Abstract
Objective
Examine the impact of non-physician health professional body mass index (BMI) on obesity care, self-efficacy, and perceptions of patient trust in weight loss advice.
Design and Methods
We analyzed a national cross-sectional internet<based survey of 500 U.S. non-physician health professionals specializing in nutrition, nursing, behavioral/mental health, exercise, and pharmacy collected between January 20 and February 5, 2014.
Results
Normal BMI professionals were more likely than overweight/obese professionals to report success in helping patients achieve clinically significant weight loss (52% vs. 29%, p=0.01). We observed no differences by health professional BMI about the appropriate patient body weight for weight-related care (initiate weight loss discussions and success in helping patients lose weight), confidence in ability to help patients lose weight, or in perceived patient trust in their advice. Most health professionals (71%) do not feel successful in helping patients lose weight until they are morbidly obese, regardless of BMI.
Conclusions
Normal BMI non-physician health professionals report being more successful than overweight and obese health professionals at helping obese patients lose weight. More research is needed to understand how to improve self-efficiency for delivering obesity care, particularly among overweight and class I obese patients.
Keywords: health professional BMI, obesity care
Introduction
Healthcare for obesity, which affects one third of the U.S. adult population (1) and is estimated to cost $147 billion annually (2), is suboptimal with only about one third of patients receiving a diagnosis and a fifth receiving weight-related counseling (3, 4). Physician body mass index (BMI) has recently been identified as a potential barrier to obesity care (5, 6). Normal weight physicians are more likely than overweight and obese physicians to provide recommended obesity care to their patients and feel confident doing so (5, 6). The body weight of non-physician health professionals may similarly impact weight management practices and self-efficacy. However, we are unaware of any studies that have examined this question.
The objective of this study was to examine differences in self-reported obesity care practices, self-efficacy, and perceived patient trust in weight-related advice by non-physician health professional BMI. We hypothesized that normal BMI non-physician health professionals would be more likely than overweight/obese professionals to report providing obesity care, to feel confident doing so, and to perceive their advice as trustworthy to patients.
Methods and Procedures
Study Design and Administration
Detail about the survey development can be found in the Appendix A. We conducted a national cross<sectional internet-based survey in the U.S. among five non-physician health professional groups: nutrition, nursing, behavioral/mental health, exercise, and pharmacy. Data collection was conducted online between January 20 and February 5, 2014. One hundred respondents from each of five professions were recruited. In order to qualify for the study, respondents needed to: (1) confirm their profession and (2) indicate that they work at their profession at least 15 hours a week in an ambulatory setting. Participants were recruited from the Medical Market Research (MMR) Panel which consists of 200,000 non-physician health professionals.
Measures
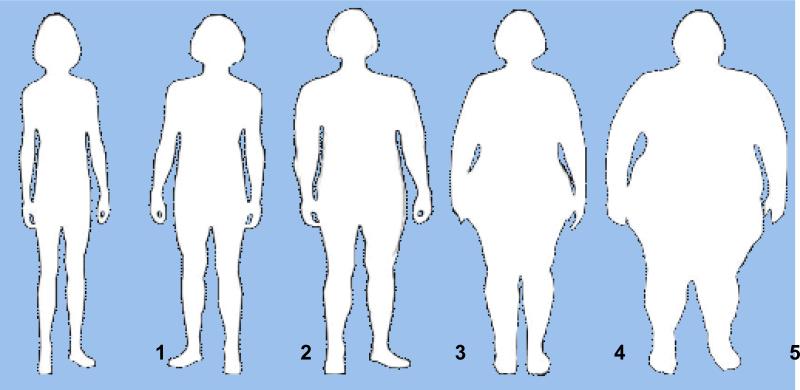
The question wording and response categories for the outcome variables can be found in Appendix B. The primary outcome was professionals’ perception of the appropriate body weight to initiate weight loss discussions and self-efficacy for helping patients achieve clinically significant weight loss (at least 5% of body weight). Like past studies (5), the survey displayed pictures of five different body sizes that ranged from normal BMI to class III obese, and respondents were asked to select the patient size at which they typically initiate obesity care. We elected to use pictures rather than provide BMI categories so as not to bias responses. Our secondary outcomes assessed self-efficacy for helping patients achieve clinically significant weight loss and perceived patient trust in health professionals’ advice. Trust was based on two survey questions: 1) “Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from overweight/obese health care professionals?” and 2) “Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from health care professionals who have a healthy weight?”
The primary independent variable of interest was non-physician health professional BMI. Health professionals were considered to be overweight or obese if their self-reported BMI was ≥25 kg/m2 and normal if their self-reported BMI was <25 kg/m2.
Statistical Analyses
The final data were weighted to address concerns with systematic under-or over-representation of health professional subpopulations in the panel, and to account for systematic nonresponse along known demographic parameters of these professions. The final weighted sample approximates the known distribution for these occupations in the American Community Survey (7).
Statistical analyses were performed using the STATA, version 13.0 software package (StataCorp LP, College Station, TX), using SVY functions to adjust for the complex survey design. The weighted margin of error for the survey was +/−5.3%. We conducted multivariate logistic regression analyses to evaluate the relationship between non-physician health professional BMI and the outcome variables. All models were adjusted for health professional age, gender, education, specialty (nutrition, nursing, behavioral/mental health, exercise, and pharmacy), and weight loss intention (assessed by a Yes or No answer to the survey question – “At this time, are you seriously trying to lose weight?”).
Results
We screened 1052 panel members who responded to the survey invitation, and excluded 290 screened as ineligible and 45 qualifying respondents who did not complete the questionnaire. The completion rate, calculated as completed interviews over the total of estimated working qualifying emails was 70%. The final sample included 500 non-physician health professionals; 100 in each professional group.
Table 1 reports the characteristics of the study sample. We observed significant differences in health professional body weight by gender, age and weight loss efforts. In addition, nutrition professionals were more likely to be normal BMI. Table 2 shows non-physician health professional responses on the appropriate patient body weight to initiate a discussion about weight loss, by health professional BMI. We observed no significant relationships between professional BMI and each of the three outcomes. Table 3 shows non-physician health professional weight management self-efficacy and perceived patient trust in advice by professional BMI. Normal BMI professionals were more likely than overweight/obese health professionals to report success in helping obese patient achieve clinically significant weight loss 52% vs. 29%, p = 0.01). We observed no differences in non-physician health professional perceptions of their confidence to help obese patients lose weight or patient trust in weight loss advice by professional BMI.
Table 1.
Characteristics of the study sample
| Normal BMI (%) | Overweight/obese (%) | P-value* | |
|---|---|---|---|
| Non-physician health professional groups | |||
| Nursing | 45 | 55 | 0.34 |
| Nutrition | 75 | 25 | <0.01 |
| Behavioral/mental health | 51 | 49 | 0.84 |
| Exercise | 46 | 54 | 0.46 |
| Pharmacy | 46 | 54 | 0.53 |
| Non-physician health professional characteristics | |||
| Female | 93 | 79 | <0.01 |
| White | 85 | 76 | 0.20 |
| Age 45 and older | 40 | 57 | 0.04 |
| Mean BMI | 22 | 29 | <0.01 |
| Seriously trying to lose weight at this time | 16 | 74 | <0.01 |
| More than college education | 49 | 57 | 0.40 |
| Completed training >20 years ago | 32 | 33 | 0.84 |
| Received high quality weight management training during degree program | 52 | 51 | 0.87 |
| Non-physician health professional-reported demographics of their patients | |||
| Almost all patients in practice are obese | 15 | 16 | 0.88 |
| Most obese patients in practice are from a broad range of demographic groups | 66 | 69 | 0.69 |
| Most obese patients in practice are low income | 49 | 39 | 0.23 |
Source: Survey of health professionals between January 20 and February 5, 2014. Health professionals included nurses, nutritionists, behavioral or mental health providers, exercise, and pharmacists.
Note: Numbers may not add up to 100% because of rounding.
Comparing characteristics between normal BMI and overweight/obese groups.
Table 2.
Health professional perceptions about the appropriate patient body weight for weight-related care by health professional BMI category (%)

| |||||
|---|---|---|---|---|---|
| Normal | OVWT† | Class I | Class II | Class III | |
| At what BMI do you... | |||||
| Start talking to your patients about weight lossa | |||||
| Normal BMI professionals | <1 | 2 | 58 | 33 | 6 |
| Overweight/obese professionals | 0 | 4 | 66 | 27 | 4 |
| Feel less successful in helping patients lose weightb | |||||
| Normal BMI professionals | 4 | 12 | 14 | 17 | 56 |
| Overweight/obese professionals | 10 | 6 | 16 | 20 | 48 |
Notes: Adjusted for age, education, weight loss intention, gender and type of health professional (nutrition, nursing, behavioral/mental health, exercise, pharmacy)
OVWT = Overweight
Survey question: At what BMI do you typically start talking to your patients or clients about weight loss?
Survey question: At what BMI do you feel that you are less likely to successfully aid patients or clients with weight loss?
1 significantly different from professionals with normal BMI, p < 0.05
2 significantly different from professionals with normal BMI, p < 0.10
Table 3.
Health professionals' self-efficacy for providing weight management and perceived patient trust in their advice, overall and by health professional BMI (%)
| Normal BMI | Overweight/Obese | P-value | |
|---|---|---|---|
| High confidence in ability to help patients with obesity achieve clinically significant weight lossa | 67 | 55 | 0.26 |
| High success in helping patients with obesity achieve clinically significant weight lossb | 52 | 29† | 0.01 |
| Perceived likelihood that patients will trust weight loss advice from an overweight/obese health professionalc | |||
| Less likely | 82 | 72 | 0.31 |
| More likely | 7 | 13 | 0.43 |
| As likely | 11 | 15 | 0.60 |
| Perceived likelihood that patients will trust weight loss advice from a normal weight health professionald | |||
| Less likely | 11 | 46 | 0.39 |
| More likely | 73 | 71 | 0.83 |
| As likely | 18 | 26 | 0.38 |
Notes: Adjusted for age, education, weight loss intention, gender and type of health professional (nutrition, nursing, behavioral/mental health, exercise, pharmacy)
significantly different from normal BMI group, p < 0.05
significantly different from normal BMI group, p < 0.10
Survey question: How confident are you in your ability to help your obese patients or clients achieve a clinically significant weight loss (at least 5% of body weight)?
How successful are you at helping your obese patients or clients achieve a clinically significant weight loss (at least 5% of body weight)?
Survey question: Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from overweight/obese health care professionals?
Survey question: Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from health care professionals who have a healthy weight?
Discussion
This study is the first to examine the impact of non-physician health professional BMI on obesity care practices and self-efficacy, as well as perceptions of patient trust in weight loss advice, although past studies have examined this relationship among primary care physician health professionals (5, 6). Contrary to our hypotheses, we found no difference by health professional BMI in obesity care practices. We observed differences in self-efficacy with normal BMI professionals being more likely than overweight/obese professionals to report success in helping patients with obesity achieve clinically significant weight loss. Interestingly, most health professionals in our sample, regardless of BMI, did not feel successful in helping patients lose weight until they are extremely obese (class II obese or greater) suggesting important missed opportunities for early intervention.
The current findings are contrary to our earlier work that suggested normal BMI physicians more frequently report discussing weight loss compared to overweight/obese physicians (5). These results suggest that normal BMI non-physician health professionals have higher self-efficacy than overweight and obese health professionals, which is similar to prior research among physicians indicating that personal health promotion behaviors are strong predictors of attitudes towards obesity care (8). For example, physicians who exercise more and maintain a healthy diet are more likely to discuss exercise and weight with their patients (9). Generally, our finding of low self-efficacy in obesity care – regardless of BMI – is consistent with past research (10, 11, 12, 13); although some research among health professionals working with the pediatric population report high confidence (14).
Going forward, it will be important to increase self-efficacy among all health professionals regardless of weight, as an unintended consequence of targeted efforts may be to increase obesity stigma, which has risen considerably overtime (15, 16). Increased self-efficacy is positively associated with weight management practices (17). Targeting all health professionals may also help address our finding that most professionals do not feel successful in helping patients with weight loss until they are morbidly obese. Increased opportunities for additional training, ideally as part of required certification, may help improve these current practice patterns and reduce negative attitudes of health professionals towards patients with obesity (18). Future research is needed to understand why healthcare professionals do not typically initiate weight management discussions until patients are morbidly obese.
There are several limitations to this analysis. First, our measures of health professional attitudes do not represent the full possible spectrum of attitude measures in the literature (such as perceived skills (19) or comfort in caring for obese patients (20)), which may bias our results towards the null. Second, some of the included health professionals may have had extensive additional training in obesity (considering themselves “obesity specialists”), which could have biased our results positively. While we did collect information on obesity training, we were unable to account for the huge variation across health professional degree programs. Third, our questions related to trust in health professionals’ advice used words to describe body weight rather than pictures, which may have biased responses. Future studies should consider using silhouettes with these questions to confirm our findings. Fourth, our use of self-reported height and weight may underestimate the prevalence of overweight/obesity in our study population. Finally, our use of body images rather than BMI to solicit health professional perspectives about appropriate patient body weights for weight loss conversations and obesity diagnosis may have been differentially interpreted.
In conclusion, this study suggests that health professional BMI does not impact obesity care practices, but it does impact self-efficacy. Normal BMI health professionals feel more successful than overweight/obese health professionals at helping obese patients lose weight. More research is needed to understand how to improve self-efficacy for delivering obesity care for non-physician health professionals through additional training and how to encourage these professionals to engage obese patients in weight management before patients reach extreme obesity.
What is already known about this subject?
Healthcare for obesity is suboptimal
Physician BMI has recently been identified as a potential barrier to obesity care
Increased self<efficacy is positively associated with weight management practices
What does this study add?
First study to examine the impact of non-physician health professional BMI on obesity care practices and self-efficacy
Health professional BMI does not impact obesity care practices
Health professional BMI does impact self-efficacy; normal BMI health professionals report being more successful than overweight/obese health professionals at helping obese patients lose weight
Acknowledgments
Funding: This work was supported by two grants from the National Heart, Lung, and Blood Institute (1K01HL096409 and K24HL083113) and one grant from the Health Resources and Services Administration (T32HP10025-17-00).
Appendix A
Survey Development
Summary
Data collection for the Health Professionals Survey on Weight Loss Management was conducted online between January 20 and February 5, 2014. . We aimed to recruit one hundred respondents from each of five professions were recruited through the Research Now Healthcare Professional Panel. In total, 3,308 invitations were sent to a randomly selected sample of panel members who were dieticians/nutritionists, nurses, behavioral psychologists or mental health professionals, physical therapists, and pharmacists. Respondents were asked to complete a 10 minute survey about obesity care. A total of 500 respondents completed the questionnaire.
Questionnaire Development and Pretesting
The questionnaire for this survey was developed by Johns Hopkins Bloomberg School of Public Health researchers with expertise in obesity and in consultation with SSRS of Media, PA and tested for length and comprehension. A total of 20 pretest interviews (4 per profession) were conducted by SSRS by inviting panel members to participate in the study and asking them for comments they had about any of the questions. A total of 5 pretest interviews (one per profession) were conducted by Johns Hopkins Bloomberg School of Public Health researchers by inviting a convenient sample of professionals working in the health system. Following the pretest, several changes were incorporated into the final questionnaire.
Recruitment/The Web Panel
The Sample Provider, Research Now of Plano, TX., randomly selected respondents from its Healthcare Panel, which recruits healthcare providers via multiple modes such as email, phone, fax and direct mail. Contact information is derived from a variety of commercial sources and association memberships. Respondents are compensated for participation in the panel.
In total 3,308 invitations were sent by email to panel members with the distribution of invitations and outcomes as following:
Table 1.
Recruitinq and Outcomes
| Dieticians/Nutritionists | Nurses | Psychologists/Mental Health Professionals | Physical Therapists | Pharmacists | |
|---|---|---|---|---|---|
| Number of invitations | 530 | 985 | 600 | 655 | 538 |
| Number of clicks on invite | 154 | 276 | 193 | 229 | 200 |
| Completed questionnaire | 100 | 100 | 100 | 100 | 100 |
| Screened ineligible | 51 | 63 | 62 | 49 | 65 |
Note: Recruitment of nurses excluded hospital/inpatient settings, and targeted private practices, group practices, clinics, affiliated clinics. Recruitment of pharmacy professionals excluded hospital/inpatient work settings, and targeted work settings in clinics/clinic pharmacy/retail/group practices/group clinics
Screening
In order to qualify for the study, respondents needed to: (1) confirm their profession and (2) indicate that they work at their profession at least 15 hours a week in an ambulatory setting.
Weighting
The final data were weighted to address concerns with systematic under- or over-representation of Health Professional subpopulations in the panel, and to account for systematic nonresponse along known demographic parameters of these professions. The data were adjusted in weighting so that the final weighted sample approximates the known distribution for these occupations as reflected in the American Community Survey (ACS). Weighting parameters were derived from a cumulative file for the years 2010 through 2012 to ensure a sufficient amount of cases for each profession in the ACS data.1 To reflect the survey's focus on practicing professionals, only those currently employed these particular occupations were included in the ACS datafile used for deriving these parameters.
Since the sample size for each profession was relatively small (n=100), a limited number of parameters were used in weighting the sample for these professions, namely:
Gender
Age: under 35 years old; 35 to 50 years old; 50 or older
Census region
In order to report about this Health Professional population as a whole, two weights were produced:
Weight1 (Comparison Weight): the sum of weights for each profession matched the unweighted sample size (n=100 for each profession). This weight can be used for comparing the professions.
Weight2 (Total Weight): this modifies Weight1 so that the relative share of each profession reflects its distribution among this population of five professions overall, based on the ACS data.
Table 2 details the weighting parameters used.
Table 2.
Weiqhtinq Parameters by Profession
| Dieticians/Nutritionists | Nurses | Psychologists/Mental Health Professionals | Physical Therapists | Pharmacists | |
|---|---|---|---|---|---|
| Male | 10% | 9% | 31% | 31% | 47% |
| Female | 90% | 91% | 69% | 69% | 53% |
| <35 years old | 32% | 24% | 19% | 33% | 32% |
| 35 to 49 years old | 31% | 37% | 29% | 44% | 36% |
| 50 or older | 37% | 38% | 53% | 23% | 32% |
| Northeast | 20% | 20% | 28% | 24% | 20% |
| Midwest | 22% | 24% | 20% | 23% | 22% |
| South | 36% | 36% | 25% | 32% | 36% |
| West | 32% | 19% | 26% | 21% | 21% |
The weighted margin of error for this survey using Weightl is +/−5.3% and wit Weight +/−8.5%.2
Appendix B
Survey Questions
Appropriate patient BMI for weight related care
Using the picture below, please use the numbers to indicate...
At what BMI do you typically start talking to your patients or clients about weight loss?
At what BMI do you feel that you are less likely to successfully aid patients or clients with weight loss?
Self efficacy and patient trust in weight related advice
How confident are you in your ability to help your obese patients or clients achieve a clinically significant weight loss (at least 5% of body weight)?
Very confident
Pretty confident
Not very confident
Not at all confident
How successful are you at helping your obese patients or clients achieve a clinically significant weight loss (at least 5% of body weight)?
Very successful
Pretty successful
Not very successful
Not at all successful
Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from overweight/obese health care professionals?
More likely
As likely
Less likely
Do you think overweight/obese patients are more likely, less likely or as likely to trust weight loss advice from health care professionals who have a healthy weight?
More likely
As likely
Less likely
Footnotes
Competing interests: The authors have no competing interests
Contributors: SNB, KAG, LAC, and WLB conceived the study and developed the hypotheses. SB analyzed the data. All authors contributed to the interpretation of study findings. SNB drafted the manuscript and all authors contributed to the final draft. SNB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Psychologists/Mental Health Professionals were weighted to population parameters of employed psychologists. The demographic distribution was overall similar to findings in the 2008 APA Survey of Psychology Health Service Providers.
Margin-of-error estimates assume random sampling, which may not be applicable to the web panel.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual Medical Spending Attributable To Obesity: Payer- And Service-Specific Estimates. Health affairs. 2009 doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–129. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Archives of internal medicine. 2009;169:313–314. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bleich SN, Bennett WL, Gudzune KA, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity. 2012;20:999–1005. doi: 10.1038/oby.2011.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perrin EM, Flower KB, Ammerman AS. Pediatricians' own weight: Self-perception, misclassification, and ease of counseling. Obes Res. 2005;13:326–332. doi: 10.1038/oby.2005.44. [DOI] [PubMed] [Google Scholar]
- 7.US Census Bureau 2005-2009 American Community Survey. 2009.
- 8.Spencer EH, Frank E, Elon LK, Hertzberg VS, Serdula MK, Galuska DA. Predictors of nutrition counseling behaviors and attitudes in US medical students. Am J Clin Nutr. 2006;84:655–662. doi: 10.1093/ajcn/84.3.655. [DOI] [PubMed] [Google Scholar]
- 9.Abramson S, Stein J, Schaufele M, Frates E, Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000;10:40–48. doi: 10.1097/00042752-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Story MT, Neumark-Stzainer DR, Sherwood NE, Holt K, Sofka D, Trowbridge FL, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–214. [PubMed] [Google Scholar]
- 11.van Gerwen M, Franc C, Rosman S, Le Vaillant M, Pelletier-Fleury N. Primary care physicians' knowledge, attitudes, beliefs and practices regarding childhood obesity: a systematic review. Obes Rev. 2009;10:227–236. doi: 10.1111/j.1467-789X.2008.00532.x. [DOI] [PubMed] [Google Scholar]
- 12.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: Pediatricians' self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5:150–156. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 13.Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians' perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowenstein LM, Perrin EM, Campbell MK, Tate DF, Cai JW, Ammerman AS. Primary Care Providers' Self-Efficacy and Outcome Expectations for Childhood Obesity Counseling. Child Obes. 2013;9:208–215. doi: 10.1089/chi.2012.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. American journal of public health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 17.Zhu DQ, Norman IJ, While AE. Nurses' self-efficacy and practices relating to weight management of adult patients: a path analysis. Int J Behav Nutr Phy. 2013:10. doi: 10.1186/1479-5868-10-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Budd GM, Mariotti M, Graff D, Falkenstein K. Health care professionals' attitudes about obesity: An integrative review. Appl Nurs Res. 2011;24:127–137. doi: 10.1016/j.apnr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Cheng TL, DeWitt TG, Savageau JA, O'Connor KG. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153:629–635. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 20.Jelalian E, Boergers J, Alday CS, Frank R. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr (Phila) 2003;42:235–245. doi: 10.1177/000992280304200307. [DOI] [PubMed] [Google Scholar]