Abstract
Thyroid swellings are a significant clinical problem in the general population but majority of them are nonneoplastic and do not require surgery. The initial screening procedures include ultrasonography, fine needle aspiration cytology (FNAC) and radionucleotide scan. An initial screening test which will diagnose thyroid lesions accurately will help to avoid surgery in nonneoplastic conditions. The aim of the present study is to correlate the cytology findings with final histopathology. Two hundred and forty-eight cases of thyroid nodules which underwent FNAC followed by surgery were included in this study. The cytology diagnoses were classified into nondiagnostic/unsatisfactory, benign, atypia of undetermined significance/follicular lesion of undetermined significance, follicular neoplasm/suspicious for a follicular neoplasm, suspicious for malignancy and malignant. The fine needle aspiration diagnosis was compared with the histopathology diagnosis. In majority of cases the FNA diagnosis was in concordance with final histopathology. A high incidence of follicular variant of papillary carcinoma thyroid was detected in this study. The awareness of this entity and the search for fine nuclear details of papillary carcinoma can lead to proper identification of this category of tumors and thus help to avoid false negative and equivocal results. Fine needle aspiration cytology is a simple, cost effective, rapid to perform procedure with high degree of accuracy and is recommended as the first line investigation for the diagnosis of thyroid lesions.
Keywords: Fine needle aspiration cytology, Follicular variant of papillary thyroid carcinoma, Papillary carcinoma thyroid, Thyroid neoplasm
Introduction
Majority of thyroid swellings are nonneoplastic and do not always require surgical intervention. Less than 5 % of thyroid nodules are malignant [1]. Thyroid surgeries can be associated with lifelong thyroid hormone dependence and hypoparathyroidism in addition to the immediate operative risks involved. If an accurate preoperative diagnosis can be made, unnecessary surgery can be avoided in benign conditions. The initial preoperative screening procedures include ultrasonography, fine needle aspiration cytology (FNAC) and radio nucleotide scan. Among these, the fine needle aspiration cytology (FNAC) is considered the most accurate diagnostic modality. The Bethesda system of thyroid cytology reporting makes the reports clinically relevant and helps the clinicians to take appropriate therapeutic interventions [2].
Materials and Methods
A retrospective analysis of 248 cases of thyroid nodules, which underwent fine needle aspiration followed by surgery, during 2009–2011 in our institution, were included in the study. The cases with a nonneoplastic or benign FNA diagnosis in which patients are kept under follow up without surgical intervention based on the clinical, radiological and aspiration cytology findings were excluded. The cases with FNA diagnosis from our center and underwent surgery from outside centers or cases with FNA diagnosis from outside centers and underwent surgery in our center were excluded.
Direct FNA was done by palpation method. Ultrasound guided FNA was done in small nodules which were difficult to palpate, cystic nodules and nodules located posteriorly in the thyroid gland. Smears were fixed in 95 % alcohol solution and papanicolaou staining done. The smears were evaluated and diagnosis assigned according to the Bethesda system as nondiagnostic/unsatisfactory, benign, atypia of undetermined significance/follicular lesion of undetermined significance, follicular neoplasm/suspicious for a follicular neoplasm, suspicious of malignancy and malignant. In the first three categories, surgery was done in cases with suspicious ultrasonographic findings, in cases with rapidly enlarging thyroid lesions and in cases with large lesions which caused discomfort to the patients. The ultrasonographic features such as hypoechogenicity, irregular nodule borders, microcalcifications, and abnormalities of vasculature favor malignant nature of the lesions.
After the FNA diagnosis, the patients underwent surgery. The tissues were fixed in formalin. The relevant areas were sampled and processed in automated tissue processing units. Histopathological examination of the Hematoxylin and eosin stained sections were done.
Fine needle aspiration cytology diagnoses were compared with the histopathology in each case. The cases with diagnostic discrepancy were reviewed and the causes of misdiagnosis were analyzed.
Results
A total of 248 cases of thyroid lesions in which FNAC was done followed by surgery were analyzed (Table 1). The age of the subjects ranged from 11 to 79 years. Sixty-nine cases were males and 179 were females. The male: female ratio was 1:3.
Table 1.
FNA diagnosis of thyroid lesions
| FNA diagnosis | Number | Percentage |
|---|---|---|
| Malignancy | 148 | 59.68 |
| Suspicious of malignancy | 10 | 4.03 |
| Follicular neoplasm/suspicious for a follicular neoplasm | 33 | 13.3 |
| Atypia of undetermined significance/Follicular lesion of undetermined significance (FLUS) | 11 | 4.43 |
| Benign | 31 | 12.5 |
| Nondiagnostic/unsatisfactory | 15 | 6.04 |
Among the 148 malignant lesions diagnosed by FNAC, 118 were papillary carcinoma, 26 were follicular variant of papillary carcinoma, 3 were medullary carcinoma and 1 was poorly differentiated malignant neoplasm.
Correlation With Final Histopathological Diagnosis
All the 148 cases, which were diagnosed as malignancy during FNAC, were found to be malignant lesions in the final histopathology also. The 118 cases of papillary carcinoma were confirmed by histopathology −5 being follicular variant of papillary carcinoma. The 26 cases of follicular variant of papillary thyroid carcinoma by FNAC were diagnosed as the same by histopathology (Figs. 1 and 2). The diagnosis of 3 cases of medullary carcinoma was confirmed histopathologically. The 1 poorly differentiated malignant neoplasm turned to be lymphoma on final histopathology.
Fig. 1.
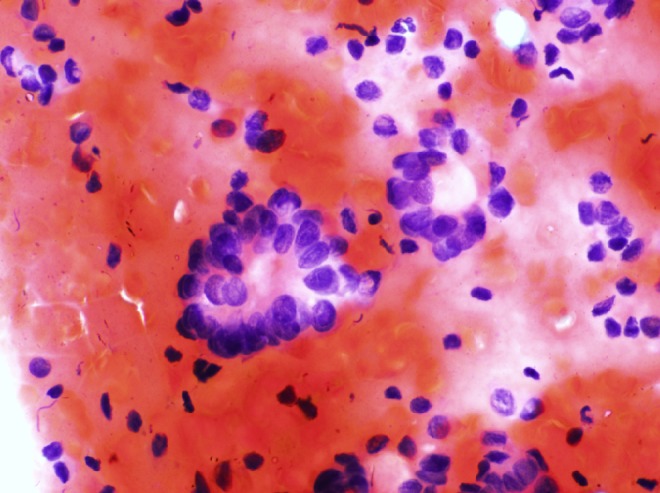
Fine needle aspiration cytology of Follicular variant of papillary thyroid carcinoma showing cells with nuclear features of papillary carcinoma arranged in follicular pattern (pap stain, X400)
Fig. 2.
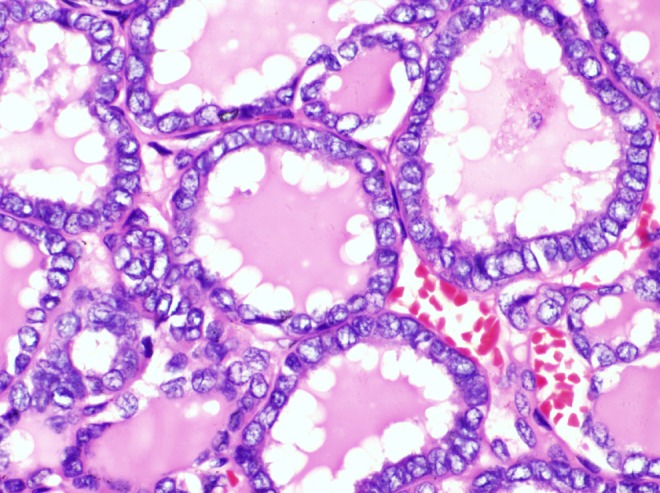
Histopathology of Follicular variant of papillary thyroid carcinoma showing cells with nuclear features of papillary carcinoma arranged in follicular pattern (H&E, X 400)
Of the 10 cases which were diagnosed as suspicious of malignancy on cytology, 7 were papillary carcinoma, 2 were follicular variant of papillary carcinoma and 1 was medullary carcinoma on histopathology.
Thirty-three cases were diagnosed as follicular neoplasm/suspicious for a follicular neoplasm by FNAC. Histopathological examination showed 17 cases as follicular variant of papillary carcinoma, 11 as papillary carcinoma, 4 as follicular adenoma and 1 as follicular carcinoma.
FNA diagnosis of Atypia of undetermined significance/follicular lesion of undetermined significance was made in 11 cases. Histopathology revealed 4 cases as follicular variant of papillary carcinoma, 1 case as papillary carcinoma, 1 case as follicular carcinoma, 4 cases as follicular adenoma and 1 as colloid nodule with cellular area.
A benign diagnosis was given by FNA in 31 cases. Four turned to be papillary carcinoma. Nineteen were colloid nodules, 2 were multinodular goiter, 5 were lymphocytic thyroiditis and 1 was cellular nodule (Table 2).
Table 2.
Correlation of FNA diagnosis with final Histopathology
| FNAC diagnosis | Histopathology-benign | Histopathology-malignant |
|---|---|---|
| Benign | 27 (TN) | 4 (FN) |
| malignant | 0 (FP) | 191 (TP) |
TN true negative, FN false negative, FP false positive, TP true positive
There were 15 cases in the diagnostic category nondiagnostic/unsatisfactory. Histopathology results were as follows- follicular variant of papillary carcinoma in 1 case, colloid nodule in 9 cases, follicular adenoma in 2 cases and lymphocytic thyroiditis in 3 cases.
Eleven cases of Atypia of undetermined significance/follicular lesion of undetermined significance and 15 cases of inadequate samples were excluded from the calculations because these diagnostic categories do not imply benign, nonneoplastic or malignant nature and require repeat aspiration.
Discussion
Although thyroid swellings are a major clinical problem, most of them are non neoplastic and do not require surgical intervention. Accurate screening investigations aid the clinician in selecting the subset of patients who truly require surgical intervention, while avoiding surgery in patients with benign conditions who might be exposed unnecessarily to surgical risk and a plethora of post surgery complications.
The available initial screening tests for thyroid lesions include ultrasonography, thyroid antibody levels, FNAC and radio nucleotide scan [3]. Among them FNAC is considered as the best initial diagnostic test. FNAC will help to identify the various thyroid lesions with high degree of accuracy, thus helping in avoiding unnecessary surgery in benign conditions.
The cytological evaluation and reporting of thyroid lesion was done in accordance with the Bethesda System [2]. It bridges the communication gap between clinicians and pathologists and thus helps the surgeons to take appropriate therapeutic interventions. It makes the cytology report unambiguous, clear, succinct and clinically relevant [2].
Thyroid FNAs should contain well prepared and well preserved follicular epithelial cells for interpretation. Adequate samples are required to reduce the false negative rates [4]. Samples with inadequate number of cells, thick smears or smears with cells obscured with blood were reported as unsatisfactory or nondiagnostic. Published studies show inadequate sample range between 2 and 20 % [5, 6]. The cellularity of the sample depends on the technique of the aspirate as well as the nature of the lesion. In lesions with calcification, sclerosis or cystic degeneration it is very difficult to get an adequately cellular aspirate. The number of inadequate samples can be minimized by taking samples from different parts of the lesion and by ultrasound guided aspiration of small lesions.
In our study a benign diagnosis of nodular goiter was reported in 24 cases and lymphocytic thyroiditis was diagnosed by cytology in 7 cases. Among these 4 cases turned to be papillary carcinoma on final histopathology -false negative cases. False negative rate is defined as percentage of benign cytology in which malignant lesions were later confirmed by histopathology in postsurgical specimens. False negative cytology can occur in cases with coexistence of malignant and benign lesions. In these cases due to sampling error the aspiration can be obtained from large benign lesion and adjacent malignant lesions can be missed. Cytomorphological overlap between benign and low grade malignant lesions can also lead to false negative reports. This false negative rate is a major pitfall and indicates the potential to miss malignant lesions [7, 8]. Most published studies report a false negative rate in the range of 1–10 % [9–11] In our series the false negative rate was 1.8 % and all the four false negative cases were papillary carcinoma with the adjacent thyroid tissue showing features of thyroiditis or colloid nodules. In these cases the aspirate was from the nonmalignant parts of the lesion and the small foci of malignancy were missed. These types of errors can be minimized by using ultrasound guided aspirations and by correlating the cytology diagnosis with scan findings. A negative cytology result should never exclude malignancy if there is strong clinical suspicion. Patients with benign cytology reports should be followed up with periodic clinical examination supplemented with ultrasonography.
A diagnosis of Atypia of undetermined significance/Follicular lesion of undetermined significance (FLUS) was given to cases that showed atypia that was not sufficient to designate as follicular neoplasm, suspicious of malignancy or malignant. Literature search shows 3–18 % of thyroid FNAs reported as FLUS [5, 12–14]. This diagnostic category should not be used indiscriminately and every attempt should be made to make specific diagnosis whenever possible by correlating clinical, pathological and radiological findings. This diagnosis should be limited to less than 7 % of all thyroid FNAs [5, 13, 14]. In our study of the 11 cases of FLUS which underwent surgery, 6 cases were malignant on histopathology. Of these malignant cases, 4 cases were follicular variant of papillary carcinoma which showed cells arranged in follicular pattern with focal nuclear clearing and occasional nuclear grooves.
An important grey zone of fine needle aspiration cytology is the follicular lesions [2]. The follicular lesions include a number of heterogeneous thyroid lesions -cellular adenomatous nodule, follicular adenoma, follicular carcinoma and follicular variant of papillary carcinoma thyroid [15, 16]. Usually smears from adenomatous nodules show more colloid than that of follicular neoplasm. Few cases in this study showed confusing cellular smears in nonneoplastic adenomatous nodules. In these cases, the presence of dispersed cells, monolayered sheets of epithelial cells and degenerative changes suggested the possibility of nonneoplastic lesion.
According to Bethesda system of reporting, Follicular neoplasm refers to a cellular aspirate composed of follicular cells with significant cell crowding and or microfollicle formation [2]. In the present study, 33 cases were diagnosed as follicular neoplasm by FNA. Tightly cohesive follicular cells favor neoplastic condition. Of these majority turned to be follicular variant of papillary carcinoma on final histopathology. Data from literature shows 27–68 % of malignancies, in which a diagnosis of follicular neoplasm was made in FNA, are interpreted as papillary carcinoma on histopathology [6, 12, 16, 17]. This may be due to focal subtle nuclear features of papillary carcinoma in some tumors which were not appreciated on the FNA samples.
In this study, 10 cases were diagnosed as Suspicious of malignancy by FNA. This diagnosis was made in cases which showed some features of malignancy but the findings were not sufficient to make a conclusive diagnosis. The features of papillary carcinoma include nuclear enlargement, powdery chromatin, nuclear membrane irregularity, nuclear grooves, nuclear moulding, intranuclear pseudo inclusions and papillary structures with distinct anatomical borders. In cases where only some of the characteristic nuclear features are present focally, a malignant diagnosis cannot be made with certainty. Such cases were classified as suspicious of malignancy. All the 10 cases turned to be malignant on final report and most were papillary carcinoma. In most of these cases the nuclear features of papillary carcinoma was focal and subtle.
One hundred forty-eight cases were diagnosed as malignant by FNAC. All the cases were malignant on final histopathology. The diagnoses of papillary carcinoma, follicular variant of papillary carcinoma and medullary carcinoma were confirmed by histopathological examination. There were no false positive results. False positive cytology can result in surgical overtreatment. Review of literature shows a false positive rate of 0–9 % [18].
In this study, 198 cases were malignant on final histopathology. The high percentage of malignancy in this study is because our institution is a tertiary cancer centre. The majority of cases were papillary carcinoma. Of the 136 cases of papillary carcinoma, FNA diagnosis was papillary carcinoma 113 cases, suspicious of malignancy in 7 cases, follicular neoplasm in 11 and follicular lesions of undetermined significance in 1 case. In cases which were diagnosed as follicular neoplasm and follicular lesions of undetermined significance, the cytology smears showed cell arranged in follicular patterns with subtle nuclear features of papillary carcinoma. In 4 cases a false negative diagnosis was given by FNA and these 4 cases were papillary carcinoma associated with benign lesions in the adjacent thyroid tissue. These findings indicate the high sensitivity of FNA in diagnosing the papillary carcinoma of the thyroid and show the potential causes of false negative results.
Follicular variant of papillary carcinoma (FVPTC) is the most common variant of papillary carcinoma and constitute around 30 % of papillary thyroid carcinomas in some series. Fifty-five cases (28.8 % of all papillary carcinoma) in this study were follicular variant of papillary thyroid carcinoma. Gupta S et al. in their study separated FVPTC into three separate entities- encapsulated follicular variant of papillary thyroid carcinoma (EFVPTC), non encapsulated follicular variant of papillary thyroid carcinoma (NFVPTC) diffuse follicular variant of papillary thyroid carcinoma [19]. They found clinical features and genetic profile of EFVPTC and NFVPTC were more like follicular adenoma and follicular carcinoma whereas the diffuse FVPTC had a clinical and genetic profile more like classical PTC with increased rates of BRAF mutations and central node metastasis.
The cytological diagnosis of FVPTC can be difficult because of paucity of nuclear changes of papillary thyroid carcinoma and because of overlapping features with both benign and malignant follicular lesions. Of 55 cases which were diagnosed as FVPTC by histopathology, the FNA diagnosis was as follows- 26 cases were diagnosed as follicular variant of papillary carcinoma, 5 as papillary carcinoma, 2 as suspicious of malignancy, 17 as follicular neoplasm and 4 as follicular lesion of undetermined significance. One case in the nondiagnostic/unsatisfactory category, when operated on basis of alarming sonographic features, showed focus of FVPTC. The cytological features which help to identify FVPTC include flat syncitial arrangement of cells with nuclear crowding, oval enlarged nuclei, nuclear clearing, nuclear grooves and thick colloid. The diagnosis of FVPTC depends mainly on nuclear features, but the nuclear changes can be focal and subtle in FVPTC compared to classical PTC. Moreover the cytomorphological features are not entirely specific for FVPTC, as the minimal nuclear changes can be seen focally in some cases of follicular neoplasm, rare cases of lymphocytic thyroiditis and nodular goiter. In the present study nuclear enlargement and fine chromatin were the most important features which helped in the FNA diagnosis of FVPTC. The awareness of this entity and the thorough search for nuclear features of papillary carcinoma in the follicular lesions can lead to proper identification of this malignancy and thus reducing the diagnostic category of follicular lesions of undetermined significance and follicular neoplasm which does not imply benign or malignant nature of the lesion. The presence of cytological atypia such as nuclear enlargement, fine chromatin and nuclear grooves even present focally are important clues to diagnose follicular variant of papillary thyroid carcinoma in smears [20]. If characteristic nuclear features are present in more than 20 % of cells there is a greater chance for papillary carcinoma [18, 21].
In conclusion, fine needle aspiration cytology is cost effective, simple procedure that has great patient acceptance and as an initial screening test provides the diagnosis with high degree of accuracy thereby limiting the number of surgeries in benign conditions of thyroid gland. A negative diagnosis should be followed up with repeat ultrasound and FNA should be repeated in suspicious cases. Correlation of cytology and histopathology is an important quality assurance measure.
Acknowledgments
Conflict of Interest
No conflict of interests.
References
- 1.Sclabas GM, Staerkel GA, Shapiro SE, Fornage BD, Sherman SL, Vassillopoulou-Sellin R, Lee JE, Evans DB. Fine Needle Aspiration thyroid and correlation with histopathology in a contemporary series of 240 patients. Am J Surg. 2003;186:702–710. doi: 10.1016/j.amjsurg.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 2.Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658–663. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 3.Hegedus L. Clinical practice.The thyroid nodule. N Engl J Med. 2004;351:1764–1771. doi: 10.1056/NEJMcp031436. [DOI] [PubMed] [Google Scholar]
- 4.Sudilovsky D. Interpretation of the paucicellular thyroid fine needle aspiration biopsy specimen. Pathol Case Rev. 2005;10:68–73. doi: 10.1097/01.pcr.0000155765.73313.be. [DOI] [Google Scholar]
- 5.Renshaw AA. Accuracy of thyroid fine needle aspiration using receiver operator characteristic curves. Am J Clin Pathol. 2001;116:477–482. doi: 10.1309/M3K5-23C2-455E-0HB5. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Schnadig V, Logrono R, Wassrman PG. Fine –needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer. 2007;111:306–315. doi: 10.1002/cncr.22955. [DOI] [PubMed] [Google Scholar]
- 7.Hall TL, Layfield LJ, Philippe A, Rosenthal DL. Source of diagnostic error in the fine needle aspiration of the thyroid. Cancer. 1989;63:718–725. doi: 10.1002/1097-0142(19890215)63:4<718::AID-CNCR2820630420>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 8.Bagga PK, Mahajan NC. Fine needle aspiration cytology of thyroid swellings: how useful and accurate is it? Indian J Cancer. 2010;47:437–442. doi: 10.4103/0019-509X.73564. [DOI] [PubMed] [Google Scholar]
- 9.Gharib H, Goellner JR. Fine needle aspiration biopsy of the thyroid: an appraisal. Ann Int Med. 1993;118:282–289. doi: 10.7326/0003-4819-118-4-199302150-00007. [DOI] [PubMed] [Google Scholar]
- 10.Yeh MW, Demircan O, Ituarte P, Clark OH. False negative fine needle aspiration cytology results delay treatment and adversely affect outcome in patients with thyroid carcinoma. Thyroid. 2004;14:207–215. doi: 10.1089/105072504773297885. [DOI] [PubMed] [Google Scholar]
- 11.Tee YY, Lowe AJ, Brand CA, Judson RT. Fine needle aspiration may miss a third of all malignancy in palpable thyroid nodules: a comprehensive literature review. Ann Surg. 2007;246:714–720. doi: 10.1097/SLA.0b013e3180f61adc. [DOI] [PubMed] [Google Scholar]
- 12.Yassa L, Cibas ES, Benson CB, et al. Long—term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer. 2007;111:508–516. doi: 10.1002/cncr.23116. [DOI] [PubMed] [Google Scholar]
- 13.Nayar R, Ivanovic M. (2009) The indeterminate thyroid FNA: Experience from an academic center using terminology similar to that proposed in the 2007 NCI Thyroid Fine Needle Aspiration State of the Science Conference. Cancer Cytopathol. 2007;117:195–202. doi: 10.1002/cncy.20029. [DOI] [PubMed] [Google Scholar]
- 14.Krane JF, Nayar R, Renshaw AA. Atypia of undetermined significance/Follicular lesion of undetermined significance. In: Cibas ES, Ali SZ, editors. The Bethesda system for reporting thyroid cytopathology. New York: Springer; 2009. [Google Scholar]
- 15.Baloch ZW, Livolsi VA. Follicular patterned lesions of the thyroid: the bane of the pathologist. Am J Clin Pathol. 2002;117:143–150. doi: 10.1309/8VL9-ECXY-NVMX-2RQF. [DOI] [PubMed] [Google Scholar]
- 16.Deveci MS, Deveci G, Li Volsi VA, Baloch ZW. Fine needle aspiration of follicular lesions of the thyroid Diagnosis and follow up. Cytojournal. 2006;3:9. doi: 10.1186/1742-6413-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faquin WC, Michael CW, Renshaw AA, Vielh . Follicular neoplasm, Hurthle cell type/Suspicious for a Follicular neoplasm, Hurthle cell type. In: Ali SZ, Cibas ES, editors. The Bethesda system for reporting thyroid cytopathology. New York: Springer; 2009. [Google Scholar]
- 18.Goldstein RE, Netterville JL, Burkey B, Johnson JE. Implications of follicular neoplasms, atypia and lesions suspicious of malignancy diagnosed by fine needle aspiration of thyroid nodules. Ann Surg. 2002;235:656–664. doi: 10.1097/00000658-200205000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta S, Ajise O, Dultz L, Wang B, Nonaka D, Ogilvie J, Heller KS, Patel KN. Follicular variant of papillary thyroid cancer: encapsulated, nonencapsulated, and diffuse: distinct biologic and clinical entities. Arch Otolaryngol Head Neck Surg. 2012;138:227–233. doi: 10.1001/archoto.2011.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu HH, Jones JN, Grzybicki DM, Elsheikh TM. Sensitive cytologic criteria for the identification of follicular variant of papillary thyroid carcinoma in fine needle aspiration biopsy. Diagn Cytopathol. 2000;29:262–266. doi: 10.1002/dc.10388. [DOI] [PubMed] [Google Scholar]
- 21.Sinna EA, Ezzat N. Diagnostic accuracy of fine needle aspiration cytology in thyroid lesions. J Egypt Natl Cancer Inst. 2012;24:63–70. doi: 10.1016/j.jnci.2012.01.001. [DOI] [PubMed] [Google Scholar]


