Abstract
Purpose of review
A novel form of anaphylaxis has been described that is due to IgE antibody (Ab) directed against a mammalian oligosaccharide epitope, galactose-alpha-1, 3-galactose (alpha-gal). Ongoing work regarding the cause and distribution of this IgE response is reviewed.
Recent findings
Our recent work has identified a novel IgE Ab response that has been associated with two distinct forms of anaphylaxis: immediate-onset anaphylaxis during first exposure to intravenous cetuximab and delayed-onset anaphylaxis 3–6 h after ingestion of mammalian food products (e.g. beef and pork). Further studies strongly suggested that tick bites were a cause, if not the only significant cause, of IgE Ab responses to alpha-gal in the United States and internationally.
Summary
Large numbers of patients with IgE Ab to alpha-gal continue to be identified in the USA and globally. Clinicians should be aware of this IgE response as the reactions often appear to be idiopathic because of the significant delay between eating mammalian meat and the appearance of symptoms.
Keywords: alpha-gal, anaphylaxis, food allergy, IgE, mammalian meat, tick bites
INTRODUCTION
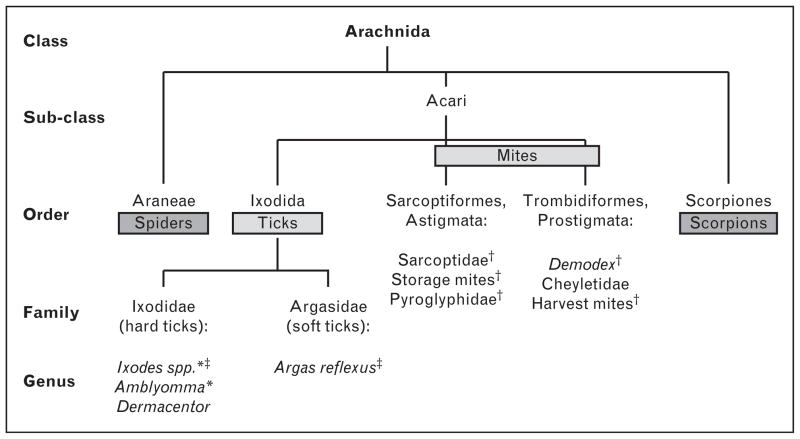
Ticks, or Ixodida, are an order of obligate bloodsucking parasites within the class Arachnida. This class includes many species that can cause immunological sensitization (Fig. 1). The ticks have been recognized as a source of infection for over 100 years, and a long list of viral, bacterial, and rickettsial diseases are primarily spread by ticks. Tick saliva contains many different proteins with antihemostatic, anti-inflammatory, anesthetic, and immunomodulatory properties, which collectively help the tick to prolong the attachment and feed successfully [1]. The host organisms make immune responses to tick saliva, and these responses play a role in reducing the tick attachment and also reducing the infection [2]. The importance of tick saliva is reflected in the rapid evolution of proteins in their saliva [3,4]. However, the evolution of ticks that feed on mammals has occurred primarily, if not exclusively, with nonprimate mammals as the primary host [5]. It could, of course, be argued that the ability to remove ticks and other parasites from our skin is one of the advantages of hands with opposable thumbs. In addition, it is likely that the immune response to ticks feeding on humans reflects the fact that we are an accidental or irrelevant host.
FIGURE 1.
Classification of the Arachnida, a class within the phylum Arthropoda. †Known to cause sensitization unrelated to alpha-gal. *Amblyomma americanum, Ixodes ricinus, and Ixodes holocyclus have been reported to induce IgE to alpha-gal. ‡Ixodes holocyclus and Argas reflexus have been associated with anaphylaxis at the time of a tick bite.
TICKS AND IgE ANTIBODY RESPONSES
Some species of ticks can cause anaphylactic reactions during the bite. There have been multiple reports from Australia and Europe, but surprisingly only one case report from the United States. These reactions have been shown to be related to IgE antibodies to salivary proteins. Interestingly, a report from Denmark demonstrated that a plant used to treat allergic reactions caused by tick bites in northern Afghanistan was indeed an active antihistamine [6▪].
Prior to 2008, three observations had been made that appeared unrelated, but were ultimately related to our story. First, the allergic disease group at the Karolinska Institute in Sweden recognized that some patients who presented with positive skin tests to cat allergens had IgE antibodies specific for an oligosaccharide on cat IgA [7]. Second, two allergists in practice had independently reported to their local societies about patients who developed allergy to meat after being bitten by ticks [8▪]. Third, the monoclonal antibody cetuximab, which is produced in a mouse cell line, SP2/0, was reported to give rise to hypersensitivity reactions in up to 20% of patients treated with this monoclonal in Tennes-see or North Carolina [9]. Working out the specificity of the IgE antibodies giving rise to cetuximab reactions became possible because pretreatment sera were available in Tennessee, Qinwei Zhou and his colleagues at ImClone defined the glycosylation of cetuximab, and ImClone provided the monoclonal antibody expressed in a different cell line (CHO) [10,11]. Using an assay for cetuximab with the mAb bound to an ImmunoCAP, it became possible to prove that reactions were ‘caused by’ preexisting IgE antibodies to the oligosaccharide on the Fab portion of this molecule [10,12▪]. This oligosaccharide, galactose-alpha-1,3-galactose (alpha-gal) is a blood group substance of the nonprimate mammals, and therefore would not be part of the immune response to tick saliva in their normal hosts. The finding of IgE antibodies to alpha-gal in up to 20% of patients (and controls) in Tennessee, Virginia, North Carolina, Arkansas, and southern Missouri led to two questions: why were these antibodies so common in this area, and were they associated with any other diseases?
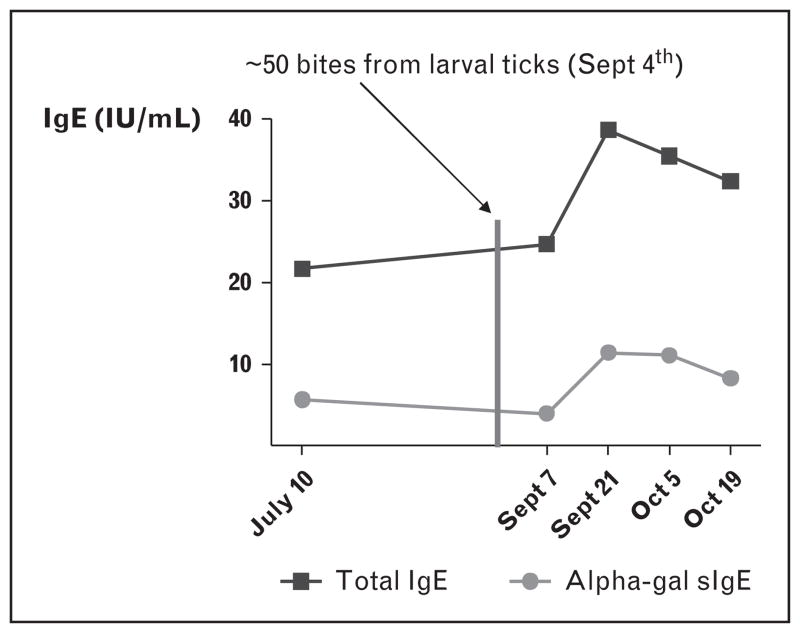
After the alpha-gal epitope had been defined, it was quickly made clear that the previously recognized oligosaccharide epitope on cat IgA was alpha-gal [13]. Although a relationship between mammalian meat allergy and tick bites had been suggested in Australia [8▪], the tick connection was not immediately obvious in the United States or Sweden. After excluding many possible causes, including helminth and fungal infections, the closest match for the distribution of these antibodies was the highest prevalence of Rocky Mountain spotted fever (RMSF). This led to a detailed analysis of histories of tick bites and serological assays using Amblyomma americanum and Dermacentor variabilis extracts [14▪▪]. In addition, it was possible to monitor the rise in IgE antibodies to alpha-gal after tick bites (Fig. 2). Taken together, the results provided strong evidence that tick bites were an important, if not the only, cause of these antibodies in the United States [14▪▪]. More recently, van Hage and her colleagues in Stockholm have reported clear evidence that the alpha-gal epitope is present in the gut of Ixodes ricinus [15▪▪]. Strikingly, the evidence was that the tick bites that gave rise to this response were characterized by persistent itching at the site of the bite [14▪▪]. By contrast, pruritic responses to tick bites in an area endemic for Lyme disease were found to be negatively associated with serological responses to Borrelia burgdorferi [16].
FIGURE 2.
Change in total IgE and alpha-gal-specific IgE over the weeks following approximately 50 bites from larval ticks in a patient.
Only very limited data are available about the cellular response in the skin following bites of different ticks. The fact that the responses to A. americanum are so persistent and so profoundly pruritic suggests that a significant immune response is occurring at the site of the bite [17]. A recent report of multiple pruritic papules caused by Haemaphysalis longicornis in Korea demonstrated abundant eosinophils at the sites of the bites [18]. However, the staining technique they used would probably not identify basophils. On the other hand, a recent study [19] of immune responses to Ixodes scapularis saliva emphasized the role of neutrophils in preventing Borrelia infection.
Studies on the antibody response to A. americanum tick bites have examined both the specificity of the antibodies and the isotypes involved. Using NMR, it has been confirmed that the antibodies are primarily directed at the two terminal galactoses [20]. It is important to remember that all immuno-competent humans (as well as Old World monkeys and apes) have circulating IgG antibodies to alpha-gal [21]. These antibodies are predominantly IgG2 and are thought to be induced by continuous antigenic stimulation by oligosaccharide antigens on bacteria in the gut [21]. Independent measurements in Virginia and Amsterdam do not support the earlier evidence that the IgG antibodies to alpha-gal are equal to 1% of circulating IgG. Our results suggest that these antibodies are around 1 μg/ml (i.e. ≤ 0.1%). Following tick bites, the IgG antibodies increase in parallel with IgE antibodies, but they are predominantly IgG1 [22▪▪]. One interesting question is whether the ‘natural’ IgG2 antibody response influences the immune response to the same epitope induced by tick bites. In addition, the resulting antibody response (IgG2 vs. IgE) likely reflects the route of sensitization (intestinal vs. skin) and predicts the clinical outcome (tolerance vs. allergy), which may establish a model for understanding the mechanisms controlling the immune responses leading to oral tolerance on the one hand or food allergy on the other.
EPIDEMIOLOGY OF THE IgE ANTIBODY RESPONSE TO ALPHA-GAL AND THE ASSOCIATED REACTIONS TO RED MEAT
Using the assay for IgE Ab to alpha-gal, we screened sera from different groups of patients who had presented to the allergy clinic. It rapidly became clear that there was a group of patients who consistently reported urticarial or anaphylactic reactions occurring 3–5 h after eating red meat [23]. In keeping with the known distribution of the oligo-saccharide, these patients also had positive skin tests and serum assays to beef, pork, and lamb, as well as milk, cat, and dog [24].
Over the 4 years since we first described delayed urticarial or anaphylactic reactions to red meat, we have become aware of over 1000 cases in which the history has been confirmed by a serum assay for IgE antibodies to alpha-gal. However, these cases include a mixture of de-identified case reports from other physicians, cases enrolled in our own clinics, and series of cases enrolled by other physicians. We have good evidence that these cases are common in the original southeastern states but also extending into the midwest states where the same ticks are prevalent (e.g. Oklahoma). In addition, we have knowledge of a few cases in surrounding states and also as far north as Nantucket. There also exist ‘hot spots’ in different areas of these states where the landscape is unique or different (e.g. East Hampton portion of Long Island, New York). However, there was initially major bias in certain locales because of enthusiasm and increased awareness of the condition. Thus, it is not yet possible to connect that data into an estimate of overall prevalence, which is a goal of future studies.
LATE-ONSET AND DELAYED REACTIONS TO MAMMALIAN FOOD PRODUCTS OUTSIDE THE USA
We are now aware of the physicians who have identified cases of delayed anaphylaxis in Australia, France, Germany, Sweden, Spain, Japan, and Korea. Notably, in each of these countries, there is evidence that tick bites are the primary cause of the sensitization and that the primary or sole sensitization is to alpha-gal.
Australia
Following Dr Van Nunen’s [8▪] original observations in Sydney, we established collaboration with Dr Mullins who works in Canberra, which is within the same region. We have now assayed more than 50 sera from that region, and there is no doubt that IgE to alpha-gal is present and associated with food reactions to mammals, including kangaroo meat [25▪].
Germany
Dr Jappe has been aware of the reactions to cetux-imab as well as allergic reactions to beef. Her lab at the Borstel Institute near Hamburg has shown IgE binding to cetuximab by western blot and, subsequently, that those results correlated well to immunoassay results for IgE to alpha-gal using biotinylated reagents [26].
France
Dr Moneret-Vautrin and her group in Nancy identified three cases in 2009 and reported on skin testing [27]. More recently, they have extended their work to study other foods including goat, horse, and particularly pork and beef kidneys as a cause of severe delayed reactions in patients with IgE to alpha-gal [28▪▪].
Sweden
Dr Van Hage and her colleagues originally reported that some IgE antibodies binding to cat extracts were specific for an oligosaccharide on cat IgA and went on to show that the oligosaccharide on cat IgA was alpha-gal [13,29]. More recently, they have used antibodies against alpha-gal in human sera to stain the cryostat preparations of the tick which is thought to induce these responses in Stockholm [15▪▪]. The area of Sweden where we have screened sera from school children is almost 800 miles north of Stockholm and less than 1% of those sera tested positive for IgE to alpha-gal [30,31▪]. Interestingly, there are no ticks in that area.
Japan
Dr Sekiya and colleagues in Sagamihara reported the case of a 74-year-old woman with no history of atopy or allergic disorders who reported anaphylaxis 5 h after eating roast beef [32]. The patient reported being bitten by ticks 2 months before the reaction. The authors performed an open challenge with 50 g of roast pork and the patient developed generalized urticaria with swelling and redness of the face 5 h after consuming the pork. An open challenge with 50 g of roast chicken produced no symptoms.
Korea
A group in Seoul led by Dr Kim has reported the case of a 67-year-old man who experienced anaphylaxis 7 h after eating mammalian meat. In addition, the patient reported recurrent episodes of delayed urticaria several hours after consuming pork, beef, or lamb. He denied any reactions to milk, fish, and poultry. The authors performed intradermal testing with cetuximab at concentrations of 5, 50, and 500 μg, which showed positive responses at each concentration, and that the response was larger with increasing concentration.
Africa
In Africa, although IgE to alpha-gal has been identified in both adults and children, those reports do not include evidence of reactions to mammalian meat [31▪,33].
IgE ANTIBODIES TO GALACTOSE ALPHA-1,3-GALACTOSE IN CHILDREN
All reported cases of hypersensitivity reactions to cetuximab have been in adults, in keeping with the use of this monoclonal Ab to treat colon cancer and head and neck cancer [34]. In addition, the original cases of delayed anaphylaxis to red meat were all in adults [23]. We assumed at that time that children were not bitten by ticks as much as adults; however, we already knew that IgE Ab to alpha-gal was common among children in an African village and in rural Ecuador [31▪,35]. In addition, we have heard reports about children having multiple tick bites at camps in Tennessee. Over the last 3 years, particularly with the screening in Lynchburg, we have identified a series of children who presented with either anaphylaxis, recurrent acute episodes of urticaria, or chronic urticaria [36▪▪]. The serology of these cases appears to be similar to that of the adults, as does the severity of the reactions: 44% had anaphylaxis at presentation and 46% sought care in an emergency department/urgent care center [36▪▪]. At this time, however, we have no local reference base to estimate the prevalence of IgE Ab to alpha-gal in children. It would be difficult to ascertain an accurate estimate without surveying a large population of children to identify the prevalence of the IgE antibodies. For the moment, we have chosen not to carry out challenges on children because we believe that the mechanism of the delay can best be studied in adults.
CONCLUSION
The discovery of IgE antibodies to the oligosaccharide alpha-gal has made it possible to investigate several novel aspects of allergic disease. The obvious thing is that the glycosylation of therapeutic recombinant molecules, particularly monoclonal antibodies, can create a risk for severe hypersensitivity reactions [24]. The IgE responses induced by tick bites give rise to multiple questions. It is clear that these responses can occur in individuals of all ages and do not appear to be different in individuals who are otherwise atopic. In some cases, the IgE responses are very high in titer and make a large contribution to total serum IgE. The possible mechanisms for these responses include direct switch of B cells from Bμ to Bε occurring outside an organized germinal center, priming of B cells in the skin, and questions about the relevance of T cells to the response. It is clear that understanding how tick bites induce such dramatic IgE responses could have great significance to IgE responses in general and to the significance of the skin in particular. In addition, because these IgE antibodies also bind to a wide range of mammalian proteins we recognized the syndrome of ‘delayed anaphylaxis to mammalian meat’ [23]. However, the most interesting feature of the clinical reactions may be that the first symptoms (i.e. itching or urticaria) occur 3–6 h after eating meat and would normally be regarded as ‘spontaneous’ or ‘idiopathic’ anaphylaxis. Understanding the factors that control the delay may provide real insight into the factors that control anaphylaxis.
KEY POINTS.
Tick bites are an important cause of IgE antibody responses, including IgE responses to tick proteins and to the oligosaccharide galactose-alpha-1,3-galactose.
Many patients who have IgE antibodies to alpha-gal experience delayed anaphylactic and urticarial reactions after eating mammalian meat, which carries the oligosaccharide.
The association between tick bites, IgE antibodies to alpha-gal, and delayed reactions to red meat has now been reported from multiple countries, including Australia, Sweden, France, Spain, and Japan, as well as the United States.
Acknowledgments
The authors are grateful to Hayley James for assistance with this manuscript.
Many of the studies discussed in this report were supported by the NIH grants R01-AI-20565, U19-AI-070364, R21-AI-087985, and K08-AI-1085190.
Footnotes
Conflicts of interest
S.P.C. and T.A.E.P.-M. report ongoing support for IgE assays from Thermo Fisher. T.A.E.P.M. has a patent for the use of IgE assays to identify the risk of anaphylaxis with recombinant molecules. He is also a consultant to Viracor-IBT Laboratories.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest Additional references related to this topic can also be found in the Current World Literature section in this issue (p. 453).
- 1.Francischetti IM, Sa-Nunes A, Mans BJ, et al. The role of saliva in tick feeding. Front Biosci. 2009;14:2051–2088. doi: 10.2741/3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reck J, Berger M, Marks FS, et al. Pharmacological action of tick saliva upon haemostasis and the neutralization ability of sera from repeatedly infested hosts. Parasitology. 2009;136:1339–1349. doi: 10.1017/S0031182009990618. [DOI] [PubMed] [Google Scholar]
- 3.Mans BJ, Andersen JF, Francischetti IM, et al. Comparative sialomics between hard and soft ticks: implications for the evolution of blood-feeding behavior. Insect Biochem Mol Biol. 2008;38:42–58. doi: 10.1016/j.ibmb.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwalie PC, Schultz J. Positive selection in tick saliva proteins of the Salp15 family. J Mol Evol. 2009;68:186–191. doi: 10.1007/s00239-008-9194-1. [DOI] [PubMed] [Google Scholar]
- 5.Mans BJ, Neitz AW. Adaptation of ticks to a blood-feeding environment: evolution from a functional perspective. Insect Biochem Mol Biol. 2004;34:1–17. doi: 10.1016/j.ibmb.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 6▪.Jeppesen AS, Kristiansen U, Soelberg J, Jäger AK. Antihistamine effect of Rubia tibetica, used to treat anaphylaxis caused by tick bites in the Pamir Mountains, Afghanistan. J Ethnopharmacol. 2012;141:1077–1079. doi: 10.1016/j.jep.2012.03.035. The data presented indicate that chewing Rubia tibetica root may alleviate fatal tongue or oropharngeal swelling during anaphylaxis via its antihistaminergic properties. The results illustrate the worldwide distribution of problems related to sensitization to tick bites. [DOI] [PubMed] [Google Scholar]
- 7.Adedoyin J, Gronlund H, Oman H, et al. Cat IgA, representative of new carbohydrate cross-reactive allergens. J Allergy Clin Immunol. 2007;119:640–645. doi: 10.1016/j.jaci.2006.11.637. [DOI] [PubMed] [Google Scholar]
- 8▪.Van Nunen SA, O’Connor KS, Clarke LR, et al. An association between tick bite reactions and red meat allergy in humans. Med J Aust. 2009;190:510–511. doi: 10.5694/j.1326-5377.2009.tb02533.x. As early as 2007, Dr van Nunen had recognized patients who developed allergic reactions to meat after being bitten by ticks in the bush north of Sydney. She reported those cases in abstract form to the Australasian Society of Clinical Immunology and Allergy, and published her findings after the connection with alpha-gal was described. [DOI] [PubMed] [Google Scholar]
- 9.O’Neil BH, Allen R, Spigel DR, et al. High incidence of cetuximab-related infusion reactions in Tennessee and North Carolina and the association with atopic history. J Clin Oncol. 2007;25:3644–3648. doi: 10.1200/JCO.2007.11.7812. [DOI] [PubMed] [Google Scholar]
- 10.Chung CH, Mirakhur B, Chan E, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-alpha-1,3-galactose. N Engl J Med. 2008;358:1109–1117. doi: 10.1056/NEJMoa074943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qian J, Liu T, Yang L, et al. Structural characterization of N-linked oligosaccharides on monoclonal antibody cetuximab by the combination of orthogonal matrix-assisted laser desorption/ionization hybrid quadrupole–quadrupole time-of-flight tandem mass spectrometry and sequential enzymatic digestion. Anal Biochem. 2007;364:8–18. doi: 10.1016/j.ab.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 12▪.Pointreau Y, Commins SP, Calais G, et al. Fatal infusion reactions tocetuximab: role of immunoglobulin E-mediated anaphylaxis. J Clin Oncol. 2012;30:334. doi: 10.1200/JCO.2011.38.4701. author reply 335. A recent report highlighing that severe reactions to infusion of cetuximab in patients with IgE to alpha-gal continue to occur, suggesting that assessment for the presence of this antibody be considered when clinically suspected prior to infusion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gronlund H, Adedoyin J, Commins SP, et al. The carbohydrate galactose-alpha-1,3-galactose is a major IgE-binding epitope on cat IgA. J Allergy Clin Immunol. 2009;123:1189–1191. doi: 10.1016/j.jaci.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14▪▪.Commins SP, James HR, Kelly LA, et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-(-1,3-galactose. J Allergy Clin Immunol. 2011;127:1286–1293. e1286. doi: 10.1016/j.jaci.2011.02.019. This study presents the data related to tick bites inducing the IgE Ab response to alpha-gal. The report is the first example of a response to an ectoparasite giving rise to an important form of food allergy. The results also document that tick bites can induce high titers of IgE antibodies to a single oligosaccharide epitope. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪▪.Hamsten C, Starkhammar M, Tran TA, et al. Identification of galactose-α-1,3-galactose in the gastrointestinal tract of the tick Ixodes ricinus; possible relationship with red meat allergy. Allergy. 2013;68:549–552. doi: 10.1111/all.12128. An initial demonstration of alpha-gal as a moiety present in ticks. These findings provide direct support for the view that antigens within the tick are the cause of the IgE Ab response after tick bites. [DOI] [PubMed] [Google Scholar]
- 16.Burke G, Wikel SK, Spielman A, et al. Hypersensitivity to ticks and Lyme disease risk. Emerg Infect Dis. 2005;11:36–41. doi: 10.3201/eid1101.040303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher EJ, Mo J, Lucky AW. Multiple pruritic papules from lone star tick larvae bites. Arch Dermatol. 2006;142:491–494. doi: 10.1001/archderm.142.4.491. [DOI] [PubMed] [Google Scholar]
- 18.Lee YB, Jun JB, Kim JY, et al. Multiple bites from the larvae of Haemaphysalis longicornis. Arch Dermatol. 2011;147:1333–1334. doi: 10.1001/archdermatol.2011.328. [DOI] [PubMed] [Google Scholar]
- 19.Menten-Dedoyart C, Faccinetto C, Golovchenko M, et al. Neutrophil extra-cellular traps entrap and kill Borrelia burgdorferi sensu stricto spirochetes and are not affected by Ixodes ricinus tick saliva. J Immunol. 2012;189:5393–5401. doi: 10.4049/jimmunol.1103771. [DOI] [PubMed] [Google Scholar]
- 20.Plum M, Michel Y, Wallach K, et al. Close-up of the immunogenic α1,3-galactose epitope as defined by a monoclonal chimeric immunoglobulin E and human serum using saturation transfer difference (STD) NMR. J Biol Chem. 2011;286:43103–43111. doi: 10.1074/jbc.M111.291823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galili U, Rachmilewitz EA, Peleg A, Flechner I. A unique natural human IgG antibody with antialpha-galactosyl specificity. J Exp Med. 1984;160:1519–1531. doi: 10.1084/jem.160.5.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22▪▪.Rispens T, Derksen NI, Commins SP, et al. IgE production to α-Gal is accompanied by elevated levels of specific IgG1 antibodies and low amounts of IgE to blood group B. PLoS One. 2013;8:e55566. doi: 10.1371/journal.pone.0055566. Contradicting the previous reports, antibodies to alpha-gal were found to be significantly less abundant in individuals with blood group B or AB. Elevated titers of IgG antialpha-gal were found in IgE-positive individuals and this was of the IgG1 isotype (the typical response to alpha-gal in individuals not exposed to tick bites is IgG2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009;123:426–433. doi: 10.1016/j.jaci.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Commins SP, Platts-Mills TA. Allergenicity of carbohydrates and their role in anaphylactic events. Curr Allergy Asthma Rep. 2010;10:29–33. doi: 10.1007/s11882-009-0079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25▪.Mullins RJ, James H, Platts-Mills TA, Commins S. Relationship between red meat allergy and sensitization to gelatin and galactose-α-1,3-galactose. J Allergy Clin Immunol. 2012;129:1334–1342. e1331. doi: 10.1016/j.jaci.2012.02.038. A consideration for physicians and patients with IgE to alpha-gal, cross-reactivity exists between gelatin and alpha-gal. Although sensitization to protein epitopes does occur, sensitization to gelatin may be explained in certain locations by IgE to alpha-gal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jappe U. Update on meat allergy: α-Gal: a new epitope, a new entity? Hautarzt. 2012;63:299–306. doi: 10.1007/s00105-011-2266-y. [DOI] [PubMed] [Google Scholar]
- 27.Jacquenet S, Moneret-Vautrin DA, Bihain BE. Mammalian meat-induced anaphylaxis: clinical relevance of antigalactose-alpha-1,3-galactose IgE confirmed by means of skin tests to cetuximab. J Allergy Clin Immunol. 2009;124:603–605. doi: 10.1016/j.jaci.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 28▪▪.Morisset M, Richard C, Astier C, et al. Anaphylaxis to pork kidney is related to IgE antibodies specific for galactose-alpha-1,3-galactose. Allergy. 2012;67:699–704. doi: 10.1111/j.1398-9995.2012.02799.x. The data emphasize the wide range of mammalian foods that are eaten in Europe, which includes not only horse, goat, and rabbit meat, but also kidneys, stomach, and other organs. In the United States, venison, bear, and squirrel are common, but they are less common causes of reactions. [DOI] [PubMed] [Google Scholar]
- 29.Adedoyin J, Johansson SG, Gronlund H, van Hage M. Interference in immunoassays by human IgM with specificity for the carbohydrate moiety of animal proteins. J Immunol Methods. 2006;310:117–125. doi: 10.1016/j.jim.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Perzanowski MS, Rönmark E, Nold B, et al. Relevance of allergens from cats and dogs to asthma in the northernmost province of Sweden: schools as a major site of exposure. J Allergy Clin Immunol. 1999;103:1018–1024. doi: 10.1016/s0091-6749(99)70173-9. [DOI] [PubMed] [Google Scholar]
- 31▪.Commins SP, Kelly LA, Rönmark E, et al. Galactose-α-1,3-galactose-specific IgE is associated with anaphylaxis but not asthma. Am J Respir Crit Care Med. 2012;185:723–730. doi: 10.1164/rccm.201111-2017OC. The data presented show that the specific IgE Ab response can contribute to total serum IgE and that the alpha-gal epitope is not airborne in homes with or without cats or dogs. The authors concluded that the association between IgE Ab and asthma relates to IgE Ab for protein allergens that are inhaled. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sekiya K, Fukutomi Y, Nakazawa T, et al. Delayed anaphylactic reaction to mammalian meat. J Investig Allergol Clin Immunol. 2012;22:446–447. [PubMed] [Google Scholar]
- 33.Arkestål K, Sibanda E, Thors C, et al. Impaired allergy diagnostics among parasite-infected patients caused by IgE antibodies to the carbohydrate epitope galactose-α-1,3-galactose. J Allergy Clin Immunol. 2011;127:1024–1028. doi: 10.1016/j.jaci.2011.01.033. [DOI] [PubMed] [Google Scholar]
- 34.Panikkar RP, Astsaturov I, Langer CJ. The emerging role of cetuximab in head and neck cancer: a 2007 perspective. Cancer Invest. 2008;26:96–103. doi: 10.1080/07357900701601002. [DOI] [PubMed] [Google Scholar]
- 35.Moncayo AL, Vaca M, Oviedo G, et al. Effects of geohelminth infection and age on the associations between allergen-specific IgE, skin test reactivity, and wheeze: a case–control study. Clin Exp Allergy. 2013;43:60–72. doi: 10.1111/cea.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36▪▪.Kennedy J, Stallings A, Platts-Mills T, et al. Galactose-alpha-1,3-galactose and delayed anaphylaxis, angioedema, and urticaria in children. Pediatrics. 2013;131:1–8. doi: 10.1542/peds.2012-2585. This report extends the syndrome of delayed anaphyalxis, urticaria, and angio-edema to children. Particularly in geographic locales where ticks are present, IgE to alpha-gal can be an important cause of allergic reactions that might otherwise be considered idiopathic. [DOI] [PMC free article] [PubMed] [Google Scholar]