Abstract
We aimed to introduce a surgical option for crushing–penetrating injuries around the metacarpophalangeal (MP) joint of the middle finger with extensor reconstruction of the interphalangeal (IP) joints. We also assessed the outcomes of patients using this surgical protocol. First, MP joint reconstruction was performed early (mean, 1.2 weeks after injury) using free autogenous cartilage or bone graft. We next performed a tendon transfer using a modified Brand method (M. Brand) at the same setting of extensor tendon tenolysis (mean, 4.7 months after injury) in order to extend the IP joints as a bonus for mutilating injuries of the hand. The mean arc of motion of each MP and IP joint increased after the M. Brand procedure. In one patient, worsening of palmar subluxation at the base of the proximal phalanx at the MP joint was observed. We found that tendon transfer by M. Brand achieves additional reconstruction for patients who have an IP joint extension lag after a crushing–penetrating injury around the MP joint. On the basis of these encouraging findings in this small series of cases, we recommend the M. Brand procedure after the MP joint stabilizes, as an optional bonus for mutilating injured hand.
Keywords: Crushing–penetrating injury around the MP joint, Finger extensor lag, Extensor reconstruction of IP joints
Introduction
Crush or penetrating trauma with a loss of compound tissue from the back of the hand is sometimes accompanied by destruction around the metacarpophalangeal (MP) joint of the middle finger. This type of trauma is often caused by machinery in factory accidents. The damage to the intrinsic muscle belly at this type of injury is a poor prognostic factor [3]. Dorsal injuries classified by Campbell [2] can be deemed crushing–penetrating injuries by considering the usual mechanism of this type of occupational injury [4]. Repairing or reconstructing the extrinsic tendons and the MP joint components is essential for these injuries. However, repairing the lateral intrinsic tendon is difficult and is generally not performed, which leads to insufficient extension of the interphalangeal (IP) joints. As a result, the fingers cannot be opened fully at the IP joints. In this case series, we describe the application of the well-known Brand method with some modifications (M. Brand) on the extensor reconstruction of proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints of the middle finger after injury [1, 6]. We describe our methods and results, including the surgical strategy.
Materials and Method
Between 2008 and 2010, three patients who each had an extension lag of the IP joint of their middle finger underwent this surgical protocol between 3 and 6 months after receiving an injury. Table 1 shows the patient data. The patients were all right handed. MP joint reconstruction with free autogenous cartilage or bone graft following repair of the injured MP joint was performed at an early stage after injury. The M. Brand procedure was performed at the chronic stage after injury. Our surgical strategy consisted of four steps: first, emergent repair; second, MP joint and tendon reconstruction at an early stage; third, flexor tenolysis if necessary; and fourth, extensor tendon reconstruction with MP joint release or extensor tendon tenolysis. The following injuries associated with the initial trauma were commonly observed for all three patients: comminuted fracture at the head of the metacarpal bone of the middle finger; extensor tendon rupture; damage to the lateral intrinsic muscles due to loss of intrinsic muscle belly with no paralysis and incomplete injury of the volar components, including partial laceration of flexor tendons; partial ruptures of the median nerve; and a superficial palmar arterial arch. In addition, each patient had other major injuries to the same hand. Patient 1 had a complex extensor tendon laceration of the extensor indicus proprius (EIP). Patient 2 had a fracture at the head of the metacarpal bone of the ring finger and dislocation at the carpometacarpal (CM) joint of the ring and little fingers. Patient 3 had an intra-articular fracture at the PIP joint of the middle finger and incomplete amputation of the little finger.
Table 1.
Patient data
| Patient | Gender | Age (year) | Injured hand | Method of MP Rec. | Duration MP Rec. (week) | Duration M. Brand (month) | Number of operation | Follow-up (year) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 56 | Lt. | Costal OG | 2.5 | 6 | 4 | 2 |
| 2 | M | 20 | Lt. | Repair by Iliac bone graft | 1 | 3 | 5 | 1.5 |
| 3 | F | 61 | Rt. | OG (Capitate and 3rd BMB) | 0.15 | 5 | 5 | 1.5 |
| Average | 46 | 1.2 | 4.7 | 4.7 | 1.7 |
OG osteochondral graft, MP Rec. MP joint reconstruction, BMB base of metacarpal bone, Duration duration from initial injury to reconstruct surgery, M. Brand modified Brand method
Passive stretching by splint was performed to improve passive range of motion (P-ROM) of the MP and IP joints starting at 6 weeks after the MP joint reconstruction. Before the M. Brand surgery, all three patients obtained adequate P-ROM of the PIP joint except patient 3 with fracture of PIP joint (patient 1: −5/85, patient 2: 20/90, and patient 3: −20/60).
Surgical Technique
The original Brand method is used to reconstruct paralyzed lateral intrinsic muscles of the four digits not occurring as a result of direct trauma by using the extensor carpi radialis longus (ECRL) as a power source through the segmental transplantation of the palmaris longus (PL) [1, 6]. Our series of cases were not of paralytic hands, but rather severely injured hands, which were not suitable for tendon transfer due to adhesion or scars. Therefore, we used the stronger power source from the more proximal site rather than the directly injured site. We applied the M. Brand surgical procedure in order to reconstruct the radial lateral intrinsic band of the single middle finger and to recover the extension lag of the IP joint (Fig. 1). Briefly, the ECRL was elevated from its insertion and withdrawn proximal to the dorsal retinacular ligament. The entire folded PL was sutured with inter-lace stitches to the end of the ECRL and reinforced with multiple sutures at the folding point into layers (Fig. 1a). Both ends of the PL were then passed through a subcutaneous tunnel obliquely across the MP joint deep to the transverse metacarpal ligament (TML) using a tendon passer (Fig. 1b). In cases where the TML was lost by the initial trauma, the PL was passed deep into the dense scar tissue. Each end of the PL was then sutured with inter-lace stitches to the radial lateral band and oblique fiber, respectively (Fig. 1c). When the length of the PL was too short to fold, the single end of the PL was divided into two (Fig. 2d). The tension of the tendon transfer was determined by placing the tendon under maximum tension with the wrist neutral and fingers in the intrinsic plus position. The extensor digitorum communis (EDC) of the middle finger was released along the dorsal MP joint in the same operative setting.
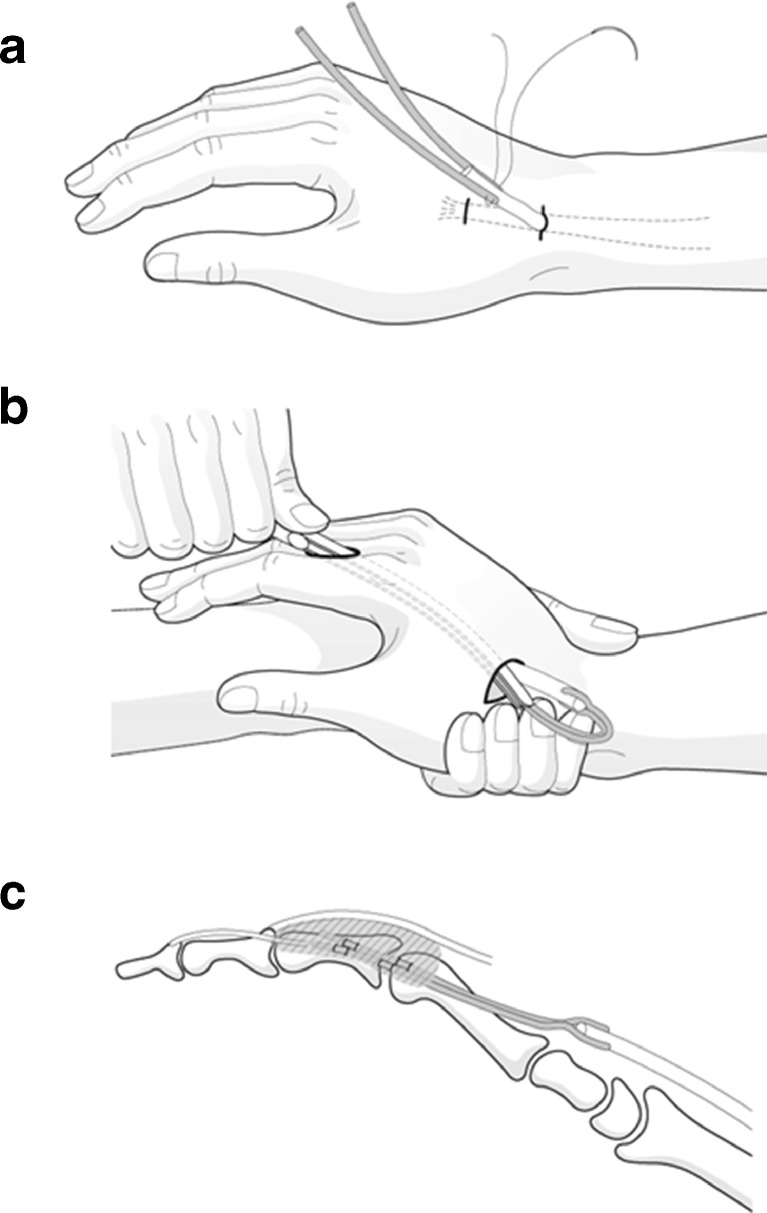
Fig. 1.
Schematic drawing of the M. Brand surgery. a The entire folded PL was sutured with inter-lace stitches to the end of the ECRL and reinforced with multiple sutures at the folding point into layers. b Both ends of the PL were then passed through a subcutaneous tunnel obliquely across the MP joint deep to the transverse metacarpal ligament (TML) using a tendon passer. c Each end of the PL was sutured with inter-lace stitches to the radial lateral band and oblique fiber, respectively
Fig. 2.
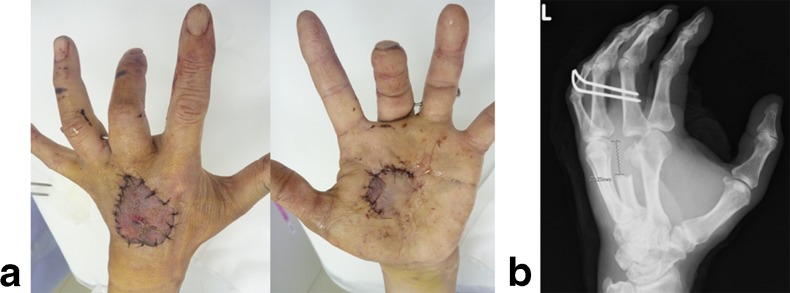
(Patient 1) Two weeks after injury at the initial consultation demonstrating, a repaired skins of both volar and dorsal sides and b missing distal metacarpal bone of the middle finger by X-ray
Post-operative Management
Post-operatively, active synergic wrist and finger movement was started under the supervision of a hand therapist starting on the third day post-surgery. A safe position for the wrist cock-up position and for the fingers in the intrinsic plus position was maintained for 3 weeks after surgery by immobilizing the hand with a volar splint, except for the abovementioned early-active rehabilitation program. Passive flexion stretching using a dynamic leather splint was started at 5 or 6 weeks post-surgery and continued for 12 weeks after the operation.
Results
After the M. Brand surgery with EDC tendon release of the middle finger, the total active movement (TAM) in both extension and flexion was improved in all joints from the IP to the MP joints (Table 2). The PIP joint extension showed the greatest improvement after the M. Brand surgery. An improvement in MP extension after the procedure seemed to be due to extensor tendon tenolysis. The 1.5-year follow-up indicated that the TAM was maintained and the outcome was satisfactory in all cases.
Table 2.
Results (TAM of before and after M. Brand final outcome)
| Patient | MP extenxion–flexion (TAM) | PIP extenxion–flexion (TAM) | DIP extenxion–flexion (TAM) | GS/CP (N. Side) at 18 months (kg) | Level of satisfaction |
|---|---|---|---|---|---|
| 1 | |||||
| Before surgery | −15/60 (45) | −45/80 (35) | −20/60 (40) | G.S. 22 (34) | Very satisfied |
| After surgery | −5/70 (65) | −10/85 (75) | −15/70 (55) | C.P. 6.4 | |
| 2 | |||||
| Before surgery | 30/55 (25) | 50/80 (30) | 10/60 (50) | G.S. 34 (44) | Very satisfied |
| After surgery | −30/85 (55) | 15/90 (105) | 0/80 (80) | C.P. 8.5 (95) | |
| 3 | |||||
| Before surgery | −40/60 (20) | −40/50 (10) | −25/30 (5) | G.S. 12 (24) | Satisfied |
| After surgery | 30/70 (40) | −20/50 (30) | −20/40 (20) | C.P. 1.9 (33) | |
| Average | |||||
| Before surgery | −28/58 (30) | −45/70 (25) | −18/50 (32) | G.S. 23 ± 9 (34 ± 8) | |
| After surgery | −22/75 (53) | −5/75 (70) | −12/63 (52) | C.P. 5.6 ± 2.8 (6.8 ± 2.6) | |
M.Br modified Brand method, TAM total active motion; GS grip strength, CP chuck pinch, N. Side not affected side
Patient 1
A 56-year-old man injured the center of his left hand while using a press machine 2 weeks prior to our initial consultation. The skin on both dorsal and volar surfaces of the hand was viable (Fig. 2a), but the distal metacarpal bone of the middle finger was missing (Fig. 2b) at the initial consultation. During the first reconstructive surgery, a reduction of the severely comminuted metacarpal head of the middle finger was difficult, and therefore, the metacarpal head was replaced by costal osteocartilage grafting (Fig. 3a,b). Severe flexor tendon adhesion was released at 4 months post-injury, which was priory to mild extensor tendon adhesion. After that, the M. Brand surgery was executed 6 months post-injury (Fig. 3c,d,e). The range of motion of the middle finger improved after the M. Brand surgery, particularly the PIP joint extension (Fig. 4a,b). Two years later, the active range of motion has been maintained without pain; the outcome is satisfactory both clinically and radiographically (Fig. 5a,b,c).
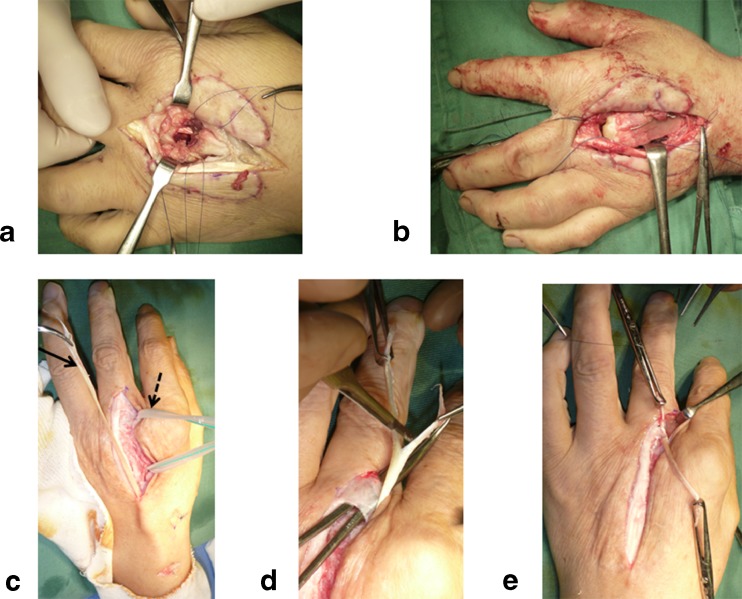
Fig. 3.
(Patient 1) Intra-operative photograph. a,b First reconstructive surgery of the MP joint at 2.5 weeks after injury demonstrating a missing distal metacarpal bone of the middle finger and b total replacement by costal osteo-cartilage grafting. c,d,e The M. Brand surgery at 6 months post-injury. The single whole PL indicated by the arrow in (c) was sutured with inter-lace stitches to the end of re-routed ECRL. The PL was passed through a subcutaneous tunnel obliquely across the MP joint, as indicated by the pointed arrow in (c). After the end of the PL was divided into two (d), each end of the PL was then sutured with inter-lace stitches to the radial lateral band and oblique fiber, respectively (e)
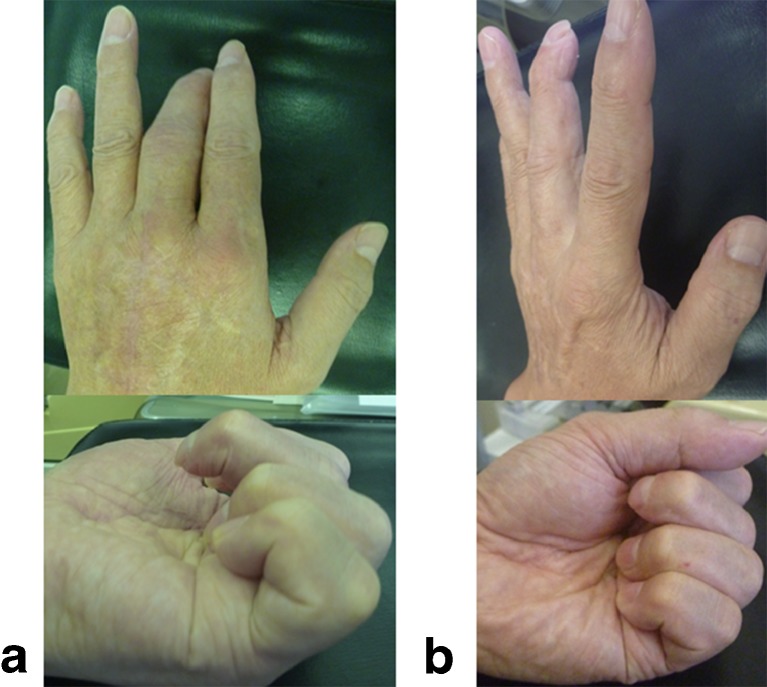
Fig. 4.
(Patient 1) Active extension and flexion of the fingers 6 months later; a before and b after surgery using the M. Brand procedure
Fig. 5.
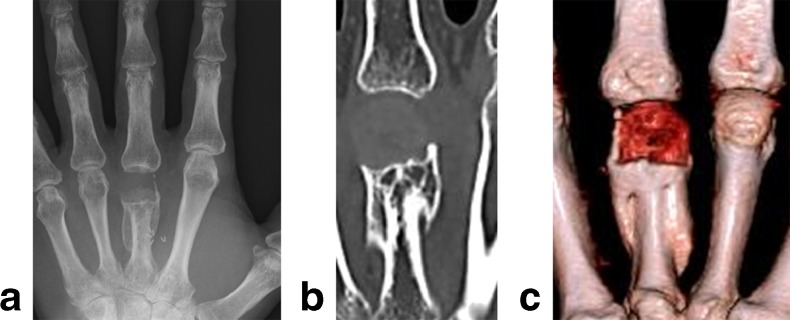
(Patient 1) Imaging 2 years after injury demonstrating a X-ray, b CT, and c 3D-CT
Patient 2
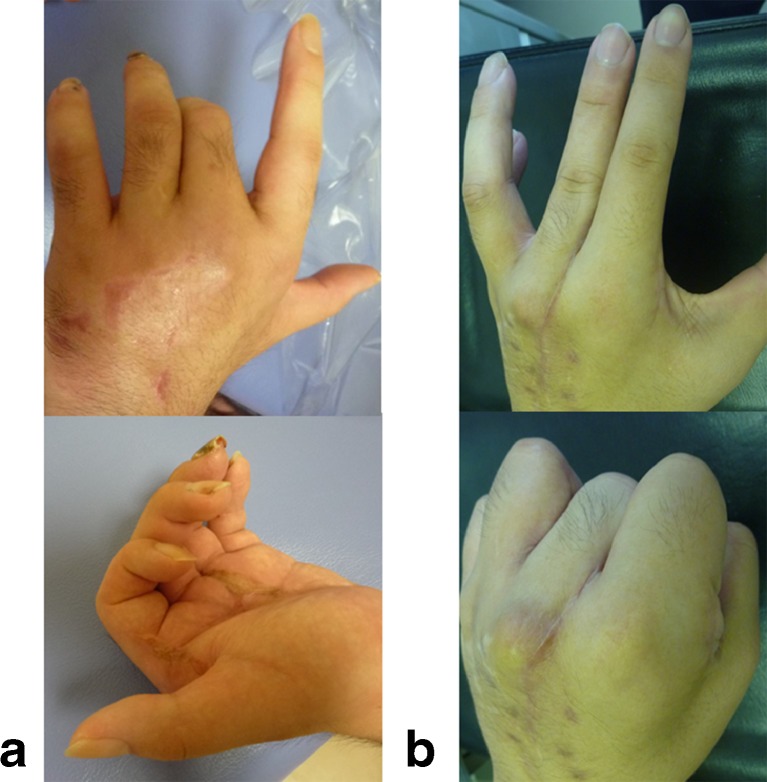
A 20-year-old man received the M. Brand surgery 3 months after an injury. The patient was very satisfied with the functional improvement by the M. Brand surgery, although the palmar subluxation of the base of the proximal phalanx at the MP joint worsened due to the increase of flexion force on the unstable MP joint (Fig. 6a,b).
Fig. 6.
(Patient 2) Active extension and flexion of the fingers 3 months post-injury, a before and b after the surgery using the M. Brand procedure
Patient 3
A 61-year-old woman was moderately satisfied with the improvement of the extension lag after the M. Brand surgery. The improvement of the TAM of the PIP joint with an intra-articular fracture was poor compared to the other two cases.
Discussion
Compared to other methods using flexor digitorum superficialis (FDS) or EIP as a power source, proximally re-routing the ECRL is an easy and safe method. In our series of three cases, partial laceration of the FDS was observed in all cases, and complete rupture of EIP was observed in one case. In the distal portion, interlacing the suture to the injured lateral band with sufficient strength was possible by adjusting the length of the grafted PL. Adjusting the tension by using PL grafting through the dense scar tissue was relatively easy and safe. Although we used ECRL in this case series, the extensor carpi radialis brevis (ECRB) can be an alternative power source.
When the radial lateral intrinsic tendon of the middle finger is reconstructed after a crushing–penetrating injury around the MP joint, disabilities due to intrinsic muscle paralysis [1] can be partially improved in terms of function. Our results show that surgical intervention using the M. Brand method was efficacious for this type of trauma in terms of both patient satisfaction and improvement of TAM. The extension lag of the finger could affect the ability of patients to perform activities of daily living, such as washing their face or typing. Increasing the IP joint extension could increase the working space of pinch motion and strengthen chuck pinch, which uses the finger pulp. Therefore, we believe that this procedure could be an option for motivated patients.
However, care must be taken in the recovery of the stability and movement of the repaired MP joints. We observed worsening of palmar subluxation of the base of the proximal phalanx at the MP joint in patient 2. Stabilization of the MP joint was a priority for repair, especially during the early reconstruction period. In our series, total replacement by costal osteocartilage grafting [5], but not partial replacement, seemed to provide better stabilization of the MP joint.
A severely damaged PIP joint or unstable MP joint seemed to be the relative contraindications for this procedure. A patient without motivation to rehabilitate also seemed to be a contraindication, as active and continuous rehabilitation and self-care were necessary.
In conclusion, tendon transfer using the M. Brand method was a useful option for patients with an extension lag of IP joints after a crushing–penetrating injury around the MP joint. The timing of the M. Brand surgery was not rushed, but MP joint reconstruction was vital. We recommend M. Brand surgery after the MP joint stabilizes.
Acknowledgments
Conflict of Interests
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this study. All named authors (Yoshitaka Hamada, MD; Naohito Hibino, MD) hereby declare that they have no conflicts of interests of interest to disclose.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation 140 (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
Identifying information, including patients' names, initials, or hospital numbers, were not published in written descriptions, photographs, and pedigrees.
References
- 1.Brand PW. Paralytic claw hand; with special reference to paralysis in leprosy and treatment by the sublimis transfer of Stiles and Bunnell. J Bone Joint Surg Br. 1958;40:618–32. doi: 10.1302/0301-620X.40B4.618. [DOI] [PubMed] [Google Scholar]
- 2.Campbell Reid DA. Multilating Injuries of the Hand. London: Churchil Livingstone; 1979. pp. 3–14. [Google Scholar]
- 3.Coulet B, Boretto JG, Lazerges C, et al. Rollover hands: classification of injuries and therapeutic strategy. Chir Main. 2011;30:246–54. doi: 10.1016/j.main.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Ozçelik B, Ertürer E, Mersa B, et al. An alternative classification of occupational hand injuries based on etiologic mechanisms: the ECOHI classification. Ulus Travma Acil Cerrahi Derg. 2012;18:49–54. doi: 10.5505/tjtes.2012.45656. [DOI] [PubMed] [Google Scholar]
- 5.Sato K, Sasaki T, Nakamura T, et al. Clinical outcome and histologic findings of costal osteochondral grafts for cartilage defects in finger joints. J Hand Surg Am. 2008;33:511–5. doi: 10.1016/j.jhsa.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Tubiana R, Gilbert A, Masquelet AC. An Atlas of Surgical Techniques of the Hand and Wrist. London: Martin Dunitz Ltd; 1999. pp. 341–2. [Google Scholar]