Abstract
Background
Social capital refers to various levels of social relationships formed through social networks. Measurement differences have lead to imprecise measurement.
Methods
A meta-analysis of eligible studies assessing the bivariate association between social capital and self-reported health and all-cause mortality.
Results
Thirty-nine studies met inclusion criteria, showing social capital increased odds of good health by 27% (95% confidence intervals [CI] =21%, 34%). Social capital variables, reciprocity increased odds of good health by 39% (95% CI = 21%, 60%), trust by 32% (95% CI =19%, 46%). Future research suggests operationalizing measures by assessing differences by race/ethnicity, gender and socioeconomic status.
More than two decades of social capital and health research has shown to reduce mortality (Kawachi, 1999; Kawachi, Kennedy, & Glass, 1999; Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997; Pollack & Knesebeck, 2004) make neighborhoods safer (Kennedy, Kawachi, Prothrow-Stith, Lochner, & Gupta, 1998), and to build more socially cohesive communities (Boneham & Sixsmith, 2006; Cattel, 2001; Woolcock & Narayan, 2000). Public health researchers have employed a communitarian approach, which reflects Robert Putnam's 1993 definition of social capital. This approach focuses on the functions of social relationships to promote an active citizenry. Public health research recommends that social capital should be separated into structural and cognitive forms because these have different relationships with health outcomes (Harpham, 2008; Harpham, Grant, & Thomas, 2002). Structural social capital refers to what people do—associational links, density of social networks, or patterns of civic engagement that can be verified objectively. Coleman (1988) conceptualizes social capital as a resource that originates from the structure of social relationships that facilitate achievement of specific goals. It is important to separate formal networks from informal networks each have different relationships with health outcomes. Also, it is important to note that all relationships can provide value, benefits, and stress.
Cognitive social capital refers to what people feel, or their values or perceptions, and is more subjective. Cognitive social capital is measured at the micro level and is considered to shape behaviors, through control of risk behavior, providing mutual aid and support, and informal means of informational exchange (Cullen & Whiteford, 2001). Cognitive and structural forms of social capital are interrelated: how people feel influences how they act, and how people behave can influence how they feel. The constructs and measures of social capital characterize both structural and cognitive social capital.
Many social capital studies seek to make examine the social capital of a geographic area and often aggregate individual-level data to an ecological level. This limits the focus of social capital constructs and measures on horizontal relationships among neighbors or community members (Kawachi, et al., 1997) and less on the vertical relationships among individuals, communities, neighborhoods, organizations, and sources of power. Bourdieu's (1985) concept of social capital addresses issues of resources and access to power. The Putnam model of social capital directly address neither the relevance of actual or potential resources inherent within social networks that may be used for personal or collective action, nor power dynamics, nor how people access (or may be denied access) to network-based resources (Carpiano, 2008; Wakefield & Poland, 2005).
Although most social capital research hypothesizes social capital as a resource or determinant of health (Szreter & Woolcock, 2004), others argue that social capital may be determined by health (Halpern, 2005). In general, social capital research is characterized as a mechanism to improve health and the causal path cannot be determined from secondary data analysis. More research is needed to identify and understand the pathways by which social capital operates. Social capital research has developed according to the level it scrutinizes: individual, ecological, network, and multilevel.
The diversity in social capital measurement is productive in the sense of showing the range of social capital measures, but becomes detrimental in the sense that it provides imprecise measurement across the literature. A more comprehensive, systematic study of the constructs of social capital may yield fuller explanations what level of analysis capital can advance the study of social capital's benefits for health promotion. The effect of context (e.g. geographical area) has important implications for public health initiatives such as policy interventions to improve the quality of life within a neighborhood. The level of analysis also furthers understanding of the compositional effects of social capital. A multilevel analysis cannot be appropriately implemented until it is clear what is being measured. One remedy for the lack of clarity of social capital is meta-analysis, which can combine all the indicators of social capital and compare their effects on health outcomes.
Methods
Selection of Studies
There was one main inclusion criteria: studies that reported a statistical test of the relationship between the constructs of social capital (e.g. efficacy, participation, trust, reciprocity, sense of community, social support, and social networks) and either/or both self-reported health and all-cause mortality. Self-reported health and all-cause mortality were the two leading outcome measures found in the social capital literature and the search strategy was limited to these variables to limit the number of outcomes being compared for analysis.
A detailed search using MEDLINE (via Pub Med, OVID), Sociological Abstracts, The Cochrane Database of Systematic Reviews, The Cochrane Library, the ISI Web of Knowledge, and PsycInfo was conducted. The searches were conducted using the following search terms: “social capital,” “health,” “self-reported health, and “mortality.” Limitations included “English only.”
Study Coding
Several methodological and conceptual issues are of concern in the social capital literature and were the dominant themes of the coding strategy. Studies were read for themes from the 39 eligible studies and from the broader social capital literature. A process of random checks with a second member of the research team helped to further identify themes and errors in coding and data entry. The coding strategy involved examining studies iteratively and reviewed for:
co-variables reported;
how the independent variables (social capital variables) were measured and conceptualized (e.g. at the individual, neighborhood, community, state, or national levels);
how the dependent variables (e.g. self-reported health measures and/or all-cause mortality) were measured and conceptualized (e.g. at the individual, neighborhood, community, state, or national levels).
After coding each study a second process of coding the social capital variables was performed. The breadth of social capital measures within these 39 studies was vast, which reflected the following larger constructs of social capital: participation, trust, efficacy, sense of community, social support, social networks, bonding, bridging and linking forms of social capital. For the purpose of analyses each of the social capital measures reported were coded to reflect the larger social capital constructs and improved the ability to combine more studies for comparative analyses. Similarly, most studies did not report social measures according to the three forms of social capital (bonding, bridging, and linking). These forms were assigned to the measures according to: bonding (constructs such as participation, trust, and reciprocity), bridging (constructs such as social networks, political or electoral participation) or linking (measures such as voting and trust in legal, political, or government institutions). A number of studies also included a combined social capital measure, constructed by each study author as a social capital index.
Data Analyses
The data analysis occurred in five steps. First, the mean effect size estimates for each study were calculated by averaging the effects across all studies. Second, an overall effect was estimated by outcome (e.g. self-reported health or all-cause mortality). Third, theoretical and methodological characteristics were tested as moderators of the overall effect. Fourth, an overall effect was estimated by each social capital variable. Fifth, an overall effect was estimated by one of the three forms of social capital (e.g. bonding, bridging and linking). Cochran's Q-statistic was calculated to assess statistical heterogeneity (p≤0.05). Sensitivity analyses were performed to identify potential outliers and other threats to validity of results. Mixed-effects models were reported for tests of heterogeneity and moderation. Data management and analyses were performed using Comprehensive Meta-Analysis (version 2) sponsored by the National Institutes of Health (Biostat, Englewood, NJ). Effects of this meta-analysis are reported as odds ratios measured at the 95% confidence level. In most cases, we entered data in the form they appeared in each individual study, correlation coefficients, t-values, P values, odds rations and confidence intervals. In certain cases, a P value and sample size (e.g. studies reporting regression analyses) were entered and the software calculated an effect size.
Initially 13 potential moderators were identified to explore the variability in effect sizes. However, as a result of the non-independence of effects, the constructs of social capital and the three forms of social capital (bonding, bridging and linking) could not be tested as moderators. Instead, the overall effect estimate for each social capital construct was calculated and described to determine its influence on effect size variability. This meta-analysis cannot determine if the independent effects on health of these constructs differ significantly from each other. Three potential moderators met the criteria of effects of dependency and were tested: (1) country (national status of the data: international (one country outside of the United States), multinational (multiple countries), U.S. (data from the United States only); (2) level of analysis (individual, ecological, multilevel), (3) outcome (self-reported health, all-cause mortality) and social capital survey methods (studies focusing on social capital only vs. studies were constructs of social capital were analyzed secondarily).
Publication bias was assessed by computing a “fail-safe” N. This value is an estimate of the number of unretrieved or unpublished studies with null results that would be required to render the observed effect non-significant. In the present analysis, the fail-safe N indicated we would need to locate and include 287.7 missing studies for every observed study for the effect to be nullified, thereby suggesting a low probability of publication bias.
Results
SEARCH STRATEGY
More than 500 studies were identified using this initial search strategy. Second, the titles and abstracts of these studies were reviewed, narrowing the sample of articles to 158. Other potential articles were reviewed from the reference sections of the articles selected from the computer search. Using these methods a total of 39 studies were identified meeting the inclusion criteria.
Study Characteristics
Table 1 contains descriptive statistics of the total sample of studies included in this meta-analysis and reports the overall effect size for each study. A total sample of 39 studies met the inclusion criteria outlined in the methods. These 39 studies yielded 288 effect size estimates. The average number of effect size estimates tested within each study was 7. Self-reported health was an outcome in 28 social capital studies and mortality was the outcome in 9 studies. These studies measured the constructs of social capital using 102 different indicators (specific measures) across social capital constructs. Each of the 288 effect sizes were coded with a social capital construct according to how they were operationally defined within their respective studies. The average number of social capital constructs per study was 2.
Table 1. Social Capital Meta-Analysis Descriptive Statistics by Study.
| Study | Outcome | #of Social Capital Constructs | # of Effects | Odds Ratio |
|---|---|---|---|---|
| Blakely 01 | SRH | 1 | 2 | 1.261 |
| Blakely 06 | Mortality | 2 | 15 | 1.000 |
| Bolin 03/80 | SRH | 1 | 1 | 1.258 |
| Bolin 03/88 | SRH | 1 | 1 | 1.156 |
| Bolin 03/96 | SRH | 1 | 1 | 1.258 |
| Carlson 04 | SRH | 3 | 5 | 1.253 |
| Drukker 05 For Peer Review | SRH | 2 | 6 | 1.300 |
| Folland 07 | Mortality | 1 | 1 | 9.762 |
| Greiner 04 | SRH | 2 | 2 | 1.291 |
| Hyppa & Maki 01 | SRH | 3 | 24 | 1.503 |
| Hyppa &Maki 03 | SRH | 2 | 4 | 1.190 |
| Hyppa 07 | Mortality | 2 | 4 | 1.131 |
| Kavanagh 06 | SRH | 3 | 6 | 1.019 |
| Kim 06a | SRH | 3 | 9 | 1.189 |
| Kim 07 | SRH | 1 | 4 | 1.120 |
| Kim 06b | SRH | 1 | 7 | 1.079 |
| Lindstrom &Lindstrom 06 | Mortality | 1 | 1 | 0.349 |
| Liukkonen et al 04 | SRH | 3 | 14 | 1.023 |
| Lochner 03 | Mortality | 3 | 12 | 1.572 |
| Mellor 05 | Both | 3 | 6 | 3.181 |
| Mohan 05 | Mortality | 5 | 36 | 1.122 |
| Mohseni | SRH | 3 | 8 | 1.628 |
| Muntaner et al 02 | Both | 4 | 44 | 0.984 |
| Pollack 04 | SRH | 4 | 6 | 1.728 |
| Poortinga 06a/00 | SRH | 3 | 7 | 1.451 |
| Poortinga 06a/02 | SRH | 3 | 7 | 1.491 |
| Poortinga 06b | SRH | 4 | 6 | 1.399 |
| Poortinga 06c | SRH | 2 | 5 | 1.364 |
| Rose 00 | SRH | 5 | 7 | 0.932 |
| Skrabski 04 | Mortality | 4 | 9 | 1.143 |
| Subramanian 01 | SRH | 1 | 1 | 1.011 |
| Subramanian 02 | SRH | 1 | 2 | 1.706 |
| Sundquist 06 | SRH | 1 | 2 | 1.173 |
| Taylor 06 | SRH | 1 | 3 | 1.890 |
| Turrell 06 | Mortality | 3 | 6 | 1.000 |
| Veenstra 00 | SRH | 2 | 3 | 2.208 |
| Veenstra 02 | Mortality | 1 | 1 | 1.091 |
| Veenstra 05a | SRH | 1 | 7 | 1.216 |
| Veenstra 05b | SRH | 2 | 3 | 1.177 |
| Total | 89 | 288 | ||
| Average # Per Study | 2 | 7 | ||
| Total # of Studies Analyzed | 39 | |||
| Effect Size Range | 0.349-9.762 |
Overall Effect Size Estimates
The overall weighted effect size estimates and methodological characteristics for each study are presented in Table 1 and Figure 1, while Figure 2 shows from moderator analysis. Results showed that an estimate for the overall weighted effect size for the relationship between social capital and health is OR=1.27 (95% confidence interval [CI] 1.21-1.34) and is significantly different than zero (p=0.0001). The mean effect size within each study estimate ranged from OR=0.35 (95%CI=0.07-1.83) to 9.76 (95%CI=2.80-37.13). The two largest effect sizes were omitted because both were almost three times larger than the next-largest effect and were therefore considered to be outliers. These results suggest that on average, a one-unit increase in social capital increases the odds of having good health by 27%.
Figure 1.
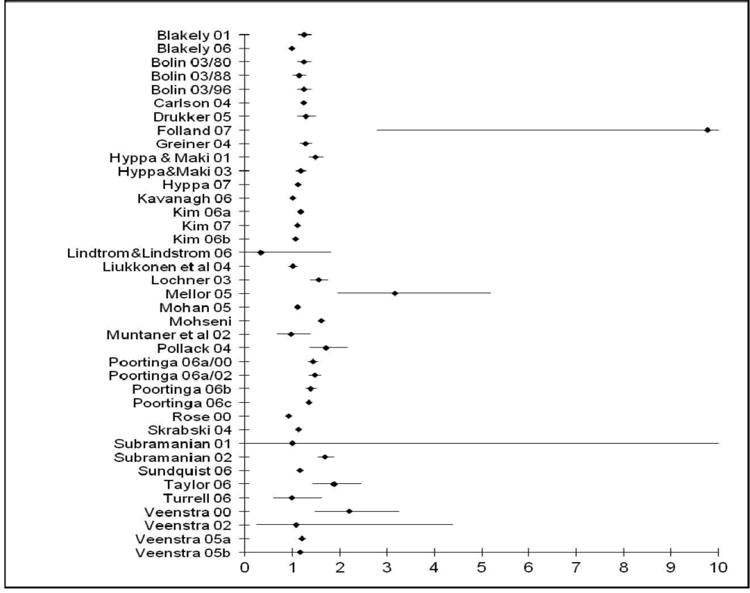
Distribution of effect sizes by study.
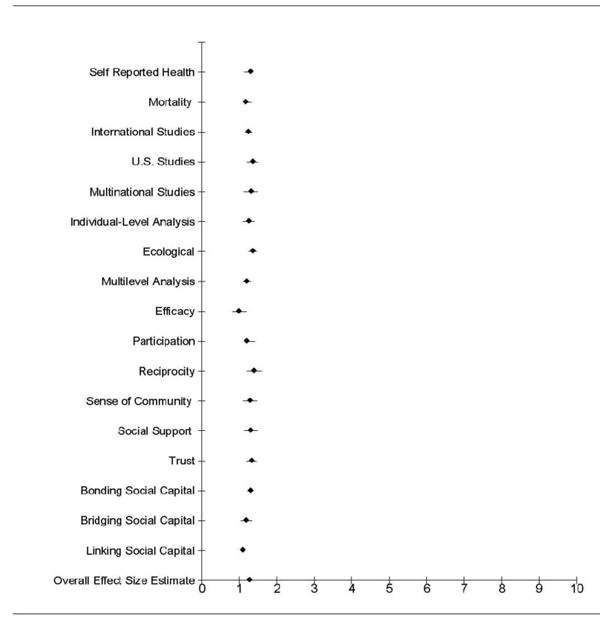
Figure 2. Distribution of Effect Sizes by Moderator.
When the overall effect was recalculated for a sensitivity analysis, with each study removed, all of the overall tests of significance remained significant (p's<0.05). Cochran's Q-test showed that the effects were significantly heterogeneous (Q=862.2, df=38, p=0.0001). As a result of the significant difference of effect sizes across studies (having significant variability), moderation was tested.
Relationship Between Social Capital, Self-Reported Health and All-Cause Mortality
Nine studies examined the relationship between social capital and mortality outcomes and 28 tested the association between social capital and self-reported health. A moderator test showed that the relationship between social capital and self-reported health and the relationship between social capital and mortality were marginally different from one another (Q=3.55, df=1, p=0.0597). Because of this marginal difference, results for each set of studies are reported separately below.
The overall weighted effect size for mortality studies was found to be OR=1.17 (95%CI=1.20-1.33) and for self-reported health OR=1.29 (95%CI=1.21-1.37). These results indicate that an average one-unit increase in social capital will increase the odds of survival by 17% and increase the odds of reporting good health by 29%. Sensitivity tests showed that no one study in either set of outcome studies significantly influenced the overall effect estimate. Regardless of which study was removed for self-reported health studies, the overall estimated effect size range was OR=1.27-1.30 and for mortality studies OR=1.12 - 1.15.
Level of Analysis
The purpose of this analysis was to test whether or not the effect size variability across studies is influenced by the conceptual level and statistical analysis of social capital (e.g., individual versus community/ecological). Thirty-nine studies were analyzed at three different levels of analysis: individual (n=12), group or ecological (n=16), and multilevel (n=11). Studies were characterized by level of analysis according to how each analyzed the relationship between social capital and health (Section 3.5.2). Cochran's Q-test for moderation showed that the effects were not significantly different across these subgroups of studies (Q=4.48, df= 2, p=0.11). The three average effect sizes estimated for each level of analysis were not statistically different from each other. Group studies, or studies measured at the ecological level, had a higher OR=1.36 (95%CI=1.26-1.47); followed by social capital studies measured using individual analyses, OR=1.25 (95%CI=1.11-1.40); the lowest overall effect size estimate was for multilevel analyses, OR=1.20 (95%CI=1.11-1.31). These results indicate that, on average, studies that examine communities, neighborhoods, states, and nations show that a one-unit increase in social capital increases the odds of having good health by 36%. Studies that examine social capital at the individual level show that a one-unit increase in social capital increases the odds for good health by 25%. Finally, studies that examine social capital using a multilevel framework show that a one-unit increase in social capital increases the odds of good health by 20%. Sensitivity tests show that no one study in any of these sets of outcome studies significantly influences the overall effect estimate.
Country
Data were categorized according to each study's country of origin. Three categories emerged: International (n=24), Multinational (n=5), and United States (n=10). Results showed that Country was not a significant moderator (Q=1.69, df=2, p=0.430). Estimates for the overall weighted effect size for the relationship between social capital and health as moderated by country were OR=1.24 (95%CI=1.16-1.33), 1.31 (95%CI=1.12-1.50), and 1.35 (95%CI=1.22-1.50), respectively for international, multinational, and U.S. studies. The U.S. studies’ effect size estimate is larger but not statistically different than the international and multinational effect size estimates. On average, studies that examined the relationship between social capital and health in one international data found that a one-unit increase in social capital increases the odds of having good health by 24%. Studies that examined the relationship between social capital and health with data based in multiple countries found that a one-unit increase in social capital increases the odds of having good health by 31%. Studies examining the relationship between social capital and health with data based in the United States showed that with every one-unit increase in social capital the odds of having good health increased by 35%.
Constructs of Social Capital
Efficacy
Four studies and 17 effect sizes tested the effects of the social capital construct of “efficacy” and health. These studies comprise two social capital indicators: self-efficacy (e.g., measured by individuals’ level of control over their lives) and collective efficacy (e.g. measured by informal social control). Collapsing these social capital constructs into one proffered one group for comparison, for which the fixed-effects model was an appropriate test of heterogeneity. Cochran's Q-test for fixed effects showed that these effects were significantly heterogeneous (Q= 13.4, df=3, p= 0.004), whereas the overall effect size was OR=0.995 (95% CI=0.82-1.20), n.s., not significantly different than zero. These results indicated that on average, people with high levels of efficacy had odds of reporting poor health almost equal to people with lower levels of efficacy. Of the four studies that reported effects of the social capital construct efficacy, two were not significant at the p<0.05 level, one study had a p-value of 0.05, and one had a p-value of <0.05. Sensitivity analysis showed that the overall effect size estimate did not change significantly with each study removed. When Skrasbski (2004) and Rose (2000) were individually removed, the overall estimated effect size increased slightly above OR=1.00; however, this non-significant finding suggests that neither study was a significant outlier.
Participation
The overall estimated effect size for participation was calculated from 124 effect sizes that yielded 51 different indicators of participation in 26 studies. These measures of participation included whether individuals had associational memberships, belonged to organizations, attended church, or volunteered. Cochran's Q-test for fixed effects showed these effects to be significantly heterogeneous (Q= 124.2, df=25, p<0.05). The overall weighted effect size was OR=1.20 (95%CI=1.25-1.41), with a range of OR=0.309 (95%CI=0.092-1.04) to OR=3.35 (95%CI-8.10). With every one-unit increase in participation, the odds of having good health increases by 20%. Results remained significant after sensitivity tests.
Reciprocity
Five studies reported measures of reciprocity (with a total of 12 effect sizes) and five indicators were used to measure reciprocity (e.g., willingness to help others in certain situations, altruistic activity, and giving). Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 24.1, df=4, p<0.05). These results are significantly different than zero (p<0.05). The overall effect size estimate was OR=1.39 (95%CI=1.21-1.6). With every one-unit increase of engagement in reciprocal activities, the odds of having good health increased by 39%. Sensitivity tests showed that regardless of which study was removed for reciprocity studies.
Sense of Community
Six studies measured sense of community, using 19 indicators such as individuals’ perceptions of neighborhood safety, social cohesion, and friendliness of neighbors. A total of 21 effect sizes were derived. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 47.17, df=5, p<0.05). They are significantly different than zero (p= 0.001). The overall effect size estimate was OR=1.28 (95%CI=1.10-1.49). With every one-unit increase in a positive sense of community, the odds of having good health increases by 28%. Sensitivity test showed that regardless of which study was removed, these results remain significant.
Social Capital Indices
Social capital indices were captured by various composites of social capital measures such as trust, participation, collective efficacy, and reciprocity. Trust and participation were the two predominant social capital measures, included across 11 studies. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 154.28, df=10, p<0.05). They are significantly different than zero (p<0.05). The overall effect size estimate was OR=1.27 (95%CI=1.12-1.43). With every one-unit increase in a composite measure including multiple indicators of social capital, the odds of having good health increases by 27%. Sensitivity test showed that regardless of which study was removed, these results remained significant.
Social Support System
The social support system analysis was compiled by aggregating social support and social network effect sizes. Measures of social support included having someone to rely on when ill and a sense of support from family, friends, and co-workers. Social network measures included the diversity of friendship networks, having a friend of another race or ethnicity, and the frequency of individuals meeting locals in their areas. There were a total of 38 effect sizes, 22 indicators of social support systems, and 10 studies reporting social support system measures. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 139.29, df=9, p<0.05). The overall effect size estimate was OR=1.30 (95%CI=1.13-1.50). With every one-unit increase in social support, the odds of having good health increases by 30%. Regardless of which study was removed, sensitivity tests showed the range of overall estimated effect sizes regardless of which study is removed was OR=1.24-1.35.
Trust
Twenty-two studies reported measures of trust, as measured by 20 different indicators, yielding 58 effect sizes. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 447.07, df=21, p<0.05). These results were significantly different than zero (p<0.05). The overall effect size estimate for trust measures was OR=1.32 (95%CI=1.19-1.46). With every one-unit increase in trust, the odds of having good health increases by 32%. Sensitivity tests showed no significant outliers regardless of which study was removed.
Bonding
Thirty-seven studies and 249 of the 288 total effect sizes captured bonding social capital. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 718.43, df=36, p<0.05). These results are significantly different than zero (p<0.05). The overall effect size estimate for trust measures was OR=1.30 (95%CI=1.22-1.37). With every one-unit increase for those with horizontal or homogenous social capital sources, the odds of having good health increases by 30%. Sensitivity tests showed that regardless of which study was removed there were not any significant outliers.
Bridging
Eleven studies and 26 effect sizes captured bridging social capital. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 196.36, df=10, p<0.05). These results are significantly different than zero (p=0.007). The overall effect size estimate for trust measures was OR=1.18 (95%CI=1.05-1.34). With every one-unit increase in both horizontal and vertical social networks, the odds of having good health increases by 18%. Sensitivity tests showed that regardless of which study was removed, no one study was a significant outlier.
Linking
Fourteen effect sizes and 8 studies reported measures of linking social capital such as electoral and political participation, as well as trust in institutions such as government, the legal system, or other political institutions. Using the fixed-effects model, Cochran's Q-statistic showed these results to be significantly heterogeneous (Q= 84.63, df=7, p<0.05). However, these results are not significantly different than zero (p=0.14). The overall effect size estimate was OR=1.10 (95%CI=0.97-1.24). With every one-unit increase for those with high levels of linking social capital, the odds of having good health increased by 10%. Sensitivity tests showed that no one study was a significant outlier.
Discussion
This is the first meta-analysis to show the overall statistical relationship between social capital and health. There have been other systematic reviews (Islam, Merlo, Kawachi, Lindstrom, & Gerdtham, 2006; Kawachi, Kim, Couts, & Subramanian, 2004) that have compiled the social capital literature and one systematic review that combined all of the studies of social capital and health and included a graphical representation of the odds ratios of each study (Kawachi, Subramanian, & Kim, 2008).
The results of this meta-analysis suggest a modest positive relationship between social capital and health as measured by self-reported health and mortality. This meta-analysis aimed to compile the social capital literature to determine whether social capital has a positive relationship with health. The results from this meta-analysis do not provide evidence of a strong positive relationship between social capital and health. The weak association presented in this meta-analysis is a result of several factors, discussed below, that have long plagued the social capital literature. Social capital, a complex phenomenon, is a result of social relationships based upon reciprocal exchanges between residents of the same neighborhood, family and friend networks, or members of social, religious, or political organizations. Results from this metaanalysis imply that research about the relationship between health and social capital (what people do and how people feel) might be better assessed by self-reported health measures. The practice of using self-reported health to predict future health status and mortality, as many social capital studies do, may also be a function of secondary data analyses in which self-reported health appears as an available health outcome in many studies.
Another goal of this meta-analysis was to examine the relationship of each social capital construct with health. Its results show that the construct of reciprocity has the largest effect on health, followed by trust. The lowest effect size found was for efficacy. This meta-analysis cannot determine if these effect size estimates are significantly different.
The heterogeneity tests from this meta-analysis showed that certain factors do account for the previously unexplained differences among the targeted studies. Testing for moderators became a function of how best to categorize or combine the social capital literature based on both theoretical and a priori assumptions. Upon careful review of the literature, 14 categories emerged as possible moderators. However, not every social capital construct could be tested as a potential moderator because of the non-independence of effects. Thus, the ability of this metaanalysis to test the significance between social capital constructs, bonding, bridging and linking forms of social capital was limited.
Limitations
One possible explanation the overall effect size estimate between social capital and health is not larger may be a lack of social capital studies to identify mediators, confounders, and moderators. The inability of these studies to systematically discuss the possible influence of mediators, confounders, and moderators is a major limitation within the literature that reduces the capacity not only of this meta-analysis but also of future meta-analyses. This analysis was unable to adequately test for moderation stratified by race/ethnicity, gender, age, income, education, or to test each of the social capital constructs and the interaction effects among them. Social capital research as an approach to health promotion contains several limitations that can be broadly described as a lack of conceptual development in theory and measurement. Because social capital research lacks clear distinctions between social capital as an attribute of a geographic space or as an individual attribute, it also suffers from the problematic operation of variables and offers limited theoretical exploration of causal linkages (Carlson & Chamberlain, 2003). Research interests in social capital and health promotion stem from strong motivation to discover a mechanism to help explain the association of income distribution with mortality, psychosocial mechanisms, and a particular psychosocial mechanism that specifically operates at an ecologic level (Moore, Haines, Hawe, & Shiell, 2006).
One of the many limitations of this meta-analysis was to be able to distinguish differences in social capital by SES, race and gender. Social capital has become useful to explain how social relationships can increase human capital (Coleman, 1988), but in a nonspecific manner. However, a possible gradient effect rather than a threshold effect may indicate that one's social positioning along various social and economic hierarchies affects income as well as health (Marmot & Feeney, 1997). Others have suggested that income inequality can lead to increased mortality by causing individuals to disinvest in social capital (Kawachi, et al., 1997). Baum and Ziersch (2003), who refer to the “darker side” as social “exclusion/inclusion and equity” argue that these problems are relevant because they link the social elements of exclusion to material deprivation and poverty and emphasize the processes of marginalization, providing further evidence that individuals’ and communities’ access to elements of social capital can vary according to characteristics such as race, gender, and socioeconomic status.
Future Research
At best, social capital may be an essential but not a sufficient ingredient for health improvement (Lochner, Kawachi, Brennan, & Buka, 2003). This conclusion is drawn from both the extensive limitations of and opportunities for social capital development in the field of public health. This conclusion is drawn from both the extensive limitations of and opportunities for social capital development in the field of public health. To determine if social capital is necessary and sufficient, researchers and practitioners will need to understand how to encourage the development of social ties and to strengthen existing social ties through increased participation in various contexts that can ultimately improve health behaviors and health outcomes.
References
- Blakely T, Atkinson J, Ivory V, Collings S, Wilton J, Howden-Chapman P. No association of neighbourhood volunteerism with mortality in New Zealand: A national multilevel cohort study. International Journal of Epidemiology. 2006;35(4):981–989. doi: 10.1093/ije/dyl088. [DOI] [PubMed] [Google Scholar]
- Blakely TA, Kennedy BP, Kawachi I. Socioeconomic Inequality in Voting Participation and Self-Rated Health American Journal of Public Health. 2001;91(1):99–104. doi: 10.2105/ajph.91.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolin K, Lindgren B, Lindstrom M, Nystedt P. Investments in social capital-implications of social interactions for the production of health. Social Science & Medicine. 2003;56:2379–2390. doi: 10.1016/s0277-9536(02)00242-3. [DOI] [PubMed] [Google Scholar]
- Boneham MA, Sixsmith JA. The voices of older women in a disadvantaged community: Issues of health and social capital. Social Science & Medicine. 2006;62:269–279. doi: 10.1016/j.socscimed.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson JG, editor. Handbook of Theory and Research for the Sociology of Education. New York: Greenwood Press; 1985. [Google Scholar]
- Carlson ED, Chamberlain RM. Social Capital, Health, and Health Disparities. Journal of Nursing Scholarship. 2003;35(4):325–331. doi: 10.1111/j.1547-5069.2003.00325.x. [DOI] [PubMed] [Google Scholar]
- Carlson P. The European health divide: A matter of financial or social capital? Social Science and Medicine. 2004;59(9):1985–1992. doi: 10.1016/j.socscimed.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Carpiano RM. Actual or Potential Neighborhood Resources for Health: What Can Bourdieu Offer for Understanding Mechanisms Linking Social Capital to Health? In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York: Springer; 2008. [Google Scholar]
- Cattel V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Social Science & Medicine. 2001;52:1501–1516. doi: 10.1016/s0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- Coleman J. Social capital in the creation of human capital. American Journal of Sociology. 1988;94(Supplement):S95–S121. [Google Scholar]
- Cullen M, Whiteford H. The Interrelations of Social Capital with Health and Mental Health. 2001 Retrieved September 15, 2008. from http://www.health.gov.au/internet/main/publishing.nsf/Content/mental-pubs-i-intsoc.
- Greiner KA, Li C, Kawachi I, Hunt DC, Ahluwalia JS. The relationships of social participation and community ratings to health and health behaviors in areas with high and low population density. Social Science & Medicine. 2004;59:2303–2312. doi: 10.1016/j.socscimed.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Halpern D. Social Capital. Cambridge: Polity Press; 2005. [Google Scholar]
- Harpham T. he Measurement of Community Social Capital Through Surveys. In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York: Springer; 2008. [Google Scholar]
- Harpham T, Grant E, Thomas E. Measuring social capital within health surveys: key issues. Health Policy and Planning. 2002;17(1):106–111. doi: 10.1093/heapol/17.1.106. [DOI] [PubMed] [Google Scholar]
- Hyyppa MT, Maki J. Individual-Level Relationships between Social Capital and Self-Rated Health in a Bilingual Community. Preventive Medicine. 2001;32:148–155. doi: 10.1006/pmed.2000.0782. [DOI] [PubMed] [Google Scholar]
- Hyyppa MT, Maki J. Social participation and health in a community rich in stock of social capital. Health Education Research. 2003;18(6):770–779. doi: 10.1093/her/cyf044. [DOI] [PubMed] [Google Scholar]
- Hyppa MT, Maki J, Impivaara O, Aromaa A. Individual-level measures of social capital as predictors of all-cause mortality and cardiovascular mortality: a population based prospective study of men and women in Finland. European Journal of Epidemiology. 2007;22(9):589–597. doi: 10.1007/s10654-007-9153-y. [DOI] [PubMed] [Google Scholar]
- Islam MK, Merlo J, Kawachi I, Lindstrom M, Gerdtham UG. Social capital and health: Does egalitarianism matter? A literature review. International Journal for Equity in Health. 2006;5(3):1–28. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Social Capital and Community Effects on Population and Individual Health. Annals of New York Academy of Sciences. 1999:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Kennedy B, Glass R. Social Capital and Self-Rated Health: A Contextual Analysis. American Journal of Public Health. 1999;89(8):1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP. The health of nations. New York: The New York Press; 2002. [Google Scholar]
- Kawachi I, Kennedy BP, Lochner KA, Prothrow-Stith D. Social capital, income inequality and mortality. American Journal of Public Health. 1997;87:1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kim D, Couts A, Subramanian SV. Commentary: Reconciling the three accounts of social capital. International Journal of Epidemiology. 2004;33(4):682–690. doi: 10.1093/ije/dyh177. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Subramanian SV, Kim D. Social Capital and Health: A Decade of Progress and Beyond. In: Kawachi I, Subramanian SV, Kim D, editors. Social Capital and Health. New York: Springer; 2008. [Google Scholar]
- Kim D, Kawachi I. A Multilevel Analysis of Key Forms of Community-and Individual Level Social Capital as Predictors of Self-Rated Health in the United States. Journal of Urban Health. 2006;83(5):813–826. doi: 10.1007/s11524-006-9082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Kawachi I. U.S. State-Level Social Capital and Health-Related Quality of Life: Multilevel Evidence of Main, Mediating, and Modifying Effects. Annals of Epidemiology. 2007;17:258–269. doi: 10.1016/j.annepidem.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Kennedy BP, Kawachi I, Prothrow-Stith D, Lochner KA, Gupta V. Social capital, income inequality and firearm violent crime. Social Science & Medicine. 1998;47:7–17. doi: 10.1016/s0277-9536(98)00097-5. [DOI] [PubMed] [Google Scholar]
- Lindstrom M. Social Capital and lack of the belief in the possibility to influence one's own health: A population-based study. Scandinavian Journal of Public Health. 2006;34:69–75. doi: 10.1080/14034940510032167. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Isacsson SO, Elmstahl S. Impact of different aspects of social participation and social capital on smoking cessation among daily smokers: a longitudinal study. Tobacco Control. 2003;12:274–281. doi: 10.1136/tc.12.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom M, Moghaddassi M, Bolin K, Lindgren B, Merlo J. Social participation, social capital and daily tobacco smoking: a population-based multilevel analysis in Malmo, Sweden. Scandinavian Journal of Public Health. 2003;31:444–450. doi: 10.1080/14034940310006203. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Moghaddassi M, Merlo J. Social capital and leisure time physical activity: a population based multilevel analysis in Malmo, Sweden. Journal of Epidemiology and Community Health. 2003;57:23–28. doi: 10.1136/jech.57.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom M, Moghaddassi M, Merlo J. Individual self-reported health, social participation and neighborhood: a multilevel analysis in Malmo, Sweden. Preventive Medicine. 2004;39:135–141. doi: 10.1016/j.ypmed.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Sundquist K, Ostergren PO. Ethnic differences in self-reported health in Malmo in southern Sweden. Journal of Epidemiology and Community Health. 2001;55:97–103. doi: 10.1136/jech.55.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner KA, Kawachi I, Brennan RT, Buka SL. Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine. 2003;56:1797–1805. doi: 10.1016/s0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- Marmot M, Feeney A. General explanations for social inequalities in health. IARC Scientific Publications. 1997;138:207–228. [PubMed] [Google Scholar]
- Mellor JM, Milyo J. State Social Capital and Individual Health Status. Journal of Health Politics, Policy and Law. 2005;30(6):1101–1130. doi: 10.1215/03616878-30-6-1101. [DOI] [PubMed] [Google Scholar]
- Mohan G, Mohan J. Placing social capital. Progress in Human Geography. 2002;26(2):191–210. [Google Scholar]
- Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated: The role of access to health care in a population-based study. Social Science & Medicine. 2006 doi: 10.1016/j.socscimed.2006.11.023. [DOI] [PubMed] [Google Scholar]
- Moore S, Haines V, Hawe P, Shiell A. Lost in translation: a genealogy of the “social capital” concept in public health. Journal of Epidemiology and Community Health. 2006;60:729–734. doi: 10.1136/jech.2005.041848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntaner C, Lynch JW, Hillemeier M, Lee JH, David R, Benach J, et al. Economic inequality, working-class power, social capital, and case-specific mortaility in wealthy countries. International Journal of Health Services. 2002;32(4):629–656. doi: 10.2190/N7A9-5X58-0DYT-C6AY. [DOI] [PubMed] [Google Scholar]
- Pollack CE, Knesebeck Ovd. Socail capital and health among the aged: comparisons between the United States and Germany. Health & Place. 2004;10:383–391. doi: 10.1016/j.healthplace.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Do health behaviors mediate the association between social capital and health? Preventive Medicine. 2006:1–6. doi: 10.1016/j.ypmed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Social capital: An individual or collective resource for health? Social Science & Medicine. 2006;62:292–302. doi: 10.1016/j.socscimed.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Social relations or social capital? Individual and community health effects of bonding social capital. Social Science & Medicine. 2006;63:255–270. doi: 10.1016/j.socscimed.2005.11.039. [DOI] [PubMed] [Google Scholar]
- Rose R. How much does social capital add to individual health? A survey study of Russians. Social Science & Medicine. 2000;51:1421–1435. doi: 10.1016/s0277-9536(00)00106-4. [DOI] [PubMed] [Google Scholar]
- Skrabski A, Kopp M, Kawachi I. Social capital and collective efficacy in Hungary: cross-sectional associations with middle aged female and male mortality rates. Journal of Community Health. 2004;58:340–345. doi: 10.1136/jech.2003.010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Kim DJ, Kawachi I. Social Trust and Self-Rated Health in US Communities: A Multilevel Analysis. Journal of Urban Health. 2002;79(4, Supplement 1):S21–S34. doi: 10.1093/jurban/79.suppl_1.S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Lochner KA, Kawachi I. Neighborhood differences in social capital: A compositional artifact or a contextual construct. Health and Place. 2003;9(1):33–44. doi: 10.1016/s1353-8292(02)00028-x. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Johansson SE, Yang M, Sundquist K. Low linking social capital as a predictor of coronary heart disease in Sweden: A cohort study of 2.8 million people. Social Science & Medicine. 2006;62:954–963. doi: 10.1016/j.socscimed.2005.06.049. [DOI] [PubMed] [Google Scholar]
- Szreter S, Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. International Journal of Epidemiology. 2004;33:650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Turrell G, Kavanagh A, Subramanian SV. Area variation in mortality in Tasmania (Australia): The contributions of socioeconomic disadvantage, social capital and geographic remoteness. Health and Place. 2006;12(3):291–305. doi: 10.1016/j.healthplace.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Veenstra G. Social capital, SES and health: An individual-level analysis. Social Science & Medicine. 2000;50:619–629. doi: 10.1016/s0277-9536(99)00307-x. [DOI] [PubMed] [Google Scholar]
- Veenstra G. Socail capital and health (plus wealth, income, income inequality and regional health governance) Social Science & Medicine. 2002;54:849–868. doi: 10.1016/s0277-9536(01)00049-1. [DOI] [PubMed] [Google Scholar]
- Veenstra G. Location, location, location: contextual and compositional health effects of social capital in British Columbia, Canada. Social Science & Medicine. 2005;60:2059–2071. doi: 10.1016/j.socscimed.2004.08.064. [DOI] [PubMed] [Google Scholar]
- Wakefield SEL, Poland B. Family, friend or foe? Critical Reflections on the relevance and role of social capital in health promotion and community development. Social Science & Medicine. 2005;60:2819–2832. doi: 10.1016/j.socscimed.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Woolcock M, Narayan D. Social Capital: Implications for Development Theory, Research and Policy. The World Bank Observer. 2000;15(2):225–249. [Google Scholar]


