Abstract
Concomitant occurrence of phyllodes tumor with an in situ or invasive carcinoma in the breast is an uncommon phenomenon and has been reported sparingly. We describe a rare case of simultaneous bilateral intraductal and infiltrating duct carcinoma with coexisting fibroadenomas and phyllodes tumor. To the best of our knowledge, only 19 cases of invasive carcinoma with phyllodes tumor have been reported so far and lymph node metastases has been described only once. A 43 year-old woman presented with multiple bilateral breast lumps. Core biopsies revealed phyllodes tumor in the right breast and invasive duct carcinoma of the left breast. Simple mastectomy done for right breast showed foci of invasive carcinoma arising in phyllodes tumor. Metastasis was detected in the left axillary lymph nodes. This case is being reported to create awareness of this rare transformation, which has significant prognostic and therapeutic implications.
Keywords: Breast, Phyllodes, Carcinoma, Invasive, Tumor
Introduction
Coexistence of phyllodes tumor (PT) and carcinoma is uncommon. We report a rare case of bilateral fibroadenomas,phyllodes tumors with development of secondary carcinoma.
Case Report
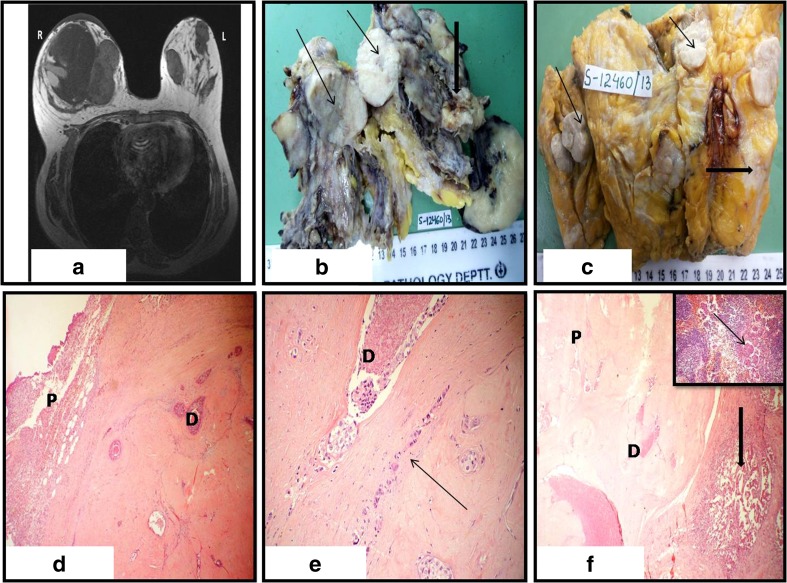
A 43 year-old woman presented with progressively increasing large firm irregular palpable lump in upper quadrant of right breast for one year along with multiple smaller breast lumps in both breasts. Nipple areola and overlying skin were normal. Past history showed that small bilateral mobile lumps had been present for last 20 years. No positive family history was present. Magnetic resonance imaging (MRI) showed a large tumor in right breast with multiple smaller lesions. Left breast showed multiple lesions of size 2 to 4 cm at 3,8,12 o‘clock positions. (Fig. 1a) Core needle biopsies showed invasive carcinoma in left and phyllodes tumor in right breast. Patient underwent left side modified radical mastectomy and simple mastectomy of right side. Grossly, right breast showed a large irregular partly nodular lesion measuring 15 × 10 × 7 cm which was grey white, lobulated with myxoid change. (Fig. 1b) and left breast showed four discrete nodules one of which was firm. (Fig. 1c) Microscopy of right breast showed a complex pathology of fibroadenomas, phyllodes tumor and carcinoma. Phyllodes tumors were benign to borderline with moderate cellularity and pleomorphism and frequent mitotis (5-9/10HPF). Some fibroadenomas showed phyllodes tumor at the periphery. Few hyalinized nodules showed ductal hyperplasia with ductal in situ comedocarcinoma and small foci of invasive carcinoma. (Fig. 1d, e). Left mastectomy microscopy showed multiple fibroadenomas and one nodule of infiltrating duct carcinoma with adjacent borderline phyllodes tumor. (Fig. 1f) which also showed foci of comedocarcinoma and infiltrating duct carcinoma. Two left axillary lymph nodes showed metastasis. Tumor was negative for ER, PR and showed 3+ positivity with Her 2 neu. Diagnosis was consistent with bilateral in -situ and infiltrating duct carcinoma (TNM pT1,pN1,pM0)with borderline phyllodes tumors and fibroadenomas. The patient received adjuvant radiotherapy and is well at six month follow-up.
Fig. 1.
a: MRI showing a large tumor in the right breast(R), occupying nearly the whole of the breast with multiple smaller lesions. Left breast (L) also shows multiple lesions b Grossly, cut surface of right breast showing multinodular lesion. One of the bisected nodule is large and irregular (thick arrow). In addition multiple well defined nodules are seen. (Thin arrows) c Left breast grossly shows multiple circumscribed grey white nodules. (Thin arrows) One of the nodules has ill defined margins (thick arrow) d Microscopy of right breast showing hyalinised nodule of fibroadenoma with ductal carcinoma in situ and comedonecrosis(D). On the left side, phyllodes tumor is seen .(H&Ex10) e Foci of invasive carcinoma (arrow) along with ductal carcinoma in situ in right breast. (H&Ex40) f Microscopy of left breast showing invasive duct carcinoma (thick arrow). Coexisting borderline phyllodes tumor nodule (P) is seen on the left with foci of ductal carcinoma in situ (D). (H&Ex20). Inset showing tumor metastasis (arrow) in left axillary lymph node
Discussion
Phyllodes tumors (PT) is a biphasic neoplasm composed of epithelial and stromal elements accounting for about 1 % of breast tumors [1]. Like fibroadenomas they arise from intralobular stroma but show relative overgrowth of stroma. Histopathologically, they are divided into benign, borderline and malignant categories based on atypia, mitosis per ten high power fields and tumor-normal interface. They are associated with local recurrences. Malignant transformation can be seen in 30 % of PTs mostly as sarcomatous change. Malignant transformation of epithelial elements although rare has been documented as ductal or lobular in situ lesions and infrequently as invasive carcinoma [2]. Lymph node metastasis is extremely rare [3]. Other carcinoma subtypes described are tubular, schirrous and squamous carcinoma [4, 5].
A review of literature shows that age of these cases ranged from 31–80 years with maximum frequency in fifth decade [6]. Carcinomas can coexist with all categories of PT and within the same or contralateral breast [6]. However, carcinoma developing within a phyllodes tumor is rare. Florid epithelial hyperplasia is encountered in phyllodes tumors [7]. Transformation of the hyperplastic epithelium to carcinoma owing to subsequent genetic alterations appears to be the most plausible explanation of this progression. Carcinoma may present simultaneously or develop in the recurrences [7]. The low incidence of breast carcinomas in PT does not support an increased risk of carcinoma in PT [8]. Rosai suggested that PT has capacity to induce glandular formation [9]. In the present case the complex findings of coexistant fibroadenomas, PT, in situ and invasive carcinomas support the fact that stroma and the epithelium can exhibit distinct molecular changes as part of the neoplastic process.
Preoperative assessment of this co- existence is difficult as phyllodes tumor usually takes up a large area. The definite diagnosis therefore relies on detailed histopathologic evaluation. The prognosis of carcinoma in phyllodes tumor is generally favourable in the majority of the cases [3]. This may be due to the relatively small size of invasive component as seen in the present case.
The prognosis of PT depends on type of the PT requiring a wide local excision or simple mastectomy and axillary nodal dissection is not necessary. Presence of coexisting carcinoma considerably alters the management warranting a more extensive surgery [3].
Conclusion
Although rare, phyllodes tumors may show DCIS and invasive carcinoma, with potential for lymph node metastasis. Therefore, a careful survey of both breasts before surgery is necessary.
Our case highlights the importance of assessing phyllodes tumors for concomitant carcinomatous association, as this may necessitate axillary lymph node resection and subsequent radiotherapy. Awareness of this co-existence will help in early detection and management.
Contributor Information
Sunila Jain, Phone: 91-9871147767, Email: s_isha19@rediffmail.com.
Ramneet Kaur, Email: drramneet@yahoo.co.in.
Rajeev Agarwal, Email: rajeevag56@gmail.com.
Prem Chopra, Email: premchopra2004@yahoo.co.in.
References
- 1.Neto GB, Rossetti C, Souza NA, LA Fonseca F, Azzalis LA, Junqueira VB, et al. Coexistence of benign phyllodes tumor and invasive ductal carcinoma in distinct breasts: case report. Eur J Med Res. 2012;25:17–8. doi: 10.1186/2047-783X-17-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan PH, Jayabaskar T, Chuah KL, Lee HY, Tan Y, Hilmy M, et al. Phyllodes tumors of the breast: the role of pathologic parameters. Am J Clin Pathol. 2005;123(4):529–40. doi: 10.1309/U6DVBFM81MLJC1FN. [DOI] [PubMed] [Google Scholar]
- 3.Parfitt JR, Armstrong C, O’malley F, Ross J, Tuck AB. In-situ and invasive carcinoma within a phyllodes tumor associated with lymph node metastases. World J Surg Oncol. 2004;2:46. doi: 10.1186/1477-7819-2-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korula A, Varghese J, Thomas M, Vyas F, Korula A. Malignant phyllodes tumour with intraductal and invasive carcinoma and lymph node metastasis. Singapore Med J. 2008;49(11):e318–21. [PubMed] [Google Scholar]
- 5.McCormick MV, Pillay SP. Malignant cystosarcoma phyllodes associated with scirrhous carcinoma of the breast: a case report. S Afr Med J. 1977;52(22):893–4. [PubMed] [Google Scholar]
- 6.Abdul Aziz M, Sullivan F, Kerin MJ, Callagy G. Malignant phyllodes tumour with liposarcomatous differentiation, invasive tubular carcinoma, and ductal and lobular carcinoma in situ: case report and review of the literature. Patholog Res Int. 2010;2010:501274. doi: 10.4061/2010/501274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen PP. Unusual clinical presentations of carcinoma. In: Rosen's Breast Pathology. 2. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 653–687. [Google Scholar]
- 8.Christensen L, Nielsen M, Madsen PM. Cystosarcoma phyllodes. A review of 19 cases with emphasis on the occurrence of associated breast carcinoma. Acta Pathol Microbiol Immunol Scand A. 1986;94(1):35–41. [PubMed] [Google Scholar]
- 9.Rosai J. Breast. In: Rosai and Ackerman’s Surgical Pathology. 10. Philadelphia: Mosby; 2011. pp. 1659–1770. [Google Scholar]