Abstract
Botulinum toxin injections ameliorate dystonic symptoms by blocking the neuromuscular junction and weakening dystonic contractions. We asked if botulinum toxin injections in dystonia patients might also affect the integrity of sensorimotor cortical plasticity, one of the key pathophysiological features of dystonia. We applied a paired associative stimulation protocol, known to induce long-term potentiation–like changes in the primary motor cortex hand area to 12 patients with cervical dystonia before and 1 and 3 months after botulinum toxin injections to the neck muscles. Primary motor cortex excitability was probed by measuring transcranial magnetic stimulation-evoked motor evoked potentials before and after paired associative stimulation. We also measured the input–output curve, short-interval intracortical inhibition, intracortical facilitation, short afferent inhibition, and long afferent inhibition in hand muscles and the clinical severity of dystonia. Before botulinum toxin injections, paired associative stimulation significantly facilitated motor evoked potentials in hand muscles. One month after injections, this effect was abolished, with partial recovery after 3 months. There were significant positive correlations between the facilitation produced by paired associative stimulation and (1) the time elapsed since botulinum toxin injections and (2) the clinical dystonia score. One effect of botulinum toxin injection treatment is to modulate afferent input from the neck. We propose that subsequent reorganization of the motor cortex representation of hand muscles may explain the effect of botulinum toxin on motor cortical plasticity.
Keywords: botulinum toxin, primary dystonia, cervical dystonia, cortical plasticity, paired associative stimulation, transcranial magnetic stimulation, TMS
Primary dystonia is a movement disorder characterized by sustained muscle contractions that cause abnormal postures of affected body parts.1 Lack of inhibition at multiple central nervous system levels2-4 and abnormal senorimotor cortical plasticity both contribute to the pathophysiology of dystonia.5,6 In dystonia, enhanced cortical plasticity extends beyond the clinically affected region and may be detected in unaffected upper limbs of patients with cervical dystonia.7 Botulinum toxin (BT) inhibits acetylcholine release from α-motoneurons and is used as an effective treatment for different forms of dystonia. Although clinical improvement roughly parallels weakness caused by injections, it is commonly observed that clinical benefit seems out of the proportion to the weakness, suggesting an additional, possibly central effect of BT.8,9 The effects of BT in dystonia have been addressed in several studies.8-13 For example, the tonic vibration reflex in patients with writer’s cramp is suppressed to a greater extent than maximal voluntary contraction (MVC) and maximum M wave amplitude (M-max) after BT injections, and this effect persists even when MVC and M-max return to baseline, but while patients are still experiencing some benefit from injections.9 BT treatment normalizes reduced spinal reciprocal inhibition8 and reduced intracortical inhibition.10 Abnormal cortical hand representations revert to normal in patients with focal limb or cervical dystonia after BT injections.11,12 BT has also been shown to reduce abnormally enhanced plasticity of the trigeminal blink reflex in patients with blepharospasm.13 These effects have been explained in part by a change in Ia afferent input from muscle spindles caused by BT.14,15
In the present study, we hypothesized that BT injections might affect abnormally enhanced sensorimotor cortical plasticity, a key feature of primary dystonia.5,6 We studied the response to the paired associative stimulation (PAS) protocol in patients with cervical dystonia (CD), with or without arm involvement, before and 1 and 3 months after BT injections into the neck muscles.
Patients and Methods
Subjects
We studied 12 patients (8 women; mean age, 53 years; range, 30–72 years) with clinically definite primary CD. Six patients had pure focal CD, and 6 patients had CD with mild arm involvement (4 writing dystonia and 2 dystonic arm tremor) that did not require treatment. For clinical assessment of dystonia, we used the Burke-Fahn-Marsden (BFM) scale rather than a specific CD scale in order to capture the additional arm involvement in CD and any possible change with BT injections to the neck muscles. All but 1 patient were chronically treated with BT type A (Dysport, Ipsen, Slough, UK). BT was injected solely into cervical muscles, and none of the patients had ever had injections into arm muscles. At the time of the study, no patient was receiving medication that could affect the measures performed. Patients’ clinical and demographic data are given in Table 1. Written informed consent was obtained from patients, and the study was approved by the local ethics committee and conducted in accordance with the Declaration of Helsinki.
TABLE 1. Clinical features of patients with primary dystonia.
| Patient | Age (y) | Disease duration (y) | BT treatment duration (y) | Time between previous injections and 1st session (weeks) | BT total dose (IU) | BFM score before BT | BFM score 1 month after BT | BFM score 3 months after BT | Pattern of cervical dystonia | Muscles injected |
|---|---|---|---|---|---|---|---|---|---|---|
| 1a | 56 | 7 | 3 | 13 | 480 | 4 | 4 | 6 | tort, to R, L shoulder elevation | spl, trp |
| 2 | 72 | 13 | 10 | 12 | 500 | 8 | 1 | 0.5 | tort, to R | spl, scm, Is |
| 3 | 52 | 5 | 3 | 18 | 425 | 4 | 2 | 4 | tort, to R, tilt to L | spl, scm, Is |
| 4a | 42 | 28 | 8 | 16 | 500 | 4 | 2 | 2 | tort, to R, L shoulder elevation | spl, scm, tr |
| 5 | 30 | 3 | 1 | 16 | 325 | 4 | 2 | 4 | tort, to L | spl, scm |
| 6a | 65 | 30 | 21 | 18 | 850 | 4 | 0 | 2 | tremulous tort, to R | spl, scm |
| 7 | 37 | 8 | 6 | 15 | 425 | 4 | 2 | 2 | tort, to L, L shoulder elevation | spl, scm, tr, Is |
| 8a | 61 | 26 | 0 | / | 440 | 2 | 2 | 2 | tort, to L, tilt to L | spl |
| 9 | 55 | 21 | 20 | 37 | 500 | 6 | 4 | 4 | tort, to R, L shoulder elevation | spl, scm, Is |
| 10a | 51 | 14 | 2 | 21 | 350 | 2 | 2 | 4 | tort, to L | spl, scm |
| 11 | 61 | 13 | 9 | 23 | 450 | 4 | 2 | 4 | tort, to L | spl |
| 12a | 58 | 3 | 2 | 16 | 600 | 6 | 4 | 6 | tort, to R, L shoulder elevation | spl, scm, Is, tr |
| Mean (range) | 53 (30–72) | 14 (3–30) | 7 (0–21) | 19 (12–37) | 487 (325–850) | 4.3 | 2.2 | 3.4 |
IU, international units; BFM, Burke-Fahn-Marsden; tort., torticollis; R, right; L, left; spl, splenius; scm, sternocleidomastoid; Is, levator scapulae; tr, trapezius.
Patients affected by cervical dystonia with arm involvement–patients 1 and 6, dystonic tremor; patients 4, 8, 10, 12, writing dystonia.
Electromyographic Recordings
Electromyographic (EMG) recordings were made from the abductor pollicis brevis (APB) and first dorsal interossei (FDI) muscles of the right side with Ag-AgCl surface electrodes using a belly-tendon montage. EMG signals were amplified (1000×) and band-pass filtered (bandwidth from 20 Hz to 2 kHz) with a Digitimer D360 amplifier (Digitimer, Hertfordshire, UK), acquired at a sampling rate of 5 kHz through a 1401 laboratory interface (Cambridge Electronic Design, Cambridge, UK). The EMG traces were analyzed using customized Signal version 4.00. The level of background EMG activity was carefully monitored, and trials with background EMG activity were rejected.
Transcranial Magnetic Stimulation
Single- and paired-pulse transcranial magnetic stimulation (TMS) of the left primary motor cortex was applied through Magstim 2002 magnetic stimulators with a monophasic current waveform (Magstim Company, Carmarthenshire, Wales, UK). Repetitive TMS of the left primary motor cortex (M1) was delivered through a Rapid-Stim stimulator (Magstim Company, Dwyfed, UK). The magnetic stimulators were connected to a figure-of-eight coil with a mean loop diameter of 7 cm. The coil was held tangentially to the skull with the handle pointing backward and laterally at an angle of about 45 degrees to the sagittal plane. The “hot spot” was marked on the participant’s head over the optimal scalp position for eliciting motor evoked potentials (MEPs) of maximal amplitudes in the contralateral APB muscle. Resting and active motor thresholds (RMT and AMT) were calculated using standard methods.16
Short-latency intracortical inhibition (SICI) and intracortical facilitation (ICF) were determined according to the paired-pulse paradigm described by Kujirai et al.17 The intensity of the conditioning stimulus was 80% of active motor threshold, whereas the intensity of the test stimulus was set to evoke MEPs with peak-to-peak amplitudes of approximately 1 mV. SICI and ICF were assessed at an interstimulus interval (ISI) of 2 and 12 ms, respectively.
Short-latency afferent inhibition (SAI) and long-latency afferent inhibition (LAI) were assessed according to the protocol by Tokimura et al,18 at an ISI of 25 and 200 ms, respectively.
After rapid paired associative stimulation (rPAS), for assessments of SICI, ICF, SAI, and LAI, the intensity of the test stimulus was readjusted to evoke MEPs of approximately 1 mV.
Repetitive TMS was delivered according to the rapid PAS (rPAS) protocol.19 The intensity for the median nerve stimulation was 200% of the perceptual threshold. The intensity of TMS was individually adjusted to 90% AMT.
Experimental Design
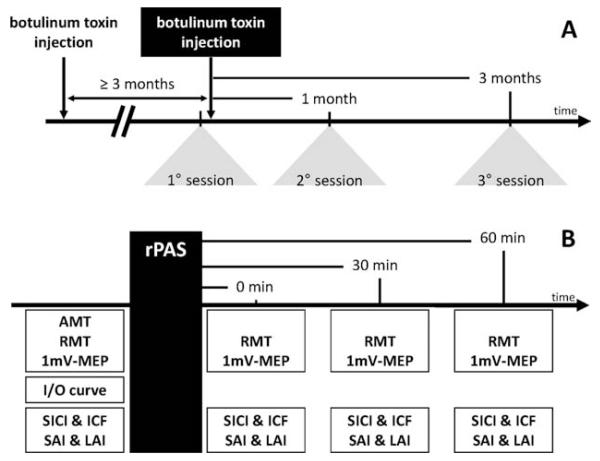
Subjects were studied in 3 sessions: before BT injections and 1 and 3 months after BT injections (Fig. 1A). In all subjects, at least 3 months elapsed between previous injections and the first experimental session (Table 1). In each session TMS parameters were measured at 4 time points: before rPAS, immediately after rPAS (0 minutes), and 30 and 60 minutes after rPAS (Fig. 1B). Before rPAS, in each patient we set the TMS intensity required to evoke MEPs in the APB muscle of approximately 1-mV peak-to-peak amplitude (1-mV MEP threshold). At each time point, 20 MEPs were collected, using TMS intensity of 1-mV MEP threshold. Before rPAS in each session, we also measured the MEP input–output (IO) curve in 7 steps, using the TMS intensity from 70% to 130% of the 1-mV MEP thresholds.
FIG. 1. Experimental design.
A: The experiment was designed to study the response to rapid paired associative stimulation (rPAS) before, 1 month, and 3 months after BT injections. B: In each session we measured: (1) M1 excitability (AMT, RMT, 1-mV MEP, and I/O curve), (2) intracortical excitability (SICI and ICF), and (3) sensorimotor integration (SAI and LAI). All measurements were repeated before rPAS and 0, 30, and 60 minutes after rPAS, except for the AMT and IO curve, which were measured only before rPAS.
Statistical Analysis
To test if the subjects with arm involvement had different responses to rPAS than did the patients with isolated CD, we first used a preliminary 3-way analysis of variance (ANOVA)—arm involvement × BT injections × rPAS. Similarly, to look if the response to rPAS depended on the main direction of head rotation, we used 3-way ANOVA (head rotation [left or right] × BT injections × rPAS). Then we used repeated-measures ANOVA to determine the interaction between BT injections and our measures of interest: baseline measures of cortical excitability (including IO curves), response to rPAS, SICI, ICF, SAI, and LAI. Where significant effects or interactions were found, post hoc tests with Bonferroni corrections were used. The clinical effect of BT injections was assessed by nonparametric Friedman’s ANOVA. We also correlated the rPAS response at 30 minutes (as a percentage of the pre rPAS MEP amplitude) in the first session with patients’ demographic characteristics, using Spearman’s correlation analysis. In addition, a correlation analysis was performed between normalized rPAS response at 30 minutes (as the response peaked at 30 minutes) in the first, second, and third sessions and the time elapsed since the previous BT injections (in weeks) and BFM score. Because in this analysis within-subjects repeated measures are combined, the correlation coefficient was calculated according to the Bland and Altman correction.20 In all tests, the level of statistical significance was P < .05. Data were expressed as means ± 1 standard error of the mean (SEM).
Results
Clinical Effect of BT Injections
As expected, there was clinical improvement in dystonia after BT injections (Friedman’s χ2(2) = 10.8, P < .01). Post hoc analysis showed that the BFM score was significantly lower (indicating less severe dystonia) 1 month after injections than before and 3 months after BT injections (P < .01), whereas no significant difference was found in BFM score before and 3 months after BT injections.
BT Injections into Neck Muscles Do Not Modify Baseline Cortical-Spinal Excitability
BT did not change the RMT or AMT of the APB muscle. A 2-way ANOVA comparing the MEP IO curve before rPAS in each of the 3 sessions showed a significant effect of stimulus intensity (F2,4 = 41.15, P < .01), but no effect of BT injections and no stimulus intensity × BT injections interaction. Further analysis of the IO curve in the range of intensities from 90% to 110% of 1-mV MEP, which corresponds to the range of MEP amplitudes before and after rPAS in all 3 sessions, confirmed that there was a main effect of stimulus intensity, but no effect of BT injections or interaction.
BT Injections Reduce rPAS Response in APB and FDI Muscles
Patients with additional arm involvement (6 of 12) did not differ from patients with isolated CD (6 of 12) in response to rPAS in any of the 3 sessions. With regard to the main direction of head rotation, no significant 2-way—head rotation × rPAS—or 3-way—head rotation × rPAS × BT injections—interactions were found. Therefore, all subsequent analyses were done on the group of patients as a whole.
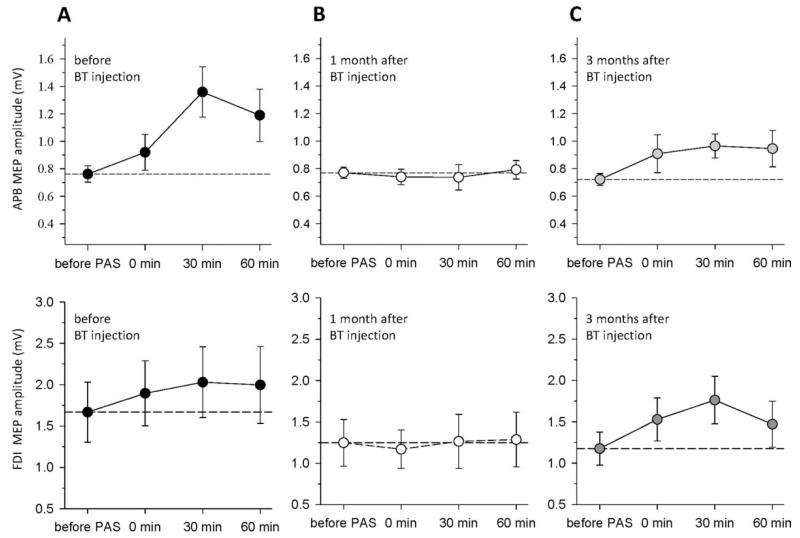
For APB muscle, a 2-way ANOVA revealed a significant effect of BT injections (3 levels: before BT and 1 and 3 months after BT; F2,22 = 6.46, P < .01) and rPAS (4 levels: before rPAS and 0, 30, and 60 minutes after rPAS; F3,33 = 3.66, P < .05), as well as a significant interaction (F6,66 = 3.06, P < .01); see Figure 2. Post hoc analysis for the factor BT injections showed that the mean MEP amplitude was lower 1 month after BT injections compared with the values before BT injections and 3 months after injections (P < .01). Post hoc analysis for the factor rPAS showed that the mean MEP amplitude was significantly higher 30 minutes after rPAS, compared with at the other time points (P < .05). The BT injections × rPAS interaction was further explored by examining the main effect of rPAS separately within each experimental session. This showed a significant effect of rPAS before BT injections (F3,33 = 4.86, P < .01) but not after 1 month (F3,33 = 0.18, P < .05) or after 3 months (F3,33 = 1.85, P < .05). There was a nonsignificant trend for rPAS response to be greater at 3 months post-BT compared with 1 month post-BT.
FIG. 2. Botulinum toxin injections in dystonic neck muscles abolished rPAS-induced plasticity of the primary motor cortex hand area.
Before botulinum toxin (BT) injections (A), rPAS induced powerful plastic changes of hand cortical-spinal excitability: MEPs in abductor pollicis brevis (APB) and first dorsal interossei (FDI) muscles increased in amplitude immediately after rPAS (0 minutes), reaching a peak after 30 minutes. One month after BT injections (B), rPAS response was completely abolished and partially recovered 3 months after (C).
In the FDI muscle ANOVA revealed a significant effect of BT injections (F2,22 = 7.60, P < .01), whereas rPAS or the interaction BT injections × rPAS was nonsignificant. Similarly to the APB muscle, the mean FDI MEP amplitude after rPAS was lower 1 month after BT (P < .01) compared with the values before BT, but not different from the value at 3 months.
To compare whether the APB and the FDI behaved similarly in response to rPAS and BT,5,7 for each individual we expressed the average facilitation 0, 30, and 60 minutes after rPAS as a percentage of the corresponding baseline values. A 2-way ANOVA with the main factors muscle (APB and FDI) and BT injections revealed a significant effect of BT injections (F2,22 = 4.04; P < .05) but not of muscle or the interaction muscle × BT injections. We concluded that rPAS response in relation to BT injections was similar in APB and FDI muscles.
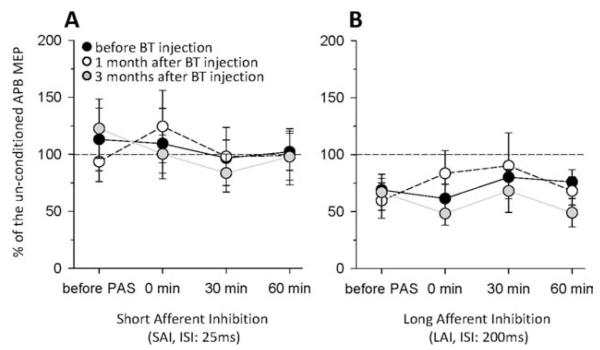
rPAS and BT Do Not Modify Intracortical Excitability and Cortical Sensorimotor Integration
There was no effect of rPAS or BT injections on SICI and ICF or on SAI and LAI (Fig. 3).
FIG. 3. SAI and LAI in response to rPAS and BT injections.
Patients with CD showed no short afferent inhibition (SAI) at an ISI of 25 ms (A), whereas long afferent inhibition (LAI) was present (B). Transmission in both SAI and LAI circuits was not modulated by BT injections or by rPAS.
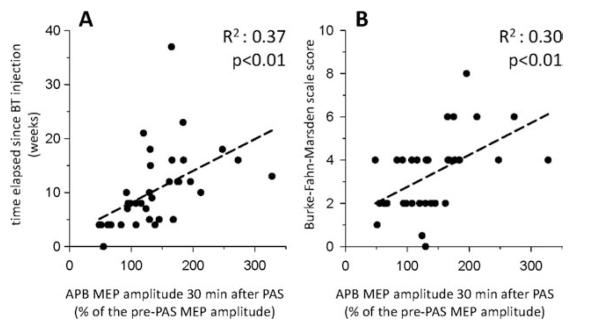
rPAS Induced Plasticity Correlates with Dystonia Severity and the Time after Previous BT Treatment
There was a significant positive correlation between the normalized MEP amplitude 30 minutes after rPAS and (1) the time elapsed after BT injections (R2 = 0.37, P < .01) and (2) the severity of dystonia assessed by BFM score (R2 = 0.30, P < .01); see Figure 4.
FIG. 4. Correlation between rPAS-induced plasticity of the primary motor cortex and clinical symptoms of dystonia.
Peak-to-peak amplitude of the normalized APB MEPs recorded 30 minutes after rPAS positively correlated with the time elapsed since the previous BT injections in weeks (A) and with the Burke-Fahn-Marsden dystonia severity score (B). Each patient with its corresponding values of rPAS response (A) or BFM score (B) is plotted 3 times—before BT injections and 1 and 3 months after BT injections.
There were no significant correlations between patient age, disease duration, duration of BT treatment, or dose of the last BT injections and rPAS response.
Discussion
Here we report that BT transiently abolished the response to an experimental sensorimotor plasticity protocol in CD patients. Before BT injections, rPAS significantly facilitated MEP amplitude in the hand muscles. One month after injections this facilitation was suppressed, whereas after 3 months it partially recovered. The response to rPAS correlated significantly with the time elapsed after previous BT injections and with the clinical severity of dystonia as measured by BFM total score. We saw no improvement in the severity of arm dystonia in those patients with CD and arm involvement after injections into the neck muscles. This suggests that the effect of BT on cortical plasticity alone may not be sufficient to clinically affect dystonia of noninjected muscles, but may contribute to the clinical benefit seen in the injected muscles. However, when using kinematic assessment, there is evidence that BT may improve kinematic abnormalities in arm muscles,21 even when injections are given elsewhere. This provides some support for the hypothesis that central changes in noninjected muscles such as we have revealed may have some functional benefit.
Possible BT Action Mechanism on Cortical Plasticity
BT can affect the release of neurotransmitters important in brain plasticity and is used in animal studies to block the connection between different brain areas in order to study changes in brain plasticity.22-24 Although there is some evidence to support hematogenous and axonal spread of large doses of BT in animals,25,26 similar evidence in humans is lacking. Therefore, a direct central effect of BT on plasticity in our patients seems unlikely, particularly at the doses used for treatment of dystonia.
Another explanation for our results is that the effect of BT on cortical plasticity may be secondary to changes in motor maps that occur after afferent input from cervical muscles is altered by injections.11,12 A considerable body of evidence demonstrates the importance of afferent input in modulating cortical organization and excitability.27-30 In dystonia, changes in “motor maps” of hand muscles have been described after BT injections.11,12 Thickbroom et al11 reported that in patients with CD, motor maps of APB are displaced in the hemisphere contralateral to the direction of head rotation. After BT injections into cervical muscles, APB motor maps reverted to a more normal position, thus showing that changes in motor cortical topography after injections may affect representations of nontreated muscles. This may be relevant for the experimental plasticity protocol we used. PAS relies on the interaction between sensory afferents and motor output of homologous muscle. If motor maps change in location after BT, then there may be a degree of disconnection between sensory afferents and the altered location of the hand motor maps, leading to a reduced PAS response measured in hand muscles. In our study design, we studied the dominant hemisphere in all patients, and a subgroup analysis comparing patients where the dominant hemisphere was contralateral or ipsilateral to the main direction of head turning did not reveal any significant differences between groups. It is possible that our study was not powered to detect such differences. However, most of our patients had complex patterns of cervical dystonia that did not easily segregate into simple left- or right-head turning, and this might explain why no group differences in BT effect on PAS response were found.
Measures of Intracortical Excitability and Their Relation to BT Injections and rPAS
We did not find any interaction between our measures of cortical inhibition and facilitation and rPAS or with BT injections. In particular, there was no effect of BT injections on SICI, which is in contrast to the findings of Gilio et al.10 This disparity may be a result of methodological differences, as in their study Gilio et al used different ISIs, of 3 and 5 ms, and studied patients with more severe arm involvement (mainly generalized dystonia), whereas we studied subjects with CD with or without minor arm involvement. Similar to our results, Boroojerdi et al31 did not report any changes in SICI or ICF after BT injections in patients with writer’s cramp. In patients with idiopathic rotational cervical dystonia who had never been treated with BT, Kanovsky et al32 found significantly decreased inhibition at 3 and 5 ms and significantly increased facilitation at 15 and 20 ms in the hemisphere contralateral to the direction of head deviation when compared with the ipsilateral hemisphere. In our patients, we always studied the dominant hemisphere, and we did not find any differences in the amount of SICI between patients where the dominant hemisphere was contralateral or ipsilateral to the main direction of head rotation. One explanation may be in the more “complex” form of CD in our group, with most patients having bilateral muscle involvement.
Measures of Sensorimotor Cortical Inhibition and Their Relation to BT Injections and rPAS
LAI was present in our group of patients and was not modified after rPAS or in relation to BT injections. However, SAI at an ISI of 25 ms was absent and was not modified after rPAS (Fig. 3). We measured SAI at an ISI of 25 ms based on previous data on healthy young subjects from Quartarone et al,19 who found that at an ISI of 25 ms SAI is present and may be modulated by rPAS. When Kessler et al33 studied SAI in patients with writer’s cramp at ISIs raging from 14 to 36 ms, the strongest inhibition was present at an ISI of 20 ms. Therefore, it is possible that we may have missed some subtle changes at shorter intervals.
Limitations of the Study
We did not record H reflex or F waves to monitor possible changes in motoneuron excitability secondary to BT. However, we did not find any effect of BT on RMT, AMT, and IO curves, that is, in parameters that test the excitability of the entire corticospinal tract including the motoneuron. In line with our observations, Priori et al8 found that 1 month after BT injections to the arm, the Hmax:Mmax ratio was unchanged, suggesting that BT does not affect motoneuron excitability. We found that BT injections reduce cortical plasticity in chronically treated dystonia patients, but we cannot comment if a similar effect would be present in dystonia patients naive to BT. Nevertheless, our single subject who was not previously treated with BT did not behave differently from the whole group. One possible limitation of the study is the lack of comparison with healthy controls. However, a number of previous studies on different forms of dystonia, including CD, have demonstrated that dystonia patients have an abnormally enhanced response to PAS protocols compared with normal subjects.5,7 Our primary interest was to see the change in PAS response with BT injections rather than the absolute level of PAS response at baseline. In the context of this study, we consider that a comparison group of CD patients treated with placebo injections or a healthy participant group given botulinum toxin injections would not have been justified ethically. However, it should be noticed that in view of our study design, we cannot comment if our patients at baseline (before BT injections) differed in response to rPAS, SICI, ICF, SAI, or LAI from normal subjects of a similar age.
Conclusions
BT injections into dystonic neck muscles decreased sensorimotor associative plasticity in the hand area in patients with CD. We propose that this central effect is mediated by changes in motor maps caused by reduced afferent input from neck muscles following injections. Modulation of sensorimotor plasticity may contribute to clinical benefit of BT injections in dystonia over and above the effects of weakness of injected muscles.
Supplementary Material
Footnotes
Relevant conflicts of interest/financial disclosures: Maja Kojovic has received honoraria for conference travel from EFNS, Movement Disorders Society, Guarantors of Brain, Ipsen, and UCB; Grants from EFNS Scientific Fellowship Grant 2009 and a Lady Astor PhD Grant; and is employed by the Department of Neurology, University of Ljubljana, Slovenia. Antonio Caronni is employed by the Department of Human Physiology, University of Milan, Italy. Matteo Bologna has received an ENS Fellowship Grant 2009 and is employed by the “Sapienza” University of Rome, Italy. John C. Rothwell has received honoraria for conference travel and meetings from the Movement Disorders Society, grants from the Dystonia Medical Research Foundation, Tourette Syndrome Association, and the FP7 Collaborative Project (222918 and 223524), and is employed by University College London. Kailash P. Bhatia is a member of the Movement Disorders Society Scientific Advisory Board, has received honoraria from GSK, Boehringer-Ingelheim, Ipsen, Merz, and Orion pharmaceutical companies and grants from the Wellcome Trust and an MRC award (ref. WT089698), and a Halley Stewart Trust grant through the Dystonia Society UK, and is employed by University College London. Mark J. Edwards has received honoraria from Teva Pharmaceuticals and Orio, an NIHR Clinician Scientist Grant, is employed by University College London, and has received royalties from Oxford University Press for Oxford Specialist Handbook of Parkinson’s Disease and Other Movement Disorders.
This work was undertaken at UCLH/UCL, which received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme.
Full financial disclosures and author roles may be found in the online version of this article.
References
- 1.Fahn S. Concept and classification of dystonia. Adv Neurol. 1988;50:1–8. [PubMed] [Google Scholar]
- 2.Berardelli A, Rothwell JC, Day BL, Marsden CD. Pathophysiology of blepharospasm and oromandibular dystonia. Brain. 1985;108:593–608. doi: 10.1093/brain/108.3.593. [DOI] [PubMed] [Google Scholar]
- 3.Nakashima K, Rothwell JC, Day BL, Thompson PD, Shannon K, Marsden CD. Reciprocal inhibition between forearm muscles in patients with writer’s cramp and other occupational cramps, symptomatic hemidystonia and hemiparesis due to stroke. Brain. 1989;112:681–697. doi: 10.1093/brain/112.3.681. [DOI] [PubMed] [Google Scholar]
- 4.Ridding MC, Sheean G, Rothwell JC, Inzelberg R, Kujirai T. Changes in the balance between motor cortical excitation and inhibition in focal, task specific dystonia. J Neurol Neurosurg Psychiatry. 1995;59:493–498. doi: 10.1136/jnnp.59.5.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quartarone A, Bagnato S, Rizzo V, et al. Abnormal associative plasticity of the human motor cortex in writer’s cramp. Brain. 2003;126:2586–2596. doi: 10.1093/brain/awg273. [DOI] [PubMed] [Google Scholar]
- 6.Edwards MJ, Huang YZ, Mir P, Rothwell JC, Bhatia KP. Abnormalities in motor cortical plasticity differentiate manifesting and nonmanifesting DYT1 carriers. Mov Disord. 2006;21:2181–2186. doi: 10.1002/mds.21160. [DOI] [PubMed] [Google Scholar]
- 7.Quartarone A, Morgante F, Sant’angelo A, et al. Abnormal plasticity of sensorimotor circuits extends beyond the affected body part in focal dystonia. J Neurol Neurosurg Psychiatry. 2008;79:985–990. doi: 10.1136/jnnp.2007.121632. [DOI] [PubMed] [Google Scholar]
- 8.Priori A, Berardelli A, Mercuri B, Manfredi M. Physiological effects produced by botulinum toxin treatment of upper limb dystonia. Changes in reciprocal inhibition between forearm muscles. Brain. 1995;118:801–807. doi: 10.1093/brain/118.3.801. [DOI] [PubMed] [Google Scholar]
- 9.Trompetto C, Curra A, Buccolieri A, Suppa A, Abbruzzese G, Berardelli A. Botulinum toxin changes intrafusal feedback in dystonia: a study with the tonic vibration reflex. Mov Disord. 2006;21:777–782. doi: 10.1002/mds.20801. [DOI] [PubMed] [Google Scholar]
- 10.Gilio F, Curra A, Lorenzano C, Modugno N, Manfredi M, Berardelli A. Effects of botulinum toxin type A on intracortical inhibition in patients with dystonia. Ann Neurol. 2000;48:20–26. [PubMed] [Google Scholar]
- 11.Thickbroom GW, Byrnes ML, Stell R, Mastaglia FL. Reversible reorganisation of the motor cortical representation of the hand in cervical dystonia. Mov Disord. 2003;18:395–402. doi: 10.1002/mds.10383. [DOI] [PubMed] [Google Scholar]
- 12.Byrnes ML, Thickbroom GW, Wilson SA, et al. The corticomotor representation of upper limb muscles in writer’s cramp and changes following botulinum toxin injection. Brain. 1998;121:977–988. doi: 10.1093/brain/121.5.977. [DOI] [PubMed] [Google Scholar]
- 13.Quartarone A, Sant’Angelo A, Battaglia F, et al. Enhanced long-term potentiation-like plasticity of the trigeminal blink reflex circuit in blepharospasm. J Neurosci. 2006;26:716–721. doi: 10.1523/JNEUROSCI.3948-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filippi GM, Errico P, Santarelli R, Bagolini B, Manni E. Botulinum A toxin effects on rat jaw muscle spindles. Acta Otolaryngol. 1993;113:400–404. doi: 10.3109/00016489309135834. [DOI] [PubMed] [Google Scholar]
- 15.Rosales RL, Arimura K, Takenaga S, Osame M. Extrafusal and intrafusal muscle effects in experimental botulinum toxin-A injection. Muscle Nerve. 1996;19:488–496. doi: 10.1002/(SICI)1097-4598(199604)19:4<488::AID-MUS9>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 16.Rossini PM, Barker AT, Berardelli A, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol. 1994;91:79–92. doi: 10.1016/0013-4694(94)90029-9. [DOI] [PubMed] [Google Scholar]
- 17.Kujirai T, Caramia MD, Rothwell JC, et al. Corticocortical inhibition in human motor cortex. J Physiol. 1993;471:501–519. doi: 10.1113/jphysiol.1993.sp019912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tokimura H, Di Lazzaro V, Tokimura Y, et al. Short latency inhibition of human hand motor cortex by somatosensory input from the hand. J Physiol. 2000;523:503–513. doi: 10.1111/j.1469-7793.2000.t01-1-00503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quartarone A, Rizzo V, Bagnato S, et al. Rapid-rate paired associative stimulation of the median nerve and motor cortex can produce long-lasting changes in motor cortical excitability in humans. J Physiol. 2006;575:657–670. doi: 10.1113/jphysiol.2006.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Calculating correlation coefficients with repeated observations: Part 1—Correlation within subjects. BMJ. 1995;310:446. doi: 10.1136/bmj.310.6977.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pelosin E, Bove M, Marinelli L, Abbruzzese G, Ghilardi MF. Cervical dystonia affects aimed movements of nondystonic segments. Mov Disord. 2009;24:1955–1961. doi: 10.1002/mds.22693. [DOI] [PubMed] [Google Scholar]
- 22.Ando S, Kobayashi S, Waki H, et al. Animal model of dementia induced by entorhinal synaptic damage and partial restoration of cognitive deficits by BDNF and carnitine. J Neurosci Res. 2002;70:519–527. doi: 10.1002/jnr.10443. [DOI] [PubMed] [Google Scholar]
- 23.Costantin L, Bozzi Y, Richichi C, et al. Antiepileptic effects of botulinum neurotoxin E. J Neurosci. 2005;25:1943–1951. doi: 10.1523/JNEUROSCI.4402-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caleo M, Restani L, Gianfranceschi L, et al. Transient synaptic silencing of developing striate cortex has persistent effects on visual function and plasticity. J Neurosci. 2007;27:4530–4540. doi: 10.1523/JNEUROSCI.0772-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boroff DA, Chen GS. On the question of permeability of the blood-brain barrier to botulinum toxin. Int Arch Allergy Appl Immunol. 1975;48:495–504. doi: 10.1159/000231337. [DOI] [PubMed] [Google Scholar]
- 26.Antonucci F, Rossi C, Gianfranceschi L, Rossetto O, Caleo M. Long-distance retrograde effects of botulinum neurotoxin A. J Neurosci. 2008;28:3689–3696. doi: 10.1523/JNEUROSCI.0375-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brasil-Neto JP, Cohen LG, Pascual-Leone A, Jabir FK, Wall RT, Hallett M. Rapid reversible modulation of human motor outputs after transient deafferentation of the forearm: a study with transcranial magnetic stimulation. Neurology. 1992;42:1302–1306. doi: 10.1212/wnl.42.7.1302. [DOI] [PubMed] [Google Scholar]
- 28.Ridding MC, Rothwell JC. Reorganisation in human motor cortex. Can J Physiol Pharmacol. 1995;73:218–222. doi: 10.1139/y95-032. [DOI] [PubMed] [Google Scholar]
- 29.Ziemann U, Corwell B, Cohen LG. Modulation of plasticity in human motor cortex after forearm ischemic nerve block. J Neurosci. 1998;18:1115, 1123. doi: 10.1523/JNEUROSCI.18-03-01115.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ziemann U, Hallett M, Cohen LG. Mechanisms of deafferentation-induced plasticity in human motor cortex. J Neurosci. 1998;18:7000–7007. doi: 10.1523/JNEUROSCI.18-17-07000.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boroojerdi B, Cohen LG, Hallett M. Effects of botulinum toxin on motor system excitability in patients with writer’s cramp. Neurology. 2003;61:1546–1550. doi: 10.1212/01.wnl.0000095965.36574.0f. [DOI] [PubMed] [Google Scholar]
- 32.Kanovsky P, Bares M, Streitova H, Klajblova H, Daniel P, Rektor I. Abnormalities of cortical excitability and cortical inhibition in cervical dystonia Evidence from somatosensory evoked potentials and paired transcranial magnetic stimulation recordings. J Neurol. 2003;250:42–50. doi: 10.1007/s00415-003-0942-2. [DOI] [PubMed] [Google Scholar]
- 33.Kessler KR, Ruge D, Ilic TV, Ziemann U. Short latency afferent inhibition and facilitation in patients with writer’s cramp. Mov Disord. 2005;20:238–242. doi: 10.1002/mds.20295. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.