Abstract
Distal radius fracture is usually associated with ulnar styloid fracture. Whether to fix the ulnar styloid or not remains a surgical dilemma as some surgeons believe that their repair is imperative while others feel that they should be managed conservatively. This prospective study involved 47 patients with unilateral fracture of the distal radius who met the inclusion criterion and underwent open reduction and internal fixation with volar locking plates; 28 patients (12 males and females = 16) had an associated ulnar styloid fracture (Group A) while 19 (7 males; 12 females) did not have any ulnar styloid fracture (Group B). At the time of final evaluation both the groups were compared clinically by measuring the grip strength and range of motion around the wrist and the radiologically by measuring radial angle, radial length, volar angle and ulnar variance. Subjective assessment was done using DASH score and final assessment using Demerit point system of Saito. In Group A, average time for consolidation was 9.4 weeks, 17 patients developed non-union of the ulnar styloid, average DASH scores was 4.4 and according to Demerit point system of Saito, there were 78.5 % excellent, 17.9 % good and 3.6 % fair results; there were 2 cases of loss of reduction out of which one had persistent ulnar sided wrist pain. In Group B the average time for consolidation was 10.2 weeks, average DASH score was 3.8.and Demerit point system of Saito yielded 78.9 % excellent, 15.8 % good and 5.3 % fair results. There was one case of loss of reduction and one case of carpal tunnel syndrome which was managed conservatively. Both groups attained excellent range of motion, grip strength and well maintained the post operative radiological parameters. The comparison of clinico-radiological parameters in both groups was found to be statistically insignificant. To conclude, ulnar styloid fracture or its non union does not affect the outcome of an adequately fixed distal end radius fracture. We urge caution in electing operative treatment of non-united fracture of the ulnar styloid until better scientific report for treatment of pain associated with these fracture is available.
Keywords: Distal radius fracture, Ulnar styloid fracture, Volar locking plate
Introduction
Fractures of the distal radius account for one sixth of all fractures seen in the emergency room [1]. The distal end of radius is especially susceptible to fracture because it comprises approximately 80 % of the wrist joint surface and bears nearly the full load from a fall on the outstretched hand. Ulnar styloid fracture is commonly associated with Distal radius fracture (DRF). The ulnar styloid plays a crucial role in the wrist bio-mechanics. It is an important supportive structure for the triangular fibrocartilage complex (TFCC) [2] and its base and the fovea are the insertion points for the primary stabilisers of the distal radio ulnar joint (DRUJ). It functions as a strut, helping to stabilise the ECU and the ulno-carpal ligaments.
The role of internal fixation of the ulnar styloid is debated. Some surgeons feel that the repair avoids the symptomatic instability or nonunion, and others feel that the added surgical time, scar, risks, and implant prominence are not justified. To the best of our knowledge only a handful of reports are available considering the effect of ulnar styloid fracture on the overall outcome when DRF is fixed using a volar locking plate [3–8] . This study was done with an aim to evaluate the effect of associated ulnar styloid fractures in distal radius fractures managed with volar locking plates.
Material and Methods
This was a prospective study which involved patients with unilateral fractures of the distal radius who presented to the accident and emergency wing of our hospital and underwent open reduction and internal fixation with volar locking plates. Exclusion criteria were previously operated or non-functional wrist, pathological fracture, radio-carpal arthritis, skeletally immature patients and open fractures. There were a total of 47 such patients who satisfied the above said criteria and formed the study cohort. The study was approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Forty seven patients (Table 1) satisfied the above said criteria and were included in the study; 28 were associated with an ulnar styloid fracture (Group A) out of which 12 were males and 16 were females with a mean age of 34.4 years and were followed up for 34.6 months while the remaining 19 had distal end radius fracture without associated ulnar styloid fracture (Group B) out of which 7 were males and 12 were females with a mean age of 32.6 years and were followed up for 36.1 months. After detailed clinical examination and radiological work up, all these patients underwent open reduction and internal fixation (ORIF) with fixed angle volar locking plate (Synthes, Switzerland, marketed by Synthes India Pvt Ltd).
Table 1.
Demographic profile of patients in Group A and B
| Group A | Group B | |||||
|---|---|---|---|---|---|---|
| AO type of fracture | A3 | 6 | A3 | 4 | ||
| B3 | 3 | B2 | 1 | |||
| C1 | 4 | B3 | 4 | |||
| C2 | 6 | C2 | 3 | |||
| C3 | 9 | C3 | 7 | |||
| Handedness | Left | 12 | Left | 8 | ||
| Right | 16 | Right | 11 | |||
| Type of trauma | RTA | 20 | RTA | 12 | ||
| Industrial accident | 4 | Fall | 4 | |||
| Fall | 4 | Sports Injury | 2 | |||
| Industrial Accident | 1 | |||||
| Ulnar styloid fracture | Base | 16 | − | |||
| Tip | 12 | |||||
The fracture was exposed by the volar approach of Henry. The volar wrist capsule was left intact to avoid devascularization of the fracture fragments and destabilization of the volar wrist ligaments. The level of the radio-carpal joint was marked by introducing a needle into the joint. Whenever there was articular involvement, the articular surface was reduced and held with K wires if found necessary. After accurate reduction, the length and alignment was verified under image intensifier, and the fracture was fixed with the plate. Satisfactory reduction was defined as <10° of dorsal tilt, <2 mm of radial shortening and <1 mm of articular incongruity [9–11].
After fixation, the stability was checked by moving the wrist joint through the complete range of motion. Associated DRUJ instability was checked with patient under anaesthesia and prior to surgery with patients elbow flexed to 90°. A shuck test was done on the DRUJ at neutral, full pronation, and full supination. More than 0.5 mm of motion at extremities, with no dislocation and soft end point (Grade II shuck) was seen in 3 patients (Group A n = 2, Group B n = 1) and they were give slab in pronation for 6 weeks, whilst in 5 of them (Group A n = 3, Group B n = 2) dislocation of the DRUJ was present at extremes (Grade III shuck) and the DRUJ was transfixed using a K-wire in mid-supination which was removed at 6 weeks. Postoperatively plaster of paris back slab was given to give rest to the operated part (6 weeks in case of DRUJ injury, 2 weeks in rest of the cases). Active finger movements were encouraged immediate post-operatively along with elevation. Supervised physiotherapy in the form of active wrist movements and hand functions pinch and grasp were begun after slab removal. Patients were reviewed at monthly interval for clinico-radiological evaluation and complications if any for 6 months; thereafter patients were evaluated at 6 monthly intervals.
The radiological evaluation was done in terms of radial inclination, radial length, volar angle and the ulnar variance on Posterio anterior (P.A) and lateral radiographs. On P.A radiographs of the wrist; the radial length was measured as the distance between two lines perpendicular to the long axis of the radius, one passing through the tip of radial styloid process and other through the surface of ulnar head. Ulnar variance was measured as the vertical distance between the line drawn parallel to the proximal surface of lunate facet of radius and another line drawn parallel to articular surface of ulnar head. The angle made by distal articular surface of radius with the longitudinal axis was recorded as radial inclination. In lateral view the angle between the line passing through the concave lower articular surface of the radius with the longitudinal axis was measured which gave the value of volar angle.
The clinical assessment included measurement of range of motion of the wrist in terms of flexion, extension, pronation and supination using a goniometer. The grip strength of both the hands was measured using a standard adjustable digital hand grip dynamometer (Takei Scientific Instruments Co. Ltd., Japan) in standing position with elbow in full extension and shoulder neutrally rotated and adducted. The value was recorded in kilograms and as a percentage of the normal side.. Subjective assessment was done by using the DASH questionnaire [12].
At the time of final follow up, the two groups were compared clinically as well as radio-logically with each other using the student paired t test, and the outcome assessment was done on the basis of Demerit point system of Saito [13]. Data was analyzed using the IBM SPSS version 19, and a p-value < 0.05 was considered statistically significant.
Results
At the time of final follow up all the distal end radius fractures united. In Group A, 17 patients had ulnar styloid non union and 11 had union of the ulnar styloid. We, grouped and compared the functional outcome in both these subgroups. The difference came out to be insignificant (p > 0.05). The average time for consolidation of the fracture in Group A was 9.4 weeks (Fig. 1) as compared to 10.2 weeks in Group B, however the difference was found to be statistically insignificant. It was observed, that both the groups attained excellent range of motion, however flexion and extension in the group with no associated fracture of the ulnar styloid was slightly more as compared to the other group. The grip strength and rotations were better in the group with ulnar styloid fracture (Table 2). The above differences were found to be statistically insignificant by student t test. The average DASH scores was 4.4 in Group A and 3.8 in Group B. Immediate post operatively the radiological parameters were measured and compared with those at final follow up to calculate any loss sustained with settling of fracture (Table 3). The losses so sustained were insignificant inside Group A and Group B. Also when Group A and B were compared with each other for loss of reduction for all four radiological parameters, the differences were insignificant. According to Demerit point system of Saito, in Group A there were 78.5 % excellent (n = 22), 17.9 %, good (n = 05), 3.6 % fair (n = 01), and none poor. In Group B there were 78.9 % excellent (n = 15), 15.8 % good (n = 03), 5.3 % fair (n = 01) and none poor.
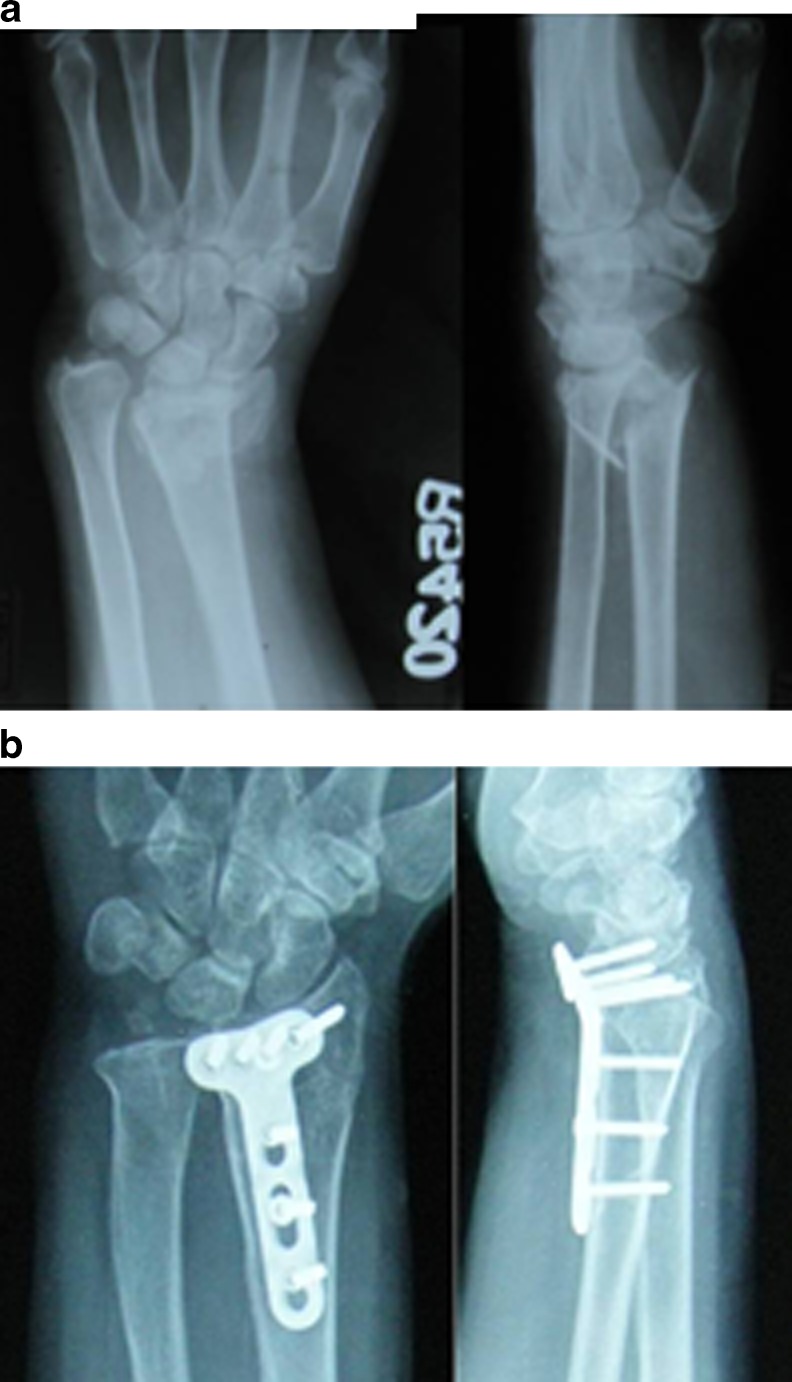
Fig. 1.
a Preoperative radiographs of a 45 years old female in Group A. b Radiographs at final follow-up of 32 months showing union of the distal radius fracture and non union of the ulnar styloid. The patient had excellent range of motion and no complaints
Table 2.
Functional evaluation
| Group A | Group B | P value | |
|---|---|---|---|
| Flexion | 75.32° +/−4.36° | 76.15°+/−6.58° | 0.260 |
| Extension | 72.28° +/− 8.74° | 71.95°+/−5.43° | 0.1840 |
| Supination | 80.38°+/−6.42° | 80.520+/−6.02° | 0.0740 |
| Pronation | 80.93°+/−3.01° | 81.20°+/−5.54° | 0.0820 |
| Grip strenth | |||
| -in kgs | 23.77+/−3.7 kg | 22.59+/−4.48 kg | 0.1660 |
| -as %age of the other side | 94.24 % | 92.05 % | |
Table 3.
Radiological evaluation
| Post op | Final follow up | Loss | P value | ||
|---|---|---|---|---|---|
| Radial inclination | Group A | 23.52°+/−4.12° | 24.34°+/−3.85° | 0.77° | 0.1420 |
| Group B | 23.73°+/−3.25° | 24.42°+/−3.12° | 0.69° | ||
| Radial length | Group A | 12.50°+/−4.15° | 12.62°+/−2.02° | 0.12 mm | 0.2810 |
| Group B | 12.68°+/−2.07° | 12.82°+/−2.42° | 0.14 mm | ||
| Volar angle | Group A | 5.96°+/−6.02° | 5.42°+/−6.85° | 0.54° | 0.0880 |
| Group B | 5.72°+/−8.60° | 5.16°+/−8.42° | 0.56° | ||
| Ulnar variance | Group A | −0.76+/−0.68 mm | −0.54+/−1.2 mm | 0.2 mm | 0.0620 |
| Group B | −0.91+/−1.06 mm | −0.63+/−1.4 mm | 0.28 mm | ||
As far as complications are concerned, in Group A there were 2 cases of loss of reduction. The first case had collapse of the fracture and developed increased post-operative loss of ulnar variance, with distal end of ulna impinging into the carpal bones resulting in persistent ulnar sided wrist pain (Fig. 2). The second case had lunate impaction injury of the distal Radius (Die punch Fracture), obtained after a fall on ship board in a 50 years old male. The compression failure of the metaphysis produced a void, which subsequent increased chances of loss of alignment. Radiographs at final evaluation revealed fracture healing with loss of reduction involving the lunate facet of the radius and collapse of the middle column. In Group B there was one case of loss of reduction with dorsal collapse of the fracture which resulted in fracture healing in a residual dorsal tilt. Though the initial radiographs confirmed adequate reduction, the subchondral screws failed to provide adequate fixation for the fracture. There was another case of carpal tunnel syndrome which was managed conservatively.
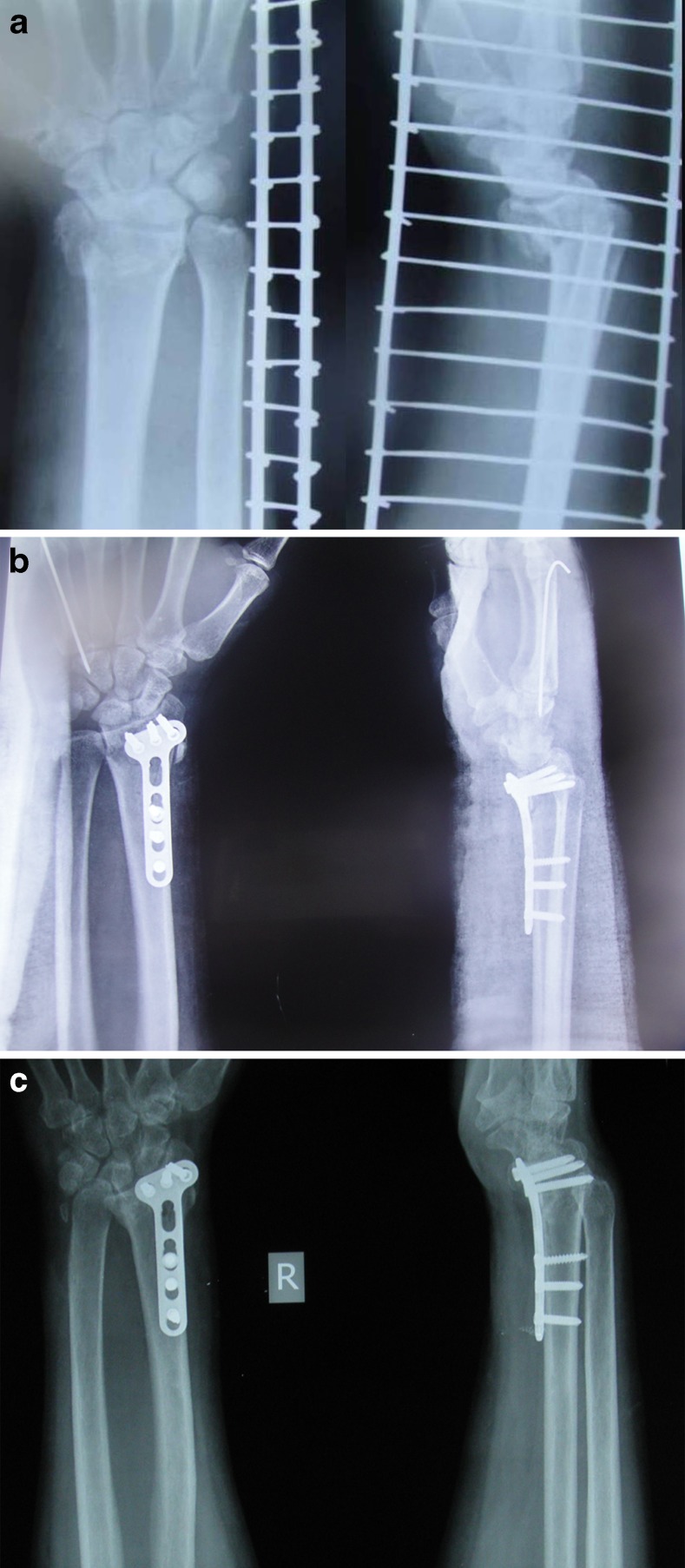
Fig. 2.
a Preoperative radiographs of fracture of the distal end of the radius and ulnar styloid in a 48 years old male b Postoperative radiographs showing adequate reduction. c This patient had collapse of the fracture and developed increased post-operative loss of ulnar variance, with distal end of ulna impinging into the carpal bones
Discussion
Ulnar styloid fracture is commonly associated with distal radius fracture. Reported rates of the association of the two have been between 50 and 65 % [14–18]; in our study the rate of this fracture was 59.57 %. Whether to fix the ulnar styloid or not is surgeons dilemma. While there are studies which opine that fixation avoids symptomatic instability and nonunion, others find that the presence or absence of an associated ulnar styloid fracture, does not affect the final outcome [2–8] .
In a study on 91 cases, Belloti et al. found that patients with both fractures had worse wrist pain and worse scores on the DASH questionnaire than the patients with an isolated distal radius fracture when both were managed by fixation. They were of the opinion that ulnar styloid fractures may be a predictive factor of worse functional outcome for distal radius fracture. Pinning and above-the-elbow casting, used to treat ulnar styloid fractures, led to better function [5]. Souer et al. found no significant differences between patients with an unrepaired fracture of the ulnar styloid base and those with no ulnar fracture in cases of DRF treated by volar locking plate. However, they observed less grip strength as compared to normal side at 6 months, 71 % in the group with ulnar styloid fracture as compared with 79 % in the control group. They also found less wrist flexion (54° compared with 59°); and ulnar deviation (32° compared with 36°) at 24 months after surgery in patients with an untreated fracture of the ulnar styloid base [7].
The possible speculations for sources of ulnar sided wrist pain after distal end radius fractures are an ulnar styloid fracture with TFCC injury, irritation from a non-united fragment, impingement of the extensor carpi ulnaris tendon sheath by a fibrous non-union of the styloid, DRUJ subluxation. Thus, imaging in the form of CT scan or MRI can aid in identifying cause of the painful wrist. Evaluation using CT scan also aids in diagnosing associated carpal bone injuries [19]. Spence et al. have found on MRI scans that an intra-articular soft tissue injury accompanies the distal radial fractures in 47.6 % cases. They reported that the scapholunate ligament was found to be ruptured in 28.6 % cases while TFCC disruption was seen in only 9.5 %. They also found that a rupture of the TFCC was rare with an ulnar styloid fracture [20]. However, the current study strongly suggests that non-union of the ulnar styloid fracture is not always associated with pain or wrist dysfunction. In our study only one patient in group A complained of ulnar sided wrist pain, though 17 had non-union. Zenke et al. and Buijze and Ring have also found that there exists no relationship between ulnar sided wrist pain and union of the ulnar styloid fracture [3, 4].
Sammer et al. studied 144 patients with a stable DRUJ after ORIF for a DRF. They found that in these patients, the presence of an ulnar styloid fracture did not affect the Michigan Hand Outcomes Questionnaire (MHQ). Furthermore, the size of the ulnar styloid fracture, the degree of displacement, and the healing status of the ulnar styloid did not affect MHQ scores [6]. Kim et al. studied 180 consecutive patients who underwent surgical treatment of an unstable distal radial fracture and did not find a significant relationship between wrist functional outcomes and an associated ulnar styloid fracture [8].
Zenke et al. in study on a total of 118 consecutive patients with a fracture of the distal radius treated with a volar locking plate found that 50 patients had no ulnar styloid fracture, 41 had a basal ulnar styloid fracture and 27 had a fracture of the tip of the ulnar styloid. There were no significant differences in radiological and clinical results among the three groups [3]. In their study of 112 patients with distal radius fractures treated with volar plates Kazemian et al. found that untreated stable or minimally displaced ulnar styloid fracture accompanied by distal radius fracture, have no adverse effect on DRUJ stability following ORIF of the radius [21]. In a retrospective study on 182 patients with distal radius fracture, Li et al. found that there was no significant difference in the wrist function in the group with associated ulnar styloid fracture and those with isolated distal radius fractures. The management in this series was done by closed reduction and casting or ORIF as needed for the DRF but the associated ulnar styloid fracture were not fixed in any of these groups. This study reinforced the importance of anatomical reduction of distal radial fracture in the treatment of distal radial fracture accompanying ulnar styloid fracture [22].
Our study had its own set of limitations. Firstly, the sample population was small. Secondly, we did not have any information about the soft tissue element of the injury as we did not perform any MRI evaluation. Finally a longer follow-up period would have been desirable. The strength of the study is that it is a single institutional study with cases operated by the same team of surgeons.
To conclude, ulnar styloid fracture does not affect the outcome of an adequately fixed distal end radius fracture and non-union of ulnar styloid has little influence on the outcome of distal radius fracture. We urge caution in electing operative treatment of non-united fracture of the ulnar styloid until better scientific report for treatment of pain associated with these fracture is available.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg. 2001;26A:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Szabo RM. Distal radioulnar joint instability. J Bone Joint Surg Am. 2006;14:884–894. doi: 10.2106/00004623-200604000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg. 2009;91B:102–107. doi: 10.1302/0301-620X.91B1.21026. [DOI] [PubMed] [Google Scholar]
- 4.Buijze GA, Ring D. Clinical impact of united versus nonunited fractures of the proximal half of the ulnar styloid following volar plate fixation of the distal radius. J Hand Surg. 2010;35A:223–227. doi: 10.1016/j.jhsa.2009.10.035. [DOI] [PubMed] [Google Scholar]
- 5.Belloti JC, Moraes VY, Albers MB, et al. Does an ulnar styloid fracture interfere with the results of a distal radius fracture? J Orthop Sci. 2010;15:216–222. doi: 10.1007/s00776-009-1443-7. [DOI] [PubMed] [Google Scholar]
- 6.Sammer DM, Shah HM, Shauver MJ, Chung KC. The effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg. 2009;34A:1595–1602. doi: 10.1016/j.jhsa.2009.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Souer JS, Ring D, Matschke S, Audige L, Marent-Huber M, Jupiter JB. Effect of an unrepaired fracture of the ulnar styloid base on outcome after plate-and-screw fixation of a distal radial fracture. J Bone Joint Surg. 2009;91A:830–838. doi: 10.2106/JBJS.H.00345. [DOI] [PubMed] [Google Scholar]
- 8.Kim JK, Koh YD, Do NH. Should an ulnar styloid fracture be fixed following volar plate fixation of a distal radial fracture? J Bone Joint Surg. 2010;92A:1–6. doi: 10.2106/JBJS.H.01738. [DOI] [PubMed] [Google Scholar]
- 9.Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg. 2006;31(3):359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Gogna P, Selhi HS, Singla R, Mohindra M, Batra A, Mukhopadhyay R, Rohilla R, Yadav U. Osteosynthesis with long volar locked plates for metaphyseo-daiphyseal fractures of the distal radius. Chin J Traumatol. 2013;16(6):339–343. [PubMed] [Google Scholar]
- 11.Gogna P, Selhi HS, Singla R, Devgan A, Magu NK, Mahindra P, Yamin M (2013) Dorsally comminuted fractures of the distal end of the radius: Osteosynthesis with Volar Fixed Angle Locking Plates. ISRN Orthopaedics. Article ID 131757, 6 pages [DOI] [PMC free article] [PubMed]
- 12.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Saito H, Shibata M. Classification of fracture at the distal end of the radius with reference to treatment of comminuted fractures. In: Boswick JA, editor. Current concepts in hand surgery. Philadelphia: Lea & Febiger; 1983. pp. 129–145. [Google Scholar]
- 14.Frykman G. Fracture of the distal radius including sequelae—shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand Suppl. 1967;108:1–155. doi: 10.3109/ort.1967.38.suppl-108.01. [DOI] [PubMed] [Google Scholar]
- 15.Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg. 1997;22:638–643. doi: 10.1016/S0266-7681(97)80364-6. [DOI] [PubMed] [Google Scholar]
- 16.Oskarsson GV, Aaser P, Hjall A. Do we underestimate the predictive value of the ulnar styloid affection in Colles fractures? Arch Orthop Trauma Surg. 1997;116:341–344. doi: 10.1007/BF00433986. [DOI] [PubMed] [Google Scholar]
- 17.Richards RS, Bennett JD, Roth JH, Milne K., Jr Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg. 1997;22A:772–776. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 18.Tsukazaki T, Iwasaki K. Ulnar wrist pain after Colles’ fracture. 109 fractures followed for 4 years. Acta Orthop Scand. 1993;64:462–464. doi: 10.3109/17453679308993668. [DOI] [PubMed] [Google Scholar]
- 19.Gogna P, Singla R, Gupta RK. Carpal bone fractures in distal radial fractures: is computed tomography expedient ? Clin Orthop Surg. 2014;6:101–102. doi: 10.4055/cios.2014.6.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spence LD, Savenor A, Nwachuku I, Tilsley J, Eustace S. MRI of fractures of the distal radius: comparison with conventional radiographs. Skelet Radiol. 1998;27(5):244–249. doi: 10.1007/s002560050375. [DOI] [PubMed] [Google Scholar]
- 21.Kazemian GH, Bakhshi H, Lilley M, Emami Tehrani Moghaddam M, Omidian MM, Safdari F, Mohammadpour I. DRUJ instability after distal radius fracture: a comparison between cases with and without ulnar styloid fracture. Int J Surg. 2011;9(8):648–651. doi: 10.1016/j.ijsu.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Li S, Chen Y, Lin Z, Fan Q, Cui W, Feng Z. Effect of associated ulnar styloid fracture on wrist function after distal radius. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012;26(6):666–670. [PubMed] [Google Scholar]