Supplemental Digital Content is Available in the Text.
Results suggest that early magnetic resonance imaging (MRI) has a strong iatrogenic effect leading to prolonged disability and increased medical costs, regardless of whether a patient has acute radiculopathy. The findings support evidence-based guidelines to avoid MRI for acute back pain during the first month except for “red flag” indications.
Keywords: low back pain, radiculopathy, nonspecific back pain, evidence-based guidelines, MRI, iatrogenic, workers compensation, disability, costs
Abstract
Study Design.
Retrospective cohort study.
Objective.
To determine the effect of early (receipt ≤30 d postonset) magnetic resonance imaging (MRI) on disability and medical cost outcomes in patients with acute, disabling, work-related low back pain (LBP) with and without radiculopathy.
Summary of Background Data.
Evidence-based guidelines suggest that, except for “red flags,” MRI is indicated to evaluate patients with persistent radicular pain, after 1 month of conservative management, who are candidates for surgery or epidural steroid injections. Prior research has suggested an independent iatrogenic effect of nonindicated early MRI, but it had limited clinical information and/or patient populations.
Methods.
A nationally representative sample of workers with acute, disabling, occupational LBP was randomly selected, oversampling those with radiculopathy diagnoses (N = 1000). Clinical information from medical reports was used to exclude cases for which early MRI might have been indicated, or MRI occurred more than 30 days postonset (final cohort = 555). Clinical information was also used to categorize cases into “nonspecific LBP” and “radiculopathy” groups and further divided into “early-MRI” and “no-MRI” subgroups. The Cox proportional hazards model examined the association of early MRI with duration of the first episode of disability. Multivariate linear regression models examined the association with medical costs. All models adjusted for demographic and medical severity measures.
Results.
In our sample, 37% of the nonspecific LBP and 79.9% of the radiculopathy cases received early MRI. The early-MRI groups had similar outcomes regardless of radiculopathy status: much lower rates of going off disability and, on average, $12,948 to $13,816 higher medical costs than the no-MRI groups. Even in a subgroup with relatively minimal disability impact (≤30 d of total lost time post-MRI), medical costs were, on average, $7643 to $8584 higher in the early-MRI groups.
Conclusion.
Early MRI without indication has a strong iatrogenic effect in acute LBP, regardless of radiculopathy status. Providers and patients should be made aware that when early MRI is not indicated, it provides no benefits, and worse outcomes are likely.
Level of Evidence: 3
Evidenced-based clinical practice guidelines for acute low back pain (LBP) recommend that magnetic resonance imaging (MRI) may be indicated in the presence of “red flags” (including infection, cancer, and cauda equina syndrome), but that imaging not be done for patients with nonspecific LBP.1 Additionally, the guidelines recommend delaying imaging in patients with a suspected herniated disc or spinal stenosis (i.e., based on consistent signs and symptoms) to allow for the natural history of improvement that occurs during the first month in up to 50% of disc herniation and radiculopathy cases.2 Then, MRI may be indicated, after a month of conservative management in these cases, to provide anatomic definition if surgery or epidural steroid injections are being considered.
Although MRI is a sensitive diagnostic tool, it is highly nonspecific and reveals abnormalities that are often poorly correlated with symptoms, with disc herniation and/or spinal stenosis found in 20% to 57% of asymptomatic subjects.3–5 Even in acute radiculopathy, early MRI does not provide information that improves treatment decisions or outcomes.6,7 Despite these concerns, the rate of spinal MRIs in Medicare beneficiaries increased 307% from 1994 to 2005,8 and they are frequently ordered prematurely and/or without a clear indication in other patient populations as well.9–13
A recent study of claimants with acute, disabling, work-related LBP suggested iatrogenic effects of early (defined as in the first month) MRI, including worse disability, increased medical costs, and increased risk for surgery that were unrelated to severity.12 However, that study was based on administrative claims data, which have known limitations,14,15 such as absence of clinical information regarding history of recurrent or chronic LBP, or presence of red flags for which an early MRI might have been indicated.
The purpose of this study was to determine whether early MRI affected the outcomes of disability and total medical costs in patients carefully selected to represent acute, disabling, work-related LBP without red flag indications, and to evaluate whether the impact was different for acute lumbar radiculopathy cases. Radiculopathy cases were specifically identified because this presentation often influences providers to obtain MRI prematurely.11
MATERIALS AND METHODS
Study Population
LBP claims identified by body part and nature of injury codes filed between January 1, 2006, and December 31, 2006, were extracted from administrative data from a workers compensation (WC) insurer as described in a prior study (N = 3264).12 The data represent approximately 10% of the US private WC market and includes cases from 45 states. Data extracted for each claim included 2 years of longitudinal capture of all paid indemnity (i.e., wage replacement) and paid medical services with the associated International Classification of Disease (ICD-9) codes.16 Inclusion criteria included 1 day or more of compensated lost time and at least 1 year of job tenure. Cases were excluded if lumbar MRI was obtained more than 30 days after date of onset because these cases are ambiguous with respect to guideline compliance. For example, some cases may represent those with significant and persistent unresolved radiculopathy where MRI was indicated; others may have had persistent but nonspecific LBP symptoms where MRI was not indicated.
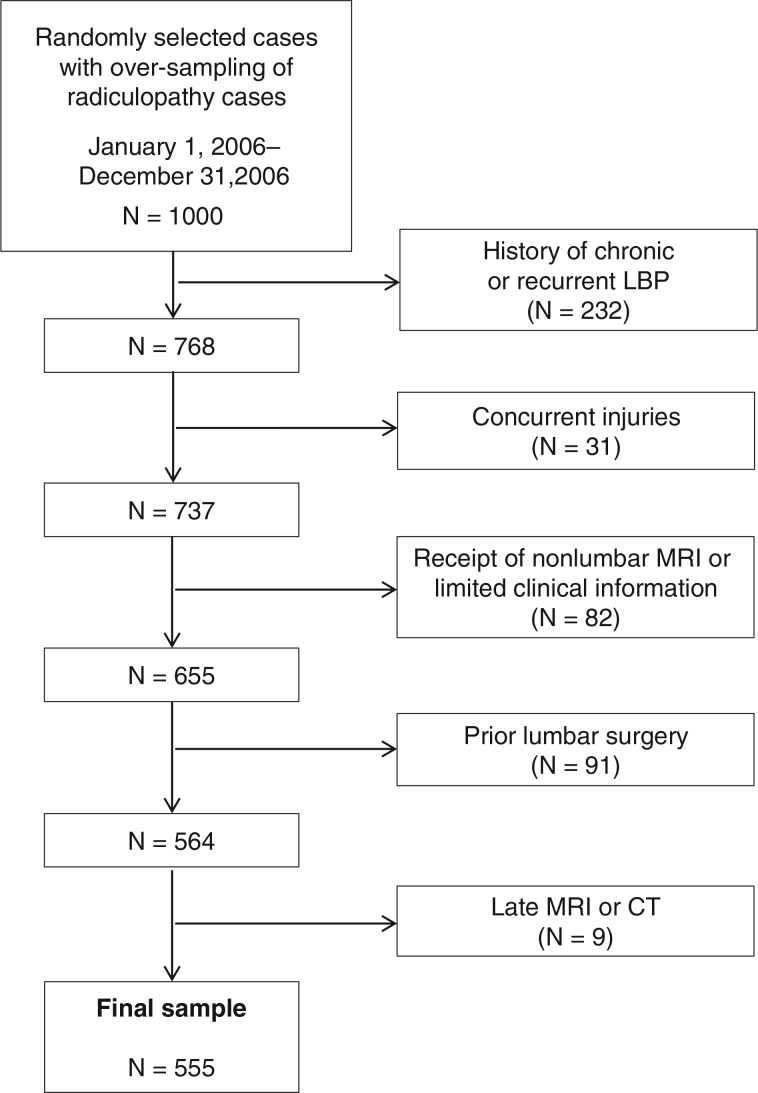
Then, a subset of 1000 claims was randomly selected, oversampling for potential radiculopathy cases based on ICD-9 codes (Appendix 1; see Supplemental Digital Content, available at http://links.lww.com/BRS/A798 which demonstrates selection based on high severity codes). Oversampling was intended to ensure that there would be a sufficient number of radiculopathy cases that did not have an early MRI for the analyses. Medical reports and notes by both claims and nurse case managers were reviewed by a registered nurse and then by 2 of the authors (A.B. and B.W.) to exclude cases with red flag indications, history of chronic or recurrent LBP or prior lumbar surgery for which early MRI might be indicated. Other exclusion criteria included concurrent injuries, receipt of nonlumbar MRI, or those with limited clinical information, resulting in a final cohort of 555 cases (Figure 1). The study was approved by the Institutional Review Board of the Liberty Mutual Research Institute for Safety.
Figure 1.
Flow diagram of case selection. MRI indicates magnetic resonance imaging; CT, computed tomography; LBP, low back pain.
Exposure
On the basis of the reported clinical signs and symptoms in the medical reports, the reviewers classified the cases into 2 diagnostic groups, nonspecific LBP and radiculopathy. Nonspecific LBP included cases with pain symptoms occurring primarily in the back and/or leg without an anatomic radicular pattern, and absence of radicular signs on physical examination. Radiculopathy cases included those with back and/or leg symptoms with an anatomic radicular pattern and/or associated radicular signs including motor weakness, decreased sensation, and decreased reflexes and/or radicular irritation signs including positive straight leg raising, positive contralateral straight leg raising, or femoral stretch.
Cases that had MRI within the first 30 days postonset (defined as the “early-MRI group”) were identified on the basis of paid medical bills with Physician's Current Procedural Terminology codes related to lumbar MRIs (72148, 72149, and 72158).17 Following medical record review, an additional 17 cases were found to have had early MRI. The outcomes of the early-MRI groups were compared with the no-MRI groups (those who never received MRI) during the 2-year follow-up period.
Outcome Measures
Disability Duration Post-MRI Within the First Disability Episode
Disability duration for all groups was defined as the number of days of continuous paid indemnity (lost wage replacement for temporary total or temporary partial lost days) followed by a more than 7-day period without indemnity payments, and truncated at the end of the 2-year follow-up period. Disability duration post-MRI for the early-MRI groups was the time on disability after the MRI to the end of the first episode of disability. Disability duration for the no-MRI groups was calculated for a comparable period-–from 16 days postonset (the median time to MRI for the early-MRI group) to the end of the first disability episode.
Total Medical Costs Post-MRI
Medical services were identified using CPT codes, and costs were based on paid-to-date medical services. Medical costs for the early-MRI group were from post-MRI to the end of the 2-year follow-up period; medical costs for the no-MRI group were calculated from 16 days postonset to the end of the follow-up period.
Covariates
The covariates included age, sex, and job tenure. State of residence was included to control for individual jurisdictional differences related to utilization review and WC cost containment efforts. Lacking direct measures in the administrative data of pain or markers of functional disability prior to MRI, the following indicators were created to control for severity.
Morphine Equivalent Amount (MEA) in the First 15 Days
Paid medical bills for opioid prescriptions received in the first 15 days postonset were identified by National Drug Codes (NDC, see http://www.fda.gov/cder/ndc/). The MEA received in the first 15 days was calculated on the basis of number of pills, strength, and equianalgesic dose, and then divided into 5 quintiles (data not shown): no opioid usage, 1 to 140 mg, 141 to 225 mg, 226 to 450 mg, and more than 450 mg, on the basis of an earlier study.18 MEA was used as an indicator of initial pain severity and has been shown to be associated with an increased risk of prolonged disability, higher medical costs, and subsequent lumbar surgery.18–20
Average Weekly Medical Costs Pre-MRI
As an index of intensity of pre-MRI care, medical costs were computed by totaling the paid costs of all pre-MRI medical services. For each case, the total pre-MRI costs were divided by the number of pre-MRI weeks to obtain the average weekly pre-MRI costs. For the no-MRI group, the first 16 days of medical costs were averaged to calculate average medical costs for a comparable period of time.
Analysis
Cohort characteristics were described using univariate statistics. To control for confounding, all potential covariates (age, sex, job tenure, pre-MRI average weekly medical costs, MEA quintile, time to first lumbar MRI, and state) were included in all models. Survival analyses (Cox proportional hazards models) were used to examine the association between receipt of an early MRI (with and without radiculopathy) with duration of the first episode of disability post-MRI. General linear multivariate regression models were used to examine the association with total medical costs post-MRI. Because medical costs could vary as a function of length of disability, we repeated the regression analyses using a subgroup (N = 169) with relatively minimal disability impact (≤30 d). SAS version 9.2 was used in all data analyses.
RESULTS
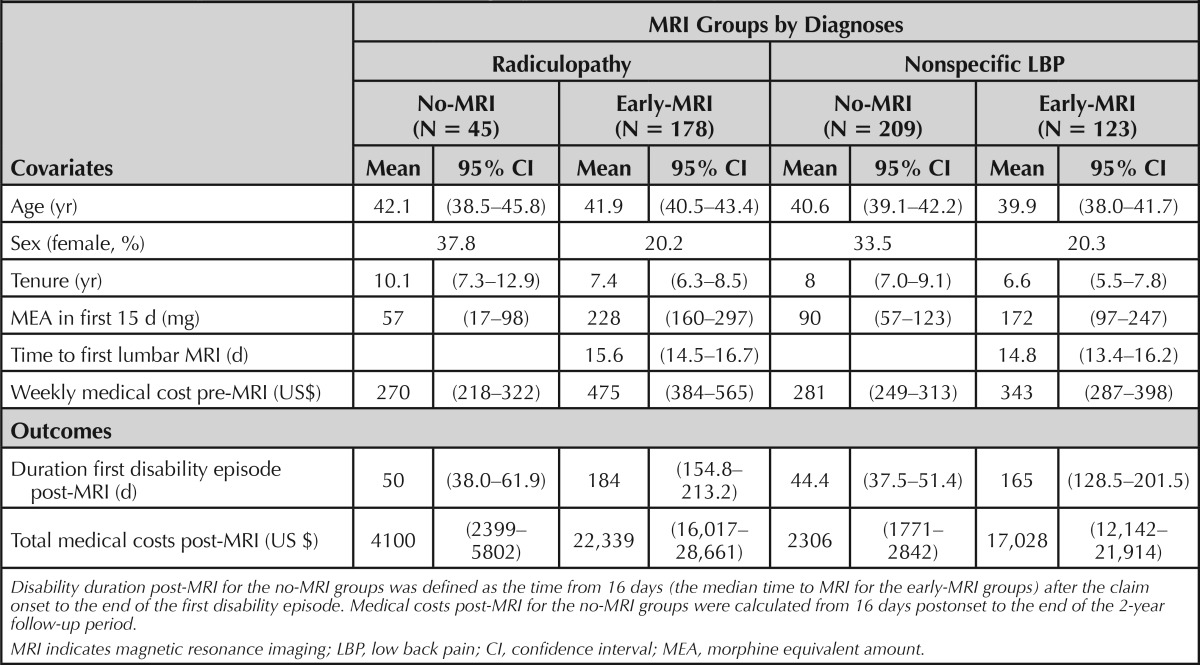
Of the final cohort, 73.3% were male, and the mean age was 41 years. Of the sample, 40.2% were classified as radiculopathy cases, and of these, 79.8% received an early MRI. Of the nonspecific LBP cases, 37.0% received an early MRI (Table 1).
TABLE 1. Descriptive Statistics for Demographic and Severity Covariates and Outcomes.
Early-MRI and No-MRI Group Comparisons
The early-MRI groups (n = 301) had fewer females, shorter job tenure, greater pre-MRI medical costs, and higher MEA in the first 15 days than the no-MRI groups (n = 254), regardless of radiculopathy status. There were no significant differences in age among the groups.
Outcomes
Disability Duration Post-MRI
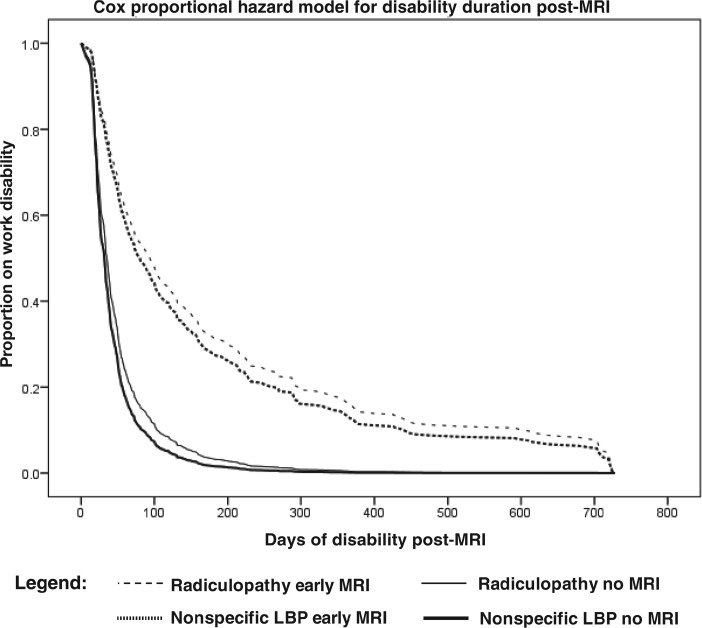
Figure 2 illustrates the length of disability curves for each of the 4 comparison groups. The early-MRI groups had significantly longer lengths of disability than the no-MRI groups, regardless of radiculopathy (Table 1). Survival analyses using fully-adjusted Cox proportional hazards models to compare the early-MRI groups to the no-MRI groups revealed that the rate of going off disability was 72% lower for the radiculopathy cases and 68% lower for the nonspecific LBP cases (Table 2).
Figure 2.
Daily proportion of cases on first episode of disability by diagnostic/MRI subgroup. MRI indicates magnetic resonance imaging; LBP, low back pain.
TABLE 2. Fully-Adjusted Cox Proportional Hazards Model to Go Off Disability Post-MRI.
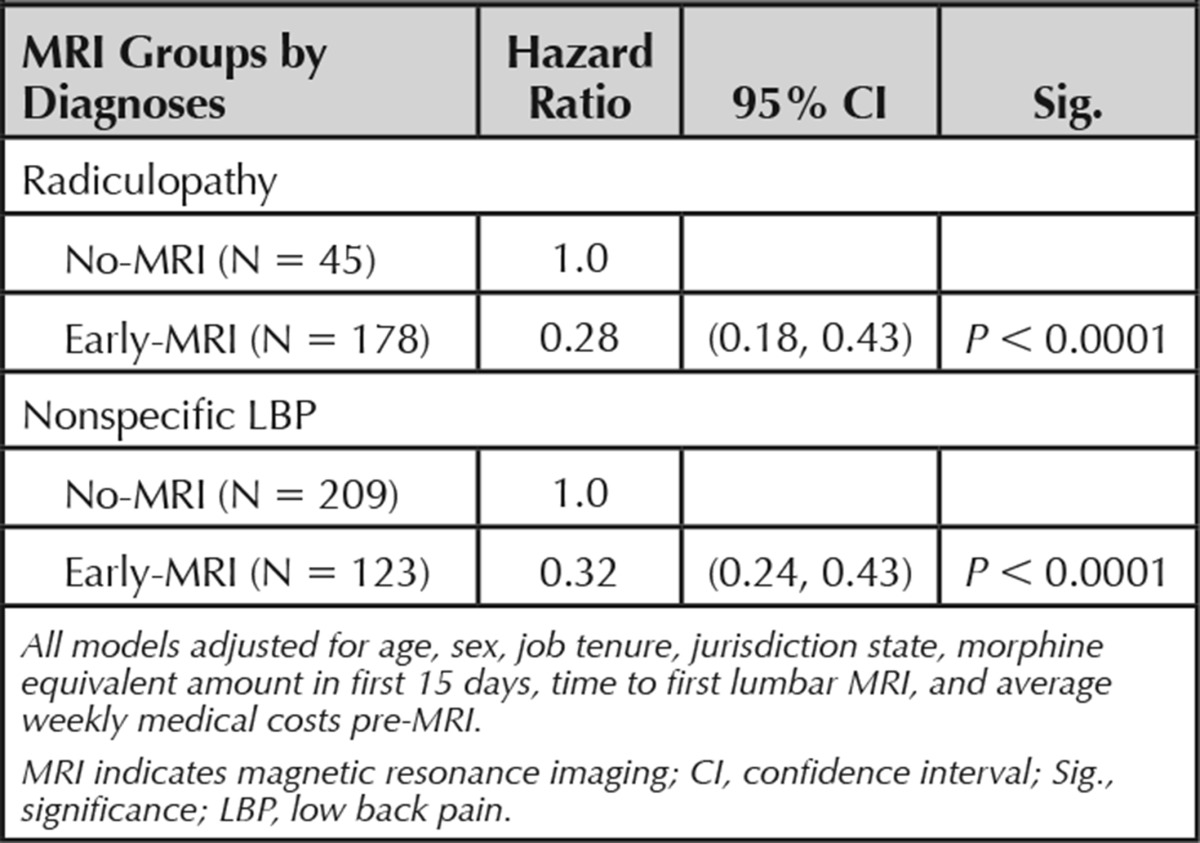
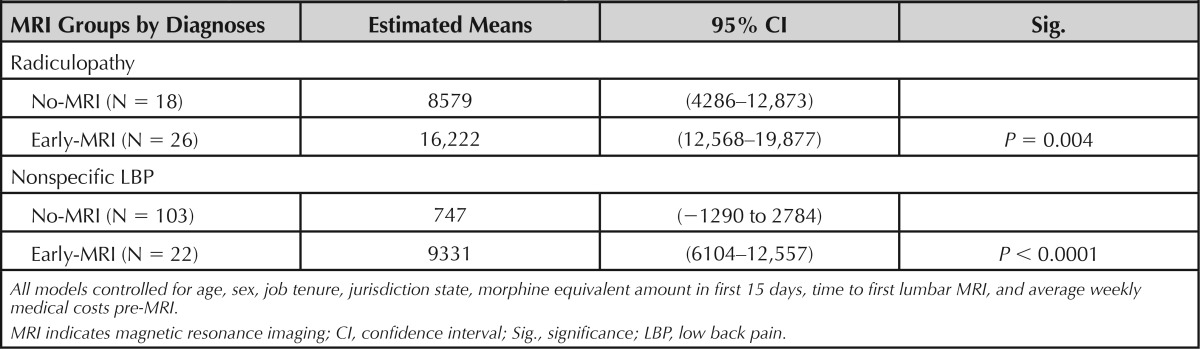
Total Medical Costs Post-MRI
The early-MRI groups had significantly higher total medical costs in the post-MRI period than the no-MRI groups (Table 3). Multivariate linear regression models measured the extent to which medical costs differed between groups while controlling for potential covariates. Medical expenditures of the nonspecific LBP and radiculopathy early-MRI groups were, on average, $12,948 and $13,816 (respectively) higher than those of the corresponding no-MRI groups.
TABLE 3. Total Medical Expenditures Post-MRI (US$), Fully-Adjusted Multivariate Regression Model Results.

In the cases with 30 days or less of total disability after the initial MRI (or after 16 d in the no-MRI groups), disability duration was not significantly different among the groups (Table 4) but total medical costs post-MRI were much higher for the early-MRI groups than the no-MRI groups (Table 5).
TABLE 4. Descriptive Statistics for Those With Disability Duration 30 Days or Less.
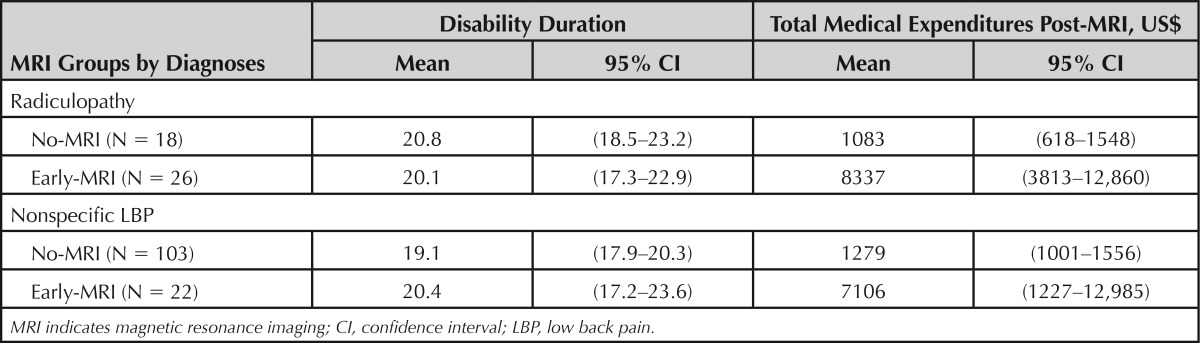
TABLE 5. Total Medical Expenditures Post-MRI (US$) for Cases With Disability Duration 30 Days or Less, Fully-Controlled Multivariate Regression Model Results.
DISCUSSION
This study examined the impact of early MRI for those with acute, disabling, work-related nonspecific, and radicular LBP on disability and medical cost outcomes. The vast majority of the radiculopathy group received MRI within the first month of care, despite guideline recommendations to delay imaging to allow for the natural history of improvement to occur. The receipt of early MRI in both groups was associated with worse outcomes, even after controlling for severity and demographic factors. On average, the rate of going off disability for those who received an early MRI was approximately one-third the rate of those who did not receive MRI. Furthermore, early MRI increased total medical costs (a surrogate for medical use) by approximately $13,000 per case. Even in the subset with relatively prompt resolution of their problem as indicated by short disability duration, there was a striking impact of early MRI on early medical use. These results strengthen the findings of an earlier study with a larger sample that suggested an iatrogenic effect of early MRI.12 However, the prior study was based on administrative claims data which have limited information regarding history of recurrent or chronic LBP and prior lumbar surgery for which an early MRI might be indicated.
The results related to disability are also similar to a recent study of patients with work-related LBP from Washington state which found that those with both mild/major sprains (comparable to our nonspecific LBP group) and radiculopathy who had early MRI had longer work disability outcomes at 1-year follow-up.13 A systematic review of randomized trials found no benefit in health, function, or disability outcomes with early MRI in LBP.21
The study results underscore the significant consequences associated with the use of nonindicated early MRI. Guidelines recommend against using this modality initially in the management of acute LBP, even with the presence of radiculopathy because it is not likely to improve care.6,7 The primary recommendation in acute LBP when red flags are not present (no cases with red flags were present in our cohort) is to pursue a conservative approach because the majority of cases with both nonspecific and radicular LBP will resolve spontaneously within the first 4 to 6 weeks after onset.2
The potential underlying reasons for ordering these tests may include the influence of radiculopathy, patient requests, provider concerns, or desire to satisfy or allay patient fears, and economic incentives to pursue overly intensive treatment strategies. The finding that the majority of radiculopathy cases received early MRI strongly supports an earlier study that suggested providers' self-reported clinical decisions are influenced by radicular signs and symptoms despite the guideline recommendations.11 They may also have felt pressured by patient requests to order MRI for unexplained LBP. Some providers may have planned to use MRI results as a way of reassuring patients.22,23 However, the results often lead to the opposite effect—instead of reassurance, patients develop a decreased sense of well-being.7,24
As MRI resolution has improved, the detection of smaller abnormalities has increased, which may potentially result in a cascade of additional testing and interventions.25 Patients and/or physicians may misinterpret unrelated abnormalities as indicative of a more specific or severe diagnosis, and focus their attention on an abnormality to which they erroneously attribute the patient's pain. Although the increase in imaging has been associated with an increase in specialist referrals and spinal surgery without improvement in outcomes, we were unable to assess the surgical outcome due to the small number of surgical procedures in the no-MRI group.26,27 The resulting diagnostic focus may also lead patients to expect a “cure” or complete recovery28 and lead to requests for more intensive interventions or a delay in the initiation of a functional restoration program.29–31
The finding of greater medical use in the early-MRI cohort suggests that obtaining an early MRI may be the first indication of a cascade pattern of care that is characterized by overprescribing, overtesting, intensive and ineffective treatment, and ultimately, poor outcomes.29 Our results suggest that this effect occurs early on in the course of care. Even in those who returned to work relatively quickly, indicative of substantial resolution of their back problem, those who had early MRI experienced much more intensive medical care, with post-MRI costs (exclusive of the cost of MRI itself) approximately $8000 higher than that of the no-MRI groups, yet there was no evidence of better outcomes, regardless of radiculopathy status. The increased services may have been due to the medicalization of clinically irrelevant findings leading to patients' requests for more intensive interventions.
Proactive education of patients and providers, timely and intensive utilization review, peer-to-peer communication, and targeted disease management programs may be helpful in efforts to decrease these aberrant practices and their negative consequences.32–34 Some have suggested that establishing clinical pathways for care that target potentially problematic cases (i.e., those at high risk for inappropriate imaging) early on may be especially helpful.35 Addressing the economic incentives that encourage physician self-referral is suggested as well.36
Strengths and Limitations
This study has several strengths. Unlike prior administrative data-based studies, clinical records enabled better classification of cases for which early MRI might be indicated and provided information on several cases with MRI services that did not appear in medical billing records. Although classification of radiculopathy by clinical notes was probably more accurate than relying on ICD-9 codes in medical bills, the results obtained here were quite similar to a prior study of a similar cohort based entirely on administrative data,12 suggesting that administrative data can be used effectively to conduct detailed health-services research evaluations in occupational LBP. WC records have the advantage of providing reasonably complete capture of all medical services regardless of provider because WC insurance is the first and sole payor in all states for medical services for accepted work-related injury claims. Finally, the cohort represents a working population, an important group not often represented in radiology health services research in the United States, and is based on typical community practice from diverse geographic regions.37
Weaknesses include the limitations of our clinical data used to categorize cases into radiculopathy and nonspecific groups, such as brevity and lack of detail in clinical notes regarding physical examination findings, and the somewhat incomplete capture of important clinical notes that may occur in the WC claims system. To some extent, this was addressed by reviewing both the case manager and clinical notes collected in an electronic document management system and, when possible, evaluating the indications provided for MRI scans.
Patient-reported pain and function information was not available in the administrative data, nor was it consistently captured in the clinical notes. Instead, indirect measures of severity were used and the results were stratified by radiculopathy status to provide another dimension of severity. However, the decision to order MRI should be based on signs and symptoms of radiculopathy or spinal stenosis that persist after 1 month of conservative care.1 Potential confounders, including psychiatric comorbidities, fear avoidance, catastrophizing, and somatization that could contribute to disability and cost, were also not available. However, these factors should not have influenced the decision to order early MRI. Lastly, although patient matching would have been ideal to adjust for baseline characteristics, the data were limited; a multivariate modeling strategy was used instead, achieving substantially the same results.
Perhaps cases that had MRI more than 30 days after onset should have been included in the no-MRI group for comparison with the early-MRI group and not excluded from the analysis. These cases may have had worse outcomes than the no-MRI group, and their inclusion in the no-MRI group may have made the differences between no-MRI and early-MRI groups less distinct. However, our study purpose was to study the effect of the “exposure” of early MRI. Specifically, the early-MRI group was exposed to the risk of iatrogenic effects in the first month, whereas the no-MRI group had no exposure to this risk. The cases receiving MRI after 30 days represent a mix of situations, both appropriate testing for those with radicular indications who failed to improve after a trial of conservative treatment, or inappropriate testing for patients with nonspecific findings requesting MRI or whose provider routinely orders MRI for cases with persistent complaints, or for reassurance. Thus, they were not included in the no-MRI group because some, like the early-MRI group, were exposed to the same risk of iatrogenic effects, but at a later time, and would likely confound the comparative results.
CONCLUSION
After selecting and grouping cases on the basis of detailed clinical information, the study results were similar to those found in a sample using administrative data; both nonspecific LBP and radiculopathy cases who received early MRI had worse outcomes, even after controlling for severity and demographic factors. The implications of this study are consistent with other results in similar populations, suggesting that early MRI without indication does not improve outcomes and seems to have a strong iatrogenic effect in acute LBP, regardless of whether a patient has acute radiculopathy. This evidence reinforces that both providers and patients should be made aware that when early MRI is not indicated, its use provides no benefits and could result in worse outcomes such as iatrogenic work disability and unnecessary medical procedures.
Key Points
Early MRI (receipt ≤30 d postonset) without clear indications was common in acute, uncomplicated, disabling, work-related LBP regardless of the presence or absence of radiculopathy.
The early-MRI groups had prolonged disability and, on average, $12,948 to $13,816 higher medical costs per case than the no-MRI groups, regardless of radiculopathy status.
Even in a subgroup with relatively short, homogeneous post-MRI disability, medical costs of the radiculopathy and nonspecific early-MRI groups were, on average, $7643 and $8584 (respectively) higher than the corresponding no-MRI groups.
The study results, based on classification of radiculopathy by clinical notes, were quite similar to a prior study of a similar cohort based on administrative data, suggesting that administrative data can be used effectively to conduct health-services research evaluations in occupational LBP.
Supplementary Material
Acknowledgments
The authors thank Marian Mamayek for her assistance in medical record review, Santosh Verma and Larry Hettinger for their reviews of earlier drafts of the manuscript, and Margaret Rothwell for proofreading and final editing of the manuscript.
Supplemental digital content is available for this article. Direct URL citation appearing in the printed text is provided in the HTML and PDF version of this article on the journal's web site (www.spinejournal.com).
Footnotes
Address correspondence and reprint requests to Glenn Pransky, MD, MOccH, Liberty Mutual Research Institute for Safety, 71 Frankland Rd, Hopkinton, MA 01748; E-mail: Glenn.Pransky@LibertyMutual.com
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
No relevant financial activities outside the submitted work.
References
- 1.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147:478–91. [DOI] [PubMed] [Google Scholar]
- 2.Vroomen PCAJ, de Krom MCTFM, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract 2002;52:119–23. [PMC free article] [PubMed] [Google Scholar]
- 3.Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Jt Surg 1990;72:403–8. [PubMed] [Google Scholar]
- 4.Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 2002;137:586–97. [DOI] [PubMed] [Google Scholar]
- 5.Jensen MC, Brant-Zawadzki MN, Obuchowski NA, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331:69–73. [DOI] [PubMed] [Google Scholar]
- 6.Gilbert FJ, Grant AM, Gillan MGC, et al. Low back pain: influence of early MR imaging or CT on treatment and outcome—multicenter randomized trial. Radiology 2004;231:343–51. [DOI] [PubMed] [Google Scholar]
- 7.Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005;237:597–604. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cherkin DC, Deyo RA, Wheeler K, et al. Physician variation in diagnostic testing for low back pain: who you see is what you get. Arthritis Rheum 1994;37:15–22. [DOI] [PubMed] [Google Scholar]
- 10.Di Iorio D, Henley E, Doughty A. A survey of primary care physician practice patterns and adherence to acute low back problem guidelines. Arch Fam Med 2000;9:1015–21. [DOI] [PubMed] [Google Scholar]
- 11.Webster BS, Courtney TK, Huang Y-H, et al. Physician's initial management of acute low back pain versus evidence-based guidelines: influence of sciatica. J Gen Intern Med 2005;20:1132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webster BS, Cifuentes M. Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. JOEM 2010;52:900–7. [DOI] [PubMed] [Google Scholar]
- 13.Graves JM, Fulton-Kehoe D, Jarvik JG, et al. Early imaging for acute low back pain: One-year health and disability outcomes among Washington State workers. Spine 2012;37:1617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deyo RA, Taylor VM, Diehr P, et al. Analysis of automated administrative and survey databases to study patterns and outcomes of care. Spine 1994;19:2083S–91S. [DOI] [PubMed] [Google Scholar]
- 15.Faciszewski T. Administrative databases in spine research. Spine 1997;22:1270–5. [DOI] [PubMed] [Google Scholar]
- 16.Commission on Professional and Hospital Activities. International Classification of Diseases, 9th Revision, Clinical Modification, ICD-9-CMed. Ann Arbor, MI: Edwards Brothers, Inc.; 1980. [Google Scholar]
- 17.American Medical Association. Current Procedural Terminology (CPT). Chicago: American Medical Association; 2002. [Google Scholar]
- 18.Webster BS, Verma S, Gatchel R. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine 2007;32:2127–32. [DOI] [PubMed] [Google Scholar]
- 19.Franklin GM, Stover BD, Turner JA, et al. Early opioid prescription and subsequent disability among workers with back injuries: the Disability Risk Identification Study Cohort. Spine 2008;33:199–204. [DOI] [PubMed] [Google Scholar]
- 20.Volinn E, Fargo JD, Fine PG. Opioid therapy for nonspecific low back pain and the outcome of chronic work loss. Pain 2009;142:194–201. [DOI] [PubMed] [Google Scholar]
- 21.Chou R, Fu R, Carrino JA, et al. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet 2009;373:463–72. [DOI] [PubMed] [Google Scholar]
- 22.Campbell EG, Regan S, Gruen RL, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med 2007;147:795–802. [DOI] [PubMed] [Google Scholar]
- 23.Little P, Dorward M, Warner G, et al. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referral, and prescribing in primary care: nested observational study. [published online ahead of print February 13, 2004]. Br Med J 2004;328:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ash LM, Modic MT, Obuchowski NA, et al. Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. Am J Neuroradiol 2008;29:1098–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deyo RA. Cascade effects of medical technology. Annu Rev Public Health 2002;23:23–44. [DOI] [PubMed] [Google Scholar]
- 26.Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs radiographs for patients with low back pain: a randomized controlled trial. J Am Med Assoc 2003;289:2810–8. [DOI] [PubMed] [Google Scholar]
- 27.Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine 2003;28:616–20. [DOI] [PubMed] [Google Scholar]
- 28.Abenhaim L, Rossignol M, Gobeille D, et al. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine 1995;20:791–5. [DOI] [PubMed] [Google Scholar]
- 29.Deyo RA. Magnetic resonance imaging of the lumbar spine. Terrific test or tar baby? N Engl J Med 1994;331:115–6. [DOI] [PubMed] [Google Scholar]
- 30.Fordyce WE. Back Pain in the Workplace: Management of Disability in Nonspecific Conditions. Fordyce WE. ed. Seattle: IASP Press; 1995. [DOI] [PubMed] [Google Scholar]
- 31.Roland M, van Tulder M. Should radiologists change the way they report plain radiography of the spine? The Lancet 1998;352:229–30. [DOI] [PubMed] [Google Scholar]
- 32.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. J Am Med Assoc 1999;282:1458–65. [DOI] [PubMed] [Google Scholar]
- 33.Good Stewardship Working Group. The “top 5” lists in primary care: Meeting the responsibility of professionalism. Arch Intern Med 2011;171:1385–90. [DOI] [PubMed] [Google Scholar]
- 34.Chou R, Qaseem A, Owens DK, et al. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med 2011;154:181–9. [DOI] [PubMed] [Google Scholar]
- 35.Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther 2011;41:838–46. [DOI] [PubMed] [Google Scholar]
- 36.Shreibati JB, Baker LC. The relationship between low back magnetic resonance imaging, surgery, and spending: impact of physician self-referral status. Health Serv Res 2011;46:1362–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baras JD, Baker LC. Magnetic resonance imaging and low back pain care for Medicare patients. Health Aff (Millwood) 2009;28:w1133–40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.