Abstract
Objective
To examine associations between perceived weight discrimination and changes in weight, waist circumference, and weight status.
Methods
Data were from 2944 men and women aged ≥50 years participating in the English Longitudinal Study of Ageing. Experiences of weight discrimination were reported in 2010-2011 and weight and waist circumference were objectively measured in 2008-2009 and 2012-2013. ANCOVAs were used to test associations between perceived weight discrimination and changes in weight and waist circumference. Logistic regression was used to test associations with changes in weight status. All analyses adjusted for baseline BMI, age, sex, and wealth.
Results
Perceived weight discrimination was associated with relative increases in weight (+1.66 kg, P < 0.001) and waist circumference (+1.12 cm, P = 0.046). There was also a significant association with odds of becoming obese over the follow-up period (OR = 6.67, 95% CI 1.85-24.04) but odds of remaining obese did not differ according to experiences of weight discrimination (OR = 1.09, 95% CI 0.46-2.59).
Conclusions
Our results indicate that rather than encouraging people to lose weight, weight discrimination promotes weight gain and the onset of obesity. Implementing effective interventions to combat weight stigma and discrimination at the population level could reduce the burden of obesity.
Introduction
Negative attitudes towards obese individuals remain one of the “last socially acceptable forms of prejudice” 1 and many obese individuals experience weight-related discrimination in their everyday lives 2. There is a common perception that weight discrimination might encourage overweight individuals to lose weight 3, but a growing literature suggests it might actually have the opposite effect. Studies show that people who experience weight stigma are more likely to report engaging in obesity-promoting behaviors, including problematic eating 4,5, refusal to diet 6, and avoidance of physical activity 7, and these effects are independent of BMI. However, there is limited evidence on associations with actual changes in body weight. The present study therefore examined relationships between perceived weight discrimination and changes in weight, waist circumference, and weight status over four years in a large population-based sample.
Methods
Study population
Data were from the English Longitudinal Study of Ageing (ELSA), a longitudinal panel study of adults aged ≥50 y 8. The first ELSA data were collected in 2001-2002 and participants have been followed up every two years, with a nurse visit every four years to take objective measurements of anthropometry. Wave 5 (2010-2011) is the only assessment that included questions on discrimination. Among the 9090 participants who were interviewed in wave 5, 8107 (93% of those eligible) answered the self-completion questionnaire that assessed discrimination. For our analyses, we use these data plus anthropometric data collected in waves 4 (2008-2009) and 6 (2012-2013), as no anthropometric data were collected in wave 5. Complete data were available for 2944 participants.
Measures
Questions on perceived discrimination were based on items developed and used widely in other longitudinal studies, notably MIDUS and the Health and Retirement Study 2,9,10. Participants were asked how often they encounter five discriminatory situations: “In your day-to-day life, how often have any of the following things happened to you: (1) you are treated with less respect or courtesy; (2) you receive poorer service than other people in restaurants and stores; (3) people act as if they think you are not clever; (4) you are threatened or harassed; and (5) you receive poorer service or treatment than other people from doctors or hospitals. Responses ranged from “never” to “almost every day”. Because data were highly skewed, with most participants reporting never experiencing discrimination, we dichotomized responses to indicate whether or not respondents had ever experienced discrimination in any domain (never vs. all other options). Participants who reported discrimination in any of the situations were asked to indicate the reason(s) they attributed their experience to from a list of options including weight, age, gender, and race. We considered participants who attributed experiences of discrimination to their weight as cases of perceived weight discrimination.
Weight, height, and waist circumference were objectively measured. Weight status was classified as normal-weight (BMI <25), overweight (25-29.9), obese class I (30-34.9), obese class II (35-39.9), and obese class III (≥40). Analyses use data on change in weight, waist circumference, and obesity between waves 4 and 6.
Age, sex, and household nonpension wealth [a sensitive indicator of socioeconomic status (SES) in this age group] were included as control variables.
Statistical analysis
Baseline demographic and anthropometric characteristics of participants who reported weight discrimination and those who did not were compared using t-tests (continuous variables) and χ2 tests (categorical variables). One-way analyses of covariance (ANCOVAs) were used to examine whether perceived weight discrimination was associated with changes in weight and waist circumference; and logistic regression was used to examine associations between weight discrimination and becoming and remaining obese. All analyses adjusted for confounding by age, sex, and wealth.
Results
Perceived weight discrimination was reported by 5.1% of participants, ranging from 0.7% in normal-weight to 35.9% in class III obese. Participants who had experienced weight discrimination were significantly younger (61.6 vs. 66.4 y, P < 0.001), less wealthy (P < 0.001), and more overweight (BMI 35.5 vs. 27.2, P < 0.001) than those who had not, but the groups did not differ significantly by sex (P = 0.090) (Table1).
Table 1.
Baseline (wave 4) demographic anthropometric characteristics of individuals who did and did not report weight discrimination (at wave 5) in the English Longitudinal Study of Ageing—mean ± SD or % (n)
| Weight discrimination (n = 150) | No weight discrimination (n = 2794) | P | |
|---|---|---|---|
| Age (years) | 61.58 ± 6.75 | 66.36 ± 8.59 | <0.001 |
| Sex | |||
| Male | 4.3% (52) | 95.7% (1164) | 0.090 |
| Female | 5.7% (98) | 94.3% (1630) | - |
| Wealth (quintile) | |||
| 1 (lowest) | 9.0% (41) | 91.0% (415) | <0.001 |
| 2 | 7.1% (41) | 92.9% (534) | - |
| 3 | 5.0% (27) | 95.0% (516) | - |
| 4 | 3.4% (23) | 96.6% (645) | - |
| 5 (highest) | 2.6% (18) | 97.4% (684) | - |
| Height (cm) | 165.23 ± 9.32 | 165.93 ± 9.29 | 0.370 |
| Weight (kg) | 96.80 ± 17.36 | 74.94 ± 15.09 | <0.001 |
| BMI (kg/m2) | 35.46 ± 5.84 | 27.17 ± 4.84 | <0.001 |
| Waist circumference (cm) | 111.87 ± 13.42 | 93.86 ± 13.21 | <0.001 |
| Weight status | |||
| Normal-weight | 0.7% (7) | 99.3% (1048) | <0.001 |
| Overweight | 1.4% (15) | 98.6% (1054) | - |
| Obese | 15.6% (128) | 84.4% (692) | - |
| Class I | 8.6% (47) | 91.4% (501) | - |
| Class II | 27.3% (53) | 72.7% (141) | - |
| Class III | 35.9% (28) | 64.1% (50) | - |
BMI, body mass index; SD, standard deviation.
Wealth quintiles were calculated using the whole ELSA sample.
There were significant associations between perceived weight discrimination and weight change over four years (Table2). There was a 1.66 kg difference in mean weight change between individuals who reported experiences of weight discrimination (+0.95 kg) and those who did not (−0.71 kg, P < 0.001). There was a trend towards greater weight gain (or less weight loss) across all BMI groups (Figure 1). There was also a 1.12 cm difference in waist circumference change, increasing in individuals who experienced weight discrimination (+0.72 cm) and decreasing in those who did not (−0.40 cm, P = 0.046), although this association was not consistently observed across BMI groups (Table2). The interaction between weight discrimination and weight status was not significant for change in weight (P = 0.271) or waist (P = 0.283).
Table 2.
Associations between perceived weight discrimination and changes in weight and waist circumference, overall and by weight status—mean ± SE
| Weight discrimination | No weight discrimination | Mean difference | P | |
|---|---|---|---|---|
| Weight change (kg) | ||||
| Overall | 0.95 ± 0.41 | −0.71 ± 0.09 | 1.66 ± 0.42 | <0.001 |
| Normal-weight | 0.46 ± 1.28 | 0.01 ± 0.10 | 0.45 ± 1.28 | 0.727 |
| Overweight | 2.22 ± 1.13 | −0.39 ± 0.13 | 2.62 ± 1.14 | 0.022 |
| Obese | −0.26 ± 0.59 | −2.07 ± 0.24 | 1.81 ± 0.65 | 0.006 |
| Class I | −0.44 ± 0.82 | −1.52 ± 0.25 | 1.07 ± 0.86 | 0.213 |
| Class II | −0.76 ± 0.98 | −2.12 ± 0.59 | 1.36 ± 1.16 | 0.243 |
| Class III | −1.54 ± 1.90 | −6.00 ± 1.40 | 4.46 ± 2.41 | 0.068 |
| Waist change (cm) | ||||
| Overall | 0.72 ± 0.54 | −0.40 ± 0.12 | 1.12 ± 0.59 | 0.046 |
| Normal-weight | 0.96 ± 0.50 | 0.39 ± 0.03 | 0.58 ± 0.50 | 0.250 |
| Overweight | 1.52 ± 0.46 | 0.75 ± 0.04 | 0.77 ± 0.46 | 0.099 |
| Obese | 0.95 ± 0.16 | 1.00 ± 0.06 | −0.05 ± 0.18 | 0.780 |
| Class I | 0.98 ± 0.24 | 0.91 ± 0.07 | 0.07 ± 0.25 | 0.778 |
| Class II | 1.02 ± 0.29 | 1.15 ± 0.15 | −1.27 ± 0.33 | 0.703 |
| Class III | 1.01 ± 0.39 | 1.37 ± 0.26 | −0.36 ± 0.47 | 0.452 |
SE, standard error.
Values are adjusted for baseline BMI, age, sex, and wealth.
Figure 1.
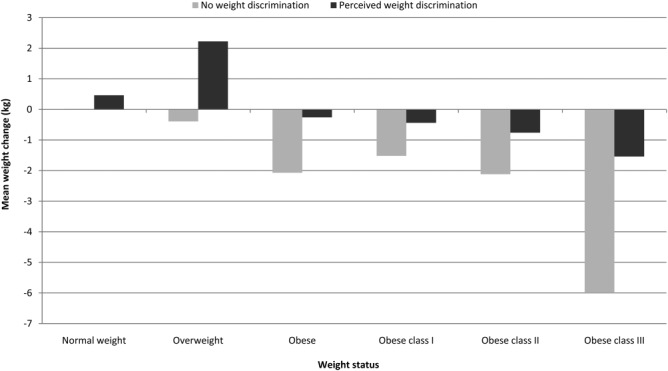
Associations between perceived weight discrimination and weight change, by baseline weight status.
Among participants who were not obese at baseline, perceived weight discrimination was associated with higher odds of becoming obese (25.2 vs. 4.4%; OR = 6.67, 95% CI 1.85-24.04, P = 0.004). However, the odds of remaining obese did not differ according to experiences of weight discrimination (OR = 1.09, 95% CI 0.46-2.59, P = 0.853), with most obese participants staying obese at follow-up (85.6 vs. 85.0%).
Discussion
This study is the first to examine the relationship between weight discrimination and weight change in a population-based sample. Weight discrimination was reported by 5.1% of participants, in line with previous prevalence estimates in this age group 2. Consistent with evidence that people who experience weight discrimination are more likely to engage in behaviors that promote weight gain (4-7), perceived weight discrimination was associated with relative increases in weight and waist circumference over time. We also found that weight discrimination was related to the onset of obesity, which has been shown previously 9, although there was no association between weight discrimination and remaining obese.
There are a number of potential mechanisms that may lead from weight discrimination to weight gain. Exposure to weight stigma is associated with psychological distress 3. Food activates dopaminergic reward pathways in the brain 11 and may provide short-term relief from the adverse psychological effects of discrimination. Many overweight/obese individuals who experience stigmatization report eating as a coping strategy 6. Stress responses to discriminatory experiences may also drive unhealthy eating behavior via activation of the hypothalamic–pituitary–adrenal axis and resultant release of cortisol and endogenous opioids 12. Experimental studies show that elevated cortisol levels and a higher cortisol response to stressors predict increased food intake, particularly of energy-dense foods 13,14, while opioids promote consumption of palatable foods 15. Weight discrimination may also influence weight change through effects on energy expenditure, with evidence indicating that people who experience stigmatization perceive themselves as less competent in physical activity and tend to avoid it 7,16.
Weight discrimination has been justified on the grounds that it encourages obese individuals to lose weight 3, but our results provide no support for this notion and rather suggest that discrimination exacerbates weight gain and promotes onset of obesity. Removing prejudice and blame from weight loss advice might be a better route to promoting weight control. Widespread weight bias has been documented in health professionals 1, including those who specialize in obesity 17. Negative attitudes are picked up on by obese patients, who often feel that doctors do not understand how difficult it is to be overweight 18, and report being treated disrespectfully by the medical profession because of their weight 19, which may hinder weight loss success. Providing support to those affected by weight discrimination and teaching adaptive coping strategies could also improve weight outcomes. One study demonstrated positive effects of a brief acceptance-based intervention in obese weight loss programme participants, with those randomized to the intervention losing more weight than controls over a three-month follow-up 20.
This study had several limitations. Weight was not measured in the same wave as discrimination was assessed, so baseline values were from two years earlier. We cannot be sure whether discrimination preceded weight gain or vice versa. It is therefore not possible to establish causal relationships; i.e. whether people gain weight as a consequence of experiencing weight discrimination, or whether gaining weight makes people more likely to experience weight discrimination or attribute experiences of discrimination to their weight. Participants were from an older population, in which weight change and experiences of weight discrimination may differ relative to younger populations so findings cannot be assumed to generalize. The sample was also predominantly white (97.9%), with just five non-white respondents reporting weight discrimination, so results may not apply to other ethnic groups that have different body weight ideals that make them less likely to perceive, or less affected by, discrimination. Our analyses were restricted to ELSA participants who had complete data. The analyzed sample was slightly younger, wealthier, and less overweight than the total ELSA sample (although the level of perceived weight discrimination did not differ), so results may not be population-representative.
The results of this study provide evidence that weight discrimination is associated with significant increases in body weight and waist circumference over time. Our findings underscore the need for effective interventions at the population level to combat weight stigma and discrimination.
References
- Puhl RM, Brownell KD. Bias, discrimination, and obesity. Obesity. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995-1996 through 2004-2006. Obesity. 2008;16:1129–1134. doi: 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. Obesity stigma: Important considerations for public health. Am J Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight-based stigmatization in a weight loss surgery population: Psychological and behavioral correlates. Obes Silver Spring Md. 2008;16(Suppl 2):S69–74. doi: 10.1038/oby.2008.457. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, Hayashi K. Perceived discrimination is associated with binge eating in a community sample of non-overweight, overweight, and obese adults. Obes Facts. 2012;5:869–880. doi: 10.1159/000345931. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Brownell KD. Confronting and coping with weight stigma: An investigation of overweight and obese adults. Obes Silver Spring Md. 2006;14:1802–1815. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior: A preliminary investigation among college-aged females. J Health Psychol. 2008;13:131–138. doi: 10.1177/1359105307084318. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: The English Longitudinal Study of Ageing. Int J Epidemiol. 2013;42:1640–1648. doi: 10.1093/ije/dys168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A. Perceived weight discrimination and obesity. PLoS ONE. 2013;8:e70048. doi: 10.1371/journal.pone.0070048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46:244–259. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- Vucetic Z, Reyes TM. Central dopaminergic circuitry controlling food intake and reward: Implications for the regulation of obesity. Wiley Interdiscip Rev Syst Biol Med. 2010;2:577–593. doi: 10.1002/wsbm.77. [DOI] [PubMed] [Google Scholar]
- Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Tataranni PA, Larson DE, Snitker S, et al. Effects of glucocorticoids on energy metabolism and food intake in humans. Am J Physiol-Endocrinol Metab. 1996;34:E317. doi: 10.1152/ajpendo.1996.271.2.E317. [DOI] [PubMed] [Google Scholar]
- Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- Nogueiras R, Romero-Picó A, Vazquez MJ, Novelle MG, López M, Diéguez C. The opioid system and food intake: Homeostatic and hedonic mechanisms. Obes Facts. 2012;5:196–207. doi: 10.1159/000338163. [DOI] [PubMed] [Google Scholar]
- Schmalz DL. “I Feel Fat”: Weight-related stigma, body esteem, and BMI as predictors of perceived competence in physical activity. Obes Facts. 2010;3:15–21. doi: 10.1159/000273210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Anderson DA, Foster GD, Bennett A, Steinberg C, Sarwer DB. Obese women's perceptions of their physicians' weight management attitudes and practices. Arch Fam Med. 2000;9:854–860. doi: 10.1001/archfami.9.9.854. [DOI] [PubMed] [Google Scholar]
- Rand CS, Macgregor AM. Successful weight loss following obesity surgery and the perceived liability of morbid obesity. Int J Obes. 1991;15:577–579. [PubMed] [Google Scholar]
- Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med Publ Soc Behav Med. 2009;37:58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]


