Abstract
Background
Both bilateral cochlear implants (CIs) and bimodal (electric plus contralateral acoustic) stimulation can provide better speech intelligibility than a single CI. In both cases patients need to combine information from two ears into a single percept. In this paper we ask whether the physiological and psychological processes associated with aging alter the ability of bilateral and bimodal CI patients to combine information across two ears in the service of speech understanding.
Materials
The subjects were 61 adult, bilateral CI patients and 94 adult, bimodal patients. The test battery was composed of monosyllabic words presented in quiet and the AzBio sentences presented in quiet, at +10 and at +5 dB signal-to-noise ratio (SNR).
Methods:
The subjects were tested in standard audiometric sound booths. Speech and noise were always presented from a single speaker directly in front of the listener.
Results
Age and bilateral or bimodal benefit were not significantly correlated for any test measure.
Conclusions
Other factors being equal, both bilateral CIs and bimodal CIs can be recommended for elderly patients.
Keywords: cochlear implant, presbycusis, bilateral, bimodal
Background
Both bilateral cochlear implants (CIs) and bimodal (electric plus acoustic) CIs can provide better speech intelligibility than a single implant [1–5]. The two interventions, however, pose different information-extraction and central-integration challenges for CI patients. In the case of bilateral CIs, signals of the same kind, i.e., electric stimulation, are presented to the two ears. The signals, however, are not identical. The degree to which the inputs differ depends, at least, on the depth of electrode insertion, the number of activated channels for each ear, and the details of the ear-specific, input-amplitude to output-amplitude functions. The listener must construct a single percept from different information in the two ears. Bimodal stimulation poses a different problem for listeners. In this case, the information specified by low-frequency acoustic stimulation directed to one ear must be integrated with the information specified by wide-band electric stimulation directed to the other ear. Moreover, it is likely that the information in the low frequencies, e.g., in the range 250–750 Hz, is presented to different places in the electrically and acoustically stimulated cochlea.
In this paper we ask whether the changes in the physiological and psychological processing of auditory signals associated with aging [6,7] alter the ability of bilateral and bimodal CI patients to combine information across two ears in the service of speech understanding. To answer this question, we tested 61 bilateral CI patients and 94 bimodal CI patients with words in quiet, sentences in quiet, and sentences in noise. At issue was whether age was correlated with either bilateral benefit (bilateral score minus best-ear score) or bimodal benefit (bimodal score minus electric-only score).
Material and Methods
Subjects
The subjects were adult bilateral CI patients and bimodal CI patients tested at either Arizona State University; Mayo Clinic, Rochester; Vanderbilt University, or the University of Ottawa. The bilateral sample ranged in age, at time of testing, from 19 to 81 years. The majority of patients were between 40 and 70 years old. The mean duration of severe to profound hearing loss was 11.7 years. The mean duration of bilateral implant use was 3.8 years. The bimodal sample ranged in age, at time of testing, from 21 to 90 years. The majority of patients were between 60 and 80 years old. The mean duration of severe to profound hearing loss was 17.8 years. The mean duration of bimodal use (CI plus hearing aid) was 3.4 years.
Testing took place over a number of years. For that reason not all patients were tested with all of the speech material: 53 bimodal patients completed all the tests and 26 bilateral patients completed all of them. The sample sizes for bimodal and bilateral patients tested with each type of speech material ranged from 94 to 27 and are shown in Figures 1 and 2. Patients were selected for testing based on their willingness to participate in research and, for some, their willingness to travel to Arizona State University for testing.
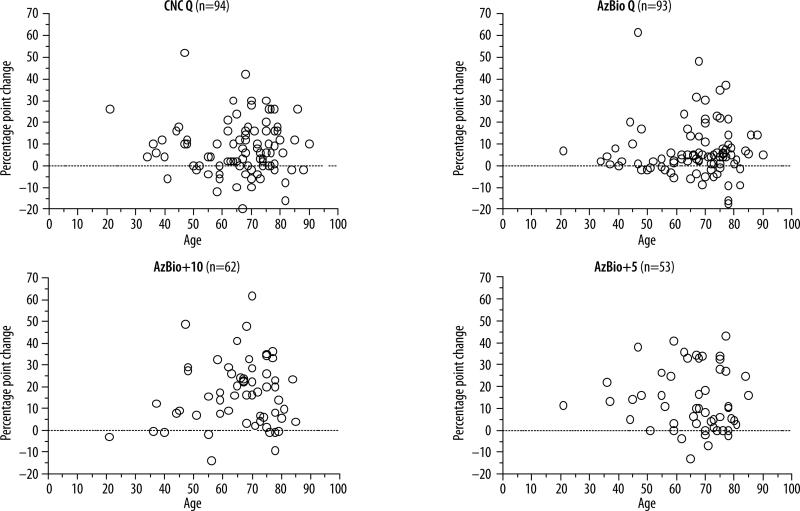
Figure 1.
Bimodal benefit as a function of age.
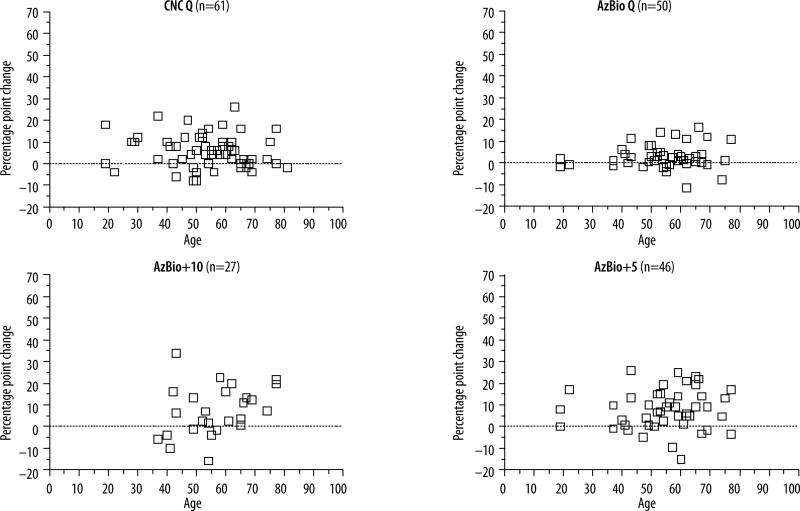
Figure 2.
Bilateral benefit as a function of age.
Speech materials
The test battery was composed of monosyllabic words [8] presented in quiet and the AzBio sentences [9] presented in quiet, at +10 and at +5 dB signal-to-noise ratio (SNR). Most commonly the tests were administered on the same day.
Listening environment
The subjects were tested in standard audiometric sound booths. Speech and noise were always presented from a single speaker directly in front of the listener with the speech signal at 60 dB SPL (a small number of patients were tested with speech at 70 dB SPL).
Results
The results for bimodal patients are shown in Figure 1 where percentage changes in performance, i.e., benefit, are plotted as a function of age. Change scores were calculated as bimodal score minus electric-only score. Visual inspection suggests that patients in their 70s derived as much bimodal benefit as younger patients for each type of test material. Pearson's correlations showed no significant relationship between age and benefit for any test measure (r=–0.04 for CNC words; r=–0.01 for AzBio sentences in quiet; r=0.11 for AzBio sentences at +10 dB SNR; and r=–0.07 for AzBio sentences at +5 db SNR).
The results for bilateral patients are shown in Figure 2 where benefit is plotted as a function of age. Change scores were calculated as bilateral score minus best-ear score. Visual inspection suggests that patients in their 70s derived as much bilateral benefit as younger patients. Pearson's correlations showed no significant relationship between age and benefit for any test measure (r=–0.11 for CNC words; r=0.16 for AzBio sentences in quiet; r=0.33 for AzBio sentences at +10 dB SNR; and r=0.07 for Az-Bio sentences at +5 db SNR).
Discussion and Conclusions
Aging is accompanied by decreases in function in multiple physiological, psychophysical, and psychological domains [6,7]. In this paper we have asked whether the accumulated consequences of decrements in these domains alter the ability of CI patients to extract and integrate speech-related information presented to the two ears. The answer to the question is relevant to health care systems as it is likely that there is an upper age limit for the benefit to be gained from bilateral and bimodal CIs.
We find that patients in their 70s and 80s can benefit from both bimodal and bilateral stimulation. Although we do not have equal sample sizes in all age decades, it does not appear that 70 and 80 year olds are less likely to benefit than younger patients. Thus, it is reasonable to recommend both bilateral CIs and bimodal CIs to elderly patients.
Acknowledgments
Source of Support: This research was supported by grants from the National Institute of Deafness and Other Communication Disorders (USA) to authors Dorman (R01 DC 010821), Gifford (R01 DC009404), Spahr (R03 DC 011052), Zang (F32 DC010937), and Loiselle (F31 DC011684-02).
References
- 1.Litovsky R, Parkinson A, Arcaroli J. Spatial hearing and speech intelligibility in bilateral cochlear implant users. Ear Hear. 2009;30(4):419–31. doi: 10.1097/AUD.0b013e3181a165be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buss E, Pillsbury HC, Buchman CA, et al. Multicenter U.S. bilateral Med-El cochlear implantation study: Speech perception over the first year of use. Ear Hear. 2008;29(1):20–32. doi: 10.1097/AUD.0b013e31815d7467. [DOI] [PubMed] [Google Scholar]
- 3.Shallop J, Arndt P, Turnacliff K. Expanded indications for cochlear implantation: Perceptual results in seven adults with residual hearing. J Speech-Lang Path & Applied Behavior Anal. 1992;16:141–48. [Google Scholar]
- 4.Ching T, Incerti P, Hill M. Binaural benefits for adults who use hearing aids and cochlear implants in opposite ears. Ear Hear. 2004;25:9–21. doi: 10.1097/01.AUD.0000111261.84611.C8. [DOI] [PubMed] [Google Scholar]
- 5.Dorman M, Gifford R. Combining acoustic and electric stimulation in the service of speech recognition. Int J Audio. 2010;49(12):912–19. doi: 10.3109/14992027.2010.509113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gordon-Salant S, Frisina R, Fay R, Popper A. The Aging Auditory System. Springer Handbook of Auditory Research, 34. 2010 [Google Scholar]
- 7.Pichora-Fuller M. Processing speed and timing in aging adults: psychoacoustics, speech perception, and comprehension. Int J Audiol. 2003;42:S59–67. doi: 10.3109/14992020309074625. [DOI] [PubMed] [Google Scholar]
- 8.Peterson GE, Lehiste I. Revised CNC lists for auditory test. J Speech Hear Disord. 1962;27:62–70. doi: 10.1044/jshd.2701.62. [DOI] [PubMed] [Google Scholar]
- 9.Spahr A, Dorman M, Litvak L, et al. Development and validation of the AzBio sentence lists. Ear and Hearing. 2012;33(1):112–17. doi: 10.1097/AUD.0b013e31822c2549. [DOI] [PMC free article] [PubMed] [Google Scholar]