Abstract
Background
Trigger digit is a common pathology encountered by hand surgeons, but there is a lack of evidence-based guidelines. We investigated the treatment preferences of hand surgeons and explored whether geographic location, type of residency training, or clinical experience is associated with differences in practice.
Methods
An online survey was distributed via email by the American Association for Hand Surgery to 615 members. The survey consisted of 17 questions related to conservative and operative management of trigger digits.
Results
One hundred thirty-nine unique responses were received (22.6 %). Geographic distribution of respondents encompassed the entire USA and was not associated with variations in practice. Of the respondents, 56.8 % were trained in orthopedic surgery while 37.4 % had plastic surgery training. In regards to duration of practice, 8.6 % were in practice for up to 5 years, 29.5 % for 6–15 years, 33.8 % for 16–25 years, and 28.1 % for more than 25 years. Notably, the great majority of respondents preferred corticosteroid injections for initial treatment. Those who were willing to give three or more injections prior to surgery were more likely to be plastic surgeons in practice for 16 years or more. A large minority of surgeons utilized splinting in their conservative management. Orthopedic surgeons were more likely to perform tenolysis during pulley release and more likely to use monitored anesthesia care.
Conclusions
Variation exists between the treatment algorithms of hand surgeons when managing a trigger digit. Some of these differences may be attributable to the type of training or the duration of clinical practice.
Keywords: Trigger finger, Trigger thumb, Questionnaire, Survey, Surgeon preferences
Introduction
Trigger digit, also known as stenosing tenosynovitis, inhibits flexor tendon gliding due to thickening of the synovial sheath over the tendon. Symptoms can range from pain and tenderness over the A1 pulley to locking of the digit. There is variability in the algorithms that different surgeons use when deciding the appropriate treatment at a particular stage in the disease process. Furthermore, there is a lack of evidence-based medicine to support decisions between splinting, corticosteroid injections, and surgery [4]. In this study, we sought to evaluate the preferences of hand surgeons in their management of trigger finger and trigger thumb. We also investigated whether surgeon demographic factors, such as type of residency training, duration of practice, or geographic location, may contribute to variations in treatment in the absence of clear clinical guidelines.
Materials and Methods
An online survey was distributed via email by the American Association for Hand Surgery (AAHS) administration to 615 AAHS surgeon members on behalf of the authors of this study. These AAHS members received an email with a link to the survey (Survey Gizmo software, surveygizmo.com). The electronic questionnaire was composed of 17 questions evaluating a surgeon’s approach to conservative and surgical treatment of trigger finger and trigger thumb. Each question required an answer for completion of the survey, and participants were instructed in their emailed link not to take the survey more than once. In addition, they were asked to refrain from forwarding the email to colleagues.
After 1 week, a second email was distributed. One hundred forty completed surveys were received during the 2 weeks that the survey was active. Duplicate submissions (n = 1) were identified by Internet Protocol address, city, and zip code and were removed from final analysis. Survey submissions remained confidential. Survey data was stratified by type of residency training, years in practice, and geographic location of practice.
Results
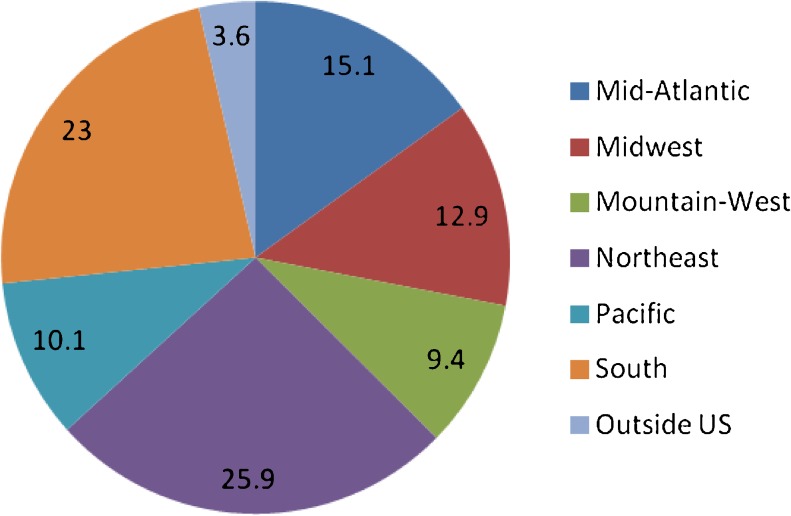
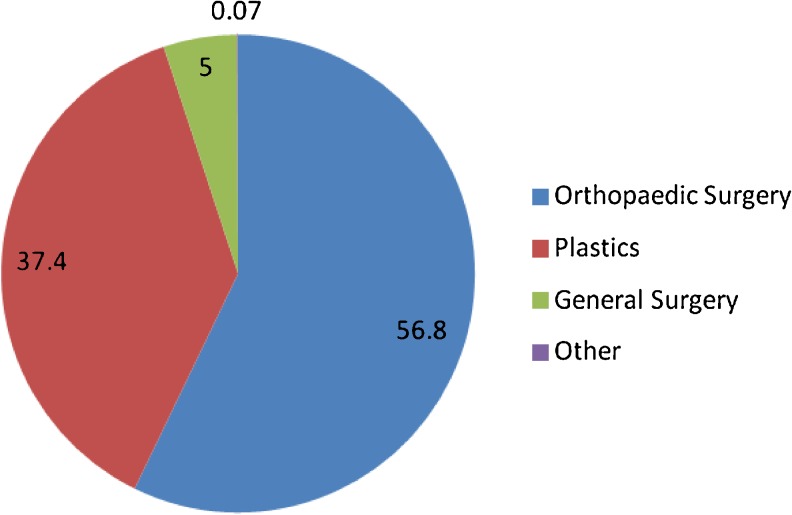
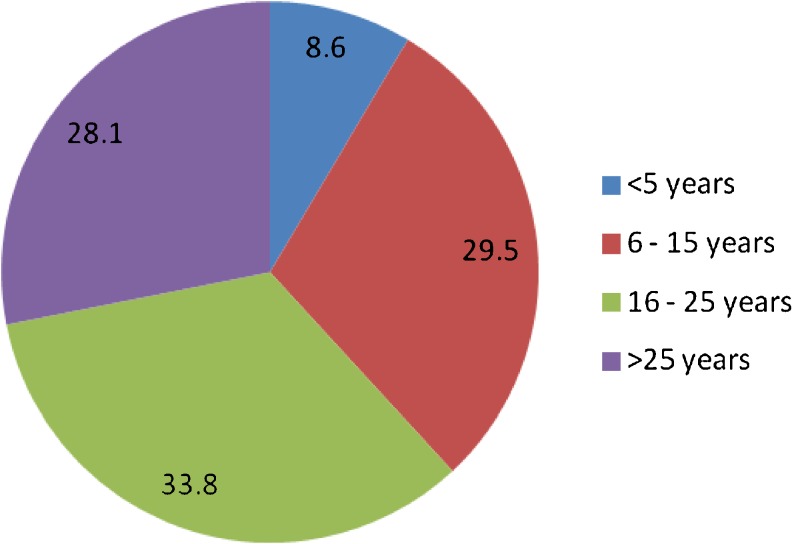
The 139 unique surgeon surveys received represented a 22.6 % response rate. The geographic distribution of respondents covered the entire USA, with a handful of responses from outside the country (Fig. 1). The majority of respondents (56.8 %) were trained in orthopedic surgery, followed by plastic surgery (37.4 %), and general surgery (5 %). One respondent had dual specialty training (Fig. 2). Respondents’ duration of practice varied, with 8.6 % in practice for up to 5 years, 29.5 % for 6–15 years, 33.8 % for 16–25 years, and 28.1 % for more than 25 years (Fig. 3).
Fig. 1.
Distribution of respondents by geographic location of practice (percent)
Fig. 2.
Distribution of respondents by type of residency training (percent)
Fig. 3.
Distribution of respondents by duration of practice (percent)
The remaining survey data are presented in Tables 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, and 14. Notably, some differences emerged between residency training type and length of years in practice. Geographic location of practice was not found to be associated with differences in treatment preferences.
Table 1.
Regarding conservative management of trigger thumb, what is your preferred initial treatment method?
| Activity modification | NSAID | Corticosteroid injection | Splinting | Corticosteroid and splinting | Other | |
|---|---|---|---|---|---|---|
| Total | 5 (3.6 %) | 11 (7.9 %) | 92 (66.2 %) | 1 (0.7 %) | 20 (14.5 %) | 10 (7.3 %) |
Table 2.
If corticosteroid injections are utilized for conservative management of trigger thumb, how many injections do you routinely offer prior to advocating surgical treatment?
| 1 | 2 | 3 or more | I do not use corticosteroid injections | |
|---|---|---|---|---|
| Total | 43 (30.9 %) | 76 (54.7 %) | 15 (10.8 %) | 5 (3.6 %) |
Table 3.
If splint immobilization is used for the conservative treatment of trigger thumb, what kind of splint is applied?
| Thumb-based splint | Hand-based thumb spica | Forearm-based thumb spica | Other | Not applicable | |
|---|---|---|---|---|---|
| Total | 29 (20.9 %) | 19 (13.7 %) | 5 (3.6 %) | 4 (2.9 %) | 82 (59.0 %) |
Table 4.
If a splint is used in the conservative management of trigger thumb, for approximately how long do you recommend usage?
| <4 weeks | 4–6 weeks | 6–8 weeks | >8 weeks | Not applicable | |
|---|---|---|---|---|---|
| Total | 20 (14.4 %) | 27 (19.4 %) | 7 (5.0 %) | 2 (1.4 %) | 83 (59.7 %) |
Table 5.
Regarding surgical treatment of trigger thumb, what is your preferred approach?
| Longitudinal incision | Transverse incision | Oblique incision | Percutaneous release | Other | |
|---|---|---|---|---|---|
| Total | 8 (5.8 %) | 99 (71.2 %) | 17 (12.2 %) | 4 (2.9 %) | 11 (7.9 %) |
Table 6.
Regarding conservative management of trigger finger, what is your preferred initial treatment method?
| Activity modification | NSAID | Corticosteroid injection | Splinting | Corticosteroid and splinting | Other | |
|---|---|---|---|---|---|---|
| Total | 6 (4.3 %) | 11 (7.9 %) | 91 (65.5 %) | 2 (0.7 %) | 20 (14.4 %) | 9 (6.5 %) |
Table 7.
If corticosteroid injections are utilized for conservative management of trigger finger, how many injections do you routinely offer prior to advocating surgical treatment?
| 1 | 2 | 3 or more | I do not use corticosteroid injections | |
|---|---|---|---|---|
| Total | 37 (26.6 %) | 80 (75.6 %) | 18 (13.0 %) | 4 (2.9 %) |
Table 8.
If splint immobilization is used for the conservative treatment of trigger finger, what kind of splint is applied?
| Finger-based splint | Hand-based splint | Forearm-based splint | Other | Not applicable | |
|---|---|---|---|---|---|
| Total | 28 (20.1 %) | 28 (20.1 %) | 1 (0.7 %) | 1 (0.7 %) | 81 (58.3 %) |
Table 9.
If a splint is used in the conservative management of trigger finger, for approximately how long do you recommend usage?
| <4 weeks | 4–6 weeks | 6–8 weeks | >8 weeks | Not applicable | |
|---|---|---|---|---|---|
| Total | 17 (12.2 %) | 29 (20.9 %) | 9 (6.5 %) | 2 (1.4 %) | 82 (59.0 %) |
Table 10.
Regarding surgical treatment of trigger finger, what is your preferred approach?
| Longitudinal incision | Transverse incision | Oblique incision | Percutaneous release | Other | |
|---|---|---|---|---|---|
| Total | 34 (24.5 %) | 49 (35.3 %) | 41 (29.5 %) | 5 (3.6 %) | 10 (7.2%) |
Table 11.
Regarding surgical treatment of trigger finger or trigger thumb, which do you routinely perform?
| Pulley release alone | Pulley release plus tenolysis | |
|---|---|---|
| Total | 110 (79.1 %) | 29 (20.9 %) |
Table 12.
When performing trigger finger or trigger thumb surgery, what type of anesthesia do you typically employ?
| Local only | Local with MAC | Regional/bier | General | Other | |
|---|---|---|---|---|---|
| Total | 47 (33.8 %) | 66 (47.5 %) | 16 (11.5 %) | 6 (4.3 %) | 4 (2.9 %) |
Table 13.
In the immediate postoperative period, do you immobilize all patients in a splint?
| Yes | No | |
|---|---|---|
| Total | 6 (4.3 %) | 133 (95.7) |
Table 14.
If a splint is employed postoperatively, for approximately how long do you immobilize patients?
| <2 weeks | 2–4 weeks | >4 weeks | I do not use a splint postoperatively | |
|---|---|---|---|---|
| Total | 8 (5.8 %) | 1 (0.7 %) | 1 (0.7 %) | 129 (92.8 %) |
Discussion
The practice of using corticosteroid injections for conservative treatment of trigger digits is widely popular. For trigger thumb, approximately two thirds of surgeons preferred corticosteroid injection alone for initial treatment, while another 14.4 % preferred corticosteroid injection in conjunction with splinting (Table 1). When considering the use of steroid injections at any point in conservative management, only 3.6 % of respondents would not use injections at all. When respondents were asked how many injections to give prior to surgery, more variability was presented; 30.9 % would offer one injection prior to surgery, 54.7 % would offer two injections, and 10.8 % would offer three or more (Table 2). Interestingly, of those surgeons offering three or more injections, 86.7 % have been in practice for 16 or more years.
For trigger finger, approximately the same number of surgeons preferred the use of steroids for initial treatment as had for trigger thumb. Only 2.9 % would not use injections at all (Table 3). Meanwhile, 26.6 % would offer one injection prior to surgery, 57.6 % would offer two, and 12.9 % would offer three or more (Table 4). Again, a vast majority (83.3 %) of surgeons offering three or more injections practiced for 16 or more years. The comfort that older surgeons have for administering more steroid injections to the thumb or finger may be the result of their greater experience with lack of complications. Perhaps also a more senior practitioner has a higher threshold to operate. Furthermore, plastic surgeons represented 80 % of the respondents who would offer three or more injections for trigger thumb and 66 % of the group for trigger finger.
Prior literature has identified the least costly treatment for trigger finger to be two steroid injections prior to surgical release for refractory cases [6]. A randomized trial identified a cure rate of 86 % by using up to two steroid injections [8]. Other series of patients have shown similar cure rates after injection [7], though meta-analysis of four randomized controlled trials revealed only 57 % of patients experienced relief [4]. Open release of the A1 pulley has been shown to be effective and safe, with cure rates approaching 100 % and with adverse events occurring in less than 1 % of patients [1, 8]. The variability in the literature for corticosteroids, and the high success rate and low risk profile of surgical release, may be a reason surgeons in our survey demonstrated different thresholds for proceeding to surgery.
A large minority of surgeons overall also considered splinting during conservative management of trigger thumb (38.1 %) and trigger finger (41 %), with most choosing not to use it for more than 6 weeks (Tables 3, 4, 8, and 9). This group, though, did not demonstrate variability due to years in practice or residency training. In previous studies, metacarpophalangeal joint splinting has been shown to have variable success, with 70–92 % of fingers cured [3, 7, 9].
Questions regarding perioperative topics yielded notable points as well. While the large majority (71.2 %) of all surgeons preferred a transverse skin incision for surgical release of trigger thumb, the same was not true for trigger finger, with only a narrow plurality (35.3 %) who favored transverse incisions (Tables 5 and 10). Of all surgeons, 79.9 % preferred pulley release alone without tenolysis (Table 11). However, among the remaining minority that also performs tenolysis, three quarters were orthopedic surgeons. Only a tiny fraction of surgeons said they would perform percutaneous release for trigger finger (3.6 %) or trigger thumb (2.9 %) (Tables 8 and 13). The low enthusiasm for percutaneous technique could be the result of a lack of training during residency. The ease of performing an open trigger release with a small incision, and the perceived risks of incomplete release or iatrogenic neurovascular/tendon injury, may also contribute to the low rates observed in the survey. Table 12 reveals that anesthesia preferences highly favored local anesthetic alone or in combination with monitored anesthesia care (MAC) (81.3 %). Two thirds of respondents who preferred the addition of MAC were orthopedic surgeons. This difference may result from orthopedic surgery-trained hand surgeons having greater experience with MAC when combined with regional blocks or local anesthetic during other upper limb surgeries. Also, plastic surgery-trained hand surgeons likely have greater familiarity with local anesthetic alone from their higher volume of office-based procedures. Postoperatively, 95.7 % of all surgeons would not use a splint (Table 14).
This study has several limitations, primarily based on the low response rate (22.6 %). Previously published surveys have had response rates between 42 and 53 % [2, 5]. We suspect that the large number of questions may have made the survey too demanding of surgeons’ limited time. In addition, the invitation to complete an online survey has become a frequent event. Fatigue may be a culprit in hindering more responses. There is also the possibility that the emails to which the survey was sent are not regularly checked or out of date. Furthermore, the emails could have ended up in spam folders depending on email account settings. Although duplicate responses were investigated, it is possible that a respondent could take the survey more than once by using different computers. Without a unique ID assigned to each respondent who completed the survey, it is difficult to safeguard against this possibility. The large number of “other” responses for some questions also suggests that some questions could have been worded differently or more answer choices provided. However, this point also reinforces the fact that there remains a wide variety of trigger digit treatments offered to patients.
Looking at the treatment preferences of a sample of hand surgeons presented in this survey data demonstrates areas of both consensus and variability. Insufficient evidence exists to explain the differences noted between orthopedic and plastic surgeon preferences. The number of corticosteroid injections to give, the use of splinting, the benefit of tenolysis during pulley release, and the use of sedation along with local anesthetic remain questions with sizable differences of opinion amidst a large group of surgeons. Further high-quality research may help find more agreement in the treatment algorithm of trigger digits by hand surgeons.
Acknowledgments
We would like to thank the AAHS board and administration for assisting with the design of this study and distribution of the survey. This study had no external sources of funding.
Conflict of Interest
Jason S. Pruzansky declares that he has no conflict of interest. Peter Goljan declares that he has no conflict of interest. David P. Lundmark declares he has no conflict of interest. Eon K. Shin declares that he has no conflict of interest. Sidney M. Jacoby declares that he has no conflict of interest. A. Lee Osterman declares that he has no conflict of interest.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Statement of Informed Consent
This study did not require informed consent by patients.
References
- 1.Bruijnzeel H, Neuhaus V, Fostvedt S, et al. Adverse events of open A1 pulley release for idiopathic trigger finger. J Hand Surg [Am] 2012;37(8):1650–6. doi: 10.1016/j.jhsa.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 2.Cavaliere CM, Chung KC. Total wrist arthroplasty and total wrist arthrodesis in rheumatoid arthritis: a decision analysis from the hand surgeons’ perspective. J Hand Surg [Am] 2008;33(10):1744–55. doi: 10.1016/j.jhsa.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colbourn J, Heath N, Manary S, et al. Effectiveness of splinting for the treatment of trigger finger. J Hand Ther. 2008;21:336–43. doi: 10.1197/j.jht.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg. 2007;15:166–71. doi: 10.5435/00124635-200703000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Kakar S, Bakri K, Shin AY. Survey of hand surgeons regarding their perceived needs for an expanded upper extremity fellowship. J Hand Surg [Am] 2012;37(11):2374–80. doi: 10.1016/j.jhsa.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Kerrigan CL, Stanwix MG. Using evidence to minimize the cost of trigger finger care. J Hand Surg [Am] 2009;34(6):997–1005. doi: 10.1016/j.jhsa.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 7.Patel MR, Bassini L. Trigger fingers and thumb: when to splint, inject, or operate. J Hand Surg [Am] 1992;17(1):110–3. doi: 10.1016/0363-5023(92)90124-8. [DOI] [PubMed] [Google Scholar]
- 8.Sato ES, Santos Gomes dos JB, Belloti JC, et al. Treatment of trigger finger: randomized clinical trial comparing the methods of corticosteroid injection, percutaneous release and open surgery. Rheumatology. 2012;51:93–9. doi: 10.1093/rheumatology/ker315. [DOI] [PubMed] [Google Scholar]
- 9.Tarbhai K, Hannah S, von Schroeder HP. Trigger finger treatment: a comparison of 2 splint designs. J Hand Surg [Am] 2012;37(2):243–9. doi: 10.1016/j.jhsa.2011.10.038. [DOI] [PubMed] [Google Scholar]