Abstract
Adult acute lymphoblastic leukemia (ALL) is a heterogeneous disease, due to the expression of different biological and clinical risk factors, for which allogeneic stem cell transplantation (alloHSCT) is an effective consolidation therapy. The non-relapse mortality of alloHSCT remains significantly higher compared with that of conventional chemotherapy. Therefore, one of the main challenges in the care of ALL is to establish a more precise prognostic definition to select patients who could take advantage from an alloHSCT. Currently, the use of minimal residual disease following induction and early consolidation therapy has improved the prognostic accuracy in defining ALL risk class. In Philadelphia-positive ALL, the introduction of tyrosine kinase inhibitors pre and post alloHSCT appears to improve outcomes significantly and, in the absence of specially designed clinical trials, alloHSCT remains the most effective post-remission therapy. Nowadays, alloHSCT can be performed according to various modalities encompassing the use of different conditioning regimens, as well as distinct donors and stem cell source, with a significant accessibility to transplant.
Introduction
Modern intensive induction chemotherapy allows most adult patients with acute lymphoblastic leukemia (ALL) to achieve a complete hematologic remission (CR). However, only 40% of patients survive five years or more.1–4 Allogeneic hematopoietic stem cell transplantation (alloHSCT) is an effective post-remission treatment in patients with ALL; however, its remarkable curative potential is often counterbalanced by a high incidence of post-transplant complications that lead to a high non-relapse mortality (NRM). Chronic graft-versus-host disease (GVHD) with a related poor quality of life represents an additional severe concern, so that the optimal timing and use of this treatment modality remains an issue of debate. Thus, it is crucial to identify patients who have high chances of cure with standard therapy and those for whom alloHSCT is the only possible post-remission therapy. In this regard, a risk-adapted strategy, using clinical and/or biological features, such as age, white cell count, time to obtain CR, disease immunophenotype, cytogenetics, and molecular abnormalities, may help in selecting patients at highest risk for relapse, who may benefit from alloHSCT. Moreover, evidence is growing that the evaluation of minimal residual disease (MRD) can further improve the prognostic accuracy in defining ALL risk classes. In this review, we update the indications for an alloHSCT in adult ALL patients. We also discuss the issue of the conditioning regimens before transplant as well as the most appropriate stem cell source.
Which Patients Should Have a Transplant?
Clinical and biological risk stratification
At diagnosis, prognostic factors can be defined as patient or disease related. Among these latter white blood cell count (WBC) and some, well defined, immunologic, cytogenetic or molecular profiles reflect the extensive biologic heterogeneity of ALL.5 A high WBC count at diagnosis (greater than 30×109/L for B lineage ALL and 100×109/L for T-lineage ALL) is associated with a poor prognosis.6–9 Similarly, a very immature phenotypes, such as pro-B or pro and pre T, and mature T phenotypes (EGIL BI and TI/TII/TIV) are considered prognosticator adverse.10,11 Some cytogenetic abnormalities such as t(9;22)(q34;q11), t(4;11)(q21;q23), t(8;14)(q24.1;q32), the presence of a complex karyotype (defined as ≥ 5 chromosomal abnormalities) or low hypodiploidy/near triploidy, are similarly associated with an adverse prognosis.12,13 Age remains the most important clinical risk factor and overall survival (OS) dramatically decreases with an increasing age. Young adults (younger than 35 years) may have a very good OS (up to 60% or more) if they are appropriately treated according to intensive pediatric protocols. On the contrary older adults (older than 55) have a probability of survival of 20% at 3 years with a disease-free survival (DFS) rate lower than 20% if no transplant options are offered as post-remission therapy.6,7,14–17 The above reported prognostic factors are summarized in Table 1.
Table 1.
Clinical and biological risk factor at diagnosis in adult ALL
| Risk factors | Very high risk |
High risk Any of the following: |
|---|---|---|
| Age≥ 35 years | ✓ | |
| WBC > 30×109/L for B cell phenotype >100×109/L for T cell phenotype |
✓ | |
| Very immature phenotypes, such as pro-B or pro and pre T phenotypes and mature-T (EGIL BI and TI/TII/TIV) | ✓ | |
| Cytogenetics: t (9;22) prior to tyrosine kinase inhibitors; t(4;11), t(8;14), t(1;19), abn 11q23, +8, −7, del6q, low hypodiploidy with 30–39 chromosomes, near triploidy with 60–78 chromosomes, complex with ≥5 unrelated anomalies | ✓ | |
| Molecular genetics: BCR-ABL1 rearrangement prior to tyrosine kinase inhibitors, KMT2A rearrangements, BCR-ABL1-like ALL (CLRF2/JAK mutations), IKZF1 deletion (B-ALL); wild-type NOTCH1/FXBW7, altered RAS/PTEN (T-ALL); dysfunctional apoptosis/proliferation mechanisms (p53, Caspases, MYC) | ✓ | |
| Late CR | ✓ | |
| MRD> 10−4 | ✓ | |
| MRD> 10−3 | ✓ |
Standard risk: none of the indicated risk factors. WBC=white blood cell; EGIL= European Group for Immunophenotyping of Leukemias; CR=complete remission; MRD=minimal residual disease.
Risk class and alloHSCT
Several studies have shown a potential benefit for alloHSCT over conventional chemotherapy for patients with high-risk (HR) disease. The French multi-center randomized trial LALA-87 found that only patients with HR features have better OS and DFS with alloHSCT, while patients with standard-risk (SR) had no significant advantage of alloHSCT over chemotherapy or autologous HSCT.18 This was confirmed by the same group in a larger study (LALA-94), that stratified only HR patients with donors to alloHSC, showing a better result in patients transplanted (5-year DFS 45% in transplanted compared to 23% in patients without donor, p=0.007).1 Similarly, the GOELAL02 trial showed an improved six year OS in the HR patients undergoing alloHSCT compared to patients without donor (6-year OS 75% vs. 40%, p=0.0027, respectively).16 Other studies suggested that alloHSCT in HR patients in first CR (CR1) offers good survival rates ranging from 40 to 60%.19–23 In contrast to the former results, there have been a number of studies, including the EORTC ALL3 trial24 or the Spanish PETHEMA ALL-93 trial,17 that failed to prove that alloHSCT produces a better outcome than autologous HSCT or chemotherapy in adults with HR ALL. More recently, the large MRC/ECOG trial7, in which the outcomes were estimated from a donor versus no donor analysis of 2000 patients between 15 and 55 years old, showed that an allogeneic transplant resulted in better disease control compared to chemotherapy or autologous transplant. However, surprisingly, in this study the 5-year OS was significantly improved in SR patients (62% vs52%, p=0.02), while in the HR group the reduction of relapse rate was offset by a high non relapse mortality (NRM) (at 2 years 36% vs. 22 with conventional therapy) with a 5-year OS of 41% vs 35%, p=0.2.
Meta-analyses and unsolved issues
The uncertain results in evaluating the real benefit of the allogeneic transplant in HR patients has been highlighted by several meta-analyses performed over the past few years.25–27 In the most recent one, including data from 13 studies involving 2962 patients (excluding Ph+ patients), the age at transplant turned out to be again the most important prognostic factor, since an actual survival benefit was reported only for patients < 35 years of age (OR 0.79; 95% CI, 0.70–0.90) because of the higher absolute risk of NRM for older patients.28 There are several explanations for these controversial results, the most likely being that some of the analyzed trials were either numerically underpowered or gave variable definitions of “high-risk” ALL.
All in all, these controversial results highlight the fact that in adult ALL, classic prognostic factors have a limited accuracy,2,3,6,12,29 since a significant proportion of SR patients (up to 40% to 50%), treated with standard chemotherapy, will eventually relapse and conversely, 20% to 25% of HR patients will not relapse even in the absence of an alloHSCT.1,7,16,17,30
Minimal residual disease
In addition to the above mentioned clinical and biologic prognostic features identified at diagnosis, the most important prognostic factor remains the sensitivity to chemotherapy. This crucial factor can be evaluated by several ways which include time to achieve complete remission, time to leukemic blast cell clearance and, particularly in childhood ALL, the initial response to prednisone. However, most recently, a number of studies performed in children and adults have clearly shown how quantitative measurements of MRD at various time points during treatment provide the most accurate estimate of chemosensitivity. The definition of MRD either by immunophenotype or molecular biology, implies the ability to identify the persistence of a very low number of leukemic cells in patients otherwise considered in hematologic remission. The persistence of such MRD is an indicator of intrinsic drug resistance that can herald overt hematologic relapse.9,31–35 The persistence after ten weeks of treatment of MRD at a level exceeding 10−4 or 10−3 identifies a condition of high or very high risk, respectively, for relapse. Recently, a panel of experts summarized how to best assess MRD analysis that can be made using either real-time quantitative polymerase chain reaction (RQ-PCR) or multichannel flow cytometry,36 which is normally applicable in the vast majority of patients.5 The use of MRD has been shown to be highly promising prognostic and decisional tool during the treatment program of ALL patients. The German Multicenter Study Group for Adult ALL (GMALL), in 196 SR patients, identified different MRD groups with 3-year relapse rates ranging from 0% to 94%.33 Data from the MRC/ECOG trial35 and Northern Italy Leukemia Group (NILG)9 confirmed that MRD was the most significant risk factor for relapse, with a favorable prognosis in patients responsive to chemotherapy obtaining a MRD negativity and a poor leukemia-free survival in patients MRD positive. The GMALL group recently published the largest cohort of MRD data in adults, corroborating the evidence that the measurement of MRD allows the identification of subgroup of patients with an inadequate initial response and a high rate of relapse.37 Finally, new data from Spanish PETHEMA group showed in multivariable analysis that reduced MRD clearance was the only prognostic factor for an unfavorable DFS and OS.38
Table 2 summarizes the association between MRD status and clinical outcomes in ALL patients, reporting data from the larger prospective studies.
Table 2.
Prognostic impact of MRD in prospective studies of adult ALL
| Study, year (reference) | Patients | MRD method | MRD study (level for negativity) | Outcomes MRD negative | Outcomes MRD positive |
|---|---|---|---|---|---|
| Bassan, R 2009 (13) | 280 adult ALL patients | RQ-PCR | MRD≤10−4 | 5-year OS 75% 5-year DFS 72% |
5-year OS 33% 5-year DFS 14% |
| Gökbuget, N 2012 (37) | 580 Ph- adult ALL patients | RQ-PCR | MRD≤10−4 | 5-year OS 80% 5-year DFS 67% |
5-year OS 42% 5-year DFS 25% |
| Ribera, JM, 2014 (38) | 326 HR Ph- adult ALL patients | Flow cytometry | Patients with MRD< 1 × 10−3 after induction and < 5 × 10−4 after early consolidation | 5-year OS 56% 5-year DFS 51% |
5-year OS 17% 5-year DFS 0% |
MRD=minimal residual disease; DFS=disease free survival; OS= overall survival; RQ-PCR= Real-time quantitative PCR
Overall, these data provide evidence of utility of introducing MRD analysis for the identification of patients at high risk of relapse who may benefit from early transplantation, despite a morphologic remission and the absence of clinico-biological risk factors and, conversely, for the identification of a group of patients who are sensitive to chemotherapy, achieving non-detectable level of MRD, who probably do not need transplantation as consolidation therapy also when risk factors are present. The most relevant and urgent challenges into future investigations about MRD are: a) to determine the most predictive time point for the measurement and the threshold during and after treatment b) to identify the best strategy in patients with high MRD before allogeneic transplantation, such as the need of further therapy to reduce tumor load before transplant c) to demonstrate the utility and efficacy of tapering or withdrawal of immunosuppressive therapy or use of donor lymphocyte infusion (DLI) in patients in molecular relapse after transplant; d) to demonstrate the efficacy of an MRD-guided choice in avoiding the alloHSCT in HR patients with no detectable MRD.
Allogeneic transplant for patients with Philadelphia-positive (Ph+) ALL
Historically, Ph+ ALL marked the most unfavorable subgroup of adult ALL and in the pre-tyrosine kinase inhibitors (TKIs) era, the overall survival observed in unselected series of patients was less than 25% even when alloHSCT was offered whenever possible.5,39 The incorporation of TKIs in the standard ALL therapy significantly changed the outcomes of ALL, increasing the remission induction rates as well as the depth of remission,40–43 allowing an improved cure rate. Unfortunately, although almost all patients receiving single agent imatinib or dasatinib achieve a hematologic CR,44,45 it is likely that at least during the consolidation phase, TKIs should be used in combination with chemotherapy.46,47 The use of refined programs with first/second generation TKIs and chemotherapy together with alloHSCT allow up to 50% of all patients to be cured.40,48,49 A positive impact of imatinib on the clinical outcome of alloHSCT has been reported early after its therapeutic use in Ph+ ALL50 and this result has been recently confirmed by the Japanese Adult Leukemia Study Group that compared the alloHSCT outcomes between 542 patients who received imatinib before alloHSCT during the initial complete remission period (imatinib cohort) and 196 patients who did not receive imatinib (non-imatinib cohort). The 5-year OS was significantly higher in the imatinib cohort than in the non-imatinib cohort (59% vs 38%; p <0.001).51 There is little information on the efficacy of TKIs administration after alloHSCT. Recently, Pfeifer et al. compared the tolerability and efficacy of post-transplant imatinib, administered either prophylactically or following detection of MRD, showing that prophylactic imatinib significantly reduced the incidence of molecular recurrence after alloHSCT compared with MRD-triggered imatinib (40% vs 69%; P=0.046).52 Ram et al reported that imatinib, given after reduced intensity conditioning (RIC) alloHSCT conditioned with fludarabine and low dose total body irradiation (TBI), was associated with significantly reduced mortality in univariate analysis, although the effect on relapse was not statistically significant.53 Finally, data from European Society for Blood and Marrow Transplantation (EBMT) registry54 showed that the introduction of TKIs pre and post alloHSCT significantly improved outcomes of Ph+ ALL patients. Of note, in this analysis the Authors described a significant association between the use of TKIs post-transplant and a low cumulative incidence of chronic GVHD, including its extensive form. In general, the available data suggest that TKIs administration at time of induction should be considered as a mainstay treatment of Ph+ ALL patients, because it increases initial remission rates with a beneficial impact in feasibility of alloHSCT and also improves outcomes after alloHSCT, while the impact of TKIs-based therapy on long term outcome after alloHSCT remains unclear.
Impact of minimal residual disease on allogeneic transplantation
It must be kept in mind that patients undergoing allogeneic transplantation with measurable level of minimal residual disease clearly show an inferior outcome after transplant due to a significant increased risk of leukemia relapse.55–58 This implies that, whenever possible, patients selected for allogeneic transplant should be considered for newer experimental treatment strategies able to achieve such a molecular remission before the transplant is performed. Among such innovative treatments for the treatment of minimal residual disease, blinatumomab, the first member of a novel class of T cell-engaging, bispecific single-chain (BiTE) antibodies (it engages T cells for redirected lysis of CD19+ target cells) showed very encouraging results.59 The crucial prognostic role of MRD has been demonstrated also in the case of Ph+ patients for whom the effort to achieve a convincing molecular CR should be pursued. In this respect, Ponatinib (a third generation TKI) has been recently shown to overcome the pharmacologic resistance mediated by some mutations of the BCR/ABL protein such as the T315I, and achieve impressive frequency of molecular CR.60
Allogeneic transplant for relapse or refractory ALL patients
ALL is primary refractory to chemotherapy in less than 10% of the cases. According to a few large studies from MRC/ECOG 61 and LALA groups62 the salvage treatment after relapse may induce an hematologic remission in some patients but the long term outcome is usually dismal, although more intensive re-induction chemotherapy programs followed by an alloHSCT may achieve durable remissions.63 Doney et al. reported a long-term DFS of 24% for patients transplanted after achieving a second remission, and of only 9% in those transplanted with refractory disease, confirming that in most cases salvage after relapse is not feasible even with transplantation.64 In this setting the use of blinatumomab65 and other innovative drugs such as inotuzumab66 or ponatinib47 may open the door to effective rescue treatments which may significantly increase the effective role of allogeneic transplant for this unlucky group of patients.
How to Perform an Allogeneic Transplant
It is now clear that alloHSCT represents a very effective post-remission therapy with high chances of achieving a long-term disease control in patients at highest risk for relapse. Nowadays, this procedure can be performed according to remarkably different modalities encompassing the use of different conditioning regimens, as well as different donors and stem cell source.
Which is the Optimal Transplant Regimen?
Myeloablative conditioning (MAC)
Myeloablative conditioning regimens based on a combination of cyclophosphamide (Cy) (120 mg/kg) and total body irradiation (TBI), ranging from 12 up to 13.2 Gy, are still currently used as standard preparative regimens for ALL, due to the intrinsic and powerful anti-leukemic activity and the peculiar ability to eradicate leukemic cells within the central nervous system and testicles67,68 of radiotherapy. However, in order to reduce radiation related toxicities other regimens have been developed. Substituting busulfan (BU) for TBI showed comparable OS, relapse rate and DFS to the TBI regimen, but until conversion from oral to IV BU the number of serious side effects, such as hepatic veno-occlusive disease (VOD) or hemorrhagic cystitis was high.69,70 Recently, the combination regimen of IV BU/Cy in CR1 patients showed a 3 year OS of 66% with a relapse rate of 40% and a decreased transplant related mortality (TRM).71 The group at the City of Hope National Medical Center evaluated the substitution of Cy with etoposide (VP-16) in combination with fractioned TBI (13.2 Gy) reporting a significant activity also in patients with advanced ALL with a DFS of 57% and a relapse rate of 32%.72 These interesting results were confirmed in a subsequent trial conducted by Southwest Oncology Group.73 Finally, Marks et al. recently published a comparative study of TBI combined with either Cy or VP-16.74 In this study 4 groups were compared based on the radiation dose: Cy-TBI<13Gy, Cy-TBI>13Gy, VP-16-TBI <13Gy and VP-16-TBI >13Gy. No difference in OS, DFS and TRM was observed by conditioning regimen in CR1 patients, while an advantage in substituting VP-16 for Cy or, when Cy is used, in increasing the TBI dose > 13 Gy was reported for patients in CR2.74
In conclusion, the standard MAC are regimens based on TBI combined with Cy or VP-16, although to avoid TBI toxicities, the use of a regimen containing IV BU and Cy is considered a valid a safe alternative. Based on EBMT registry data,71 the use of regimens using IV BU is increasing.
Reduced intensity conditioning (RIC)
The procedure of RIC transplant has been established in acute myeloid leukemia setting, while the experience in ALL is limited with no randomized trial comparing RIC to MAC. Two large registry studies have demonstrated the feasibility and potential efficacy of RIC for ALL. The retrospective study from the EBMT75 compared the outcome of 576 adult ALL patients who received a RIC (n=127) or MAC (n=449) alloHSCT in CR. As expected, the multivariate analysis showed that RIC patients experienced a decreased risk for NRM compared to MAC (hazard ratio (HR) 1.98, p=0.0001), but a higher relapse rate (HR 0.59, p=0.03). However, in multivariate analysis, the type of conditioning regimen (RIC vs. MAC) was not significantly associated with leukemia free survival (LFS) (HR 0.84, p=0.23). Data from a second large registry of International Bone Marrow Transplant Registry (IBMTR) confirmed the feasibility of RIC with OS at 3 years of 45%.76 In keeping with registry data, other small studies, reporting single Institution experience, demonstrated RIC feasible with good outcomes with OS over 50% and TRM between 10 and 20%.53,77–79 Of note, in patients transplanted in CR2, or not in remission RIC regimen seems to have a limited benefit.53,80
In conclusion, even if these results did not allow definitive conclusions, due to the absence of randomized clinical trial comparing RIC vs MAC, they suggest that RIC could be a reasonable therapeutic option for ALL patients not eligible for MAC.
Is there Evidence about the Optimal Donor Cell Source?
Matched related donors are the ideal choice for alloHSCT due to lower incidence and severity of GVHD, but only about 30% of patients who need a transplant have an identical sibling donor. Advances in high-resolution human leukocyte antigen (HLA) typing and improvements in GVHD prophylaxis have made possible the use of alternative donor sources of stem cells, including matched unrelated, cord blood and haploidentical donor. According to a retrospective analysis of the IBMTR registry in 672 ALL patients a similar incidence of relapse and NRM after alloHSCT from matched unrelated donor (MUD) and matched related was observed with an OS approximately of 50% at 5 years.81 Recent retrospective studies comparing unrelated with sibling donors confirmed comparable outcomes: Kiehl et al. reported no significant difference in 5 years DFS in 221 patients in CR1 who underwent MUD vs sibling donor transplant (45% vs 42%, respectively)82 and a larger study of 1139 patients83 showed no significant difference between related and unrelated alloHSCT (at 4 years OS 65% vs 62% in related vs unrelated, respectively p=0.19).
For patients without MUD donors, the use of unrelated cord blood (UCB) and haploidentical donor are under clinical investigations. According to IBMTR registry data of 150 UCB transplants, of which 45 in patients with ALL, OS was 26% in UCB compared to 35% in MUD, with a higher TRM.84 The EBMT and eurocord data showed similar results between UCB group (including 53 patients with ALL of 98) and MUD group (including 267 ALL patients of 584) in terms of OS, NRM and relapse rate.85 Several recent small studies confirmed encouraging results with the use of UCB reporting no significant difference in OS and DFS between patients who underwent a UCB vs MUD transplantation.86–88 Finally, a very recent study comparing outcomes of 116 UCB transplants with 686 unrelated adult donor found that the survival of UCB graft recipients at 3 years (44%) was similar to that of recipients of matched or mismatched unrelated adult donor grafts (44% and 43%, respectively).89 The use of haploidentical HSCT should be still considered an experimental procedure. Early results obtained with an ex vivo T cell depletion approach showed dismal results.90 More recently, and in a pediatric setting, more attractive results have been reported and it is tempting to speculate that the different laboratory procedures for ex vivo T cell depletion or the use of post-transplantation cyclophosphamide may be responsible for these better results.91–93
In general, the results of the above discussed studies demonstrate the feasibility of alloHSCT from alternative source of stem cells and, in particular, the use of UCB should be considered a valid alternative source of stem cells for adults with ALL in the absence of an identical sibling donor or MUD. However, further studies specifically designed to test prospectively whether or not alternative cell sources are effective and safe for adult ALL need to be developed.
Conclusions
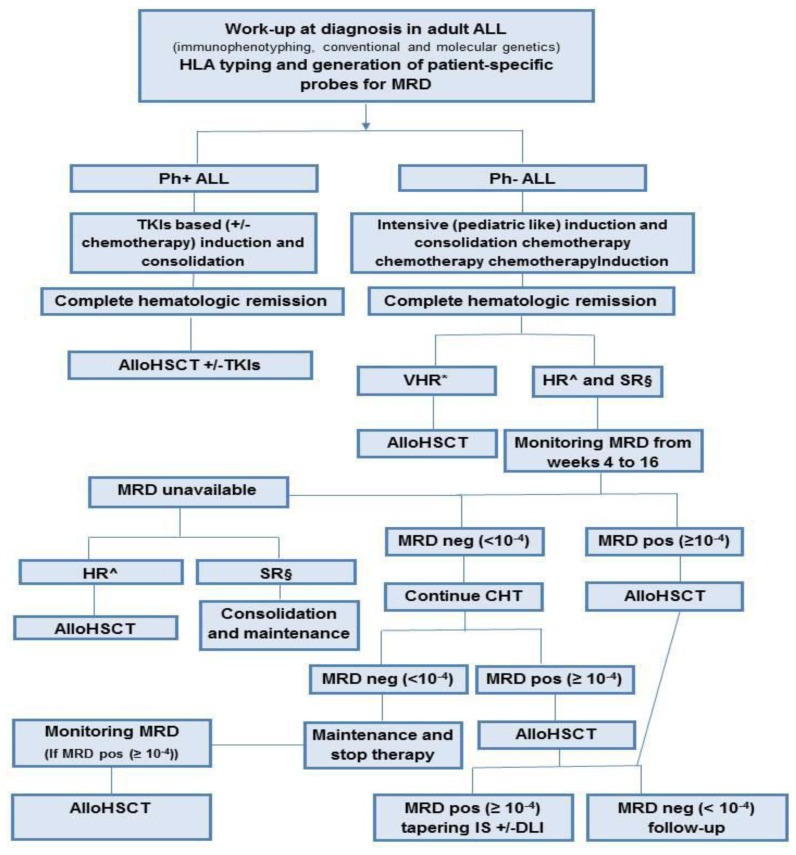
Adult ALL is a heterogeneous disease for which alloHSCT is an effective consolidation therapy. The non-relapse mortality of alloHSCT remains significantly high compared with that of conventional chemotherapy, thus, one of the main challenges in the care of ALL is to establish a more precise prognostic definition for selection of patients at higher risk for relapse to make better therapeutic decisions. In this context, a risk-adapted strategy is critical and the use of MRD has shown promising results in establishing more precise prognostic definitions of patients at highest risk for relapse. MRD status must be considered also after alloHSCT for deciding additional treatments to prevent relapse. In Ph+ ALL the introduction of TKI pre and post alloHSCT appears to significantly improve outcomes and, in the absence of specifically designed clinical trials, it remains the most effective post-reemission therapy for this HR ALL. An appropriate timing for alloHSCT is crucial to obtain better results, given that the prognosis of relapsed ALL is very poor and the possibility of achieving CR2 is uncertain. Thus, in most patients HLA typing should be performed at diagnosis for considering transplant options early during the treatment. The development of RIC regimens and the possibility of using alternative sources of stem cells, such as MUD and UCB grafts, facilitate the possibility of transplant in a wider range of patients including those without a family donor and also elderly patients and those with comorbid conditions. Balancing the risks of relapse rate against the potential adverse effects of alloHSCT, in Figure 1 we summarized our suggestions for treatment of adult ALL. As discussed in the review, our strategy was derived also from observational databases and from small retrospective single Institution experience and is therefore subject to debate. Further prospective clinical studies are needed to obtain definitive and reliable data and, considering the low incidence of ALL in adults; these efforts should probably be made within collaborative multicenter studies.
Figure 1.
Summary of our suggestions for the treatment of adult acute lymphoblastic leukemia.
ALL=acute lymphoblastic leukemia; HLA=human leukocyte antigen; MRD=minimal residual disease; Ph+=Philadelphia-positive; Ph-=Philadelphia-negative; TKIs=tyrosine kinase inhibitors; alloHSCT= allogeneic stem cell transplantation; CHT=chemotherapy; IS= immunosuppressive; DLI= donor lymphocyte infusion.
* VHR (very high risk)= cytogenetics (t(4;11), t(8;14), t(1;19), abn 11q23, +8, −7, del6q, low hypodiploidy with 30–39 chromosomes, near triploidy with 60–78 chromosomes, complex with ≥5 unrelated anomalies); molecular genetics (KMT2A rearrangements, BCR-ABL1-like ALL (CLRF2/JAK mutations), IKZF1 deletion (B-ALL); wild-type NOTCH1/FXBW7, altered RAS/PTEN (T-ALL); dysfunctional apoptosis/proliferation mechanisms (p53, Caspases, MYC); MRD>10−3
^ HR (high risk)= age≥ 35 years; white blood cell > 30×109/L for B cell phenotype >100×109/L for T cell phenotype; Very immature phenotypes, such as pro-B or pro and pre T phenotypes and mature-T (European Group for Immunophenotyping of Leukemias BI and TI/TII/TIV); late complete remission; minimal residual disease MRD> 10−4
§ SR (standard risk): none of the indicated risk factors
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Thomas X, Boiron JM, Huguet F, Dombret H, Bradstock K, Vey N, Kovacsovics T, Delannoy A, Fegueux N, Fenaux P, Stamatoullas A, Vernant JP, Tournilhac O, Buzyn A, Reman O, Charrin C, Boucheix C, Gabert J, Lheritier V, Fiere D. Outcome of treatment in adults with acute lymphoblastic leukemia: analysis of the LALA-94 trial. J Clin Oncol. 2004;22:4075–4086. doi: 10.1200/JCO.2004.10.050. [DOI] [PubMed] [Google Scholar]
- 2.Kantarjian H, Thomas D, O’Brien S, Cortes J, Giles F, Jeha S, Bueso-Ramos CE, Pierce S, Shan J, Koller C, Beran M, Keating M, Freireich EJ. Long-term follow-up results of hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (Hyper-CVAD), a dose-intensive regimen, in adult acute lymphocytic leukemia. Cancer. 2004;101:2788–2801. doi: 10.1002/cncr.20668. [DOI] [PubMed] [Google Scholar]
- 3.Gokbuget N, Hoelzer D, Arnold R, Bohme A, Bartram CR, Freund M, Ganser A, Kneba M, Langer W, Lipp T, Ludwig WD, Maschmeyer G, Rieder H, Thiel E, Weiss A, Messerer D. Treatment of Adult ALL according to protocols of the German Multicenter Study Group for Adult ALL (GMALL) Hematol Oncol Clin North Am. 2000;14:1307–1325. doi: 10.1016/S0889-8588(05)70188-X. [DOI] [PubMed] [Google Scholar]
- 4.Rowe JM, Buck G, Burnett AK, Chopra R, Wiernik PH, Richards SM, Lazarus HM, Franklin IM, Litzow MR, Ciobanu N, Prentice HG, Durrant J, Tallman MS, Goldstone AH. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood. 2005;106:3760–3767. doi: 10.1182/blood-2005-04-1623. [DOI] [PubMed] [Google Scholar]
- 5.Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532–543. doi: 10.1200/JCO.2010.30.1382. [DOI] [PubMed] [Google Scholar]
- 6.Hoelzer D, Thiel E, Loffler H, Buchner T, Ganser A, Heil G, Koch P, Freund M, Diedrich H, Ruhl H, et al. Prognostic factors in a multicenter study for treatment of acute lymphoblastic leukemia in adults. Blood. 1988;71:123–131. [PubMed] [Google Scholar]
- 7.Goldstone AH, Richards SM, Lazarus HM, Tallman MS, Buck G, Fielding AK, Burnett AK, Chopra R, Wiernik PH, Foroni L, Paietta E, Litzow MR, Marks DI, Durrant J, McMillan A, Franklin IM, Luger S, Ciobanu N, Rowe JM. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993) Blood. 2008;111:1827–1833. doi: 10.1182/blood-2007-10-116582. [DOI] [PubMed] [Google Scholar]
- 8.Huguet F, Leguay T, Raffoux E, Thomas X, Beldjord K, Delabesse E, Chevallier P, Buzyn A, Delannoy A, Chalandon Y, Vernant JP, Lafage-Pochitaloff M, Chassevent A, Lheritier V, Macintyre E, Bene MC, Ifrah N, Dombret H. Pediatric-inspired therapy in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia: the GRAALL-2003 study. J Clin Oncol. 2009;27:911–918. doi: 10.1200/JCO.2008.18.6916. [DOI] [PubMed] [Google Scholar]
- 9.Bassan R, Spinelli O, Oldani E, Intermesoli T, Tosi M, Peruta B, Rossi G, Borlenghi E, Pogliani EM, Terruzzi E, Fabris P, Cassibba V, Lambertenghi-Deliliers G, Cortelezzi A, Bosi A, Gianfaldoni G, Ciceri F, Bernardi M, Gallamini A, Mattei D, Di Bona E, Romani C, Scattolin AM, Barbui T, Rambaldi A. Improved risk classification for risk-specific therapy based on the molecular study of minimal residual disease (MRD) in adult acute lymphoblastic leukemia (ALL) Blood. 2009;113:4153–4162. doi: 10.1182/blood-2008-11-185132. [DOI] [PubMed] [Google Scholar]
- 10.Maury S, Huguet F, Leguay T, Lacombe F, Maynadie M, Girard S, de Labarthe A, Kuhlein E, Raffoux E, Thomas X, Chevallier P, Buzyn A, Delannoy A, Chalandon Y, Vernant JP, Rousselot P, Macintyre E, Ifrah N, Dombret H, Bene MC. Adverse prognostic significance of CD20 expression in adults with Philadelphia chromosome-negative B-cell precursor acute lymphoblastic leukemia. Haematologica. 2010;95:324–328. doi: 10.3324/haematol.2009.010306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marks DI, Paietta EM, Moorman AV, Richards SM, Buck G, DeWald G, Ferrando A, Fielding AK, Goldstone AH, Ketterling RP, Litzow MR, Luger SM, McMillan AK, Mansour MR, Rowe JM, Tallman MS, Lazarus HM. T-cell acute lymphoblastic leukemia in adults: clinical features, immunophenotype, cytogenetics, and outcome from the large randomized prospective trial (UKALL XII/ECOG 2993) Blood. 2009;114:5136–5145. doi: 10.1182/blood-2009-08-231217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moorman AV, Harrison CJ, Buck GA, Richards SM, Secker-Walker LM, Martineau M, Vance GH, Cherry AM, Higgins RR, Fielding AK, Foroni L, Paietta E, Tallman MS, Litzow MR, Wiernik PH, Rowe JM, Goldstone AH, Dewald GW. Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood. 2007;109:3189–3197. doi: 10.1182/blood-2006-10-051912. [DOI] [PubMed] [Google Scholar]
- 13.Rowe JM. Prognostic factors in adult acute lymphoblastic leukaemia. Br J Haematol. 2010;150:389–405. doi: 10.1111/j.1365-2141.2010.08246.x. [DOI] [PubMed] [Google Scholar]
- 14.Pui CH, Evans WE. Acute lymphoblastic leukemia. N Engl J Med. 1998;339:605–615. doi: 10.1056/NEJM199808273390907. [DOI] [PubMed] [Google Scholar]
- 15.Takeuchi J, Kyo T, Naito K, Sao H, Takahashi M, Miyawaki S, Kuriyama K, Ohtake S, Yagasaki F, Murakami H, Asou N, Ino T, Okamoto T, Usui N, Nishimura M, Shinagawa K, Fukushima T, Taguchi H, Morii T, Mizuta S, Akiyama H, Nakamura Y, Ohshima T, Ohno R. Induction therapy by frequent administration of doxorubicin with four other drugs, followed by intensive consolidation and maintenance therapy for adult acute lymphoblastic leukemia: the JALSG-ALL93 study. Leukemia. 2002;16:1259–1266. doi: 10.1038/sj.leu.2402526. [DOI] [PubMed] [Google Scholar]
- 16.Hunault M, Harousseau JL, Delain M, Truchan-Graczyk M, Cahn JY, Witz F, Lamy T, Pignon B, Jouet JP, Garidi R, Caillot D, Berthou C, Guyotat D, Sadoun A, Sotto JJ, Lioure B, Casassus P, Solal-Celigny P, Stalnikiewicz L, Audhuy B, Blanchet O, Baranger L, Bene MC, Ifrah N. Better outcome of adult acute lymphoblastic leukemia after early genoidentical allogeneic bone marrow transplantation (BMT) than after late high-dose therapy and autologous BMT: a GOELAMS trial. Blood. 2004;104:3028–3037. doi: 10.1182/blood-2003-10-3560. [DOI] [PubMed] [Google Scholar]
- 17.Ribera JM, Oriol A, Bethencourt C, Parody R, Hernandez-Rivas JM, Moreno MJ, del Potro E, Torm M, Rivas C, Besalduch J, Sanz MA, Ortega JJ. Comparison of intensive chemotherapy, allogeneic or autologous stem cell transplantation as post-remission treatment for adult patients with high-risk acute lymphoblastic leukemia. Results of the PETHEMA ALL-93 trial. Haematologica. 2005;90:1346–1356. [PubMed] [Google Scholar]
- 18.Sebban C, Lepage E, Vernant JP, Gluckman E, Attal M, Reiffers J, Sutton L, Racadot E, Michallet M, Maraninchi D, et al. Allogeneic bone marrow transplantation in adult acute lymphoblastic leukemia in first complete remission: a comparative study. French Group of Therapy of Adult Acute Lymphoblastic Leukemia. J Clin Oncol. 1994;12:2580–2587. doi: 10.1200/JCO.1994.12.12.2580. [DOI] [PubMed] [Google Scholar]
- 19.Attal M, Blaise D, Marit G, Payen C, Michallet M, Vernant JP, Sauvage C, Troussard X, Nedellec G, Pico J, et al. Consolidation treatment of adult acute lymphoblastic leukemia: a prospective, randomized trial comparing allogeneic versus autologous bone marrow transplantation and testing the impact of recombinant interleukin-2 after autologous bone marrow transplantation. BGMT Group. Blood. 1995;86:1619–1628. [PubMed] [Google Scholar]
- 20.Doney K, Fisher LD, Appelbaum FR, Buckner CD, Storb R, Singer J, Fefer A, Anasetti C, Beatty P, Bensinger W, et al. Treatment of adult acute lymphoblastic leukemia with allogeneic bone marrow transplantation. Multivariate analysis of factors affecting acute graft-versus-host disease, relapse, and relapse-free survival. Bone Marrow Transplant. 1991;7:453–459. [PubMed] [Google Scholar]
- 21.Blume KG, Forman SJ, Snyder DS, Nademanee AP, O’Donnell MR, Fahey JL, Krance RA, Sniecinski IJ, Stock AD, Findley DO, et al. Allogeneic bone marrow transplantation for acute lymphoblastic leukemia during first complete remission. Transplantation. 1987;43:389–392. doi: 10.1097/00007890-198703000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Chao NJ, Forman SJ, Schmidt GM, Snyder DS, Amylon MD, Konrad PN, Nademanee AP, O’Donnell MR, Parker PM, Stein AS, et al. Allogeneic bone marrow transplantation for high-risk acute lymphoblastic leukemia during first complete remission. Blood. 1991;78:1923–1927. [PubMed] [Google Scholar]
- 23.Jamieson CH, Amylon MD, Wong RM, Blume KG. Allogeneic hematopoietic cell transplantation for patients with high-risk acute lymphoblastic leukemia in first or second complete remission using fractionated total-body irradiation and high-dose etoposide: a 15-year experience. Exp Hematol. 2003;31:981–986. doi: 10.1016/S0301-472X(03)00231-5. [DOI] [PubMed] [Google Scholar]
- 24.Labar B, Suciu S, Zittoun R, Muus P, Marie JP, Fillet G, Peetermans M, Stryckmans P, Willemze R, Feremans W, Jaksic B, Bourhis JH, Burghouts JP, de Witte T. Allogeneic stem cell transplantation in acute lymphoblastic leukemia and non-Hodgkin’s lymphoma for patients <or=50 years old in first complete remission: results of the EORTC ALL-3 trial. Haematologica. 2004;89:809–817. [PubMed] [Google Scholar]
- 25.Yanada M, Matsuo K, Suzuki T, Naoe T. Allogeneic hematopoietic stem cell transplantation as part of postremission therapy improves survival for adult patients with high-risk acute lymphoblastic leukemia: a metaanalysis. Cancer. 2006;106:2657–2663. doi: 10.1002/cncr.21932. [DOI] [PubMed] [Google Scholar]
- 26.Ram R, Gafter-Gvili A, Vidal L, Paul M, Ben-Bassat I, Shpilberg O, Raanani P. Management of adult patients with acute lymphoblastic leukemia in first complete remission: systematic review and meta-analysis. Cancer. 2010;116:3447–3457. doi: 10.1002/cncr.25136. [DOI] [PubMed] [Google Scholar]
- 27.Pidala J, Djulbegovic B, Anasetti C, Kharfan-Dabaja M, Kumar A. Allogeneic hematopoietic cell transplantation for adult acute lymphoblastic leukemia (ALL) in first complete remission. Cochrane Database Syst Rev. 2011:CD008818. doi: 10.1002/14651858.CD008818.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta V, Richards S, Rowe J. Allogeneic, but not autologous, hematopoietic cell transplantation improves survival only among younger adults with acute lymphoblastic leukemia in first remission: an individual patient data meta-analysis. Blood. 2013;121:339–350. doi: 10.1182/blood-2012-07-445098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mancini M, Scappaticci D, Cimino G, Nanni M, Derme V, Elia L, Tafuri A, Vignetti M, Vitale A, Cuneo A, Castoldi G, Saglio G, Pane F, Mecucci C, Camera A, Specchia G, Tedeschi A, Di Raimondo F, Fioritoni G, Fabbiano F, Marmont F, Ferrara F, Cascavilla N, Todeschini G, Nobile F, Kropp MG, Leoni P, Tabilio A, Luppi M, Annino L, Mandelli F, Foa R. A comprehensive genetic classification of adult acute lymphoblastic leukemia (ALL): analysis of the GIMEMA 0496 protocol. Blood. 2005;105:3434–3441. doi: 10.1182/blood-2004-07-2922. [DOI] [PubMed] [Google Scholar]
- 30.Bassan R, Pogliani E, Casula P, Rossi G, Fabris P, Morandi S, Lambertenghi-Deliliers G, Vespignani M, Lerede T, Rambaldi A, Borleri G, Spedini P, Cortelezzi A, Izzi T, Coser P, Broccia G, Corneo G, Barbui T. Risk-oriented postremission strategies in adult acute lymphoblastic leukemia: prospective confirmation of anthracycline activity in standard-risk class and role of hematopoietic stem cell transplants in high-risk groups. Hematol J. 2001;2:117–126. doi: 10.1038/sj.thj.6200091. [DOI] [PubMed] [Google Scholar]
- 31.Cave H, van der Werff ten Bosch J, Suciu S, Guidal C, Waterkeyn C, Otten J, Bakkus M, Thielemans K, Grandchamp B, Vilmer E. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer--Childhood Leukemia Cooperative Group. N Engl J Med. 1998;339:591–598. doi: 10.1056/NEJM199808273390904. [DOI] [PubMed] [Google Scholar]
- 32.van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L, Stolz F, Schrappe M, Masera G, Kamps WA, Gadner H, van Wering ER, Ludwig WD, Basso G, de Bruijn MA, Cazzaniga G, Hettinger K, van der Does-van den Berg A, Hop WC, Riehm H, Bartram CR. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet. 1998;352:1731–1738. doi: 10.1016/S0140-6736(98)04058-6. [DOI] [PubMed] [Google Scholar]
- 33.Bruggemann M, Raff T, Flohr T, Gokbuget N, Nakao M, Droese J, Luschen S, Pott C, Ritgen M, Scheuring U, Horst HA, Thiel E, Hoelzer D, Bartram CR, Kneba M. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood. 2006;107:1116–1123. doi: 10.1182/blood-2005-07-2708. [DOI] [PubMed] [Google Scholar]
- 34.Holowiecki J, Krawczyk-Kulis M, Giebel S, Jagoda K, Stella-Holowiecka B, Piatkowska-Jakubas B, Paluszewska M, Seferynska I, Lewandowski K, Kielbinski M, Czyz A, Balana-Nowak A, Krol M, Skotnicki AB, Jedrzejczak WW, Warzocha K, Lange A, Hellmann A. Status of minimal residual disease after induction predicts outcome in both standard and high-risk Ph-negative adult acute lymphoblastic leukaemia. The Polish Adult Leukemia Group ALL 4-2002 MRD Study. Br J Haematol. 2008;142:227–237. doi: 10.1111/j.1365-2141.2008.07185.x. [DOI] [PubMed] [Google Scholar]
- 35.Patel B, Rai L, Buck G, Richards SM, Mortuza Y, Mitchell W, Gerrard G, Moorman AV, Duke V, Hoffbrand AV, Fielding AK, Goldstone AH, Foroni L. Minimal residual disease is a significant predictor of treatment failure in non T-lineage adult acute lymphoblastic leukaemia: final results of the international trial UKALL XII/ECOG2993. Br J Haematol. 2010;148:80–89. doi: 10.1111/j.1365-2141.2009.07941.x. [DOI] [PubMed] [Google Scholar]
- 36.Bruggemann M, Schrauder A, Raff T, Pfeifer H, Dworzak M, Ottmann OG, Asnafi V, Baruchel A, Bassan R, Benoit Y, Biondi A, Cave H, Dombret H, Fielding AK, Foa R, Gokbuget N, Goldstone AH, Goulden N, Henze G, Hoelzer D, Janka-Schaub GE, Macintyre EA, Pieters R, Rambaldi A, Ribera JM, Schmiegelow K, Spinelli O, Stary J, von Stackelberg A, Kneba M, Schrappe M, van Dongen JJ. Standardized MRD quantification in European ALL trials: proceedings of the Second International Symposium on MRD assessment in Kiel, Germany, 18–20 September 2008. Leukemia. 2010;24:521–535. doi: 10.1038/leu.2009.268. [DOI] [PubMed] [Google Scholar]
- 37.Gokbuget N, Kneba M, Raff T, Trautmann H, Bartram CR, Arnold R, Fietkau R, Freund M, Ganser A, Ludwig WD, Maschmeyer G, Rieder H, Schwartz S, Serve H, Thiel E, Bruggemann M, Hoelzer D. Adult patients with acute lymphoblastic leukemia and molecular failure display a poor prognosis and are candidates for stem cell transplantation and targeted therapies. Blood. 2012;120:1868–1876. doi: 10.1182/blood-2011-09-377713. [DOI] [PubMed] [Google Scholar]
- 38.Ribera JM, Oriol A, Morgades M, Montesinos P, Sarra J, Gonzalez-Campos J, Brunet S, Tormo M, Fernandez-Abellan P, Guardia R, Bernal MT, Esteve J, Barba P, Moreno MJ, Bermudez A, Cladera A, Escoda L, Garcia-Boyero R, Del Potro E, Bergua J, Amigo ML, Grande C, Rabunal MJ, Hernandez-Rivas JM, Feliu E. Treatment of High-Risk Philadelphia Chromosome-Negative Acute Lymphoblastic Leukemia in Adolescents and Adults According to Early Cytologic Response and Minimal Residual Disease After Consolidation Assessed by Flow Cytometry: Final Results of the PETHEMA ALL-AR-03 Trial. J Clin Oncol. 2014;32:1595–1604. doi: 10.1200/JCO.2013.52.2425. [DOI] [PubMed] [Google Scholar]
- 39.Fielding AK, Rowe JM, Richards SM, Buck G, Moorman AV, Durrant IJ, Marks DI, McMillan AK, Litzow MR, Lazarus HM, Foroni L, Dewald G, Franklin IM, Luger SM, Paietta E, Wiernik PH, Tallman MS, Goldstone AH. Prospective outcome data on 267 unselected adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia confirms superiority of allogeneic transplantation over chemotherapy in the pre-imatinib era: results from the International ALL Trial MRC UKALLXII/ECOG2993. Blood. 2009;113:4489–4496. doi: 10.1182/blood-2009-01-199380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomas DA, Faderl S, Cortes J, O’Brien S, Giles FJ, Kornblau SM, Garcia-Manero G, Keating MJ, Andreeff M, Jeha S, Beran M, Verstovsek S, Pierce S, Letvak L, Salvado A, Champlin R, Talpaz M, Kantarjian H. Treatment of Philadelphia chromosome-positive acute lymphocytic leukemia with hyper-CVAD and imatinib mesylate. Blood. 2004;103:4396–4407. doi: 10.1182/blood-2003-08-2958. [DOI] [PubMed] [Google Scholar]
- 41.Ravandi F, Jorgensen JL, Thomas DA, O’Brien S, Garris R, Faderl S, Huang X, Wen S, Burger JA, Ferrajoli A, Kebriaei P, Champlin RE, Estrov Z, Challagundla P, Wang SA, Luthra R, Cortes JE, Kantarjian HM. Detection of MRD may predict the outcome of patients with Philadelphia chromosome-positive ALL treated with tyrosine kinase inhibitors plus chemotherapy. Blood. 2013;122:1214–1221. doi: 10.1182/blood-2012-11-466482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bassan R, Rossi G, Pogliani EM, Di Bona E, Angelucci E, Cavattoni I, Lambertenghi-Deliliers G, Mannelli F, Levis A, Ciceri F, Mattei D, Borlenghi E, Terruzzi E, Borghero C, Romani C, Spinelli O, Tosi M, Oldani E, Intermesoli T, Rambaldi A. Chemotherapy-phased imatinib pulses improve long-term outcome of adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia: Northern Italy Leukemia Group protocol 09/00. J Clin Oncol. 2010;28:3644–3652. doi: 10.1200/JCO.2010.28.1287. [DOI] [PubMed] [Google Scholar]
- 43.Fielding AK, Rowe JM, Buck G, Foroni L, Gerrard G, Litzow MR, Lazarus H, Luger SM, Marks DI, McMillan AK, Moorman AV, Patel B, Paietta E, Tallman MS, Goldstone AH. UKALLXII/ECOG2993: addition of imatinib to a standard treatment regimen enhances long-term outcomes in Philadelphia positive acute lymphoblastic leukemia. Blood. 2014;123:843–850. doi: 10.1182/blood-2013-09-529008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vignetti M, Fazi P, Cimino G, Martinelli G, Di Raimondo F, Ferrara F, Meloni G, Ambrosetti A, Quarta G, Pagano L, Rege-Cambrin G, Elia L, Bertieri R, Annino L, Foa R, Baccarani M, Mandelli F. Imatinib plus steroids induces complete remissions and prolonged survival in elderly Philadelphia chromosome-positive patients with acute lymphoblastic leukemia without additional chemotherapy: results of the Gruppo Italiano Malattie Ematologiche dell’Adulto (GIMEMA) LAL0201-B protocol. Blood. 2007;109:3676–3678. doi: 10.1182/blood-2006-10-052746. [DOI] [PubMed] [Google Scholar]
- 45.Foa R, Vitale A, Vignetti M, Meloni G, Guarini A, De Propris MS, Elia L, Paoloni F, Fazi P, Cimino G, Nobile F, Ferrara F, Castagnola C, Sica S, Leoni P, Zuffa E, Fozza C, Luppi M, Candoni A, Iacobucci I, Soverini S, Mandelli F, Martinelli G, Baccarani M. Dasatinib as first-line treatment for adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood. 2011;118:6521–6528. doi: 10.1182/blood-2011-05-351403. [DOI] [PubMed] [Google Scholar]
- 46.Ottmann O, Dombret H, Martinelli G, Simonsson B, Guilhot F, Larson RA, Rege-Cambrin G, Radich J, Hochhaus A, Apanovitch AM, Gollerkeri A, Coutre S. Dasatinib induces rapid hematologic and cytogenetic responses in adult patients with Philadelphia chromosome positive acute lymphoblastic leukemia with resistance or intolerance to imatinib: interim results of a phase 2 study. Blood. 2007;110:2309–2315. doi: 10.1182/blood-2007-02-073528. [DOI] [PubMed] [Google Scholar]
- 47.Cortes JE, Talpaz M, Kantarjian H. Ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med. 2014;370:577. doi: 10.1056/NEJMc1315234. [DOI] [PubMed] [Google Scholar]
- 48.de Labarthe A, Rousselot P, Huguet-Rigal F, Delabesse E, Witz F, Maury S, Rea D, Cayuela JM, Vekemans MC, Reman O, Buzyn A, Pigneux A, Escoffre M, Chalandon Y, MacIntyre E, Lheritier V, Vernant JP, Thomas X, Ifrah N, Dombret H. Imatinib combined with induction or consolidation chemotherapy in patients with de novo Philadelphia chromosome-positive acute lymphoblastic leukemia: results of the GRAAPH-2003 study. Blood. 2007;109:1408–1413. doi: 10.1182/blood-2006-03-011908. [DOI] [PubMed] [Google Scholar]
- 49.Yanada M, Takeuchi J, Sugiura I, Akiyama H, Usui N, Yagasaki F, Kobayashi T, Ueda Y, Takeuchi M, Miyawaki S, Maruta A, Emi N, Miyazaki Y, Ohtake S, Jinnai I, Matsuo K, Naoe T, Ohno R. High complete remission rate and promising outcome by combination of imatinib and chemotherapy for newly diagnosed BCR-ABL-positive acute lymphoblastic leukemia: a phase II study by the Japan Adult Leukemia Study Group. J Clin Oncol. 2006;24:460–466. doi: 10.1200/JCO.2005.03.2177. [DOI] [PubMed] [Google Scholar]
- 50.Lee S, Kim YJ, Min CK, Kim HJ, Eom KS, Kim DW, Lee JW, Min WS, Kim CC. The effect of first-line imatinib interim therapy on the outcome of allogeneic stem cell transplantation in adults with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood. 2005;105:3449–3457. doi: 10.1182/blood-2004-09-3785. [DOI] [PubMed] [Google Scholar]
- 51.Mizuta S, Matsuo K, Nishiwaki S, Imai K, Kanamori H, Ohashi K, Fukuda T, Onishi Y, Miyamura K, Takahashi S, Onizuka M, Atsuta Y, Suzuki R, Morishima Y, Kato K, Sakamaki H, Tanaka J. Pretransplant administration of imatinib for allo-HSCT in patients with BCR-ABL-positive acute lymphoblastic leukemia. Blood. 2014;123:2325–2332. doi: 10.1182/blood-2013-11-538728. [DOI] [PubMed] [Google Scholar]
- 52.Pfeifer H, Wassmann B, Bethge W, Dengler J, Bornhauser M, Stadler M, Beelen D, Vucinic V, Burmeister T, Stelljes M, Faul C, Dreger P, Kiani A, Schafer-Eckart K, Schwerdtfeger R, Lange E, Kubuschok B, Horst HA, Gramatzki M, Bruck P, Serve H, Hoelzer D, Gokbuget N, Ottmann OG. Randomized comparison of prophylactic and minimal residual disease-triggered imatinib after allogeneic stem cell transplantation for BCR-ABL1-positive acute lymphoblastic leukemia. Leukemia. 2013;27:1254–1262. doi: 10.1038/leu.2012.352. [DOI] [PubMed] [Google Scholar]
- 53.Ram R, Storb R, Sandmaier BM, Maloney DG, Woolfrey A, Flowers ME, Maris MB, Laport GG, Chauncey TR, Lange T, Langston AA, Storer B, Georges GE. Non-myeloablative conditioning with allogeneic hematopoietic cell transplantation for the treatment of high-risk acute lymphoblastic leukemia. Haematologica. 2011;96:1113–1120. doi: 10.3324/haematol.2011.040261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brissot M, Labopin M, Beckers G, Socie L, Volin A, Rambaldi J, Finke S, Lenhoff N, Kröger G, Ossenkopple C, Craddock I, Yakoub-Agha G, Gurman N, Russell V, Koza J, Cornelissen J, Esteve, Mohty M. Tyrosine kinase inhibitors (TKIs) improve outcome of allogeneic haematopoietic stem cell transplantation (allo-HCST) for Philadelphia chromosome acute lymphoblastic leukaemia (Ph+ALL) in first complete remission (CR1): a study from the ALWP of EBMT. Bone Marrow Transplant. 2013;48:S2. [Google Scholar]
- 55.Spinelli O, Peruta B, Tosi M, Guerini V, Salvi A, Zanotti MC, Oldani E, Grassi A, Intermesoli T, Mico C, Rossi G, Fabris P, Lambertenghi-Deliliers G, Angelucci E, Barbui T, Bassan R, Rambaldi A. Clearance of minimal residual disease after allogeneic stem cell transplantation and the prediction of the clinical outcome of adult patients with high-risk acute lymphoblastic leukemia. Haematologica. 2007;92:612–618. doi: 10.3324/haematol.10965. [DOI] [PubMed] [Google Scholar]
- 56.Sramkova L, Muzikova K, Fronkova E, Krejci O, Sedlacek P, Formankova R, Mejstrikova E, Stary J, Trka J. Detectable minimal residual disease before allogeneic hematopoietic stem cell transplantation predicts extremely poor prognosis in children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2007;48:93–100. doi: 10.1002/pbc.20794. [DOI] [PubMed] [Google Scholar]
- 57.Bar M, Wood BL, Radich JP, Doney KC, Woolfrey AE, Delaney C, Appelbaum FR, Gooley TA. Impact of Minimal Residual Disease, Detected by Flow Cytometry, on Outcome of Myeloablative Hematopoietic Cell Transplantation for Acute Lymphoblastic Leukemia. Leukemia Research and Treatment. 2014;2014 doi: 10.1155/2014/421723.. doi: 10.1155/2014/421723.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bachanova V, Burke MJ, Yohe S, Cao Q, Sandhu K, Singleton TP, Brunstein CG, Wagner JE, Verneris MR, Weisdorf DJ. Unrelated Cord Blood Transplantation in Adult and Pediatric Acute Lymphoblastic Leukemia: Effect of Minimal Residual Disease on Relapse and Survival. Biology of Blood and Marrow Transplant. 2012;18:963–968. doi: 10.1016/j.bbmt.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Topp MS, Kufer P, Gokbuget N, Goebeler M, Klinger M, Neumann S, Horst HA, Raff T, Viardot A, Schmid M, Stelljes M, Schaich M, Degenhard E, Kohne-Volland R, Bruggemann M, Ottmann O, Pfeifer H, Burmeister T, Nagorsen D, Schmidt M, Lutterbuese R, Reinhardt C, Baeuerle PA, Kneba M, Einsele H, Riethmuller G, Hoelzer D, Zugmaier G, Bargou RC. Targeted therapy with the T-cell-engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic leukemia patients results in high response rate and prolonged leukemia-free survival. J Clin Oncol. 2011;29:2493–2498. doi: 10.1200/JCO.2010.32.7270. [DOI] [PubMed] [Google Scholar]
- 60.Jabbour E, Kantarjian H, Thomas D, Ravandi F, Cortes J, Hoehn D, Pemmaraju N, Kadia T, Garris R, Garcia-Manero G, Borthakur G, Wierda W, O’Brien S. Phase II study of combination of HyperCVAD with ponatinib in fron line therapy of patients (PTS) with Philadelphia chromosome (PH) positive acute lymphoblastic leukemia (ALL) Haematologica. 2014;99:S724. [Google Scholar]
- 61.Fielding AK, Richards SM, Chopra R, Lazarus HM, Litzow MR, Buck G, Durrant IJ, Luger SM, Marks DI, Franklin IM, McMillan AK, Tallman MS, Rowe JM, Goldstone AH. Outcome of 609 adults after relapse of acute lymphoblastic leukemia (ALL); an MRC UKALL12/ECOG 2993 study. Blood. 2007;109:944–950. doi: 10.1182/blood-2006-05-018192. [DOI] [PubMed] [Google Scholar]
- 62.Reman O, Buzyn A, Lheritier V, Huguet F, Kuentz M, Stamatoullas A, Delannoy A, Fegueux N, Miclea JM, Boiron JM, Vernant JP, Gardin C, Hacini M, Georges M, Fiere D, Thomas X. Rescue therapy combining intermediate-dose cytarabine with amsacrine and etoposide in relapsed adult acute lymphoblastic leukemia. Hematol J. 2004;5:123–129. doi: 10.1038/sj.thj.6200353. [DOI] [PubMed] [Google Scholar]
- 63.Kozlowski P, Astrom M, Ahlberg L, Bernell P, Hulegardh E, Hagglund H, Karlsson K, Markuszewska-Kuczymska A, Tomaszewska-Toporska B, Smedmyr B, Hallbook H. High curability via intensive reinduction chemotherapy and stem cell transplantation in young adults with relapsed acute lymphoblastic leukemia in Sweden 2003–2007. Haematologica. 2012;97:1414–1421. doi: 10.3324/haematol.2011.057851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Doney K, Hagglund H, Leisenring W, Chauncey T, Appelbaum FR, Storb R. Predictive factors for outcome of allogeneic hematopoietic cell transplantation for adult acute lymphoblastic leukemia. Biol Blood Marrow Transplant. 2003;9:472–481. doi: 10.1016/S1083-8791(03)00149-6. [DOI] [PubMed] [Google Scholar]
- 65.Topp MS, Gokbuget N, Zugmaier G, Degenhard E, Goebeler ME, Klinger M, Neumann SA, Horst HA, Raff T, Viardot A, Stelljes M, Schaich M, Kohne-Volland R, Bruggemann M, Ottmann OG, Burmeister T, Baeuerle PA, Nagorsen D, Schmidt M, Einsele H, Riethmuller G, Kneba M, Hoelzer D, Kufer P, Bargou RC. Long-term follow-up of hematologic relapse-free survival in a phase 2 study of blinatumomab in patients with MRD in B-lineage ALL. Blood. 2012;120:5185–5187. doi: 10.1182/blood-2012-07-441030. [DOI] [PubMed] [Google Scholar]
- 66.Kantarjian H, Thomas D, Jorgensen J, Kebriaei P, Jabbour E, Rytting M, York S, Ravandi F, Garris R, Kwari M, Faderl S, Cortes J, Champlin R, O’Brien S. Results of inotuzumab ozogamicin, a CD22 monoclonal antibody, in refractory and relapsed acute lymphocytic leukemia. Cancer. 2013;119:2728–2736. doi: 10.1002/cncr.28136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thomas E, Storb R, Clift RA, Fefer A, Johnson FL, Neiman PE, Lerner KG, Glucksberg H, Buckner CD. Bone-marrow transplantation (first of two parts) N Engl J Med. 1975;292:832–843. doi: 10.1056/NEJM197504172921605. [DOI] [PubMed] [Google Scholar]
- 68.Thomas ED, Storb R, Clift RA, Fefer A, Johnson L, Neiman PE, Lerner KG, Glucksberg H, Buckner CD. Bone-marrow transplantation (second of two parts) N Engl J Med. 1975;292:895–902. doi: 10.1056/NEJM197504242921706. [DOI] [PubMed] [Google Scholar]
- 69.Carreras E, Bertz H, Arcese W, Vernant JP, Tomas JF, Hagglund H, Bandini G, Esperou H, Russell J, de la Rubia J, Di Girolamo G, Demuynck H, Hartmann O, Clausen J, Ruutu T, Leblond V, Iriondo A, Bosi A, Ben-Bassat I, Koza V, Gratwohl A, Apperley JF. Incidence and outcome of hepatic veno-occlusive disease after blood or marrow transplantation: a prospective cohort study of the European Group for Blood and Marrow Transplantation. European Group for Blood and Marrow Transplantation Chronic Leukemia Working Party. Blood. 1998;92:3599–3604. [PubMed] [Google Scholar]
- 70.Shi-Xia X, Xian-Hua T, Hai-Qin X, Bo F, Xiang-Feng T. Total body irradiation plus cyclophosphamide versus busulphan with cyclophosphamide as conditioning regimen for patients with leukemia undergoing allogeneic stem cell transplantation: a meta-analysis. Leuk Lymphoma. 2010;51:50–60. doi: 10.3109/10428190903419130. [DOI] [PubMed] [Google Scholar]
- 71.Tang W, Wang L, Zhao WL, Chen YB, Shen ZX, Hu J. Intravenous busulfan-cyclophosphamide as a preparative regimen before allogeneic hematopoietic stem cell transplantation for adult patients with acute lymphoblastic leukemia. Biol Blood Marrow Transplant. 2011;17:1555–1561. doi: 10.1016/j.bbmt.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 72.Blume KG, Forman SJ, O’Donnell MR, Doroshow JH, Krance RA, Nademanee AP, Snyder DS, Schmidt GM, Fahey JL, Metter GE, et al. Total body irradiation and high-dose etoposide: a new preparatory regimen for bone marrow transplantation in patients with advanced hematologic malignancies. Blood. 1987;69:1015–1020. [PubMed] [Google Scholar]
- 73.Blume KG, Kopecky KJ, Henslee-Downey JP, Forman SJ, Stiff PJ, LeMaistre CF, Appelbaum FR. A prospective randomized comparison of total body irradiation-etoposide versus busulfan-cyclophosphamide as preparatory regimens for bone marrow transplantation in patients with leukemia who were not in first remission: a Southwest Oncology Group study. Blood. 1993;81:2187–2193. [PubMed] [Google Scholar]
- 74.Marks DI, Forman SJ, Blume KG, Perez WS, Weisdorf DJ, Keating A, Gale RP, Cairo MS, Copelan EA, Horan JT, Lazarus HM, Litzow MR, McCarthy PL, Schultz KR, Smith DD, Trigg ME, Zhang MJ, Horowitz MM. A comparison of cyclophosphamide and total body irradiation with etoposide and total body irradiation as conditioning regimens for patients undergoing sibling allografting for acute lymphoblastic leukemia in first or second complete remission. Biol Blood Marrow Transplant. 2006;12:438–453. doi: 10.1016/j.bbmt.2005.12.029. [DOI] [PubMed] [Google Scholar]
- 75.Mohty M, Labopin M, Volin L, Gratwohl A, Socie G, Esteve J, Tabrizi R, Nagler A, Rocha V. Reduced-intensity versus conventional myeloablative conditioning allogeneic stem cell transplantation for patients with acute lymphoblastic leukemia: a retrospective study from the European Group for Blood and Marrow Transplantation. Blood. 2010;116:4439–4443. doi: 10.1182/blood-2010-02-266551. [DOI] [PubMed] [Google Scholar]
- 76.Marks DI, Wang T, Perez WS, Antin JH, Copelan E, Gale RP, George B, Gupta V, Halter J, Khoury HJ, Klumpp TR, Lazarus HM, Lewis VA, McCarthy P, Rizzieri DA, Sabloff M, Szer J, Tallman MS, Weisdorf DJ. The outcome of full-intensity and reduced-intensity conditioning matched sibling or unrelated donor transplantation in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia in first and second complete remission. Blood. 2010;116:366–374. doi: 10.1182/blood-2010-01-264077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stein AS, Palmer JM, O’Donnell MR, Kogut NM, Spielberger RT, Slovak ML, Tsai NC, Senitzer D, Snyder DS, Thomas SH, Forman SJ. Reduced-intensity conditioning followed by peripheral blood stem cell transplantation for adult patients with high-risk acute lymphoblastic leukemia. Biol Blood Marrow Transplant. 2009;15:1407–1414. doi: 10.1016/j.bbmt.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cho BS, Lee S, Kim YJ, Chung NG, Eom KS, Kim HJ, Min CK, Cho SG, Kim DW, Lee JW, Min WS, Kim CC. Reduced-intensity conditioning allogeneic stem cell transplantation is a potential therapeutic approach for adults with high-risk acute lymphoblastic leukemia in remission: results of a prospective phase 2 study. Leukemia. 2009;23:1763–1770. doi: 10.1038/leu.2009.102. [DOI] [PubMed] [Google Scholar]
- 79.Bachanova V, Verneris MR, DeFor T, Brunstein CG, Weisdorf DJ. Prolonged survival in adults with acute lymphoblastic leukemia after reduced-intensity conditioning with cord blood or sibling donor transplantation. Blood. 2009;113:2902–2905. doi: 10.1182/blood-2008-10-184093. [DOI] [PubMed] [Google Scholar]
- 80.Arnold R, Massenkeil G, Bornhauser M, Ehninger G, Beelen DW, Fauser AA, Hegenbart U, Hertenstein B, Ho AD, Knauf W, Kolb HJ, Kolbe K, Sayer HG, Schwerdtfeger R, Wandt H, Hoelzer D. Nonmyeloablative stem cell transplantation in adults with high-risk ALL may be effective in early but not in advanced disease. Leukemia. 2002;16:2423–2428. doi: 10.1038/sj.leu.2402712. [DOI] [PubMed] [Google Scholar]
- 81.Ringden O, Pavletic SZ, Anasetti C, Barrett AJ, Wang T, Wang D, Antin JH, Di Bartolomeo P, Bolwell BJ, Bredeson C, Cairo MS, Gale RP, Gupta V, Hahn T, Hale GA, Halter J, Jagasia M, Litzow MR, Locatelli F, Marks DI, McCarthy PL, Cowan MJ, Petersdorf EW, Russell JA, Schiller GJ, Schouten H, Spellman S, Verdonck LF, Wingard JR, Horowitz MM, Arora M. The graft-versus-leukemia effect using matched unrelated donors is not superior to HLA-identical siblings for hematopoietic stem cell transplantation. Blood. 2009;113:3110–3118. doi: 10.1182/blood-2008-07-163212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kiehl MG, Kraut L, Schwerdtfeger R, Hertenstein B, Remberger M, Kroeger N, Stelljes M, Bornhaeuser M, Martin H, Scheid C, Ganser A, Zander AR, Kienast J, Ehninger G, Hoelzer D, Diehl V, Fauser AA, Ringden O. Outcome of allogeneic hematopoietic stem-cell transplantation in adult patients with acute lymphoblastic leukemia: no difference in related compared with unrelated transplant in first complete remission. J Clin Oncol. 2004;22:2816–2825. doi: 10.1200/JCO.2004.07.130. [DOI] [PubMed] [Google Scholar]
- 83.Nishiwaki S, Inamoto Y, Sakamaki H, Kurokawa M, Iida H, Ogawa H, Fukuda T, Ozawa Y, Kobayashi N, Kasai M, Mori T, Iwato K, Yoshida T, Onizuka M, Kawa K, Morishima Y, Suzuki R, Atsuta Y, Miyamura K. Allogeneic stem cell transplantation for adult Philadelphia chromosome-negative acute lymphocytic leukemia: comparable survival rates but different risk factors between related and unrelated transplantation in first complete remission. Blood. 2010;116:4368–4375. doi: 10.1182/blood-2010-02-269571. [DOI] [PubMed] [Google Scholar]
- 84.Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang MJ, Champlin RE, Stevens C, Barker JN, Gale RP, Lazarus HM, Marks DI, van Rood JJ, Scaradavou A, Horowitz MM. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med. 2004;351:2265–2275. doi: 10.1056/NEJMoa041276. [DOI] [PubMed] [Google Scholar]
- 85.Rocha V, Labopin M, Sanz G, Arcese W, Schwerdtfeger R, Bosi A, Jacobsen N, Ruutu T, de Lima M, Finke J, Frassoni F, Gluckman E. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351:2276–2285. doi: 10.1056/NEJMoa041469. [DOI] [PubMed] [Google Scholar]
- 86.Tomblyn MB, Arora M, Baker KS, Blazar BR, Brunstein CG, Burns LJ, DeFor TE, Dusenbery KE, Kaufman DS, Kersey JH, MacMillan ML, McGlave PB, Miller JS, Orchard PJ, Slungaard A, Tomblyn MR, Vercellotti GM, Verneris MR, Wagner JE, Weisdorf DJ. Myeloablative hematopoietic cell transplantation for acute lymphoblastic leukemia: analysis of graft sources and long-term outcome. J Clin Oncol. 2009;27:3634–3641. doi: 10.1200/JCO.2008.20.2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferra C, Sanz J, de la Camara R, Sanz G, Bermudez A, Valcarcel D, Rovira M, Serrano D, Caballero D, Espigado I, Morgades M, Heras I, Solano C, Duarte R, Barrenetxea C, Garcia-Noblejas A, Diez-Martin JL, Iriondo A, Carreras E, Sierra J, Sanz MA, Ribera JM. Unrelated transplantation for poor-prognosis adult acute lymphoblastic leukemia: long-term outcome analysis and study of the impact of hematopoietic graft source. Biol Blood Marrow Transplant. 2010;16:957–966. doi: 10.1016/j.bbmt.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 88.Atsuta Y, Suzuki R, Nagamura-Inoue T, Taniguchi S, Takahashi S, Kai S, Sakamaki H, Kouzai Y, Kasai M, Fukuda T, Azuma H, Takanashi M, Okamoto S, Tsuchida M, Kawa K, Morishima Y, Kodera Y, Kato S. Disease-specific analyses of unrelated cord blood transplantation compared with unrelated bone marrow transplantation in adult patients with acute leukemia. Blood. 2009;113:1631–1638. doi: 10.1182/blood-2008-03-147041. [DOI] [PubMed] [Google Scholar]
- 89.Marks DI, Woo KA, Zhong X, Appelbaum FR, Bachanova V, Barker JN, Brunstein CG, Gibson J, Kebriaei P, Lazarus HM, Olsson R, Perales MA, Pidala J, Savani B, Rocha V, Eapen M. Unrelated umbilical cord blood transplant for adult acute lymphoblastic leukemia in first and second complete remission: a comparison with allografts from adult unrelated donors. Haematologica. 2014;99:322–328. doi: 10.3324/haematol.2013.094193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ciceri F, Labopin M, Aversa F, Rowe JM, Bunjes D, Lewalle P, Nagler A, Di Bartolomeo P, Lacerda JF, Lupo Stanghellini MT, Polge E, Frassoni F, Martelli MF, Rocha V. A survey of fully haploidentical hematopoietic stem cell transplantation in adults with high-risk acute leukemia: a risk factor analysis of outcomes for patients in remission at transplantation. Blood. 2008;112:3574–3581. doi: 10.1182/blood-2008-02-140095. [DOI] [PubMed] [Google Scholar]
- 91.Federmann B, Bornhauser M, Meisner C, Kordelas L, Beelen DW, Stuhler G, Stelljes M, Schwerdtfeger R, Christopeit M, Behre G, Faul C, Vogel W, Schumm M, Handgretinger R, Kanz L, Bethge WA. Haploidentical allogeneic hematopoietic cell transplantation in adults using CD3/CD19 depletion and reduced intensity conditioning: a phase II study. Haematologica. 2012;97:1523–1531. doi: 10.3324/haematol.2011.059378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, Devine SM, Wingard JR, Aljitawi OS, Cutler CS, Jagasia MH, Ballen KK, Eapen M, O’Donnell PV. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118:282–288. doi: 10.1182/blood-2011-03-344853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, Gooley TA, Piantadosi S, Kaup M, Ambinder RF, Huff CA, Matsui W, Bolanos-Meade J, Borrello I, Powell JD, Harrington E, Warnock S, Flowers M, Brodsky RA, Sandmaier BM, Storb RF, Jones RJ, Fuchs EJ. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–650. doi: 10.1016/j.bbmt.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]