Abstract
Background
Depressive symptoms and clinical depression are highly prevalent in low-income mothers and negatively affect their infants and toddlers.
Objectives
To test interpersonal psychotherapy combined with parenting enhancement on depressive symptoms and parenting behavior, compared with usual care.
Method
Mothers (n = 226) of Early Head Start infants and toddlers from the southeastern and northeastern United States were randomized to the intervention delivered in-home by psychiatric mental health advanced practice nurses or usual care delivered by generalist nurses. Rigorous clinical depressive symptom and depression assessments and videotaped, coded mother-child interactions were used as baseline and 14-, 22-, and 26-week postintervention measures.
Results
Both the intervention and control groups had significantly reduced Hamilton Rating Scale for Depression scores at each subsequent time point compared to baseline (p < .0001). However, only mothers receiving the intervention showed a significant increase in positive involvement with their child, as measured by closeness, positive affect, affection, and warm touch at T4 (t = 2.22, df = 156, p < .03).
Discussion
Both intervention and control conditions resulted in symptom reduction, but only the intervention mothers showed significant interaction changes with their child, an essential step in reducing the negative child outcomes associated with maternal depressive symptoms. Results suggest that a combination of generalist and specialist nurses could be used to treat depressive symptoms in these mothers. Further study with longer postintervention observation is needed to see if, over time, the intervention led to longer-lasting symptom reduction.
Keywords: mothers, depression, psychotherapy
The prevalence of depressive symptoms in low-income mothers is high--40-59% (Mayberry, Horowitz, & Declercq, 2007), four times that of middle-income mothers (Brown & Moran, 1997). Depressive symptoms, or the cognitive, affective, behavioral, and somatic changes that accompany an unremitting sad mood, are typically less severe than major depressive episode (MDE; American Psychiatric Association, 2000) but progress to MDE in 25% percent of individuals (Kessler et al., 2003). Depressive symptoms limit low-income mothers’ ability to manage stressors effectively and interfere with their use of education and work-training programs (Feder et al., 2009; Mickelson & Williams, 2008). Most profoundly, depressive symptoms compromise their parenting.
The capacity of depressive symptoms to compromise mothering has been well-documented. Even at moderate levels, maternal depressive symptoms rob mothers of the energy and focus needed for supportive, stimulating parenting (Hammen, 1991) and interfere with mothers’ contingent, sensitive responses to children’s needs and cues (National Institute of Child Health and Development [NICHD] Early Child Care Research Network, 1999). Maternal depressive symptoms have been associated with poorer development in infants and toddlers. In addition to reduced fetal body and head growth (El Marroun et al., 2012), infants of mothers with depressive symptoms vocalize less, engage in less play and exploratory behavior, and lag on standardized language and mental development scales, especially if maternal symptoms last longer than 6 months (Campbell et al., 2004). Toddlers of symptomatic mothers demonstrate more negative affect and severe temper tantrums (Needlman, Stevenson, & Zuckerman, 1991). As they reach school age, children reared by mothers with depressive symptoms are at higher risk than other children for depression, aggressive behavior, conduct disorders, speech and learning difficulties, and problems adjusting to school (Campbell, Morgan-Lopez, Cox, & McLoyd, 2009).
Compromised mothering has been implicated as the mediator between depressive symptoms and negative child outcomes (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Strong, competent mothering is especially critical to infants and toddlers growing up in low-income families because it can offset conditions such as substandard housing, failing schools, and exposure to violence that threaten optimal child development (Jarrett, 1997). Since economic hardship inflicts the greatest damage on children under the age of 3 years (Knitzer & Lefkowitz, 2006), depressive symptoms that compromise mothering remove the most powerful buffer against poverty from the infant or toddler when it matters the most. It is critical to reduce depressive symptoms in these mothers quickly and help them parent more effectively even while symptoms are present.
Low-income women have had difficulty staying in depressive symptom treatment protocols, in part because of transportation difficulties, childcare needs, and stigma (Miranda et al., 2006). To circumvent these barriers, psychotherapy has been delivered to mothers in their home. Most of the trials have been conducted during the immediate postpartum period, with varying results depending whether an evidence-based treatment was provided, fidelity was maintained, and mothers were retained long enough to receive a minimum dose (Appleby, Warner, Whitton, & Faragher, 1997; Cooper, Murray, Wilson, & Romaniuk, 2003; Spinelli & Endicott, 2003; van Doesum, Riksen-Walraven, Hosman, & Hoefnagels, 2008). Prior to the current study, interpersonal psychotherapy (IPT), an effective treatment for depressive symptoms and MDE, had been tested in middle-income antepartum and postpartum mothers (Grote et al., 2009; Weissman, Markowitz, & Klerman, 2007) but had not been adapted for in-home delivery to low-income mothers. In addition, these studies had showed that symptom reduction with IPT without intervention to improve parenting did not change mothering behaviors (Forman et al., 2007). Since improved mothering is one empirically supported route to optimal child outcomes (Lovejoy et al., 2000), the in-home adaptation of IPT tested in this study was enhanced with intervention materials to help mothers change the parenting interactions that were most affected by their current depressive symptoms. After piloting the adapted intervention (Beeber, Holditch-Davis, Belyea, Funk, & Canuso, 2004), the combined IPT and depression-specific parenting enhancement intervention (IPT+PE) was tested in a sample of mothers of infants and toddlers enrolled in Early Head Start (EHS), a federal enrichment program for low-income children between 0-3 years of age.
Method
Design
The study used a randomized, two-group, repeated measures design. Mothers who received the IPT+PE plus EHS enrichment as usual were compared to mothers receiving an attention-control health education plus EHS enrichment as usual (ACTAU). The IPT+PE and ACTAU conditions were delivered over a 20-week period. Data were collected at four points: at baseline prior to randomization (T1), partway through the intervention (T2: 14 weeks), after completion of the intervention and termination with the nurse (T3: 22 weeks), and 1 month after all intervention stopped (T4: 26 weeks).
Hypotheses
Study hypotheses were: (a) mothers receiving IPT+PE would demonstrate significantly less depressive symptom severity midway through treatment (T2: 14 weeks), at the conclusion of treatment (T3: 22 weeks), and 1 month following completion of treatment (T4: 26 weeks) than mothers who received an ACTAU; and (b) when interacting with their infant or toddler, mothers receiving IPT+PE would demonstrate significantly more positive involvement, more developmental stimulation, and less negative control at 14 weeks (T2) and 26 weeks (T4) than mothers who received ACTAU.
Sample
The sample consisted of 226 mothers and their infants and toddlers who were enrolled in one of six EHS programs in the southeastern and northeastern United States. To be screened for depressive symptoms, mothers had to be the biological parent and primary caretaker of an enrolled EHS child, speak English as their primary language, be at least 15 years of age, and be at least 6 weeks postpartum. The last criterion was set to eliminate mothers who might have transient depressive symptoms during the postpartum period (American Psychiatric Association, 2000). Mothers were screened using the Center for Epidemiological Studies Depression scale (CES-D), a 20-item self-report on which a score of 16 or higher is indicative of clinically significant symptomatology (Radloff, 1977). A total of 827 mothers were screened, 429 (52%) of whom scored 16 or higher on the CES-D. To be eligible for the study, mothers had to score at least 16 on the CES-D, could not be in regular psychotherapy or counseling (two or more sessions per month) or taking a psychotropic medication and, after having a full explanation of the study, had to agree to random assignment to either condition. Eligibility criteria for the children were age (minimum 6 weeks old and maximum 36 months old at baseline) and enrollment in EHS. Children with health and developmental problems were not excluded because these phenomena are associated strongly with depressive symptoms in mothers; 56% of these children had been referred for language or developmental delays or behavioral problems at the time of enrollment. Mothers provided written consent for both the preliminary screening and the study. Mothers younger than 18 years old were asked to assent to the study and have a guardian’s written consent. The primary author’s institutional review board approved the study.
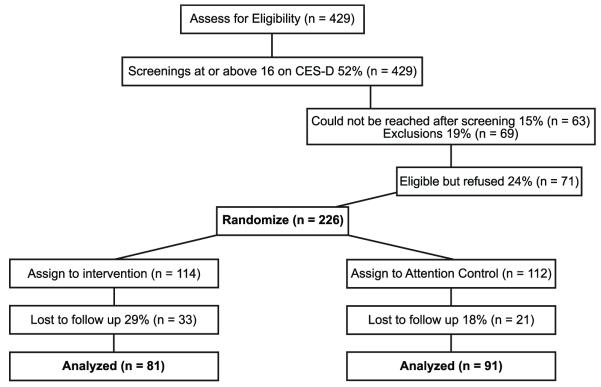
Calculation of the sample size was made to reflect a .20 effect size over the four data collection points, with maximum and minimum correlation between time points of .60 and .45, respectively. A sample size of 192 was determined to be adequate to detect a time trend difference between the intervention and ACTAU group with .80 power (Cohen, 1977). An additional 34 mothers were recruited to compensate for possible 15% attrition. A Consolidated Standards of Reporting Trials (CONSORT) diagram of the study is presented in Figure 1 (Moher, Schulz, & Altman, 2005).
Figure 1.
CONSORT Diagram for Enrollment in Study
At the time of randomization, mothers’ average age was 26 years and 69% reported their ethnicity as Black or African American, Native American, or mixed race (Table 1). Mothers had very limited economic resources. An income-to-needs ratio was used to determine that the sample included low-income mothers. This ratio is a precise measure of income developed by the NICHD in which the family’s reported total income is divided by the government poverty threshold based on family size and number of children younger than 18 years old for the year in which the mother’s income data were obtained (NICHD Early Child Care Research Network, 1999). Approximately 88% of the sample reported incomes below the poverty threshold and, using the formula, on average, the sample income-to-need ratio was half (M = 0.5; SD = 0.4) of the poverty threshold for the year in which the income data were obtained (NICHD Early Child Care Research Network, 1999). More than half of the mothers were screened as having significant depressive symptoms; 24% met criteria for a diagnosis of MDE and an additional 35% for minor depression.
Table 1. Demographics.
| Variable | Total Sample (n = 226) |
Intervention (n = 114) |
Control (n = 112) |
p |
|---|---|---|---|---|
| Maternal age | 26.0 (5.7) | 26.3 (5.9) | 25.8 (5.6) | .523 |
| Education (years of school) | 11.9 (2.2) | 12.0 (2.3) | 11.7 (2.1) | .393 |
| Work Status | ||||
| Working full- or part-time | 96 (43%) | 52 (46%) | 44 (39%) | .362 |
| In school | 43 (19%) | 23 (20%) | 20 (18%) | |
| Ethnicity | .491 | |||
| Black/African American | 147 (61%) | 73 (64%) | 64 (57%) | |
| White | 65 (27%) | 30 (26%) | 31 (28%) | |
| Mixed/Native American/Native | 19 (8%) | 8 (7%) | 10 (9%) | |
| Hawaiian/Pacific Islander/Asian | 10 (4%) | 3 (3%) | 7 (6%) | |
| Unreported | ||||
| Living without spouse or partner | 140 (63%) | 67 (60%) | 73 (65%) | .457 |
| Self-reported Maternal health as poor or | ||||
| fair (1 question MOS-SF-12) | 121 (54%) | 61 (54%) | 60 (54%) | .993 |
| Maternal CES-D score | 26.5 (12.2) | 26.1 (12.4) | 26.9 (12.1) | .598 |
| Maternal HRSD | 16.2 (7.7) | 16.8 (7.8) | 15.7 (7.6) | .309 |
| Depression Status | .429 | |||
| Maternal Diagnosis MDE* | 55 (24%) | 28 (25%) | 27 (24%) | |
| Minor Depression‡ | 80 (35%) | 36 (32%) | 44 (39%) | |
| Child age (months) | 24.9 (13.5) | 24.7 (13.7) | 25.0 (13.4) | .861 |
| Child female gender | 117 (52%) | 62 (54%) | 55 (49%) | .427 |
| Children with chronic health condition, | ||||
| disability, developmental lag, behavioral issues |
127 (56%) | 66 (58%) | 61 (54%) | .603 |
| Number of children in household 5 years | ||||
| old and under (including study child) | 1.8 (0.8) | 1.7 (0.8) | 1.9 (0.8) | .072 |
Notes. Percentages may not sum to 100% due to rounding. The p-value reflects extent of random imbalance between Intervention and Control groups.
MOS-SF-12 = 12-item short form survey from the Medical Outcomes Study, CES-D = Center for Epidemiologic Studies Depression Scale, HRSD = Hamilton Rating Scale for Depression, MDE = Major Depressive Episode
Reported or observed to have 5 or more symptoms of MDE, including sad mood or anhedonia that met sufficient intensity and duration thresholds during the same 2-week period
at least 2 but fewer than 5 symptoms of MDE including significant sad mood or anhedonia that met sufficient intensity and duration thresholds during the same 2-week period (American Psychiatric Association, 2000).
Intervention
Interpersonal psychotherapy is focused on one of four areas (disputes, role transitions, grief, or interpersonal deficits) to determine interpersonal sources of depressive symptoms. Using descriptive data from symptomatic low-income mothers, the intervention was tailored to fit low-income mothers by organizing the four IPT foci around problems they typically faced (Beeber, Perreira, & Schwartz, 2008). The content for each interpersonal area was distilled into several one-page modules written in the vernacular that mothers used to describe their interpersonal problems. In each IPT module, specific strategies were introduced as the means to resolve the problems (Beeber et al., 2004). The modules were written using words that mothers with limited literacy could read. To personalize the intervention, the child’s name was embedded in the text, mothers could write their own reflections and thoughts on the worksheets, and the mother and child’s photograph was placed on the sheet. In addition to the focus on one primary IPT theme, all mothers received content on relapse management and parenting interaction enhancement. A personalized parenting guidance intervention was created for each mother that was based on an in-home assessment of the mother’s unstructured interactions with her child. The parenting guidance helped mothers identify how selected depressive symptoms were interfering with a contingent, sensitive response to their child’s cues. Specialized parenting enhancement modules, written in the same manner as the IPT modules, helped mothers enact strategies to override the symptoms, focus on their infant or toddler, and interact more sensitively.
The IPT was adapted further for in-home delivery by coordinating the intervention with EHS programming. Nurses were essential to this process. Nurses already provided in-home visits to EHS families for health promotion. By using advanced practice psychiatric mental health nurses (PMH-APRNs) as interventionists, mothers could tell inquisitive family or neighbors that the nurse was visiting without drawing attention to the mental health focus of the visit (Beeber et al., 2007). The intervention incorporated the infant-toddler enrichment activities that EHS was already providing and, if the mother was willing, the nurse involved EHS home visitors and staff as adjunct support providers.
The intervention began as soon as the mother completed the baseline data collection and was conducted weekly over the next 5 months. The initial phase was conducted during 10 face-to-face in-home visits followed by a month of booster telephone calls. At a final face-to-face visit, the nurse and the mother developed a plan for continuing treatment if needed. Fidelity was maintained using a manualized training program, weekly audits of each nurse’s sessions to assure that the protocols specified in the intervention manual were followed, and weekly reflective supervision conducted with all the PMH-APRNs linked together in a conference call format (see Supplemental Digital Content 1, which provides a detailed description of the IPT and PE intervention and ACTAU conditions).
Procedures
The EHS home visitors and daycare center teachers worked in partnership with the research team to obtain consent and screen all eligible mothers in their caseload with the CES-D. Mothers were paid $10 for completing the screening. Mothers were randomized equally to the intervention or ACTAU condition at each site using a computer-generated assignment list. Research staff administered the study consent and prerandomization baseline data and, blinded to the assignment of the mother, conducted subsequent data collections with participating mothers.
The ACTAU condition consisted of 10 in-person, in-home sessions followed by a month of booster telephone calls delivered by a registered nurse who did not have specialized training in psychiatric mental health except for the project-related training in the assessment and management of suicidal and other crisis situations. The attention-control nurse established an ongoing relationship with the mother through which she conducted a scripted, nonindividualized health education lesson on a topic unrelated to stressors and depressive symptoms, such as preventing home accidents and healthy eating. The nurse assessed and intervened only if the mother’s safety was endangered, and did not address other problems that the mother brought up. Fidelity was monitored through regular reflective supervision by conference call. Mothers in the ACTAU condition were promised that they would receive the intervention after their last data collection was completed; 46% completed it. Data were collected between 2004 and 2010.
Both sets of mothers participated in four data collections in their home consisting of a 45-minute unstructured videotaping during a time of day when the EHS child was awake. Mothers were asked to go about their normal activities and interactions with the child. When the videotaping was finished, data collectors completed the clinical examinations (Hamilton Rating Scale for Depression [HRSD] and the Structured Clinical Interview for DSM-IV, Research version [SCID-R]) and observational assessment (HOME Inventory). The remainder of the self-report instruments were administered orally to allow mothers with low literacy to participate. To assist with oral administration, mothers held a card with the numbers and the response set for each instrument and pointed to their chosen answers. Mothers were assessed at each data collection for symptom severity, suicidal risk, and endangerment, and were referred for ongoing care if still symptomatic (>6 on the HRSD) at their final contact with the study.
Mothers receiving the intervention were not offered antidepressants as an adjunct treatment. Mothers were assessed at 6 and 12 weeks using standard practice guidelines to ascertain that their symptoms were being treated adequately with IPT+PE alone. A small number of mothers (n = 4) were assessed to be in need of evaluation for antidepressant treatment at the conclusion of IPT+PE or complementary post-ACTAU treatment, and were assisted in finding a provider after their final data collection.
Because the four contacts from data collectors were positive attention for mothers undergoing hardship, care was taken to assure that mothers in both groups received identical contacts and incentives. Mothers received $25 for each data collection and framed photographs of themselves and their children taken during the previous data collection. Appreciation letters containing small gifts such as hand cream samples and holiday cards were sent between data collections to remind mothers of their participation. Mothers and children were given personal gifts such as a kitchen towel and a small toy, a copy of their videotapes, and mental health resource lists at the last study contact.
Measures
Understanding the difficulty of fitting the study into these mothers’ lives and the toll that depressive symptoms took on their energy and motivation, flexibility was built into the intervention delivery schedule to assure that all mothers had completed the same number of intervention contacts by each data point. All of the measures used in the study had excellent reported reliability and validity indices with low-literacy populations; most had been used in previous studies in this population by the research team (Beeber et al., 2004; Beeber et al., 2010). In addition, measurement techniques used in previous clinical trials of in-home interventions were improved upon. Stringent measures of depressive symptoms (HRSD and SCID-R) were included that used clinically trained observers. These measures provided sufficient data to determine a diagnosis of MDE, which allowed comparison of this sample to those in larger epidemiological studies (Kessler & Wang, 2008). In addition, using the SCID-R provided data from which the DSM-IV-R diagnosis of minor depression (symptoms met initial criteria but fell short of full diagnostic severity; Table 2) could be determined, which had not been done previously in this population.
Table 2. Measures, Reliability Indices, and Measurement Timepoints.
| Construct or Variable | Instrument | α* k IRR |
Timepoint‡ | |||
|---|---|---|---|---|---|---|
| Screening for Depressive | Center for Epidemiological Studies Depression Scale | |||||
| Symptom Severity | (CES-D; Radloff, 1977) | α = .90 | ||||
| Outcomes | T1 | T2 | T3 | T4 | ||
| Depressive Symptom Severity | Hamilton Rating Scale for Depression (Hamilton, 1960) | α = .75 | X | X | X | X |
| Major Depressive Episode | Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 2001) |
IRR>.85 | X | — | — | X |
| Maternal Positive Involvement, Negative Control, Developmental |
Maternal-Child Observation (MCO; Videotaped; Holditch-Davis et al., 2007) |
k = .66-.95 | X | X | — | X |
| Stimulation | HOME Inventory (Observer-rated; Caldwell & Bradley, 1980) | IRR > .90 | X | X | — | X |
| Perceived Stress | Everyday Stressors Index (ESI; Hall & Farel, 1988) | α = .83 | X | X | X | X |
| Satisfaction with Social Support | Interpersonal Inventory (IPRI; Tilden, Nelson, & May, 1990) | α = .90 | X | X | X | X |
| Mediators | ||||||
| Self-Efficacy | General Self-Efficacy Scale (GSE: Schwarzer & Born, 1997) | α = .89 | X | X | X | X |
| Social Support Seeking | Social Support Seeking Inventory (SSSI; Greenglass, Fiksenbaum, & Burke, 1996) | |||||
| Moderators | ||||||
| Maternal Characteristics | Family Information Interview (Beeber et al., 2007) | α = .84 | X | — | — | X |
| Maternal Health-Related Function | MOS Health Form (SF-12; Hurst, Ruta, & Kind, 1998) | X | X | X | X | |
| Maternal Burden Factors | X | — | — | X | ||
| Family Information Interview (FII) | ||||||
Notes. Reliability indices for this study; α = Cronbach’s alpha; IRR = interrater reliability; k = Kappa;
Timepoint: T1 = baseline, T2 = 14 weeks, T3 = 22 weeks, T4 = 26 weeks
Unlike previous studies using maternal self-report of parenting, a method that is biased by maternal depressive symptoms, 45-minute videotapes of unstructured maternal-child interactions in the home were used in this study. The 45-minute length was used because experience with other populations had shown that it was long enough to obtain a variety of caregiving situations without being unduly burdensome for the mother. Maternal interactive behaviors (e.g., location of the mother, caregiving, looking, moving, talking, gesturing, touching, and playing) were coded every 10 seconds for the entire observation by trained coders who achieved adequate interrater reliability (>85% exact agreements, and kappas >.70) throughout the study. Frequency counts of maternal behavioral codes were combined and percentages of the observation in which the mother and child engaged in a particular interaction were calculated to create the behavioral variables. For analysis, related maternal behavioral variables along with HOME inventory subscales were clustered into three theoretically derived dimensions--(a) maternal positive involvement (made up of playing with child, total interaction percentage, positive behaviors, warm touch, uninvolved with child reversed, HOME subscale V); (b) developmental stimulation (talk and teach); and (c) negative control (HOME subscale II reversed)--by converting each variable to a Z-score calculated over similarly aged children and then averaging the Z-scores for all of the variables in the dimension (Holditch-Davis, Schwartz, Black, & Scher, 2007). This method removed any age-related differences in the dimension score and allowed comparisons over the varying age groups. Maternal positive involvement and developmental stimulation had acceptable internal consistency alphas (.86 and .74); maternal negative control was represented by a single variable and alpha was not calculated (Table 2).
Data Analysis
The impact of IPT+PE on maternal depressive symptoms across the postrandomization period was evaluated via an intent-to-treat approach to analysis. The general linear mixed model was used to provide a random coefficients formulation, allowing for the actual timing of all available postrandomization data collections for each mother. The response variable was specified as the change from randomization value for the HRSD score at each postrandomization data collection; explanatory variables were the main effects of randomized group and number of weeks postrandomization, as well as their interaction. The HRSD score at the time of randomization was included as a covariate. This formulation allowed for separate linear fit for each randomized group across the postrandomization period, adjusting for HRSD score at randomization. Polynomial (i.e., quadratic and cubic) terms for postrandomization weeks and their interaction with randomized group were included. Random effects included specification of random intercepts and slopes for each mother, which permitted a mother-specific regression line across time. An unstructured covariance matrix was specified for the random effects. Prespecified statistical contrasts were constructed from the longitudinal trajectories to compute randomized group-specific mean HRSD scores at the ideal timing of each postrandomized data collection (i.e., 14 weeks for T2, 22 weeks for T3, and 26 weeks for T4), as well as to compare the randomized groups’ mean difference in HRSD score at these same idealized timings. This procedure was repeated separately for the measures of perceived stress, social-support-seeking and satisfaction, self-efficacy, and health-related function as response variables. Statistical significance was determined at the two-sided .05 level; no adjustment to the p-values is reported to account for multiple comparisons.
To examine associations between HRSD scores and the self-efficacy measure, mother-specific change scores from the value at randomization for each were formed. Pearson correlation coefficients were computed between these change scores at each postrandomization data collection (i.e., T2, T3, and T4). Separate regression models were fitted for each of the dimensions arising from the maternal-child observations. However, as these variables were only measured at the time of randomization and at T4, ordinary analyses of covariance (ANCOVAs) were fitted to the T4 values as response variables, with a main effect for randomized group, and covariate adjustment for the corresponding value at randomization and child age. All analyses were performed using SAS version 9 software.
Results
One hundred fourteen mothers were assigned randomly to receive IPT+PE plus EHS enrichment, and 112 received the ACTAU plus EHS enrichment; the overall attrition rate (i.e., mothers not having a data collection point beyond T2) was 23%, 20 from the ACTAU group and 31 from the IPT+PE group. The attrition rate between the two groups was not significant (p = .09). Using a minimum dose comparable to IPT administered to similar populations (Grote et al., 2009), 75% of the IPT+PE mothers completed the minimum dose of seven or more face-to-face sessions. Both the IPT+PE and ACTAU conditions significantly reduced HRSD scores by 14 weeks, midway through the intervention and control visits (IPT+PE = −4.7; ACTAU = −4.52), and the means continued to remain significantly lower than at baseline at 22 weeks, the end of the IPT+PE and ACTAU visits (Intervention = −4.8; ACTAU = −4.9), and at 26 weeks, a month after contact with the nurses had stopped (Intervention = −5.0; ACTAU = −5.3).All p-values were <.0001 for each group at each timepoint). No statistically significant mean differences between randomized groups were found in the reduction of mothers’ depressive symptoms at the ideal timing of T2, T3, or T4.
The impact of IPT+PE on the videotaped, coded interactions of mothers with their children was analyzed using T4 as the measurement point (a month after cessation of all contact with the nurse-interventionist). An important finding emerged: only mothers receiving IPT+PE showed a significant increase in positive involvement with their child as measured by their observed behaviors of closeness, eye contact, positive affect, affection, and warm touch (T4, 26 weeks: t = 2.22, df = 156, p < .03). No significant group differences were observed in mothers’ developmental stimulation or negative control of the child.
To guide future studies, post hoc analysis was conducted on several key variables: perceived stress, social support, and self-efficacy. These variables were expected to change as a result of the intervention. At T4, change from T1 to T4 in both intervention and attention-control groups showed significant within-group reductions in perceived stress (p < .001) and significant increases in social support seeking (p < .005) and self-efficacy (p < .001).
Discussion
While IPT+PE significantly reduced depressive symptoms at three timepoints subsequent to baseline (14, 22, and 26 weeks), regular visits from generalist nurses reduced ACTAU mothers’ depressive symptoms also, indicating that the nurse visitation and health education were active interventions. The capacity of mild, nonspecific comparison conditions to significantly reduce depressive symptoms in populations undergoing severe economic hardship has been found previously (Cooper et al., 2003; Spinelli & Endicott, 2003). While the ACTAU nurses followed a protocol directing them to focus on health education and deflect issues that the mother raised about depressive symptoms and stressors, poor health itself was a stressor that the ACTAU condition addressed. In addition, the AC nurses needed to engage the ACTAU mothers actively to retain them in the health education condition. To do this, the nurses reached out, pursued mothers, helped them schedule weekly appointments, relayed respect, and expressed caring and personal interest in the mothers. These relationship-building, engagement strategies were present in both the IPT+PE and ACTAU protocols. When added to the regular structuring of the ACTAU appointments, these strategies used by the generalist nurses may have increased ACTAU mothers’ perceived self-efficacy and social support by helping them gain greater control over their lives. Self-efficacy and social support are perceived mediators between stress and depressive symptoms. This finding suggests that generalist nurses already providing intervention through enrichment programs such as Head Start, EHS, and the Nurse Family Partnership could reach low-income, high-risk symptomatic mothers and help them reduce their depressive symptoms. If a generalist nurse intervention was used for all symptomatic mothers and IPT+PE by the mental health specialist nurse used for more severely affected or nonresponsive mothers, the cost of the in-home mental health intervention could be reduced.
The outcome of the intervention may have resulted from design limitations of the study. The relatively short (6-month) subsequent measurement of outcomes did not allow determination of whether the depressive symptom reduction persisted equally in both groups over time. Mothers receiving IPT+PE learned strategies that were designed to help them reduce symptoms and the stressors associated with them, as well as actions to take when depressive symptoms reoccurred. Mothers’ ongoing use of these strategies should have maintained the reduction in symptoms, which might have changed the patterns of symptom reduction in the two groups over time. The ACTAU mothers knew at the outset that they would be offered help for depressive symptoms at the end of their involvement in the study. Their positive expectations may have been an important factor in their symptom reduction especially at T4.
A key finding was that only mothers receiving IPT+PE who enhanced their responsiveness to their child in the face of depressive symptom reduction made significant increases in maternal involvement. In this study, maternal involvement was operationalized as the frequency of four key observed parenting behaviors -- interacting with the child for longer periods, and smiling, affection, and warm touch with the child. Forman et al. (2007) have proposed that, for the child to respond positively to maternally focused interventions, reduction in maternal depressive symptoms must be followed by positive changes in the mother’s parenting behaviors. The IPT+PE used in this study combined emerging knowledge of infant mental health promotion and depression treatment to achieve significant change in maternal interactions. By directing attention to the depressive symptoms that interfered with her mothering, the mother could make immediate changes in her behaviors and witness the effects on the child. In detailed, session-by-session observational notes, the nurses reported that mothers showed positive affect when their children had an immediate affirmative response to improved parenting. The child’s quick response seemed to motivate mothers to maintain their new parenting behaviors, which then may have helped mothers remain in the intervention. Maternal behavioral change is a powerful benefit to the child, the long-term impacts of which could justify the additional expense of providing IPT+PE by way of the PMH specialist nurse. Ultimately, a deeper understanding of the differential effects of nurse generalists and PMH nurse specialists offers the potential to combine generalist-specialist nurses in a cost-effective program of outreach and retention of these high-risk mothers.
Another important finding of the study was to demonstrate that an evidence-based intervention could be adapted to home delivery and accessed by mothers with significant depressive symptoms who were not using either primary care providers or formal mental health services. We attributed the improved retention in the intervention to the skill of the nurses and to the strategy of embedding a mental health intervention in an existing in-home child enrichment service (EHS) that reduced stigma and removed instrumental barriers. Compared to a retention rate of 36% in a psychotherapy trial with disadvantaged women (Miranda et al., 2006), 75% of mothers in the intervention group in the current study completed a minimum dose of IPT+PE sessions. Empirical data on the tailoring of IPT+PE and the strategies that were successful in engaging these mothers has been published previously (Beeber et al., 2007).
Clinically, this study demonstrated that in this sample of low-income mothers enrolled in a child enrichment program, clinical depression and less severe depressive symptoms were prevalent and persisted well past the postpartum era into the child’s second and third year of life. The stringent measure of clinical depression indicated that 24% of the sample met DSM-IV criteria for MDE and an additional 35% met clinical criteria for minor depression (American Psychiatric Association, 2000). These sample percentages exceeded the incidence in the US population (Kessler & Wang, 2008) and yet none of these mothers were in treatment at the time of recruitment.
Furthermore, 56% of the children in the sample had been referred for health conditions, developmental lags, behavioral problems, or disabilities. These conditions are associated highly with maternal depressive symptoms, suggesting that child health providers and developmental specialists who uncover such conditions should be alert for depressive symptoms and clinical depression in the mothers.
Additionally, 54% of the mothers reported fair or poor health on the MOS SF-12; poor health in a mother should prompt providers to screen for depressive symptoms. Postpartum providers should screen for depressive symptoms beyond the 6-week checkup for a mother of an infant or toddler and offer screening, support, and intervention. However, the current commitment of resources to tertiary treatment of only mental health symptoms that reach clinical levels have curtailed sharply the development, testing, and availability of intervention resources when depressive symptoms are at subthreshold or subsyndromal levels. This and other studies have documented the prevalence of such conditions in low-income mothers, an important step in determining the need for early intervention services.
Ideally, interventions should extend beyond the mother to the prevention or reduction of negative outcomes in infants and toddlers. Future research should be focused on whether symptom reduction and improved parenting can prevent the well-documented developmental lags and behavioral problems in the children of symptomatic mothers. Such studies will require sensitive child measures over sufficient time to show meaningful behavioral change over the multiple developmental stages that occur in the first 3 years of life. While complex, the benefits of refining early targeted, tailored, and stigma-free mental health intervention will outweigh the long-term cost of inattention to depressive symptoms and compromised parenting in low-income mothers and their infants and toddlers.
Supplementary Material
Acknowledgements
This study was funded by the National Institutes of Health, National Institute of Mental Health, R01MH065524. Thank you to the psychiatric mental health advanced practice nurses, the generalist nurses, the research staff, the staff of the collaborating Early Head Start programs, and the mothers who gave of their time and limited energy to teach us how to help them.
Footnotes
Supplemental Digital Content 1. Additional information that provides detailed description of the IPT and PE intervention and ACTAU conditions. Doc
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Linda S. Beeber, School of Nursing The University of North Carolina at Chapel Hill.
Todd A. Schwartz, School of Nursing and The Gillings School of Global Public Health The University of North Carolina at Chapel Hill.
Diane Holditch-Davis, School of Nursing, Duke University.
Regina Canuso, New York State Early Childhood Advisory Council.
Virginia Lewis, School of Nursing The University of North Carolina at Chapel Hill.
Helen Wilde Hall, School of Nursing The University of North Carolina at Chapel Hill.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th edition. Author; Washington, DC: 2000. text revision ed. [Google Scholar]
- Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ. 1997;314(7085):932–936. doi: 10.1136/bmj.314.7085.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeber LS, Cooper C, Van Noy BE, Schwartz TA, Blanchard HC, Canuso R, Emory SL. Flying under the radar: Engagement and retention of depressed low-income mothers in a mental health intervention. ANS: Advances in Nursing Science. 2007;30:221–234. doi: 10.1097/01.ANS.0000286621.77139.f0. [DOI] [PubMed] [Google Scholar]
- Beeber LS, Holditch-Davis D, Belyea MJ, Funk SG, Canuso R. In-home intervention for depressive symptoms with low-income mothers of infants and toddlers in the United States. Health Care for Women International. 2004;25:561–580. doi: 10.1080/07399330490444830. [DOI] [PubMed] [Google Scholar]
- Beeber LS, Holditch-Davis D, Perreira K, Schwartz TA, Lewis V, Blanchard H, Goldman BD. Short-term in-home intervention reduces depressive symptoms in Early Head Start Latina mothers of infants and toddlers. Research in Nursing & Health. 2010;33:60–76. doi: 10.1002/nur.20363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeber LS, Perreira KM, Schwartz T. Supporting the mental health of mothers raising children in poverty: How do we target them for intervention studies? Annals of the New York Academy of Sciences. 2008;1136:86–100. doi: 10.1196/annals.1425.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GW, Moran PM. Single mothers, poverty and depression. Psychological Medicine. 1997;27:21–33. doi: 10.1017/s0033291796004060. [DOI] [PubMed] [Google Scholar]
- Caldwell B, Bradley R. Home Observation for Measurement of the Environment. University of Arkansas at Little Rock; Little Rock, AR: 1980. [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker SI, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology. 2004;16:231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. Journal of Abnormal Psychology. 2009;118:479–493. doi: 10.1037/a0015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Academic Press; New York, NY: 1977. [Google Scholar]
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression. I. Impact on maternal mood. The British Journal of Psychiatry. 2003;182:412–419. [PubMed] [Google Scholar]
- El Marroun H, Jaddoe VW, Hudziak JJ, Roza SJ, Steegers EAP, Hofman, Tiemeier H. Maternal use of selective serotonin reuptake inhibitors, fetal growth, and risk of adverse birth outcomes. Archives of General Psychiatry. 2012;69:706–714. doi: 10.1001/archgenpsychiatry.2011.2333. doi:10.1001/archgenpsy.2011.2333. [DOI] [PubMed] [Google Scholar]
- Feder A, Alonso A, Tang M, Liriano W, Warner V, Pilowsky D, Weissman M. Children of low-income depressed mothers: Psychiatric disorders and social adjustment. Depression and Anxiety. 2009;26:513–520. doi: 10.1002/da.20522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis disorders (research version) Biometrics Research Department, New York State Psychiatric Institute; New York, NY: 2001. [Google Scholar]
- Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Greenglass E, Fiksenbaum L, Burke RJ. Components of social support, buffering effects and burnout: Implications for psychological functioning. Anxiety, Stress, and Coping: An International Journal. 1996;9:185–197. [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatric Services. 2009;60:313–321. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall LA, Farel AM. Maternal stresses and depressive symptoms: Correlates of behavior problems in young children. Nursing Research. 1988;37:156–161. [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Depression runs in families. Springer-Verlag; New York, NY: 1991. [Google Scholar]
- Holditch-Davis D, Schwartz T, Black B, Scher M. Correlates of mother-premature infant interactions. Research in Nursing & Health. 2007;30:333–346. doi: 10.1002/nur.20190. [DOI] [PubMed] [Google Scholar]
- Hurst NP, Ruta DA, Kind P. Comparison of the MOS short form-12 (SF12) health status questionnaire with the SF36 in patients with rheumatoid arthritis. British Journal of Rheumatology. 1998;37:862–869. doi: 10.1093/rheumatology/37.8.862. [DOI] [PubMed] [Google Scholar]
- Jarrett RL. African American family and parenting strategies in impoverished neighborhoods. Qualitative Sociology. 1997;20:275–288. [Google Scholar]
- Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-IV. Archives of General Psychiatry. 2003;60:1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual Review of Public Health. 2008;29:115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- Knitzer J, Lefkowitz J. Helping the most vulnerable infants, toddlers, and their families. Columbia University Mailman School of Public Health; New York, NY: 2006. [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. Journal of Obstetrical Gynecological and Neonatal Nursing. 2007;36:542–549. doi: 10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- Mickelson KD, Williams SL. Perceived stigma of poverty and depression: Examination of interpersonal and intrapersonal mediators. Journal of Social and Clinical Psychology. 2008;27:903–930. [Google Scholar]
- Miranda J, Green BL, Krupnick JL, Chung J, Siddique J, Belin T, Revicki D. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. Journal of Consulting and Clinical Psychology. 2006;74:99–111. doi: 10.1037/0022-006X.74.1.99. [DOI] [PubMed] [Google Scholar]
- Moher D, Schulz KF, Altman D. The CONSORT Statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials 2001. Explore. 2005;1:40–45. doi: 10.1016/j.explore.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Needlman R, Stevenson J, Zuckerman B. Psychosocial correlates of severe temper tantrums. Journal of Developmental and Behavioral Pediatrics. 1991;12:77–83. [PubMed] [Google Scholar]
- National Institute of Child Health and Development Early Child Care Research Network Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:285–401. [Google Scholar]
- Schwarzer R, Born A. Optimistic self-beliefs: Assessment of general perceived self-efficacy in thirteen cultures. World Psychology. 1997;3:177–190. [Google Scholar]
- Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. The American Journal of Psychiatry. 2003;160:555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- Tilden VP, Nelson C, May BA. The IPR Inventory: Development and psychometric characteristics. Nursing Research. 1990;39:337–343. [PubMed] [Google Scholar]
- van Doesum KT, Riksen-Walraven JM, Hosman CM, Hoefnagels C. A randomized controlled trial of a home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development. 2008;79:547–561. doi: 10.1111/j.1467-8624.2008.01142.x. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman GL. Clinician’s quick guide to interpersonal psychotherapy. Basic Books; New York, NY: 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.