Abstract
Background: To describe trends in labor induction, including elective induction, from 2001 to 2007 for six U.S. health plans and to examine the validity of induction measures derived from birth certificate and health plan data.
Methods: This retrospective cohort study included 339,123 deliveries at 35 weeks' gestation or greater. Linked health plan and birth certificate data provided information about induction, maternal medical conditions, and pregnancy complications. Induction was defined from diagnosis and procedure codes and birth certificate data and considered elective if no accepted indication was coded. We calculated induction prevalence across health plans and years. At four health plans, we reviewed medical records to validate induction measures.
Results: Based on electronic data, induction prevalence rose from 28% in 2001 to 32% in 2005, then declined to 29% in 2007. The trend was driven by changes in the prevalence of apparent elective induction, which rose from 11% in 2001 to 14% in 2005 and then declined to 11% in 2007. The trend was similar for subgroups by parity and gestational age. Elective induction prevalence varied considerably across plans. On review of 86 records, 36% of apparent elective inductions identified from electronic data were confirmed as valid.
Conclusions: Elective induction appeared to peak in 2005 and then decline. The decrease may reflect quality improvement initiatives or changes in policies, patient or provider attitudes, or coding practices. The low validation rate for measures of elective induction defined from electronic data has important implications for existing quality measures and for research studies examining induction's outcomes.
Introduction
Nearly one million U.S. births (23%) were induced in 2008.1 Induction can be performed for a medical or obstetric indication or it can be “elective,” which includes inductions performed for the woman's comfort or convenience or for conditions not meeting criteria for an accepted indication (e.g., induction for “post-term pregnancy” at 40 weeks gestation). We are not aware of evidence that induction for these reasons improves outcomes.
Prior studies reported that induction increased rapidly in the 1990s, for example, from 9% in 1989 to 19% in 1998.2,3 As induction rates rose, concerns were raised that induction might increase the risk of cesarean delivery and other adverse outcomes. In addition, influential studies demonstrated that delivery before 39 weeks' gestation (including early elective delivery) was associated with worse outcomes, including increases in neonatal intensive care unit (NICU) admission and infant death.4–6 These findings spurred local and national initiatives, many beginning between 2001 and 2008, to reduce elective delivery, particularly before 39 weeks' gestation.7–11
While studies have examined the impact of specific initiatives at single institutions or health care systems, there is little information available about general trends in induction in the United States in recent years. Two studies reported that early-term12 and late preterm13 induction rates increased through 2006, but these studies relied on birth certificate data, which miss many inductions14 and do not reliably distinguish elective from indicated inductions.15 A recent study of specialty hospitals was the first to provide nationally representative data, reporting an 11% increase in induction from 2006 to 2010.16 At the same time, the authors observed a substantial reduction in early-term iatrogenic delivery, including elective induction. It would be valuable to know whether these trends hold true for a broader range of U.S. hospitals, as well as those providing advanced perinatal care. In addition, few studies have examined trends for induction at 39–40 weeks' gestation, when most elective inductions are performed, or drawn on health plan or medical records data, which would likely improve accuracy compared to birth certificate data.
Our objective was to describe trends in induction for women enrolled in six U.S. health plans delivering in a variety of hospital settings from 2001 through 2007, drawing on health plan as well as birth certificate data. We also examined the validity of an algorithm for identifying inductions from these computerized data.
Materials and Methods
Overview
We conducted a retrospective cohort study using linked health plan and birth certificate data from 2001 to 2007. Data came from the Medication Exposure in Pregnancy Risk Evaluation Program (MEPREP).17 Six health plans participated: Group Health (Seattle, Washington); HealthPartners (Minneapolis, Minnesota); and Kaiser Permanente Colorado (Denver), Southeast (Atlanta, Georgia), Northwest (Portland, Oregon), and Northern California (Oakland). Procedures were approved by each organization's institutional review board and state departments of public health.
MEPREP methods have been described.17 Each health plan identified potential deliveries, linked them with infants, obtained birth certificate data, and created standardized datasets of health plan and birth certificate data.18 A validation study showed high positive predictive value (PPV) for selected maternal medical conditions and birth certificate variables.19 For the current study, a programmer at the lead site wrote SAS programs that were implemented at other sites, yielding deidentified summary data that were returned to the lead site for analysis.
Population
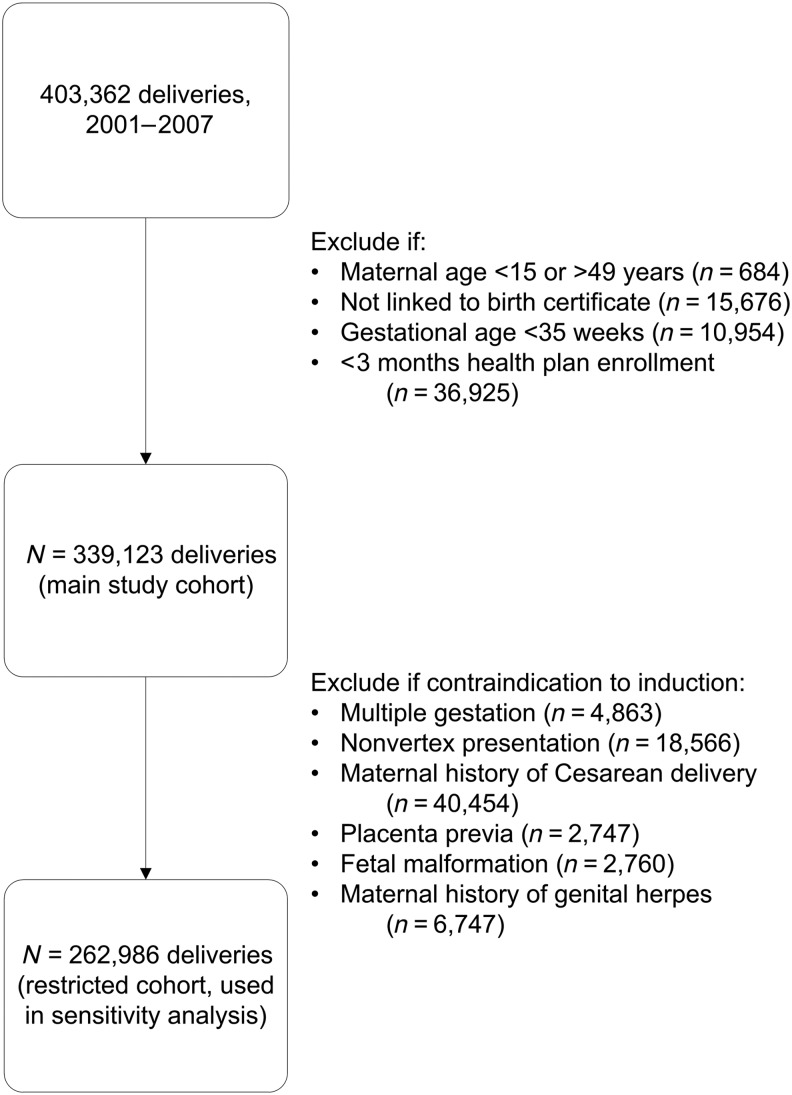
These analyses included deliveries of live-born infants to women age 15–49 years at 35 weeks' gestation or beyond from January 1, 2001, to December 31, 2007. We included only women enrolled in the health plan for at least the 3 months prior to the birth and only deliveries that could be linked to a birth certificate and an enrolled infant. Figure 1 shows the impact of applying these inclusion criteria to create the main study cohort (middle box). For a sensitivity analysis, we limited the population to women with no contraindications to vaginal delivery or induction (Fig. 1, bottom). More information about these contraindications and how they were measured is provided below.
FIG. 1.
Flow of deliveries through the study, showing inclusion and exclusion criteria.
Measures
In defining the study population, we used information about maternal age and enrollment from health plan data. Gestational age was defined from the clinical estimate recorded on the birth certificate or when missing (1%), the date of the last menstrual period, also from the birth certificate.
Contraindications to induction and/or vaginal delivery (used as exclusion criteria in a sensitivity analysis) were based on recommendations from the American College of Obstetrics and Gynecology (ACOG)20 and included multiple gestation, nonvertex presentation, genital herpes, placenta previa, and fetal malformation. We also excluded women with a history of cesarean delivery because our data do not allow us to specifically identify women with a history of a classical or other high-risk incision, in whom the risk of uterine rupture is high. These conditions were defined as present if documented in birth certificate or health plan data.
Induction was defined as present if documented in either health plan or birth certificate data. This approach improves sensitivity (e.g., from 52% to 86%) compared to relying on birth certificate data alone.14 Induction was identified based on International Classification of Diseases, Ninth Revision diagnosis codes (659.0[0,1,3] or 659.1[0,1,3]) and procedure codes (73.01, 73.1, and 73.4).
No variables specifically identify elective induction. Therefore, we operationalized elective induction as induction without an accepted medical indication recorded in birth certificate or health plan data. Indications (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/jwh) were based on ACOG recommendations 20 and included post-term pregnancy (≥41 completed weeks of gestation), diabetes, hypertension, preeclampsia, eclampsia, prelabor rupture of membranes, maternal heart disease, and others. Inductions with no documented indication other than macrosomia (2%) were categorized as elective because there is scant evidence that such inductions improve outcomes.21 We also conducted a sensitivity analysis with these inductions reclassified as indicated.
Birth certificate data cover the entire duration of pregnancy. In health plan data, we searched for indications during the current pregnancy (at a minimum, the final 3 months of pregnancy). Health plan data were needed because birth certificate data alone lack sensitivity for indications for induction.14,15,22
Maternal age and insurance status were defined from health plan data, while maternal race, education, parity, and infant birth weight were defined from birth certificate data. Race/ethnicity data were unavailable at one site for deliveries in 2007 (accounting for 64.7% of deliveries in 2007 and 9.4% of the overall study population) due to changes in birth certificate race coding.
Validation study
We conducted a small chart review study to validate our elective induction algorithm. Because resources were limited, this process was designed to be exploratory and to provide context about the validity of our elective induction measure that was not available in previous large studies. We chose to focus on deliveries that appeared to be electively induced, rather than those with no evidence of induction or that appeared to be induced for a medical or obstetric indication. Thus we can estimate the PPV of our algorithm but not its sensitivity or specificity, which would have required a much larger validation study.
Four health plans volunteered to participate in the validation study, performing 18, 22, 23, and 23 reviews, respectively (86 total). Sites did as many reviews as resources could support. The prevalence of induction was similar at the plans that participated (range, 30% to 38% of deliveries) and those that did not (27% and 33%). To improve efficiency, plans limited review to readily available records (e.g., deliveries at health plan-owned hospitals or those with electronic medical records). Because we wanted to compare the accuracy of birth certificate and health plan data, we selected approximately half of the cases from those identified as induced from the birth certificate alone. Apart from these considerations, sampling was random. A trained abstractor at each site was provided with a standardized abstraction form and manual and participated in a joint training call. A physician-investigator (SD) adjudicated all reviews with input from an obstetrician-investigator (AC).
Statistical analyses
We examined characteristics of the study population overall and stratified by study year or induction status. We calculated percentages for categorical variables and means and standard deviations for continuous variables. Chi-squared tests and analysis of variance were used to test for statistical significance. Because race/ethnicity data were missing for one large site in 2007, which could potentially yield misleading results in these descriptive analyses, we imputed the 2007 race/ethnicity distribution at that site based on its 2006 data.
Our primary analyses examined trends in the prevalence of induction overall, medically indicated induction, and apparent elective induction. Prevalence was calculated by dividing the number of induced births by the total births for the time period. Prevalence estimates were also calculated for subgroups defined by health plan, gestational age, and parity. This process was repeated for elective induction. To assess whether changes in population characteristics explained temporal changes in induction, we carried out sensitivity analyses that standardized estimates using the predictive marginal method.23 Results changed little, and so the non-standardized results are presented.
In sensitivity analyses, we explored the impact of defining induction from health plan data alone and also of excluding women with conditions that may be contraindications to induction (listed in Fig. 1).
For the validation study, we estimated the PPV of our algorithm for elective induction and calculated exact 95% binomial confidence intervals.
Analyses were performed using SAS software, version 9.2 (SAS Institute, Inc., Cary, NC).
Results
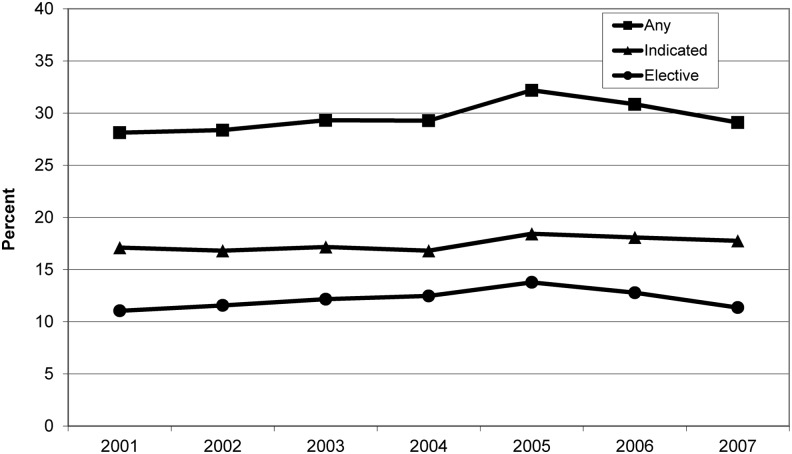
There were 339,123 eligible deliveries from 2001 to 2007 (Table 1). Between 2001 and 2007, there was a shift toward delivery at earlier gestational ages. Overall, 100,459 deliveries (29.6%) were induced. This proportion rose from 28.1% in 2001 to 32.2% in 2005 and then declined to 29.1% in 2007 (Fig. 2). Among induced deliveries, 58.9% had one or more accepted indications documented (Table 2). The prevalence of medically indicated induction changed little over time (Fig. 2). Elective induction (that is, with no accepted indication documented) occurred in 11.0% (95% confidence interval [95% CI], 10.7%–11.3%) of deliveries in 2001, rising to 13.8% (13.5%–14.1%) in 2005 and then declining to 11.3% (11.1%–11.6%) in 2007 (Fig. 2). Results were similar when estimates were standardized for race/ethnicity, maternal age, and parity.
Table 1.
Characteristics of the Study Population
| Characteristic | All years N=339,123 %a | 2001 n=46,446 %a | 2002 n=48,131 %a | 2003 n=47,608 %a | 2004 n=46,947 %a | 2005 n=48,664 %a | 2006 n =51,825 %a | 2007 n=49,502 %a |
|---|---|---|---|---|---|---|---|---|
| Gestational age, weeks | ||||||||
| 35–38 | 28.0 | 25.5 | 25.9 | 27.3 | 29.0 | 29.2 | 29.4 | 29.3 |
| 39 | 29.7 | 27.6 | 27.9 | 29.0 | 30.5 | 30.4 | 30.3 | 31.7 |
| 40 | 28.8 | 31.3 | 31.3 | 29.4 | 27.5 | 27.7 | 27.5 | 26.7 |
| 41+ | 13.6 | 15.5 | 14.8 | 14.4 | 12.9 | 12.7 | 12.8 | 12.3 |
| Maternal race/ethnicitya | ||||||||
| Non-Hispanic White | 52.3 | 53.3 | 52.6 | 52.4 | 52.6 | 52.1 | 51.8 | 51.5 |
| Hispanic White | 19.9 | 19.9 | 19.8 | 19.0 | 18.7 | 20.0 | 20.1 | 21.6 |
| Asian | 9.4 | 8.0 | 8.8 | 9.4 | 9.9 | 9.8 | 9.6 | 9.8 |
| Black | 8.4 | 9.6 | 9.1 | 8.7 | 8.3 | 8.0 | 8.3 | 6.7 |
| Other | 10.1 | 9.1 | 9.7 | 10.4 | 10.4 | 10.1 | 10.2 | 10.4 |
| Parity | ||||||||
| Nulliparous | 43.1 | 40.4 | 41.3 | 43.0 | 42.7 | 43.8 | 44.9 | 45.1 |
| Maternal age, years | ||||||||
| 15–19 | 4.6 | 5.7 | 5.1 | 4.4 | 4.2 | 4.1 | 4.5 | 4.5 |
| 20–24 | 15.2 | 17.5 | 16.4 | 15.6 | 14.5 | 14.1 | 14.2 | 14.2 |
| 25–29 | 28.8 | 28.0 | 28.4 | 28.5 | 28.7 | 28.8 | 29.7 | 29.6 |
| 30–34 | 30.9 | 29.9 | 30.7 | 31.6 | 31.7 | 31.4 | 30.3 | 30.6 |
| 35–39 | 16.6 | 15.5 | 15.7 | 16.1 | 17.0 | 17.3 | 17.4 | 17.2 |
| 40–44 | 3.7 | 3.3 | 3.5 | 3.7 | 3.8 | 3.9 | 3.8 | 3.7 |
| 45–49 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 |
Percent of non-missing values. At the time of this study, race/ethnicity data were unavailable at one site for deliveries in 2007 (accounting for 64.7% of deliveries in 2007 and 9.4% of the study population overall) because of changes in birth certificate race coding. Thus for that site only, we imputed the race/ethnicity distribution in 2007 based on the distribution in 2006. Otherwise, <1% of data were missing for all characteristics in all years. No statistical tests were used to compare proportions over time because due to very large numbers, nearly all tests would be highly statistically significant, even for clinically unimportant differences.
FIG. 2.
Prevalence of induction of labor in six U.S. health plans, 2001–2007. The lines indicate the prevalence of induction for any indication (squares), induction for a medical or obstetric indication (triangles), and elective induction (circles). Elective induction was defined as induction between 35 and 40 completed weeks' gestation with no documentation of an indication listed in Table 2.
Table 2.
Indications for Induction
| Reason for inductiona | % of inductionsa |
|---|---|
| Medical or obstetrical indication | 58.9 |
| Gestational age of ≥41 completed weeks | 23.2 |
| Prelabor rupture of membranes | 18.1 |
| Gestational hypertension or preeclampsia | 19.2 |
| Diabetes (pre-existing or gestational) | 10.0 |
| Oligohydramnios | 7.0 |
| Hypertension, chronic | 5.8 |
| Intrauterine growth restriction | 3.8 |
| Maternal chronic heart disease | 2.1 |
| Maternal chronic renal disease | 1.2 |
| Placental abruption | 1.0 |
| Eclampsia | 0.4 |
| ABO incompatibility or isoimmunization | 0.3 |
| Fetal distress before onset of labor | <0.1 |
| Elective (gestational age of 35–40 completed weeks with none of the above indications)b | 41.1 |
From linked health plan and birth certificate data. Percentages add up to more than the subgroup total because multiple indications can be present for a single delivery.
Includes 2.3% of induced deliveries that had a code for macrosomia and no other documented indication.
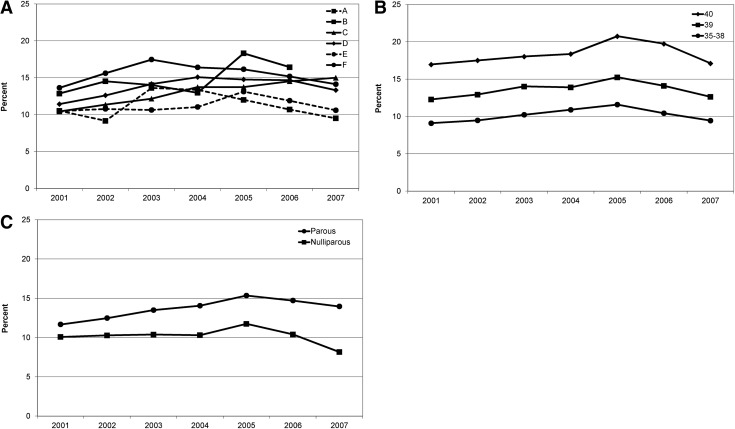
For elective induction, the lowest prevalence at any site in any year was 9.2% and the highest 18.3%. The temporal trend was similar at nearly all sites (Fig. 3A). The peak occurred in 2003 at two sites, 2004 at one site, and 2005 at two sites (Fig. 3A). One site (Site C) showed an increase over the entire time period.
FIG. 3.
Prevalence of elective induction for subgroups of deliveries, 2001–2007. (A) By health plan. Each line represents one health plan, labeled with a letter (A–F). (B) By gestational age. Lines represent the following gestational ages: 40 completed weeks (diamonds); 39 completed weeks (squares); and 35–38 completed weeks (circles). (C) By parity. Lines represent parous (circles) and nulliparous (squares) women.
Elective induction was most common at 40 completed weeks of gestation (Fig. 3B), and this group experienced the greatest absolute decline in elective induction, from 20.8% to 17.1% of births. The decline was 2.6-fold greater in nulliparous than parous women (Fig. 3C).
Women undergoing elective induction were less likely to be nulliparous (39.2%) than women who were not induced (47.3%) or who underwent indicated induction (57.6%; p<0.001; Table 3). Women with elective induction were more likely to be non-Hispanic white than women who were not induced.
Table 3.
Characteristics of Deliveries by Induction Status
| Characteristica | Not induced n=178,404%c | Indicated inductionb n=50,583%c | Elective inductionb n=33,999%c |
|---|---|---|---|
| Maternal age, years | |||
| 15–19 | 5.8 | 5.1 | 4.4 |
| 20–24 | 16.9 | 16.4 | 16.8 |
| 25–29 | 30.0 | 29.6 | 30.9 |
| 30–34 | 29.7 | 29.4 | 30.7 |
| 35–39 | 14.5 | 15.7 | 14.1 |
| 40–44 | 2.9 | 3.7 | 2.8 |
| 45–49 | 0.1 | 0.2 | 0.1 |
| Maternal age, mean (SD), years | 29.0 (5.7) | 29.3 (5.8) | 29.1 (5.5) |
| Maternal race/ethnicity | |||
| Non-Hispanic White | 49.4 | 58.7 | 61.6 |
| Hispanic White | 21.0 | 16.7 | 15.3 |
| Asian | 10.5 | 7.1 | 7.1 |
| Black | 7.8 | 9.3 | 8.7 |
| Other | 11.3 | 8.2 | 7.3 |
| Nulliparous | 47.3 | 57.6 | 39.2 |
| Gestational age, completed weeks | |||
| 35–38 | 26.8 | 23.6 | 22.1 |
| 39 | 30.1 | 17.6 | 32.3 |
| 40 | 32.3 | 18.1 | 45.6 |
| 41+ | 10.8 | 40.6 | 0.0 |
| Gestational age, mean (SD), weeks | 39.2 (2.0) | 39.6 (2.1) | 39.1 (1.0) |
| Maternal education | |||
| <High school | 9.7 | 7.4 | 7.2 |
| High school graduate/some college | 59.6 | 62.1 | 63.1 |
| College graduate or above | 30.8 | 30.3 | 29.7 |
| Insurance status | |||
| Medicaid | 5.8 | 5.9 | 6.1 |
| Other insurance | 94.2 | 94.1 | 93.9 |
| Diabetes | 6.4 | 15.9 | 0.0 |
| Hypertension, chronic | 2.3 | 10.0 | 0.0 |
| Gestational hypertension or pre-eclampsia | 6.2 | 30.4 | 0.0 |
| Infant birth weight, g | |||
| <2500 | 2.2 | 4.9 | 1.2 |
| 2500–3499 | 54.8 | 45.4 | 48.5 |
| 3500–3999 | 31.9 | 33.0 | 35.9 |
| 4000+ | 11.0 | 16.6 | 14.4 |
| Birth weight, mean (SD), g | 3,429 (472) | 3,477 (560) | 3,516 (442) |
Population is the restricted cohort (women without contraindications to induction; see Fig. 1 for a list of contraindications). All values are % unless otherwise indicated. Percentages are of non-missing values. Less than 5% of data were missing for all characteristics except for race, which was missing for 9.9% of deliveries (10.3% of non-induced deliveries, 9.5% of medically indicated inductions, and 8.3% of elective inductions). The high proportion of missing data for race is due to changes in birth certificate race coding affecting one large site in 2007. Results changed little in a sensitivity analysis imputing that site's 2007 racial distribution was based on its 2006 data.
p-values were calculated using chi-squared tests for categorical variables and analysis of variance for continuous variables; p <0.001 for all comparisons.
Elective induction was defined as induction between 35 and 40 completed weeks' gestation without documentation of an indication from Table 2.
Results were similar in sensitivity analyses (Supplementary Fig. S1), including analyses excluding women with possible contraindications to induction, defining induction from only health plan data, and reclassifying inductions for macrosomia as medically indicated.
The validation study included only deliveries which based on both health plan and birth certificate data appeared to be initiated by elective induction. Of 86 deliveries, 43 (50%) were confirmed as induced. The proportion confirmed as induced was similar for the 43 inductions identified only on the birth certificate (43%, 95% CI 27%–59%) and the 27 identified only from health plan data (44%, 95% CI 25%–65%). It was higher for the 19 deliveries for which both sources identified the delivery as induced (74%, 95% CI 49%–91%). 31 of the 43 induced deliveries were confirmed to be elective. Thus, the overall PPV for our elective induction algorithm was 36% (31/86), with 95% CI 26%–47%. The PPV ranged from 22% to 52% across the four sites. It was the same in the first and second halves of the study period (2001–2004 vs. 2005–2007), though these estimates are subject to uncertainty because they are based on small numbers.
In some cases, circumstances were noted on chart review that might have led to a woman being coded as induced when in fact she was not. For example, in some cases it appeared that induction was planned but a woman went into spontaneous labor before she could be induced, while in other cases, medical records showed that labor was augmented rather than induced.
Discussion
In this U.S. cohort, the prevalence of induction overall and of apparent elective induction rose from 2001 to 2005 and then declined slightly. The largest absolute decreases were seen for nulliparous women and women delivering at 40 weeks' gestation.
An important finding is that only 36% of apparent elective inductions defined from computerized data were confirmed on medical record review. If this proportion has been stable over time, as our validation study suggests, then the trends we describe are likely accurate. Rates of medically indicated induction were stable over time, which offers indirect evidence for stability of coding practices. Still, there is uncertainty around our trend estimates due to the low PPV of our induction measures. Of note, most previous studies relied on birth certificate data alone and did not validate their measures.2,3,12,13 We combined health plan data with birth certificate data, which should improve accuracy.14
We observed an apparent prevalence of 30% for induction overall and 12% for elective induction in 2001 through 2007. The exact proportions may not be that meaningful given the measurement challenges discussed above. For comparison, U.S. birth certificate data (which lack sensitivity for induction14) showed an induction prevalence of 23% in 2008,1 while a study using electronic medical records (EMR) data reported a prevalence of 45% in nulliparous women and 31% in parous women for 2002 through 2009.24 In terms of trends, Danilack et al. reported that at U.S. specialty hospitals, the overall prevalence of induction increased from 20% in 2006 to 22% in 2010 while at the same time induction declined slightly in preterm and early-term deliveries.16 In contrast, Murthy et al. examined birth certificate data and reported that between 2001 and 2006, the prevalence of early-term induction increased.12 None of these studies validated their measure of induction nor examined whether validity changed over time.
The trends we observed may have been influenced by national or local initiatives, physician practice changes, patient preferences, or coding changes. Studies have shown that at specific institutions, initiatives to reduce elective induction decreased induction rates between 2001 and 2008.7–11 For example, at one hospital, induction prevalence decreased from 30% to 25%,11 while at another, elective induction declined from 26% to 21%.8 At U.S. specialty hospitals, from 2006 to 2010 there was a marked decrease in non-indicated iatrogenic delivery (including both induction and cesarean delivery) at 37 and 38 weeks' gestation.16 Few studies have examined clinical outcomes accompanying these changes. Ehrenthal reported that after a local initiative to limit elective delivery before 39 weeks' gestation, NICU admissions decreased but macrosomia and stillbirth increased.10 These findings raise concern that such initiatives could have unintended consequences.
Strengths of this study include the inclusion of 6 health plans representing a large and diverse population and multiple hospitals and U.S. regions. Incorporating electronic health plan data should improve accuracy compared to birth certificate data alone.14 Nonetheless, our measure of elective induction has limitations. In addition to false positives, there may be false negatives: some true inductions may have been missed, and some inductions that were truly elective may have been coded as having an indication. Other limitations are that all women in the study were insured and only 5.8% enrolled in Medicaid. Trends may differ for women without commercial insurance. We could not assess whether the trends we observed resulted from specific initiatives or policies.
Many of the participating health plans transitioned from paper records to EMRs between 2003 and 2008. This change may have impacted coding practices and data quality, although it is difficult to predict how it might have affected our results. Different health plans made this transition in different years, and on investigation we found no correlation between the transition to an EMR and induction prevalence. In our validation study, the PPV for elective induction was the same in the first and second halves of our time period, roughly corresponding to the time periods before and after EMR implementation.
Validation of induction measures is a strength of this study, since no prior studies of induction trends have validated their measures. The inclusion of four health plans in the validation study strengthens generalizability. Still, the validation study has limitations. We were able to review only a small number of records at each site, which decreased the precision of our estimates and precluded us from carrying out subgroup analyses (e.g., by parity or gestational age) or drawing conclusions about differences in validity between sites or over time. The ideal study would review a large number of medical records across many years, health care systems, and geographic regions. Such a study is not likely to be feasible because it would be very costly and time consuming.
Our validation study highlights the challenges in using routine electronic data (birth certificate or health plan data) to accurately measure rates of elective delivery. Our findings have important implications for policy, especially for the use of quality measures derived from such data. More research is needed about the optimal algorithms to identify elective induction from electronic data. Other directions for future research include examining the validity of induction measures for patient subgroups and comparing validity between health care systems and over time. Such a study could also explore the impact of the transition from paper to electronic medical records. In addition, to understand the quality of data available to support policy decisions, it would be useful to compare induction trends based on birth certificate data alone with those incorporating health plan, insurance claims, or EMR data.
The broader context for our work is that considerable uncertainty remains about the risks and benefits of elective induction at term. Few randomized trials have been conducted, all were small,25–30 and most took place 20 or more years ago.26–28,30 Given this lack of data, it is notable that in our cohort, the greatest decline in elective induction was seen for deliveries at 40 weeks—a group in which elective induction is not thought to be harmful. Initiatives to prevent early-term elective delivery may also decrease elective induction at 39 and 40 weeks, the clinical impact of which is not known.
Conclusions
We observed an apparent decline in elective induction in recent years, as well as considerable variation between health plans. This variation may be influenced by differences in patient preferences or coding patterns. It likely also reflects true variability in clinical practice. Better evidence is needed to support clinical decisions and policy related to elective induction at term. Initiatives to decrease elective induction should be accompanied by monitoring of clinical outcomes to detect unintended consequences.
Supplementary Material
Acknowledgments
We thank the state departments of health that provided birth certificate data used in this project and the programmers and project managers in the Medication Exposure in Pregnancy Risk Evaluation Project.
This study was funded by AHRQ U18HS0169555 (HMORN CERT) and Group Health Research Institute. Dr. Dublin was funded by grant K23AG028954 from the National Institute on Aging. Dr. Avalos was funded by the University of California San Francisco–Kaiser Permanente Division of Research Building Interdisciplinary Research Careers in Women's Health Program (K12HD052163, National Institute of Child Health and Human Development/National Institutes of Health, PI: Guglielmo). Data linkages for MEPREP were supported through contracts HHSF223200510012C, HHSF223200510009C, and HHSF223200510008C from the U.S. Food and Drug Administration (Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research). The sponsors played no role in the collection, analysis, and interpretation of data or the writing of the manuscript. The opinions expressed are solely the responsibility of the authors and do not necessarily represent the official views or endorsement of the U.S. Food and Drug Administration, National Institute on Aging, or the National Institutes of Health.
Author Disclosure Statement
Dr. Dublin received a Merck/American Geriatrics Society New Investigator Award for unrelated work. Dr. Herrinton received funding from Centocor, Proctor & Gamble, Genentech, and Medimmune. Other authors have no conflicts to report.
References
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ. Births: Final data for 2008. Natl Vital Stat Rep 2010;59:1–72 [PubMed] [Google Scholar]
- 2.Zhang J, Yancey MK, Henderson CE. U.S. national trends in labor induction, 1989–1998. J Reprod Med 2002;47:120–124 [PubMed] [Google Scholar]
- 3.MacDorman MF, Mathews TJ, Martin JA, Malloy MH. Trends and characteristics of induced labour in the United States, 1989–98. Paediatr Perinat Epidemiol 2002;16:263–273 [DOI] [PubMed] [Google Scholar]
- 4.Tita AT, Landon MB, Spong CY, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med 2009;360:111–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol 2009;200:156.e1–4 [DOI] [PubMed] [Google Scholar]
- 6.Zhang X, Kramer MS. Variations in mortality and morbidity by gestational age among infants born at term. J Pediatr 2009;154:358–362, 362.e1. [DOI] [PubMed] [Google Scholar]
- 7.Clark SL, Frye DR, Meyers JA, et al. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol 2010;203:449.e1–6 [DOI] [PubMed] [Google Scholar]
- 8.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol 2009;113:804–811 [DOI] [PubMed] [Google Scholar]
- 9.Donovan EF, Lannon C, Bailit J, et al. A statewide initiative to reduce inappropriate scheduled births at 36(0/7)-38(6/7) weeks' gestation. Am J Obstet Gynecol 2010;202:243.e1–8 [DOI] [PubMed] [Google Scholar]
- 10.Ehrenthal DB, Hoffman MK, Jiang X, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol 2011;118:1047–1055 [DOI] [PubMed] [Google Scholar]
- 11.Reisner DP, Wallin TK, Zingheim RW, Luthy DA. Reduction of elective inductions in a large community hospital. Am J Obstet Gynecol 2009;200:674.e1–7 [DOI] [PubMed] [Google Scholar]
- 12.Murthy K, Grobman WA, Lee TA, Holl JL. Trends in induction of labor at early-term gestation. Am J Obstet Gynecol 2011;204:435.e1–6 [DOI] [PubMed] [Google Scholar]
- 13.Murthy K, Holl JL, Lee TA, Grobman WA. National trends and racial differences in late preterm induction. Am J Obstet Gynecol 2011;205:458.e1–7 [DOI] [PubMed] [Google Scholar]
- 14.Lydon-Rochelle MT, Holt VL, Nelson JC, et al. Accuracy of reporting maternal in-hospital diagnoses and intrapartum procedures in Washington State linked birth records. Paediatr Perinat Epidemiol 2005;19:460–471 [DOI] [PubMed] [Google Scholar]
- 15.Bailit JL. Rates of labor induction without medical indication are overestimated when derived from birth certificate data. Am J Obstet Gynecol 2010;203:269.e1–3 [DOI] [PubMed] [Google Scholar]
- 16.Danilack VA, Botti JJ, Roach JJ, Savitz DA, Muri JH, Caldwell DL. Changes in delivery methods at specialty care hospitals in the United States between 2006 and 2010. J Perinatol 2013;33:919–923 [DOI] [PubMed] [Google Scholar]
- 17.Andrade SE, Davis RL, Cheetham TC, et al. Medication Exposure in Pregnancy Risk Evaluation Program. Matern Child Health J 2011;16:1349–1354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson KE, Beaton SJ, Andrade SE, et al. Methods of linking mothers and infants using health plan data for studies of pregnancy outcomes. Pharmacoepidemiol Drug Saf 2013;22:776–782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrade SE, Scott PE, Davis RL, et al. Validity of health plan and birth certificate data for pregnancy research. Pharmacoepidemiol Drug Saf 2013;22:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ACOG Committee on Practice Bulletins. ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol 2009;114:386–397 [DOI] [PubMed] [Google Scholar]
- 21.Irion O, Boulvain M. Induction of labour for suspected fetal macrosomia. Cochrane Database Syst Rev 2000:CD000938. [DOI] [PubMed] [Google Scholar]
- 22.Lydon-Rochelle MT, Holt VL, Cardenas V, et al. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol 2005;193:125–134 [DOI] [PubMed] [Google Scholar]
- 23.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics 1999;55:652–659 [DOI] [PubMed] [Google Scholar]
- 24.Laughon SK, Zhang J, Grewal J, Sundaram R, Beaver J, Reddy UM. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gynecol 2012;206:486e481–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amano K, Saito K, Shoda T, Tani A, Yoshihara H, Nishijima M. Elective induction of labor at 39 weeks of gestation: a prospective randomized trial. J Obstet Gynaecol Res 1999;25:33–37 [DOI] [PubMed] [Google Scholar]
- 26.Cole RA, Howie PW, Macnaughton MC. Elective induction of labour. A randomised prospective trial. Lancet 1975;1:767–770 [DOI] [PubMed] [Google Scholar]
- 27.Egarter C, Kofler E, Fitz R, Husslein P. Is induction of labor indicated in prolonged pregnancy? Results of a prospective randomised trial. Gynecol Obstet Invest 1989;27:6–9 [DOI] [PubMed] [Google Scholar]
- 28.Martin DH, Thompson W, Pinkerton JH, Watson JD. A randomized controlled trial of selective planned delivery. Br J Obstet Gynaecol 1978;85:109–113 [DOI] [PubMed] [Google Scholar]
- 29.Nielsen PE, Howard BC, Hill CC, Larson PL, Holland RH, Smith PN. Comparison of elective induction of labor with favorable Bishop scores versus expectant management: A randomized clinical trial. J Matern Fetal Neonatal Med 2005;18:59–64 [DOI] [PubMed] [Google Scholar]
- 30.Tylleskar J, Finnstrom O, Leijon I, Hedenskog S, Ryden G. Spontaneous labor and elective induction—A prospective randomized study. I. Effects on mother and fetus. Acta Obstet Gynecol Scand 1979;58:513–518 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.