Abstract
Arthrodesis of the distal interphalangeal joint of the hand is a reliable procedure for creating a painless stable joint. Numerous techniques are described within the literature for varying indications. We undertook a systematic review of all studies published within the English literature to provide a comparison of the different techniques. The published studies were predominantly of Level IV evidence. The most commonly employed techniques were Kirschner wire, headless compression screw and cerclage wires. There was no difference in infection rates. Headless compression screws appear to have increased union rates but are associated with complications not seen with other well-established and cheaper techniques. The screw diameter is often similar to or larger than the joint itself, which can result in penetration. Furthermore, they limit the available angle for achieving fusion. Other than in terms of union, there is insufficient evidence to show the headless compression screw is superior to other techniques.
Keywords: Arthrodesis, Review, Distal interphalangeal joint, Hand, Techniques
Introduction
Arthrodesis of a finger distal interphalangeal joint (DIPJ) or a thumb interphalangeal joint (IPJ) is predominantly undertaken for a painful degenerate joint. This may be due to osteoarthritis, inflammatory arthropathy, post-traumatic condition such as chronic mallet deformity and infection. Other indications include instability or hyperextension deformity. Moberg and Henrickson stated that ‘the prime requisites of a good digital arthrodesis are a painless and stable union in a proper position and in a reasonable space of time’ [1]. To this end, several techniques have been described for both preparation of the bone ends and the methods of stabilization.
The bones ends can be prepared as two straight surfaces [1], chevron [2], cup and cone [3], or as a tenon [4]. The straight surfaces are simplest but do not provide highest intrinsic bony stability to the construct. The other techniques are more surgically demanding but do provide better inherent stability. Furthermore, in the cup and cone preparation, the position of arthrodesis can be adjusted following bone preparation.
Early methods of bone fixation involved the use of Kirschner wires, either two crossed [5] or one single wire and the use of a supplementary plaster cast [6]. In order to reduce the period of finger immobilisation, Tupper developed an external device though this can interfere with adjacent digits’ function [7]. It has been shown that compression with a modified Charnley clamp could accelerate fusion in comparison to Kirschner wires (K wires) [8]. Various other stabilization methods have been utilised to provide compression at the arthrodesis site such as tension band wire [9], lag screw [10] and headless compression screw [11].
There is no universal agreement on the best technique. The aim of this study is to perform a systematic review on the various techniques of arthrodesis of the DIPJ of the fingers and the IPJ of the thumb with a view to elucidate the safest and most reliable technique of stabilization.
Methods
Selection Criteria
The inclusion criteria for the study were any randomized controlled trials, non-randomized or quasi-randomized controlled trials, prospective cohort trials and retrospective cohort studies of patients who underwent fusion of the DIPJ of the fingers or the IPJ of the thumb.
The exclusion criteria were: 1) patients undergoing revision arthrodesis; 2) studies that included arthrodesis of other joints and in combined studies where it was not possible to extract the data for the DIPJ; 3) case reports, reviews, biomechanical studies, description of technique only and animal studies; 4) studies not available in English.
Literature Search
The following sources of data were searched up to 28th February 2014: Medical Literature Analysis and Retrieval System online (MEDLINE, Bethesda, MD, USA) and the Exerpta Medica Database (EMBASE, Amsterdam, The Netherlands), The Cochrane Library and Google Scholar using the search strategy of (‘DIPJ fusion’) OR (‘DIPJ Arthrodesis’) OR (‘Distal Interphalangeal Joint Arthrodesis’) OR (‘Distal Interphalangeal Joint Fusion’) OR (‘Digital Arthrodesis’) OR (‘Digital Fusion’) OR (‘Small Joint Fusion’) OR (‘Small Joint Arthrodesis’) OR (Finger Fusion] OR (Finger Arthrodesis) OR (Thumb Fusion] or [Thumb arthrodesis], with limitation to the English language but not on the year of publication. In addition we searched the following journals using the same terms: European Journal Hand Surgery, American Journal Hand Surgery, American Journal Bone Joint Surgery, Bone Joint Journal. The bibliographies of all included papers were cross- referenced and further papers obtained where appropriate.
Data Extraction and Analysis
The titles and abstracts of the citations were screened against the eligibility criteria. The patient demographics (sample size, age, gender) surgical indication, review criteria (follow-up, loss to follow-up and methodology), study design and level of evidence, intervention (bone preparation, fixation method, treatment protocol) and assessment of outcome including all documented complications and scoring systems were extracted where the information was available. Extraction of results from graphs in trial reports was considered where data were not provided in the text or tables.
An analysis was performed using RevMan analysis software (RevMan 5.1.6) of the Cochrane Collaboration.
Results
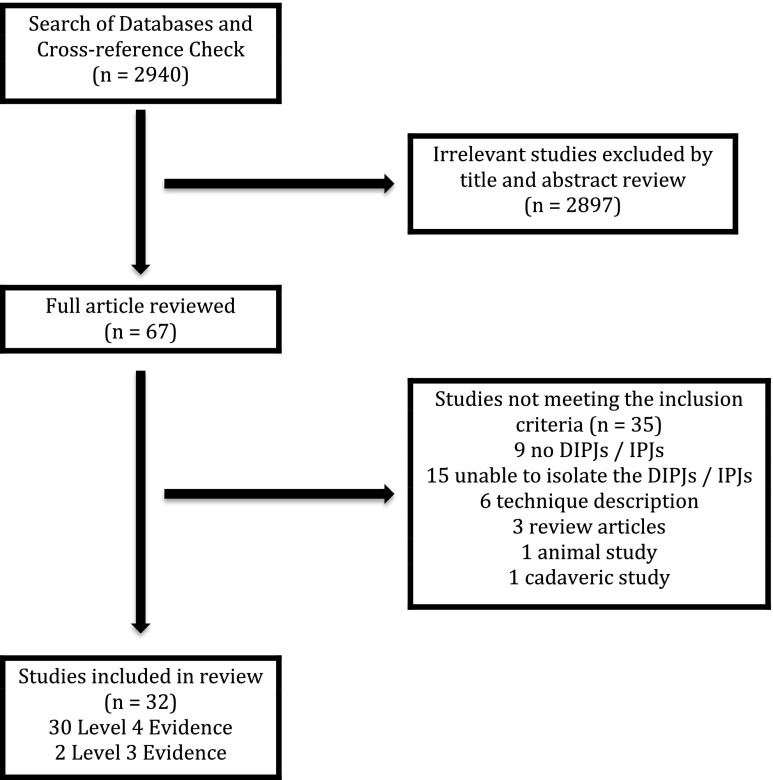
The literature search yielded 2940 articles; 2908 were excluded because they did not fulfil the selection criteria. 32 studies (1125 digits) were included for further analysis. Figure 1 shows a flowchart of how these studies were selected.
Fig. 1.
Flowchart illustrating the selection of studies included in the systematic review
Table 1 shows the details of the studies included based on the surgical techniques. Our analysis revealed 7 groups based on the surgical intervention as follows: eight K-wire studies (389 joints), four interosseous wire studies (114 joints), three headed screw studies (47 joints), 13 headless compression screw studies (492 joints), three absorbable rod studies (37 joints), one plate fixation study (15 joints) and three external fixation studies (31 joints). There were two studies (6 %) with level 3 and the remainder (94 %) with level 4 evidence.
Table 1.
Details of the studies included in the review, including level of evidence, demographic details, method of bone preparation, fixation method, treatment and follow-up protocol
| Paper Type and Name | Level of Evidence | Joint No | Sex | Age | Follow up Period | Follow Up Protocol | Fusion Position | Bone End Preparation | Bone Grafting | Period of Immobilisation |
|---|---|---|---|---|---|---|---|---|---|---|
| Headless Compression Screw | ||||||||||
| Konan [12] | Level IV | 38 | 9 M 26 F | 59 (30–83) | minimum 6 months | Stated | 0 | flat | none | Splint for 6 weeks |
| Song [13] | Level IV | 23 | 6 M 16 F | 54 (22–77) | not stated | Stated | 0–10 | flat | none | None |
| Brutus [14] | Level IV | 27 | 10 M, 12 F | 47 (38–60) | minimum 3 months | Stated | 0–10 | flat | none | Splinting for 2–4 weeks |
| Iwamoto [15] | Level IV | 28 | 2 M 21 F | 65 (58–74) | minimum 6 months | Stated | 0–10 | flat | none | Splint for 2 weeks |
| Cox [16] | Level IV | 48 | 5 M, 24 F | 59 (35–80) | 12 months (2–50) | Not stated | zero | flat | none | 6 weeks |
| Villani [17] | Level IV | 102 | 3 M, 56 F | 61 (43–80) | minimum of 7 months | Not stated | 0 | flat | none | 4–8 weeks |
| Ruchelsman [18] | Level IV | 2 | 1 M 1 F | 27, 79 | minimum 6 weeks | Not stated | 0 | flat | none | initially! |
| Matsumoto [19] | Level IV | 89 | 3 M, 57 F | 62 (36–89) | minimum 5 months | Not stated | 0 | flat | none | Splint for 6 weeks |
| El-Hadidi [20] | Level IV | 13 | 8 M, 5 F | 26 (15–51) | minimum 3 years | Not stated | 0 | flat | none | none stated |
| Faithfull [11] | Level IV | 11 | Not Stated | Not Stated | Not Stated | Not stated | flat | none | None | |
| Kocak [21] | Level IV | 64 | M 17 34 F | 57 (19–89) | minimum 3 months | Not stated | 0 | cup and cone | none | Splint for 2 days |
| Lamas-Gomez [22] | Level IV | 20 | 6 M 14 F | 53 (22–73) | minimum 6 months | Not stated | 10 | flat | none | 10 days |
| Stern [23] | Level III | 27 | Not Calculable | Not Calculable | Not Calculable | Not stated | Not Stated | flat | none | Not Stated |
| Headless Compression Screw Total | 1 Level III, 12 Level IV | 492 | Not Calculable | Not Calculable | Variable | Variable | Up to 10° | Variable | None | Variable |
| K-wire Studies | ||||||||||
| Carroll [3] | Level IV | 79 | not stated | not stated | not stated | Not stated | 25 | cup and cone | none | 6 weeks |
| Engel [24] | Level III | 15 | not stated | not stated | not stated | Stated | 0 | cup and cone | none | 4–12 weeks |
| Moberg [1] | Level IV | 21 | not stated | not stated | not stated | Not stated | Not stated | flat | Yes | not stated |
| Pribyl [2] | Level IV | 4 | Not able to separate | not able to separate | not stated | Not stated | not stated | chevron | none | until fusion occurred |
| Burton [25] | Level IV | 59 | Not able to separate | not able to separate | not stated | Stated | 10–20 | flat | Yes | 3–5 weeks |
| Stern [23] | Level III | 111 | Not able to separate | not able to separate | Not stated | Not stated | flat | not stated | not stated | |
| Lewis [4] | Level IV | 57 | Not able to separate | not able to separate | until fusion occurred | Stated | Not stated | tenon | none | Splint for 6 weeks |
| K-Wire Total | 2 Level III, 5 Level IV | 346 | Not Calculable | Not Calculable | Variable | Variable | Up to 25° | Variable | Variable | Variable |
| Headed Screw Studies | ||||||||||
| Engel [24] | Level III | 15 | not stated | not stated | not stated | Stated | 0 | not stated | none | 1 week |
| Olivier [26] | Level IV | 18 | Not able to separate | 48 (15–72) | minimum 6 months | Not stated | 0 | Flat | Bone chips | 4 weeks |
| Teoh [27] | Level IV | 14 | 15 M 7 F | 35.4 (19–64) | minimum 2 months | Not stated | 25 | flat | none | None |
| Headed Screw Total | 1 Level III, 2 Level IV | 47 | Not Calculable | Not Calculable | Variable | Variable | Up to 25° | Variable | Variable | Variable |
| Plate Study | ||||||||||
| Mantovani [28] | 1 Level IV | 15 | 8 M, 3 F | 41 (23–73) | minimum 18 months | Not Stated | 0–5 | Flat | None | 1 week |
| Interosseous Wire Studies | ||||||||||
| Stern [23] | Level III | 43 | Not able to separate | not able to separate | not able to separate | Not Stated | Not stated | flat | not stated | not stated |
| Shanker [29] | Level IV | 37 | Not able to separate | not able to separate | not able to separate | Not Stated | Not stated | flat | none | None |
| Lister [30] | Level IV | 33 | Not able to separate | not able to separate | not stated | Not Stated | not stated | variable | none | not stated |
| Stahl [31] | Level IV | 20 | Not able to separate | not able to separate | minimum 18 months | Not Stated | Not stated | flat | none | 4–6 days |
| Zavitsanos [32] | Level IV | 24 | not stated | 58 (29–78) | minimum 18 weeks | Not Stated | 0 | flat | none | not stated |
| Interosseous Wire Total | 1 Level III, 4 Level IV | 114 | Not calculable | Not Calculable | Variable | Not Stated | Not stated | Variable | None | Variable |
| External Fixator Studies | ||||||||||
| Leonard [33] | Level IV | 16 | Not able to separate | 22–65 | not stated | Not stated | Not stated | ball and socket | none | 6 weeks whilst ex-fix on! |
| Seitz [34] | Level IV | 4 | 3 M, 1 F | 54 (47–66) | not stated | Stated | not stated | cup and cone | none | 4–6 weeks (Ex-FIX in situ) |
| Wexler [35] | Level IV | 11 | Not able to separate | not able to separate | not stated | Not stated | not stated | flat | none | 4 weeks |
| Ex Fix Total | 3 Level IV | 31 | Not Calculable | Not Calulable | not stated | Variable | Not stated | Variable | None | 4–6 weeks |
| Resorbable pegs Studies | ||||||||||
| Sabbagh [36] | Level IV | 15 | Not able to separate | not able to separate | minimum 2 years | Not stated | 30–50 | flat | none | 2 weeks |
| Arata [37] | Level IV | 16 | 11 M 5 F | 49 (21–64) | minimum 2 months | Stated | 0–20 | flat | none | 3 weeks |
| Harrison [38] | Level IV | 6 | not stated | not stated | not stated | Not stated | not stated | flat | none | 14 days |
| Resorbable pegs total | 3 Level IV | 37 | Not Calculable | Not Calculable | Variable | Variable | Up to 50° | Flat | None | up to 3 weeks |
Out of total 1125 joints, 607 joints were followed-up for 6 weeks to 50 months but no follow-up period was stated for the remaining 518 joints. Union was assessed by clinical assessment alone in one study (3 %), radiological assessment alone in three studies (9 %), by both radiological and clinical assessment in 14 studies (44 %) with the remaining 14 studies not stating how union was assessed (44 %). A follow-up protocol was described in 8 studies (25 %), which consisted of fixed time intervals until fusion occurred.
None of the studies provided a list of assessed complications. Three studies simply stated that no complications were seen. In assessing each complication, we included data where the complication was specifically mentioned.
Table 2 shows the overall union rates, time to union, infection rates and other complications between the different surgical techniques. The number of joints in each group is shown in the brackets.
Table 2.
Details of the outcomes from each study, including union, infection, malunion and complications
| Paper | Union Rate | Malunion | Infection | Nail Abnormality | Metalwork Prominence | Metalwork removal | Cold intolerance | Skin Necrosis | PIPJ stiffness | Fractures | Screw Cut out | Amputation | Paraesthesia |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Headless Compression Screw Studies | |||||||||||||
| Konan [12] | 38/38 | Not stated | 1/38 | 0/38 | 0/38 | 3/38 | Not stated | not stated | Not stated | 2/38 | 2/38 | none | not stated |
| Song [13] | 23/23 | Not stated | 0/23 | 0/23 | 0/23 | 0/23 | Not stated | 0/23 | 0/23 | 0/23 | 0/23 | not stated | 0/23 |
| Brutus [14] | 23/27 | Not stated | 4/27 | 3/27 | 0/27 | 3/27 | not stated | 1/27 | not stated | not stated | 0/27 | none | not sstated |
| Iwamoto [15] | 27/28 | Not stated | 2/28 | 0/28 | 0/28 | 1/28 | not stated | 0/28 | not stated | 1/28 | 0/28 | none | 0/28 |
| Cox [16] | 45/48 | 0/43 | Not stated | 0/48 | 0/48 | not stated | not stated | 0/48 | Not stated | 1/48 | 0/48 | none | not stated |
| Villani [17] | 102/102 | 0/102 | 0/102 | 0/102 | 2/102 | 4/102 | 0/102 | 0/102 | Not stated | 0/102 | 0/102 | none | not stated |
| Ruchelsman [18] | 2/2 | Not stated | Not stated | Not stated | Not stated | Not stated | not stated | not stated | not stated | not stated | not stated | none | not stated |
| Matsumoto [19] | 86/89 | Not stated | 0/89 | 0/89 | 1/89 | not stated | 0/89 | 0/89 | Not stated | not stated | not stated | none | 0/89 |
| El-Hadidi [20] | 12/13 | Not stated | 0/13 | 0/13 | 1/13 | 1/13 | 2/13 | 0/13 | Not stated | not stated | 1/13 | none | not stated |
| Faithfull 1984 | 11/11 | Not stated | 0/11 | 0/11 | 0/11 | 0/11 | Not stated | 0/11 | Not stated | 0/11 | not stated | none | not stated |
| Kocak [21] | 61/64 | Not stated | 1/64 | not stated | 5/64 | 5/64 | not stated | not stated | Not stated | Not stated | not stated | none | not stated |
| Lamas-Gomez [22] | 19/20 | 0/20 | 0/20 | 0/20 | 0/20 | 0/20 | 0/20 | 1/20 | 0/20 | not stated | not stated | 1/20 due to pulp necrosis | not stated |
| Stern [23] | 24/27 | 1/27 | 2/27 | Not stated | 2/27 | not stated | 2/27 | 4/27 | 0/27 | not stated | not stated | none | 3/27 |
| Headless Compression Screw Total | 473/492 (96.1%) | 1/192 (0.5%) | 10/ 442 (2.3%) | 3/399 (0.8%) | 11/490 (2.2%) | 17/326 (5.2%) | 4/191 (2.1%) | 6/377 (1.6%)_ | 0/70 | 4/250 (1.6%) | 3/279 (1.1%) | 1/492 (0.2%) | 3/167 (1.8%) |
| K-wire Studies | |||||||||||||
| Carroll [3] | 72/79 | Not stated | 0/79 | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Engel [24] | 12/15 | not calculable | 1/15 | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Moberg [1] | 17/21 | not calculable | 1/21 | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Pribyl [2] | 4/4 | 0/4 | Not calculable | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Burton [25] | 59/59 | not calculable | 0/59 | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Stern [23] | 98/111 | 4/111 | 6/111 | not stated | 0/111 | not stated | 2/111 | 3/111 | 2/111 | not stated | not stated | not stated | 2/111 |
| Lewis [4] | 55/57 | Not stated | 0/57 | 0/57 | not stated | not stated | not stated | 0/57 | not stated | not stated | not stated | not stated | not stated |
| K-Wire Total | 317/346 (91.6%) | 4/115 (3.5%) | 8/342 (2.3%) | 0/57 | 0/111 | None | 2/111 (1.8%) | 3/168 (1.8%) | 2/111 (1.8%) | none | n/a | none | 2/111 (1.8%) |
| Headed Screw Studies | |||||||||||||
| Engel [24] | 12/15 | not stated | 0/15 | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated | not stated |
| Olivier [26] | 18/18 | Not stated | 2/18 | 1/18 | 0/18 | 2/18 | Not stated | 0/18 | Not stated | Not stated | not stated | Not stated | not stated |
| Teoh [27] | 14/14 | 0/14 | 0/14 | not stated | 0/14 | 0/14 | not stated | 0/14 | not stated | not stated | not stated | not stated | not stated |
| Headed Screw Total | 44/47 (93.6%) | 0/14 | 2/47 (4.3%) | 1/18 (5.6%) | 0/32 | 2/32 (6.25%) | not stated | 0/32 | not stated | not stated | not stated | not stated | not stated |
| Plate Study | |||||||||||||
| Mantovani [28] | 15/15 | 0/15 | 0% | 0/15 | 2/15 | 2/15 | Not stated | 0/15 | 0/15 | 0/15 | N/A | not stated | 0/15 |
| Interosseous Wire Studies | |||||||||||||
| Stern [23] | 38/43 | 1/43 | 4/43 | not stated | 0/43 | not stated | 2/43 | 1/43 | 3/43 | not stated | n/a | not stated | 0/43 |
| Shanker [29] | 32/37 | Not stated | Not calculable | Not calculable | Not calculable | Not calculable | Not calculable | not stated | not stated | not stated | n/a | not stated | not stated |
| Lister [30] | 30/33 | Not stated | 0/33 | not stated | 3/33 | 3/33 | not stated | not stated | not stated | not stated | n/a | not stated | not stated |
| Stahl [31] | 20/20 | Not stated | 0/20 | Not calculable | Not calculable | Not calculable | Not calculable | Not calculale | Not stated | Not stated | n/a | not stated | not stated |
| Zavitsanos [32] | 23/24 | 0/24 | 1/24 | 0/24 | 2/24 | 2/24 | not stated | 0/24 | 0/24 | not stated | N/A | not stated | not stated |
| Interosseous Wire Total | 143/157 (91.1%) | 1/67 (1.5%) | 5/120 (4.2%) | 0/24 | 5/100 (5%) | 5/57 (8.8%) | 2/43 (4.7%) | 1/67 (1.5%) | 3/67 (4.5%) | not stated | n/a | not stated | 0/43 |
| External Fixator Studies | |||||||||||||
| Leonard [33] | 15/16 | Not stated | 0/16 | not stated | N/a | N/A | Not stated | not stated | not stated | not stated | N/A | not stated | not stated |
| Seitz [34] | 3/4 | 0/4 | 0/4 | 0/4 | 0/4 | N/A | Not stated | not stated | not stated | 0/4 | N/A | not stated | not stated |
| Wexler [35] | Not calculable | 2/11 | 0/11 | not calculable | not calculable | N/A | Not stated | 0/11 | not stated | not stated | N/A | not stated | not stated |
| Ex Fix Total | 18/20 (90%) | 2/15 (13.3%) | 0% | 0/4 | 0/4 | N/A | not stated | 0/11 | not stated | 0/4 | n/a | not stated | not stated |
| Resorbable pegs Studies | |||||||||||||
| Sabbagh [36] | not able to separate | Not stated | 3/15 | Not calculable | N/A | N/A | not stated | not stated | Not stated | Not stated | N/A | not stated | not stated |
| Arata [37] | 16/16 | 0/16 | 0/16 | 0/16 | N/A | N/A | not stated | 0/16 | not stated | 0/16 | N/A | not stated | not stated |
| Harrison [38] | 6/6 | Not stated | Not stated | not stated | N/A | N/A | not stated | not stated | Not stated | Not stated | N/A | not stated | not stated |
| Resorbable pegs total | 22/22 | 0/16 | 3/37 (8.1%) | 0/16 | N/a | N/A | not stated | 0/22 | 0/6 | 0/22 | 0/6 | ||
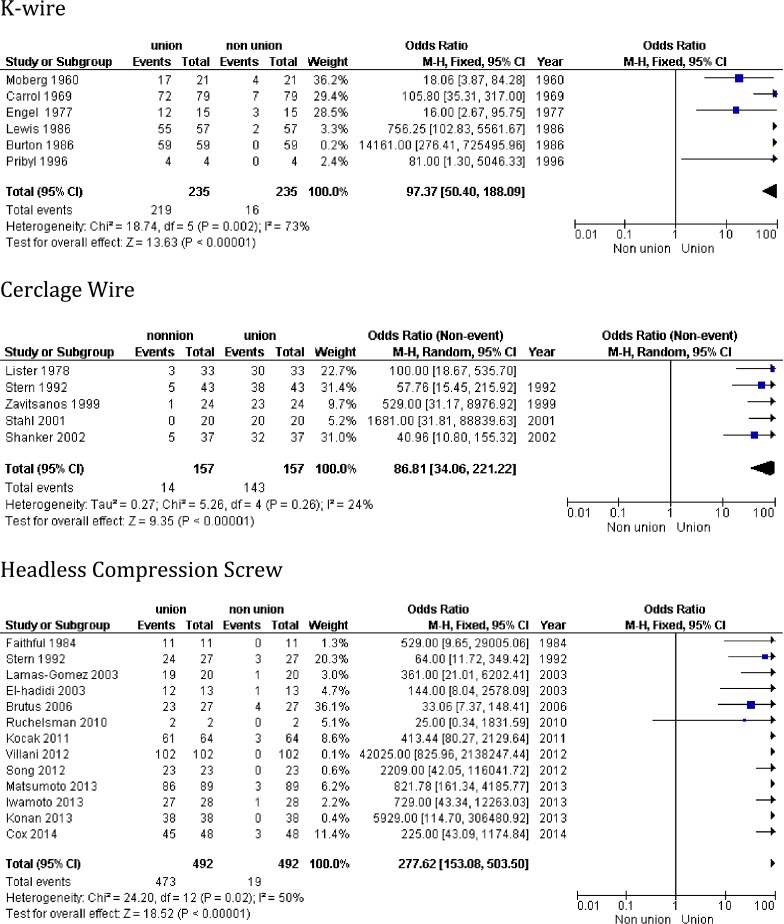
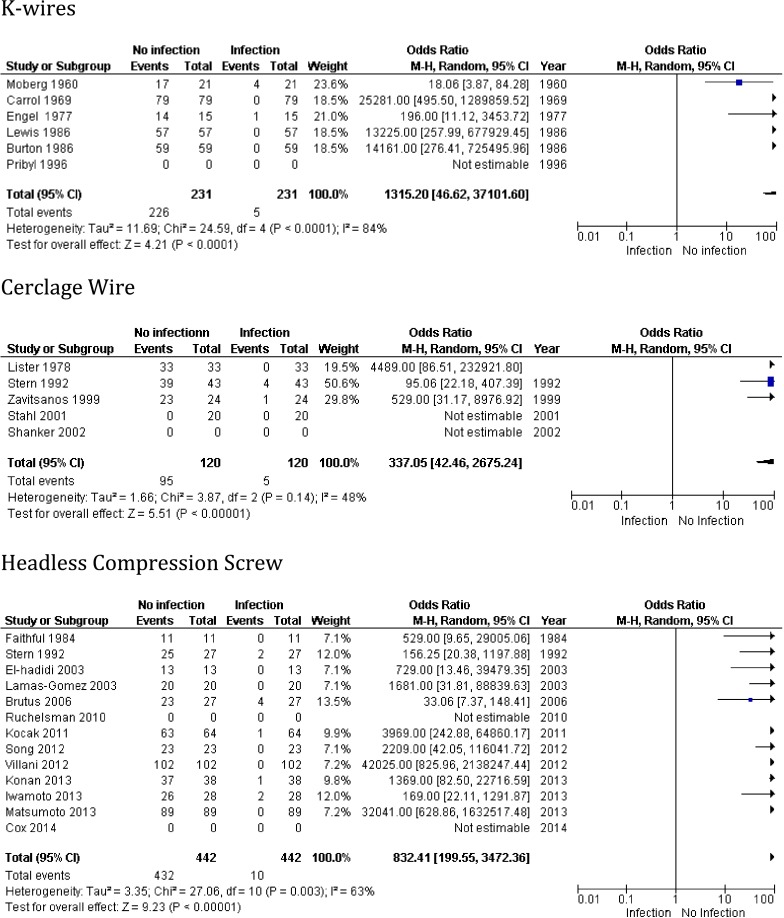
Due to the quality of the data available, only two outcome measures (union rate and infection rate) were amenable for further analysis in order to generate odds ratios of occurrence among the three most commonly employed techniques (Kirschner wire, headless compression screw and cerclage wires). These are shown in Figs. 2 and 3. The rates of non-union and infection were compared using Fisher Exact test and the results are shown in Table 3.
Fig. 2.
The Forest plots with Odds Ratios for K-wires, Cerclage wires and Headless Compression Screw respectively
Fig. 3.
Forest Plots and Odds Ratios for Infection using K-wires, Cerclage wire and Headless Compression Screws respectively
Table 3.
Fisher exact method results showing differences in infection and union rates between the three main methods
| Technique | Infection Rate | P-value compared to Technique | Union rate | P-value compared to Technique | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Not Infected | Infected | K-wire | Cerclage | Headless Compression | Union | Non-Union | K-wire | Cerclage | Headless Compression | |
| K-wire | 342 | 8 | N/A | 0.35 | 1 | 346 | 29 | N/A | 0.86 | <0.01 |
| Cerclage | 115 | 5 | 0.35 | N/A | 0.34 | 143 | 14 | 0.85 | N/A | 0.02 |
| Headless Compression | 432 | 10 | 1 | 0.34 | N/A | 473 | 19 | <0.01 | 0.02 | N/A |
A patient rated outcome score was reported in 4 studies. Only one paper reported the time of return to work. No analyses were possible in either of these parameters.
Discussion
A wide range of surgical techniques have been described for achieving arthrodesis of the DIPJ. Literature search revealed that the published studies are predominantly case series of Level 4 evidence, which highlights a lack of good quality data to guide surgical choice. Nevertheless, the majority of joints were fused with Kirschner wires, interosseous wiring or headless compression screws. Each of these three techniques has over 100 joints when the results from studies were collated. We have, therefore, performed statistical analysis of these three techniques. The results however should be interpreted with caution due to the levels of evidence of the studies as well as the heterogeneous mix of patients in terms of age and surgical indications. It is notable that of the 12 papers published within the last 10 years which had been included in our review, 9 of them reported the results of headless compression screws. None of the studies reported the use of Kirschner wires since 1996. This may represent a shift amongst hand surgeons to using headless compression screws or a publication bias.
The odds ratios showed strong trends towards both union and no infection in all three techniques. In comparing the techniques with each other there was also no difference in the infection rates but there was a statistically increased rate of union with the headless compression screw when compared to either the K-wire (p < 0.01) or cerclage wire (p = 0.02). There was no statistically significant difference in the union rates between the K-wires or cerclage wire. However, whilst headless compression screws appear to achieve a higher rate of union there are a number of complications unique to this technique such as 1 % nail abnormalities, 1 % fracture and 1 % screw cut through. Further surgery to remove the screw was required in 5 % of cases, compared with 9 % for cerclage wires, whilst the K-wires can easily be removed in the outpatient setting.
Whilst the surgeon tends to view union and no infection as the main desirable outcomes, there is no comparable patient reported outcome data to show advantage of one technique over another. The cost of a headless compression screw is significantly greater than that for a K-wire (for instance, £205 compared with £8 in our hospital). However headless compression screw may facilitate earlier mobilization and potentially earlier return to work when compared to the wires. The potential savings thus may offset the increased cost of a screw. The risk reward balance of these different techniques and costs to the patient and the healthcare system should be borne in mind when deciding on the choice of implant.
The headless compression screws have been grouped together for the purposes of this review though they vary in shape and size. The Acutrak™ screw has a conical shape with threads along its length, which has been purported to reduce pistoning and increase the surface area for bone purchase [39]. They have also been reported to provide greater compression than Herbert™ screws [40] but there has been no clinical correlation to support one over another. It is also important to note that the screw diameter varies between designs from 2.5 mm for the Acutrak™ screw up to 4.1 mm for the Twinfix™ screw. The average lateral diameter for the distal phalanx also varies in diameter from 3.17 mm in the middle finger to 2.64 mm in the little finger [13]. Mintalucci et al. have found similar problems with a mismatch between the phalangeal and screws sizes [40]. They compared the anteroposterior and lateral dimensions of the phalanx with 16 different headless compression screws and found a mismatch occurred in 66 % index, 53 % middle, 49 % ring and 72 % of little fingers [40]. Indeed they found that only one of these screws, the Acutrak Fusion™, had a compatibility of over 90 % for all DIP joints. This means that in some instances it may not be possible to place a screw without cortical penetration whilst in other cases there is only a very small margin for error. Careful assessment should be made of the size of the phalanx particularly the little finger and if in doubt use a different technique [14, 40]. This is supported by Wyrsch who reported dorsal cortex penetration in 25 out of 30 cadaveric specimens [41]. Conversely, it has also been suggested that headless compression screws should not be used in the phalanges of the thumb as the intramedullary cavity is too wide for adequate purchase [17]. Further studies are required to ascertain whether there is an optimum screw to phalanx diameter ratio. As the diameter of the little phalanx is smaller than that of the index or middle fingers it may be that cortical penetration and nail deformities are higher in this finger, though it has not been possible to establish this from our review as most studies failed to comment on the specific digit the complications occurred in.
There is a wide variety of the optimum angle of fusion within the literature. It has been postulated that most surgeons would fuse the joint in full extension because it is adequate for most work of the hand [24]. Whilst full extension may be cosmetically acceptable this may have an impact on function. For instance in the presence of restricted flexion in the proximal interphalangeal and metacarpophalangeal joints a greater angle of fusion may be required in the DIPJ to optimize function [42, 43]. Straub recommended fusing the joint in the position it would normal rest in, as such the flexion would increase (from radial to ulnar digits) from approximately 10° in the index finger to 40° in the little finger [44]. It would seem sensible to assess the mobility in the proximal joints prior to deciding on the fusion angle. It is important to appreciate that the angle of fusion with retrograde headless compression screw is generally limited to 0–10°. If the screw is placed in an antegrade manner across the joint a greater angle can be achieved but there may be only minimal purchase for the proximal part of the screw within the middle phalanx [24]. It is easier to achieve a greater angle by using other techniques such as Kirschner wires [24].
The success of arthrodesis will be determined not just on surgical technique but also on patient factors, in particular the indication for surgery. Most studies have included multiple indications from traumatic to inflammatory and non-inflammatory arthritis. The soft-tissue envelope, bone stock and bone quality can differ considerably between these conditions. Complication rates of 40 % have been reported in patients with psoriatic arthropathy [23]. Bone stock rather than the fixation method was the greatest determinant of successful arthrodesis in these patients [23]. In addition, in patients with poor bone stock, K-wires have been preferred to screw stabilization due to the poor purchase of the screw into the bone [45]. In the presence of any irregularity use of bone graft (from the condyles, distal radius or iliac crest) has been recommended.
When determining the fixation method of DIPJ arthrodesis, we recommend the following considerations:
What is the desired angle of arthrodesis? If greater than 10° of flexion is required then do not use a compression screw.
Assess the bone stock and quality. If the bone stock is poor, consider supplemental use of bone graft. Consider whether the bone is of sufficient quality to support compression with either the wire or screw.
What is the size of the distal phalanx in relation to the metalwork? Be aware of the diameter of the screw or wire.
Conclusion
With the limited evidence of the studies available, the three most commonly reported techniques for DIPJ fusion in the hand are Kirschner wire, headless compression screw and cerclage wire. There is insufficient evidence to support any particular technique. The technique with the least reported complications appears to be Kirschner wires. Further level one studies with well-matched controls taking into considerations of surgical indications, specific digit, bone preparation techniques, immobilization period, union time, complications and patient reported outcomes, are required.
References
- 1.Moberg E, Henrickson B. Technique for digital arthrodesis: a study of 150 cases. Acta Chir Scand. 1960;118:331–338. [PubMed] [Google Scholar]
- 2.Pribyl CR, Omer GR, Jr, McGinty L. Effectiveness of the chevron arthrodesis in small joints of the hand. J Hand Surg [Am] 1996;21:1052–1058. doi: 10.1016/S0363-5023(96)80315-7. [DOI] [PubMed] [Google Scholar]
- 3.Carroll RE, Hill NA. Small joint arthrodesis in hand reconstruction. J Bone Joint Surg. 1969;51:1219–1221. [PubMed] [Google Scholar]
- 4.Lewis RC, Nordyke MD, Tenny JR. The tenon method of small joint arthrodesis in the hand. J Hand Surg [Am] 1986;11:567–569. doi: 10.1016/S0363-5023(86)80201-5. [DOI] [PubMed] [Google Scholar]
- 5.Bunnel S. Surgery of the hand. 2. Philadelphia: J.B. Lippincott Co.; 1948. [Google Scholar]
- 6.Von Saal FH. Intramedullary fixation in fractures of the hand and finger. JBJS. 1953;35A:5. [PubMed] [Google Scholar]
- 7.Tupper JW. A compression arthrodesis device for small joints of the hands. Hand. 1972;4:62–64. doi: 10.1016/0072-968X(72)90015-0. [DOI] [PubMed] [Google Scholar]
- 8.Micks JE, Hager D. A compression apparatus for fusion of the hand joints. Med Trial Tech. 1970;16:35–37. [PubMed] [Google Scholar]
- 9.Weber BG. Grundlagen und moglichkeiten der juggertungs osteosynthesis. Chirurgie. 1964;35:81. [PubMed] [Google Scholar]
- 10.Muller G, Schoenberger F. Technik der compression arthrodese am finger mittels jug shraube. Handchirurgie. 1970;2:218. [PubMed] [Google Scholar]
- 11.Faithfull DK, Herbert TJ. Small joint fusions of the hand using the Herbert bone screw. J Hand Surg (Br) 1984;9:167–168. doi: 10.1016/S0266-7681(84)80021-2. [DOI] [PubMed] [Google Scholar]
- 12.Konan S, Das A, Taylor E, Sorene E. Distal interphalangeal joint arthrodesis in extension using a headless compressive screw. Acta Ortho Belg. 2013;79:154–158. [PubMed] [Google Scholar]
- 13.Song JH, Lee JY, Chung YG, Park IJ. Distal interphalangeal joint arthrodesis with a headless compression screw: morphometric and functional analyses. Arch Orthop Trauma Surg. 2012;132:663–669. doi: 10.1007/s00402-011-1413-3. [DOI] [PubMed] [Google Scholar]
- 14.Brutus JP, Palmer AK, Mosher JF, Harley BJ, Loftus JB. Use of a headless compression screw for distal interphalangeal joint arthrodesis in digits: clinical outcome and review of complications. J Hand Surg. 2006;31A:85–89. doi: 10.1016/j.jhsa.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Iwamoto T, Matsumura N, Sato K, Momohara S, Toyama Y, Nakamura T. An obliquely placed headless compression screw for distal interphalangeal joint arthrodesis. J Hand Surg [Am] 2013;38A:2360–2364. doi: 10.1016/j.jhsa.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 16.Cox C, Earp BE, Floyd WE, Blazar PE. Arthrodesis of the thumb interphalangeal joint and finger distal interphalangeal joints with a headless compression screw. J Hand Surg [Am] 2014;39:24–28. doi: 10.1016/j.jhsa.2013.09.040. [DOI] [PubMed] [Google Scholar]
- 17.Villani F, Uribe-Echevarria B, Vaienti L. Distal interphalangeal joint arthrodesis for degenerative osteoarthritis with compression screw: results in 102 digits. J Hand Surg [Am] 2012;37A:1330–1334. doi: 10.1016/j.jhsa.2012.02.048. [DOI] [PubMed] [Google Scholar]
- 18.Ruchelsman DE, Hazel A, Mudgal CS. Treatment of symptomatic distal interphalangeal joint arthritis with percutaneous arthrodesis: a novel technique in select patients. Hand. 2010;5:434–439. doi: 10.1007/s11552-010-9265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsumoto T, Nakamura I, Miura A, Momoyama G, Ito K. Distal interphalangeal joint arthrodesis with the reverse fix nail. J Hand Surg [Am] 2013;38A:1301–1306. doi: 10.1016/j.jhsa.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 20.El-Hadidi S, Al-Kdah H. Distal interphalangeal joint arthrodesis with Herbert screw. Hand Surgery. 2003;8:21–24. doi: 10.1142/S0218810403001364. [DOI] [PubMed] [Google Scholar]
- 21.Kocak E, Carruthers KH, Kobus RJ. Distal interphalangeal joint arthrodesis with the Herbert headless compression screw: outcomes and complications in 64 consecutively treated joints. Hand. 2011;5:56–59. doi: 10.1007/s11552-010-9295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lamas Gomez C, Proubasta I, Escriba I, Itarte J, Caceres E. Distal interphalangeal joint arthrodesis: treatment with Herbert screw. J South Orth Ass. 2003;12:154–159. [PubMed] [Google Scholar]
- 23.Stern PJ, Fulton DB. Distal interphalangeal joint arthrodesis: an analysis of complications. J Hand Surg. 1992;17A:1139–1145. doi: 10.1016/S0363-5023(09)91081-4. [DOI] [PubMed] [Google Scholar]
- 24.Engel J, Tsur H, Farin I. A comparison between K-wire and compression screw fixation after arthrodesis of the distal interphalangeal joint. Plast Recon Surg. 1977;60:611–614. doi: 10.1097/00006534-197710000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Burton RI, Margles SW, Lunseth PA. Small-joint arthrodesis in the hand. J Hand Surg. 1986;11A:678–682. doi: 10.1016/S0363-5023(86)80011-9. [DOI] [PubMed] [Google Scholar]
- 26.Olivier LC, Gensigk F, Board TN, Kendoff D, Krehmeier U, Wolfhard U. Arthrodesis of the distal interphalangeal joint: description of a new technique and clinical follow-up at 2 years. Arch Orthop Trauma Surg. 2008;128:307–311. doi: 10.1007/s00402-007-0457-x. [DOI] [PubMed] [Google Scholar]
- 27.Teoh LC, Yeo SJ, Singh I. Interphalangeal joint arthrodesis with oblique placement of an AO lag screw. J Hand Surg. 1994;19B:208–211. doi: 10.1016/0266-7681(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 28.Mantovani G, Fukushima WY, Cho AB, Aita MA, Lino W, Nunes Faria F. Alternative to the distal interphalangeal joint arthrodesis: lateral approach and plate fixation. J Hand Surg [Am] 2008;33A:31–34. doi: 10.1016/j.jhsa.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Shanker HK, Johnstone AJ, Rizzo L, Chesney RB. Pepper-pot arthrodesis of the small joints of the hand: our experience in 68 cases. J Hand Surg. 2002;27B:430–432. doi: 10.1054/jhsb.2002.0798. [DOI] [PubMed] [Google Scholar]
- 30.Lister G. Intraosseous wiring of the digital skeleton. J Hand Surg [Am] 1978;5:427–435. doi: 10.1016/S0363-5023(78)80135-X. [DOI] [PubMed] [Google Scholar]
- 31.Stahl S, Rozen N. Tension-band arthrodesis of the small joints of the hand. Orthopedics. 2001;24:981–983. doi: 10.3928/0147-7447-20011001-19. [DOI] [PubMed] [Google Scholar]
- 32.Zavitsanos G, Watkins F, Britton E, Somia N, Gupta A, Kleinert H. Distal interphalangeal joint arthrodesis using intramedullary and interosseous fixation. Hand Surgery. 1999;4:51–55. doi: 10.1142/S0218810499000125. [DOI] [PubMed] [Google Scholar]
- 33.Leonard MH, Capen DA. Compression arthrodesis of finger joints. Clinc Orth Rel Res. 1979;145:193–198. [PubMed] [Google Scholar]
- 34.Seitz WH, Jr, Sellman DC, Scarcella JB, Froimson AI. Compression arthrodesis of the small joints of the hand. Clin Orthop Rel Res. 1994;304:116–121. [PubMed] [Google Scholar]
- 35.Wexler MR, Rousso M, Weinberg H. Arthrodesis of finger joints by dynamic external compression. Plast Recon Surg. 1977;59:882–885. doi: 10.1097/00006534-197712000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Sabbagh W, Grobbelaar AO, Clarke C, Smith PJ, Harrison DH. Long-term results of distal arthrodesis with the Harrison-Nicolle peg. J Hand Surg. 2001;26B:568–571. doi: 10.1054/jhsb.2001.0649. [DOI] [PubMed] [Google Scholar]
- 37.Arata J, Ishikawa K, Soeda H, Kitayama T. Arthrodesis of the distal interphalangeal joint using a bioabsorbable rod as an intramedullary nail. Scan J Plast Recon. 2003;37:228–231. doi: 10.1080/02844310310016403. [DOI] [PubMed] [Google Scholar]
- 38.Harrison SH, Nicolle PV. A new intramedullary bone peg for digital arthrodesis. Br J Plast Surg. 1974;27:240–241. doi: 10.1016/S0007-1226(74)90081-2. [DOI] [PubMed] [Google Scholar]
- 39.Faran K, Ichioka N, Trzeciak MA, Han S, Medige J, Moy OJ. Effect of bone quality on the forces generated by compressive screws. J Biomech. 1999;32:861–864. doi: 10.1016/S0021-9290(99)00076-7. [DOI] [PubMed] [Google Scholar]
- 40.Mintalucci D, Lutsky KF, Matzon JL, Rivlin M, Niver G, Beredjiklian Distal interphalangeal joint bony dimensions related to headless compression screw sizes. J Hand Surg [Am] 2014;39:1068–1074. doi: 10.1016/j.jhsa.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Wyrsch B, Dawson J, Weikert D, Milek M. Distal interphalangeal joint arthrodesis comparing tension band wire and Herbert screw: a biomechanical and dimensional analysis. J Hand Surg [Am] 1996;21A:438–443. doi: 10.1016/S0363-5023(96)80360-1. [DOI] [PubMed] [Google Scholar]
- 42.Hooper G. Techniques of interphalangeal arthrodesis. In: Bowers WH, editor. The interphalangeal joints. UK: Churchill Livingstone; 1987. pp. 174–180. [Google Scholar]
- 43.Katzman SS, Gibeault JD, Dickson K, Thompson JD. Use of a Herbert screw for interphalangeal joint arthrodesis. Clin Orth Rel Res. 1993;296:127–132. [PubMed] [Google Scholar]
- 44.Straub LR. The rheumatoid hand. Clinical Orthopaedics. 1959;15:127–139. [PubMed] [Google Scholar]
- 45.Tomaino MM. Distal interphalangeal joint arthrodesis with screw fixation: why and how. Hand Clin. 2006;22:207–210. doi: 10.1016/j.hcl.2006.02.015. [DOI] [PubMed] [Google Scholar]