHAs quoted above felt a great deal of identification with the people they helped. They recognized that they had been in similar situations and taken similar risks and felt proud that they were able to help them.
Many Contact Referrals (CRs) we interviewed reported that they saw changes in the PHAs who were more likely to practice risk reduction like using new syringes or bleaching used ones. When their peers mentioned the positive changes they saw, PHAs expressed a sense of pride because they saw themselves as not just “talking the talk, but walking the walk” by modeling risk reduction behavior in everyday practice.
One thing that I loved when he [drug-using peer] talked to me one time, he told me that he saw a lot of difference in me. Even if I was on drugs he would say, “I see a lot of difference in you because you change. If you don’t have bleach or an alcohol pad, you don’t want to go and get high out there.” Every time we used to get high, we used to get a new kit. (Puerto Rican man)
Recognition of behavior change in PHAs motivated them to continue their role as advocate for and model of risk reduction among their peers.
Risk reduction changes observed in PHAs and in their peers also helped create new social norms for risk reduction behavior.
We had a lot of change ’cause the few people that usually come over to my house and get off…I let them read the [RAP Intervention] book. Like one guy I been running the streets with over 50 years, well, he said, “You know, this is a lot of stuff that we really didn’t [practice].” I say, “Yeah, man, this book is enlightening.” So, like I said, we all follow the rules. And if we’re not together and they with somebody else, they always tell them, “Look man, you gotta do this and do that, or else you can go by yourself.” Like even the dirty cookers [bottle caps used to mix or heat drug solutions]…Every time we go to the needle van, we get a new kit, you know. Water, bleach, the cotton and everything…And they [other people] still don’t clean their works with the bleach…It’s just ridiculous…Like I said, “That’s on you though…I’m telling you how to save your life. And you don’t wanna take heed to that. You’re not hurting me, you’re hurting yourself, “cause I’m not gonna do drugs with you” (African American man)
Qualitative data indicate that PHAs’ and their peers’ recognition of mutual behavior change create risk reduction behavioral norms. As indicated in the quote above, social norm change includes not only support for risk reduction practices within the PHAs’ social networks, but also penalties for those who do not comply with the new norms. If group members did not “follow the rules,” they were not allowed to be part of the bartering drug use network of this PHA and his close friends. Supportive norms for risk reduction and sanctions against those who did not practice them are additional mechanisms through which PHAs and their social networks reduce their HIV risk.
Finally, support from other PHAs and project staff was important in motivating many participants to continue in their PHA role. Many received continuing support from staff in their staff-partnered field sessions or when they stopped by project offices to receive bleach kits and condoms to continue their PHA work. In addition to supporting the outreach and providing materials, project staff supported PHAs by encouraging them to continue in their role, emphasizing the importance of the work they were doing, and even helping support them in times of personal crisis by, for example, helping them enroll in in-patient drug treatment programs when they desired. Peer Health Advocates also received support from both staff and other PHAs during monthly Community Advisory Group meetings as described by the participant below.
PHA: I’m so mad. I just missed the last one because I was in the hospital…I looked forward to that meeting once a month like I looked forward to the training because that would have been a good chance to see everybody. Or see the dedicated ones…The ones that paved the way so we could be there. They are still there. That is what I am wondering about. Why are they still coming? Interviewer: Why do you think?
PHA: I don’t know, but I better keep coming too. They know something is wrong though. They are still working. You asked me if I see people. Okay I see people from my training…But old people [the ones who went through the training in early cycles], the old timers they are working. They are working bad. These are the people who I met in the beginning when I first started using. I used with some of them and I can remember then they had that little bottle of bleach and that crazy looking cooker. I remember that…It is crazy how our lives pass. You never know who you are really getting high with. There is more to them than what they are doing [using drugs]… PHAs are here to stay. Too much up here to just let go. I couldn’t stop if I wanted to. Couldn’t. (African American woman)
Although many PHAs conducted active outreach outside of formal outreach sessions (Weeks et al., 2006), a few became highly active interventionists, defined as the top 5% of PHAs in terms of the number of peers to whom they gave HIV prevention intervention. It is probable that the participant is referring to people like these when she refers to “the dedicated ones” who went above and beyond what was expected of them in the project, and who continued to be active long after they stopped receiving project incentives. When this participant talked about these PHAs, she implied that they do it because many drug users are still putting themselves at risk for HIV and other diseases. As long as some people still do not know how to protect themselves or choose not to either because they are new injectors or because they are not motivated to change their behavior, she feels that there will still be a need for PHAs to work in the community of drug users. The fact that other PHAs continued providing peer intervention after their formal training ended, and that some had been advocating risk reduction for a number of years, helped motivate and encourage her to keep working as a peer interventionist.
Cognitive Dissonance
Peer Health Advocates described several ways that their participation in the project helped them reduce their own risk. Some saw contradictions between telling others how to reduce their risk and their own continued risk behaviors, and were thus motivated to change their behaviors to be more consistent with the risk reduction practices they were advocating. For many PHAs this included attempting to cut down on or abstain from drug use altogether. This is surprising considering that the RAP project advocated harm reduction and did not require PHAs to cease drug use to participate in the project. In fact, being an active drug user was an eligibility criterion to enter the project, though participants could remain in the project if they stopped using.
Every time I would go out and someone would listen to me…and I could answer their questions, I definitely felt like a leader. I do believe that this program helped me stay sober…because I was in the process of becoming sober before I got here. So it did help me become sober towards the end, but also stay sober. It is just like raising kids. When you are raising kids you are telling them right from wrong, you tend to do more right than wrong because you don’t want your kids doing wrong. If you are out there preaching, “You shouldn’t use drugs or if you do, use these things. You need to protect yourself, use this kit…if you shoot coke or whatever.” You tend to do what you are preaching because, me, I would feel like a hypocrite and I imagine most people would. It helps keep you in check. (White man)
As can also be seen in this quote, having people ask him questions and listen to his answers (social reinforcement) made him feel like a leader (prosocial identity). In turn, being recognized as an expert by his peers increased his feelings of cognitive dissonance (feeling like a hypocrite if he continued to put himself at risk for HIV, or continued to use drugs) and motivated behavior change to be consistent with his role. Although relapse is common among substance users and also occurred among those in our sample of PHAs who achieved a period of sobriety, no PHAs reported relapsing because of being around drug users or observing drug use. In fact, more often PHAs expressed a desire to abstain from drugs as a result of engaging in PHA work.
Others described becoming more aware of their own risks as a result of completing the PHA training and doing outreach. In particular, PHAs reported seeing the behaviors of other drug users and recognizing that they also had taken similar risks by not cleaning their injection works or not using condoms. In other cases, others’ risk taking and its consequences gave them a sense of what could happen to them if they did not change their own behavior.
PHA: When I first came into the RAP program I was still using cocaine. It wasn’t long until I started really going out and see people [when I was] sober because when I would leave here I would go out onto the street with [my staff partner] and I would see all these people and I would be sober. I wouldn’t come here high. It meant a lot to me to do this. It made me feel like I was somebody…
Interviewer: When you said that you saw people sober, what did that mean? PHA: Saw people using when I was sober…It makes me angry. I shouldn’t feel angry. It’s more anger at myself. Maybe it’s not even anger, it’s embarrassment. Like, God, I used to look like that. I used to smell like that. I used to act like that. Straighten out…So for me just being out there and seeing people that were high I found myself doing things…I went out by myself [after] I had finished the six months. I ended up carrying around gloves because there was a gentleman that I found on Park Street that he was in the same place every day and he was just so high all the time and he had an abscess that he would use [inject in] the same abscess in his arm. He’s going to lose his arm and it was so big and there was nothing I could do for him but tell him you need to go see somebody and explain to him, “Here’s your alcohol pad. Please wipe this down before you inject. Don’t use that site. Clean your needles.” I was going through the whole thing with him. He was so high he wasn’t listening or he couldn’t listen. I just put the antibiotic cream on him and bandaging him up and walking away with a feeling of sadness, this guy is going to die or he is going to lose his arm and that could be me. [White woman]
Although we did not prohibit PHAs from using drugs to participate in the project, we did ask that they not use when conducting partnered field sessions with staff. Being relatively sober may have helped PHAs see others’ risk behaviors in a new light. Some PHAs said that it was the increased knowledge about HIV risks gained from the RAP training that helped them recognize others’ risk behavior. Other PHAs said it was seeing people on the streets that were “even worse than them,” i.e., heavier heroin users, engaging in greater risk behavior and homelessness. Underlying the empathy that motivated PHAs to continue outreach among the most marginalized drug users was the heightened recognition of their own risk behaviors, “that could be me.” The discomfort caused by seeing their own risk behaviors and the contradictions between that and what they were advocating as peer interventionists reinforced their own risk reduction.
DISCUSSION
Peer-delivered interventions are increasingly advocated as a cost-effective way to reach active drug users to reduce their risk for acquiring HIV (Broadhead et al., 1995). Outcomes of these interventions are often measured in terms of the reach of such peer-delivered interventions (i.e., how many drug users received HIV education and materials) and behavior change among the peer interventionists and their contacts (Latkin, Sherman et al., 2003; Latkin et al., 2009). The theory behind evaluations of peer-delivered interventions, however, often focuses on the social influence of peer interventionists on their contacts, and not on the effect of performing peer intervention (Coyle et al., 1998).
Results from this study suggest a model for understanding the social psychological processes underlying the greater decreases in HIV risk among peer interventionists found in many research studies (Kelly et al., 1997; Latkin et al., 2003, Sikkema et al., 1996). These processes include prosocial identity change, positive social reinforcement, and cognitive dissonance in addition to increased and sustained risk reduction efficacy. Participants in the RAP project reported that the PHA role was important and meaningful to them. They identified with other PHAs and felt that they were “doing an important job” in their community. They indicated that social reinforcement, including expressions of gratitude from peers and other community members, risk reduction among their peers, support from PHAs and project staff, and others’ recognition of their own behavior changes were important in motivating them to continue their PHA role. They also described feelings of cognitive dissonance between performing their PHA work and engaging in risky practices that helped them to recognize and reduce their own HIV risk behaviors.
Our qualitative data suggest that these social psychological processes have mutually reinforcing effects. The more the PHAs fulfilled their roles by modeling and advocating risk reduction, the more likely they were to receive positive social reinforcement, which in turn helped motivate them to continue work as PHAs. Advocating risk reduction among peers and receiving public recognition for these efforts in many cases produced cognitive dissonance among PHAs, motivating further reductions in their own risk behaviors. Changes in their risk behaviors, in turn, may have increased positive social reinforcement as peers recognized the PHAs’ change, and further motivated PHAs to continue in their role. Receiving the support of PHAs and project staff in monthly CAG meetings helped them feel that they were part of an important movement to reduce HIV risk among their peers and in their community reinforcing prosocial identity change.
The social psychological mechanisms illustrated in our model may help further explain the processes by which risk reduction self-efficacy increases and changes in peer norms supporting risk reduction behaviors occur. Risk reduction efficacy can occur directly through skills learned in peer interventionists’ training sessions and increase with practice as they demonstrate and model risk reduction behavior to others. Our study indicates that social reinforcement may also contribute to increases in risk reduction efficacy. Observing others like themselves reduce their risks gave PHAs hope that they could reduce their own HIV risk behaviors. Social reinforcement may also contribute to establishing social norms supporting risk reduction. It is important to understand the social context in which social norm change occurs. It is likely not sufficient to train active drug users to advocate and model risk reduction behaviors. These efforts must be recognized and appreciated by a significant number of group members, who then also model and advocate new behaviors. Without such social reinforcement, peer interventionists may become frustrated and quit advocating risk reduction behaviors. In turn, PHAs’ peers will be less likely to adopt and advocate the new behaviors and social norms will remain unchanged.
Our results suggest that having less stringent criteria for selecting PHAs and recruiting persons regardless of their perceived influence and popularity may, in the case of drug users, have beneficial effects both for PHAs and their peers. In fact, seeing positive change (i.e., doing positive things for the community and reducing their own risk behaviors) in people who were not necessarily the most popular may be more salient than intervention messages from someone who is already admired. In other words, if PHAs can change, then this may give hope to other drug users that they can control their drug use, reduce their risk, and do positive things in the community.
The social support provided by project staff was also extremely important in PHAs’ engagement and continued motivation as peer interventionists. Project facilitators were former drug users and ethnically similar to participants. They offered advice from their years of experience in HIV prevention outreach, words of encouragement and for many, a model of what they could become—drug free and engaged in meaningful work to help others who were still using drugs.
Implications for Practice
The model presented in this article is an initial attempt to understand the social psychological processes underlying the greater risk reduction among peer interventionists than those receiving small group or individual interventions. As such, the model has implications for refining peer-delivered interventions and evaluating their success. More research is needed to develop and validate measures to capture the social and psychological processes described above. Peer-delivered interventions are most often evaluated using risk reduction efficacy, behavioral intentions, and motivations as mediators (Kelly et al., 1997). Our model suggests that these individual-level psychological mechanisms are important but not sufficient for understanding behavior change among peer interventionists. One measure often missing in peer-delivered interventions is peer interventionists’ self-efficacy to advocate and model risk reduction among their peers. The Risk Avoidance Partnership used a 13-item measure on a 4-point Likert scale to assess these attitudes (Weeks, Li et al., 2009). Other measures need development or further refinement. Qualitative results suggest that cognitive dissonance and social reinforcement may have several dimensions. For example, expressions of appreciation could be measured by a Likert scale assessing the degree to which PHAs agree with statements like “Most people I approach on the street are grateful to receive condoms and advice from me”; recognition of peers’ behavior change could include statements like “Some people have changed their behavior based on things I’ve said to them”; peers’ recognition of PHA change could include statements such as “Other people have said they noticed that I’m a lot safer when I do drugs”; and social support can be assessed with statements like, “Other PHAs encourage me to continue to work to prevent HIV.” Creating survey items to measure cognitive dissonance is more complicated as it requires capturing participants’ recognition of their own risk behaviors, and the discomfort caused by the contradiction between their public endorsement of risk reduction and continued risk behaviors. As mentioned, attitude change caused by cognitive dissonance is often not in participants’ awareness. However, qualitative data suggest that participants’ do recognize inconsistency between advocating protective behaviors and their own past or current risk behaviors as a source of their discomfort and a motivator to change. Cognitive dissonance could be measured with items such as “I felt like a hypocrite telling people to reduce their risk when I was acting in ways that put me at risk for HIV,” “Being a PHA helped me practice what I preach,” or “I feel uncomfortable seeing people engage in risk behaviors that I used to engage in.” Measurement of cognitive dissonance is perhaps best captured after conducting the first peer intervention outreach activities, as it is likely to decrease as PHAs change their behavior to be more consistent with the risk reduction they publicly endorse. Social identity could be measured by evaluating the extent to which participants identify with other PHAs and find the PHA role meaningful and rewarding. Evaluations of peer-delivered interventions could test the direct and indirect effects of these factors on peer interventionists’ behavioral change, in addition to their intentions, motivations and behavioral skills that have been found to predict behavioral change in more individually focused HIV prevention interventions.
Recognizing the importance of the social psychological mechanisms proposed in our model may also help refine the development and content of peer-delivered interventions. Understanding the social and psychological processes that lead to behavior change among peer interventionists and those who mimic their health advocacy efforts is essential to identifying the “core components” of these evidence-based interventions, i.e., those parts of the intervention that must be retained for the intervention to work as originally designed and tested. Issues of the proper balance between fidelity and adaptation have gained importance as researchers attempt to disseminate evidence-based interventions into service provider settings (Bausell & Sussman, 2006; Sussman, Valente, Rohrbach, Skara, & Pentz, 2006). Many have argued that fidelity to core components is essential to program success and that adaptation is acceptable as long as those core components are not affected. However, inclusion and assessment of key social psychological processes are often not built systematically into many intervention designs and evaluations, as researchers focus on behavioral outcomes more than the processes of behavior change (Backer, 2002; Elliott & Mihalic 2004; Schinke, Brounstein, & Gardner, 2002).
If, as suggested by our qualitative results, having an opportunity to practice peer-delivered interventions with staff reduces initial fear of negative reactions and increases peer-interventionists’ sense of efficacy that they can fulfill this new role, having some sort of support during peer interventionists’ first outreach attempts is essential. Many efforts to translate peer-delivered interventions have eliminated this step because of time and staffing constraints (C. Latkin, personal communication, June 2004). However, personnel costs could be reduced and the social reinforcement role of other peer interventionists enhanced by having new peer interventionists partner with older ones. This may also sustain and strengthen the prosocial identity created by the PHA role, particularly if the older PHAs’ role in training new PHAs is recognized and rewarded. Similarly, if positive social reinforcement by peers, other community members and project staff is essential to producing sustained behavior change among peer interventionists, regular peer intervention delivery, and ongoing booster sessions (like our monthly CAG meetings) to address difficulties in engaging in peer-delivered interventions and to encourage peer interventionists may also be a core component of such interventions. Finally, if inconsistencies between public advocacy of risk reduction practices and peer interventionists’ own risk behaviors creates cognitive dissonance that may motivate them to reduce their own risk, peer intervention to peers and in community settings may be a core component of peer-delivered interventions and should be encouraged in as many ways as possible.
Further research is needed to quantitatively test the direct and indirect influences of the social psychological mechanisms suggested by qualitative data and incorporated into our theoretical model. Such research may help further identify the direct, indirect, and synergistic effects of the social psychological mechanisms. This knowledge, in turn, can help further refine peer-delivered interventions and translate effective peer-delivered interventions to new cultural contexts and subpopulations. Finally, discovery of synergistic effects of the social psychological mechanisms suggested by our model may help sustain risk reduction, a problem that continues to plague most HIV prevention interventions. In particular, finding ways to sustain risk reduction advocacy and social reinforcement may be key to continued risk reduction in individuals and communities.
Acknowledgments
This study was funded by the National Institute on Drug Abuse, grant #R01 DA13356. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. All procedures and measures used in this study were fully reviewed and approved by the Institutional Review Board of the Institute for Community Research.
Contributor Information
Julia Dickson-Gomez, Medical College of Wisconsin, Milwaukee, WI.
Margaret R. Weeks, Institute for Community Research, Hartford, CT
Mark Convey, Institute for Community Research, Hartford, CT.
Jianghong Li, Institute for Community Research, Hartford, CT.
References
- Amirkhanian YA, Kelly JA, Kabakchieva E, McAuliffe TL, Vassileva S. Evaluation of a social network HIV prevention intervention program for young men who have sex with men in Russia and Bulgaria. AIDS Education and Prevention. 2003;15:205–220. doi: 10.1521/aeap.15.4.205.23832. [DOI] [PubMed] [Google Scholar]
- Aronson E, Fried C, Stone J. Overcoming denial and increasing the intention to use condoms through the induction of hypocrisy. American Journal of Public Health. 1991;81:1626–1638. doi: 10.2105/ajph.81.12.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backer TE. Finding the balance: Program fidelity and adaptation in substance abuse prevention. a state-of-the-art review. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Prevention; 2002. [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente R, Peterson J, editors. Preventing AIDS: Theories and methods of behavioral interventions. New York: Plenum Press; 1994. [Google Scholar]
- Bausell RB, Sussman S. Translation issues in HIV, mental health, childhood obesity, and tobacco and drug abuse prevention. Evaluation & the Health Professions. 2006;29:159–161. doi: 10.1177/0163278706287347. [DOI] [PubMed] [Google Scholar]
- Bem D, McConnell HK. Testing the self-perception explanation of dissonance phenomena. Journal of Personality and Social Psychology. 1970;14:23–31. doi: 10.1037/h0020916. [DOI] [PubMed] [Google Scholar]
- Broadhead R, Heckathorn DD, Grund JPC, Stern LS, Anthony DL. Drug users versus outreach workers in combating AIDS: Preliminary results of a peer-driven intervention. Journal of Drug Issues. 1995;25:531–564. [Google Scholar]
- Brown ER. Community action for health promotion: A strategy to empower individuals and communities. International Journal of Health Services. 1991;21:441–456. doi: 10.2190/AKCP-L5A4-MXXQ-DW9K. [DOI] [PubMed] [Google Scholar]
- Coyle SL, Needle RH, Normand J. Outreach-based HIV prevention for injecting drug users: A review of published outcome data. Public Health Reports. 1998;113(Suppl 1):19–30. [PMC free article] [PubMed] [Google Scholar]
- Davey-Rothwell MA, Latkin C. HIV-related communication and perceived norms: an analysis of the connection among injection drug users. AIDS Education and Prevention. 2007;19:298–309. doi: 10.1521/aeap.2007.19.4.298. [DOI] [PubMed] [Google Scholar]
- Dickson-Gomez J, Weeks M, Martinez M, Convey M. Times and places: Process evaluation of a peer-led HIV prevention intervention. Substance Use & Misuse. 2006;41:669–690. doi: 10.1080/10826080500411403. [DOI] [PubMed] [Google Scholar]
- Elford J, Bolding G, Sherr L. Peer education has no significant impact on HIV risk behaviours among gay men in London. AIDS. 2001;15:535–537. doi: 10.1097/00002030-200103090-00018. [DOI] [PubMed] [Google Scholar]
- Elford J, Hart G, Sherr L, Williamson L, Bolding G. Peer led HIV prevention among homosexual men in Britain. Sexually Transmitted Infections. 2002;78:158–159. doi: 10.1136/sti.78.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Mihalic S. Issues in disseminating and replicating effective prevention programs. Prevention Science. 2004;5(1):47–53. doi: 10.1023/b:prev.0000013981.28071.52. [DOI] [PubMed] [Google Scholar]
- Emerson RM, Fretz RI, Shaw LL. Writing ethnographic fieldnotes. Chicago: University of Chicago Press; 1995. [Google Scholar]
- Festinger L. A theory of cognitive dissonance. Stanford, CA: Stanford University Press; 1957. [Google Scholar]
- Flowers P, Hart GJ, Williamson LM, Frankis JS, Der GJ. Does bar-based, peerled health promotion have a community-level effect amongst gay men in Scotland? International Journal of STD & AIDS. 2002;13:102–108. doi: 10.1258/0956462021924721. [DOI] [PubMed] [Google Scholar]
- French R, Power R, Mitchell S. An evaluation of peer-led STD/HIV prevention work in a public sex environment. AIDS Care. 2000;12:225–234. doi: 10.1080/09540120050001913. [DOI] [PubMed] [Google Scholar]
- Friedman S, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy: “Intravention” by injection drug users as a community prevention goal. AIDS Education and Prevention. 2004;16:250–263. doi: 10.1521/aeap.16.3.250.35439. [DOI] [PubMed] [Google Scholar]
- Kelley MS, Murphy S, Lune H. A cultural impact of needle exchange: The role of safer-injection mentors. Contemporary Drug Problems. 2001;28:485–508. [Google Scholar]
- Kelly JA. Popular opinion leaders and HIV prevention peer education: Resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16:139–150. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- Kelly JA, McAuliffe TL, Sikkema KJ, Murphy DA, Somlai AM, Mulry G, et al. Reduction in risk behavior among adults with severe mental illnes who learned to advocate for HIV prevention. Psychiatric Services. 1997;48:1283–1288. doi: 10.1176/ps.48.10.1283. [DOI] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. American Journal of Public Health. 1992;82:1483–1489. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C. Outreach in natural settings: The use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Reports. 1998;113:151–159. [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Social Science and Medicine. 2009;68:740–748. doi: 10.1016/j.socscimed.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Hua W, Tobin K. Social network correlates of self-reported non-fatal overdose. Drug and Alcohol Dependence. 2003;73:61–67. doi: 10.1016/j.drugalcdep.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Latkin C, Knowlton A. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17(Suppl 1):S102–S113. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]
- Latkin C, Sherman S, Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology. 2003;22:332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- Muhr T. Atlas.ti: The knowledge workbench, visual qualitative data analysis, management and theory building. Berlin: Scientific Software Development; 1997–2004. [Google Scholar]
- Neaigus A. The network approach and interventions to prevent HIV among injection drug users. Public Health Reports. 1998;113:140–150. [PMC free article] [PubMed] [Google Scholar]
- Prochaska J, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: A review. Health Education Quarterly. 1994;21:471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Metsch LR, Latka M, Santibanez S, Gómez CA, Eldred L, et al. Interventions for seropositive injectors—research and evaluation. Journal of Acquired Immune Deficiency Syndromes. 2004;37(Suppl 2):S110–S118. doi: 10.1097/01.qai.0000140609.44016.c4. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J. The protective effects of community involvement for HIV risk behavior: A conceptual framework. Health Education Research. 2002;17:389–403. doi: 10.1093/her/17.4.389. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 4. New York: The Free Press; 1995. [Google Scholar]
- Ross MW, Harzke AJ, Scott DP, McCann K, Kelley M. Outcomes of Project Wall Talk: An HIV/AIDS peer education program implemented within the Texas State Prison System. AIDS Education and Prevention. 2006;18:504–517. doi: 10.1521/aeap.2006.18.6.504. [DOI] [PubMed] [Google Scholar]
- Schinke S, Brounstein P, Gardner P. Science-based prevention programs and principles. Rockville, MD: Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services Administration; 2002. [Google Scholar]
- Sikkema K, Heckman TG, Kelly JA, Anderson ES, Winett RA, Solomon LJ, et al. HIV risk behaviors among women living in low-income, inner-city housing developments. American Journal of Public Health. 1996;86:1123–1128. doi: 10.2105/ajph.86.8_pt_1.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Kelly JA, Winett RA, Solmon LJ, Cargill VA, Roffman RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. American Journal of Public Health. 2000;90:57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons P, Rietmeijer CA, Kane MS, Guenther-Grey C, Higgins DL, Cohn DL. Building a peer network for a community level HIV prevention program among injecting drug users in Denver. Public Health Reports. 1996;111(Suppl 1):50–53. [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Valente TW, Rohrbach LA, Skara S, Pentz MA. Translation in the health professions—Converting science into action. Evaluation & the Health Professions. 2006;29:7–32. doi: 10.1177/0163278705284441. [DOI] [PubMed] [Google Scholar]
- Tajfel H. Human groups and social categories. London: Cambridge University Press; 1981. [Google Scholar]
- Trautmann F. Peer support as a method of risk reduction in injecting drug user communities: Experiences in Dutch projects and the “European Peer Support Project. Journal of Drug Issues. 1995;25:617–628. [Google Scholar]
- Trotter R, Bowen AM, Potter JM. Network models for HIV outreach and prevention programs. NIDA Research Monograph. 1995;151:144–180. [PubMed] [Google Scholar]
- Turner JC. Social comparison and social identity: Some perspectives for intergroup behavior. European Journal of Social Psychology. 1978;5:5–34. [Google Scholar]
- Van Khoat D, West GR, Valdiserri RO, Phan NT. Peer education for HIV prevention in the socialist republic of Vietnam: A national assessment. Journal of Community Health. 2003;28:1–17. doi: 10.1023/a:1021321704417. [DOI] [PubMed] [Google Scholar]
- Weeks M, Convey M, Dickson-Gomez J, Li J, Radda K, Martinez M, et al. Changing drug users’ risk environments: Peer health advocates as multi-level community change agents. American Journal of Community Psychology. 2009;43:330–344. doi: 10.1007/s10464-009-9234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks M, Dickson-Gomez J, Mosack KE, Convey M, Martinez M, Clair S. The Risk Avoidance Partnership: Training active drug users as peer health advocates. Journal of Drug Issues. 2006;36:541–570. doi: 10.1177/002204260603600303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks M, Li J, Dickson-Gomez J, Convey M, Martinez M, Radda K, et al. Outcomes of a peer HIV prevention program with injection drug and crack users: The risk avoidance partnership. Substance Use and Misuse. 2009;44:139–162. doi: 10.1080/10826080802347677. [DOI] [PMC free article] [PubMed] [Google Scholar]


