Abstract
Purpose
Examine reliability and validity of a specialized health-related quality of life questionnaire for rectal cancer (RC) survivors (≥5 years post diagnosis).
Methods
We mailed 1,063 Kaiser Permanente (KP) RC survivors (313 ostomy, 750 anastomosis) a questionnaire containing the Modified City of Hope Quality of Life-Ostomy (mCOH-QOL-O), SF-12v2, Duke–UNC Functional Social Support Questionnaire (FSSQ), and Memorial Sloan-Kettering Cancer Center Bowel Function Index (BFI). We adapted certain BFI items for use by subjects with intestinal ostomies. We evaluated reliability for all instruments with inter-item correlations and Cronbach’s alpha. We assessed construct validity only for the BFI in the ostomy group, because such use has not been reported.
Results
The overall response rate was 60.5% (577 respondents/953 eligible). Compared to nonresponders, participants were on average 2 years younger and more likely non-Hispanic white, resided in educationally nondeprived areas, and had KP membership through a group. The mCOH-QOL-O, SF-12, and FSSQ were found to be highly reliable for RC survivors. In the ostomy group, BFI Urgency/Soilage and Dietary subscales were found to be reliable, but Frequency was not. Factor analysis supported the construct of Urgency/Soilage and Dietary subscales in the ostomy group, although one item had a moderate correlation with all three factors. The BFI also demonstrated good concurrent validity with other instruments in the ostomy group.
Conclusions
With possible exception of the BFI Frequency subscale in populations with ostomies, components of our survey can be used for the entire population of RC survivors, no matter whether they received anastomosis or ostomy.
Keywords: Rectal cancer, health-related quality of life, HRQOL, HMOs, survivorship, ostomy, anastomosis, bowel function, abdominal stoma, psychometric properties
Introduction
Colorectal cancer accounts for over 9% of worldwide cancer incidence, the developed world with a Western culture accounting for over 63% of all cases [1]. It is the third most common cancer worldwide and the fourth most common cause of death [1]. Treatment for most rectal cancer (RC) patients includes major surgery to remove a segment of the bowel and either an intestinal ostomy (externalization of the bowel to the abdominal wall) or, more frequently, an anastomosis (reconnection of the rectum to the colon). Some operations mandate a temporary ostomy to protect a low bowel resection during the healing process. While most temporary ostomies are reversed, there are instances, due to medical or operative complications, when reversal is not performed. Instances also occur when complications from an anastomosis lead to a later ostomy. Radiation and chemotherapy are also the standard of care for RC patients with locally aggressive features (TNM stages T3 and/or N1).
As RC patients are often diagnosed early, and newer chemotherapeutics have augmented survival, the majority of RC survivors will live for many years after diagnosis. The Institute of Medicine report of 2007 [2] recommends that care for cancer survivors should involve addressing the late and long-term effects of the cancer and its treatments. Some information on RC late and long-term effects can be found in the literature related to quality of life [3–14]. Our research program has examined patient-centered issues in the general long-term (≥5 years since diagnosis) RC survivor population. The studies from our previous work addressed gender differences (women living with an ostomy showing a greater adverse impact on health-related quality of life compared to men), skin problems in those with ostomies, relationship challenges, dietary changes, work concerns, and spiritual well-being [3–7, 15–17].
Gaps in knowledge remain regarding bowel function in RC survivors with ostomies and the relationship of bowel function to social and recreational activities, work-related issues, and caregiver support among RC survivors. The Memorial Sloan-Kettering Cancer Center Bowel Function Index (BFI) is a validated tool to assess bowel function in RC survivors with anastomosis [18], but to our knowledge no tool has been disseminated to assess bowel function in RC survivors with ostomies. Towards that end, our aim was to adapt the BFI to create a new version applicable to bowel function of a person with an ostomy, and to test it psychometrically, combined with a multi-item survey incorporating multiple validated questionnaires. The study reported here addresses the reliability of the components of the entire survey, and validity of the BFI adapted for RC survivors with ostomies.
Methods
The target population was long-term (≥5 years post diagnosis) RC survivors from two Kaiser Permanente (KP) Regions, Northern California (KPNC) and Northwest (KPNW), who had undergone a major intra-abdominal operation as part of their cancer treatment, resulting in either an ostomy or anastomosis. We recruited by mailed survey all potentially eligible participants (current KP members age 18 years or older with tissue-verified RC diagnoses) identified through an electronic search of each site’s computerized tumor registry. The study was coordinated at the University of Arizona Cancer Center (AZCC) and approved by its Internal Review Board (IRB) as well as those at both KP sites. The survey cover letter contained all elements of informed consent, and all participants gave implied consent by completing and returning the survey, a process that was approved by the IRBs.
A comprehensive demographic and medical history was obtained via the survey and analysis of electronic medical record data. Multiple demographic parameters were collected, including age, gender, ethnicity, weight, height, educational status, marital status, and employment history. Medical history items included type of surgery; reason for surgery; distance of tumor from anal verge; length of time since surgery; Surveillance, Epidemiology, and End Results (SEER) general summary stage; and comorbidities, including the Charlson-Deyo comorbidity index [19].
Survey packets included scannable forms programmed with Teleforms 10.3 (Copyright 2007 Cardiff) and developed at the AZCC site, which were sent to potential participants by their respective KP site. Two weeks after each survey packet was mailed, potential subjects who had not yet returned the study questionnaire were contacted by phone (up to ten attempts). If they were interested in participating, individuals were asked to complete the questionnaire and return it in the postage-paid envelope, or if they preferred they were given the option to answer the questionnaire items over the phone. Patients refusing participation were no longer contacted.
The survey in this report combined portions or all of the following four survey instruments: (1) the Modified City of Hope Quality of Life-Ostomy (mCOH-QOL-O) [20]; (2) the Short-Form health survey, version 2 SF-12v2 [21]; (3) the Duke–UNC Functional Social Support Questionnaire (FSSQ) [22]; and, (4) the Memorial Sloan-Kettering Cancer Center Bowel Function Index (BFI) [18].
The mCOH-QOL-O was developed as part of a program of research in health-related quality of life (HRQOL) that spanned over 20 years and included development of multidimensional instruments for assessing HRQOL in a variety of cancer populations. Utilizing the City of Hope four-dimensional framework [20], the mCOH-QOL-O questionnaire provided subscale scores for the following domains: physical well-being (11 items); psychological well-being (13 items); social well-being (12 items); and spiritual well-being (six items). In addition, there is an overall HRQOL item, as well as a total HRQOL scale that is the arithmetic mean of all the other items. We have previously reported the confirmation of construct validity of the subscales, reliability (alpha) ranging from 0.77 to 0.90, and the ability of the questionnaire to discriminate between subpopulations with specific concerns [20]. The items, subscales, and total HRQOL scale use an 11-point response scale. About one-third of the items were reverse scaled in the instrument, but for analysis, all items were coded as 0 = poorest and 10 = best functioning and/or quality of life. The mCOH-QOL-O also includes several optional open-ended questions related to ostomy equipment problems, ostomy location issues, and irrigation practices, which were included in the version for the RC-ostomy survivors but not in the abridged version for the RC-anastomosis survivors. The mCOH-QOL-O was originally designed for subjects with ostomies, and we have previously reported its modification for subjects with anastomosis, including those who had had temporary ostomies. The anastomosis version of the mCOH-QOL-O has demonstrated comparable reliability to the original [8].
The SF-12v2 is an improved version of the SF-12, has established validity and is one of the most frequently used measures of functional health and well-being in the world today [21]. The SF-12v2 produces scores for the following eight multi-item subscales: physical functioning (2 items), role limitations due to physical health problems (2 items), pain (1 item), perceived general health (1 item), mental health (2 items), role limitations due to emotional problems (2 items), social functioning (1 item), and energy/fatigue (1 item). The subscale scores can range from 0 to 100, with higher scores reflecting better functioning or well-being. In addition, physical (PCS) and mental (MCS) component summary scores can be calculated from the SF-12v2 based on a population norm-based scoring function. Subscale and summary scores were calculated with QualityMetric Health Outcomes Scoring Software 4.5 (copyright QualityMetric, Lincoln, Rhode Island, USA 2004–2011).
The Duke–UNC Functional Social Support Questionnaire (FSSQ) is a validated single scale and measures the individual’s perception of their amount and type of personal social support [22]. The eight items have response options on a 5-point scale ranging from 1 (“Much less than I would like”) to 5 (“As much as I would like”).
The BFI was developed to assess bowel function for rectal cancer patients undergoing surgery with anastomosis. It is the only instrument of which we are aware that is designed to measure bowel function specifically for rectal cancer survivors. The 18-item questionnaire contains three subscales—Frequency, Dietary, and Soilage, with published test-retest reliability of 0.74, 0.62, and 0.87, respectively, and 0.84 for the overall instrument [18]. The BFI demonstrated discriminant validity among survivors with preoperative radiation, postoperative radiation, and no radiation; among local excision, low anterior resection, and coloanal anastomosis; and between handsewn and stapled anastomosis. It further demonstrated consistency with four of four Fecal Incontinence Quality of Life subscales and 9 of 17 European Organization for Research and Treatment of Cancer (EORTC) subscales. [18] The BFI provides unique information about the bowel functioning in survivors who have been treated for rectal cancer. Recently, it has been shown [23] that it is much more effective in detecting functional differences in survivors when compared to the EORTC QLQ-C30 and QLQ-CR38 questionnaires, which are commonly used to evaluate function. Because the BFI was designed for and validated in survivors with anastomoses, we adapted certain BFI items for use by permanent ostomy subjects, on whom it had never been reported. We established content validity for use of this instrument in subjects with ostomies by review, selection, and adaptation of the items from each subscale based on in-depth qualitative research with rectal cancer survivors. We subsequently adapted this instrument to address bowel concerns of survivors with ostomies and report the reliability and validity of this adapted instrument below.
Statistical Analysis
We compared demographic and clinical characteristics between RC survivors with ostomy and anastomosis using the Student’s t-test for continuous measures and the chi-square test for categorical measures. The anastomosis and ostomy groups were analyzed separately when scales had different versions for each group. In order to demonstrate that instruments showed persistent reliability in our study sample, we evaluated the reliability of all scales within the survey with internal consistency reflected by inter-item correlations and Cronbach’s alpha. A value of 0.7 or greater was considered acceptable. Because the BFI had not been used or validated previously with an RC-ostomy population, we assessed the validity of the ostomy version of the BFI in this group only. We assessed construct validity (whether items measured latent constructs or underlying concepts) in the ostomy group with factor analysis. Item-todomain correlations were calculated to evaluate the extent to which each item was associated with its domain or with another competing domain. A correlation of 0.3 was considered acceptable. After finding in exploratory factor analysis that the items loaded on three factors, we limited the factor analysis to 3 factors, using an orthogonal varimax rotation [24]. These factors were named for those previously validated by Temple and colleagues for anastomosis survivors (Urgency/Soilage, Frequency, and Dietary) [18]. Concurrent validity was assessed for subscales from the mCOH-QOL-O and the SF12v2 via Pearson’s correlations. We evaluated discriminant validity by testing (Student’s t-test) whether the BF subscales could differentiate between survivors according to theorized clinical and demographic variables previously used in validation studies of the BFI [18, 25] and the mCOH-QOL-O [20]: age (dichotomized at median 75 years), time since surgery (dichotomized at median 14 years), and sexual satisfaction.
Results
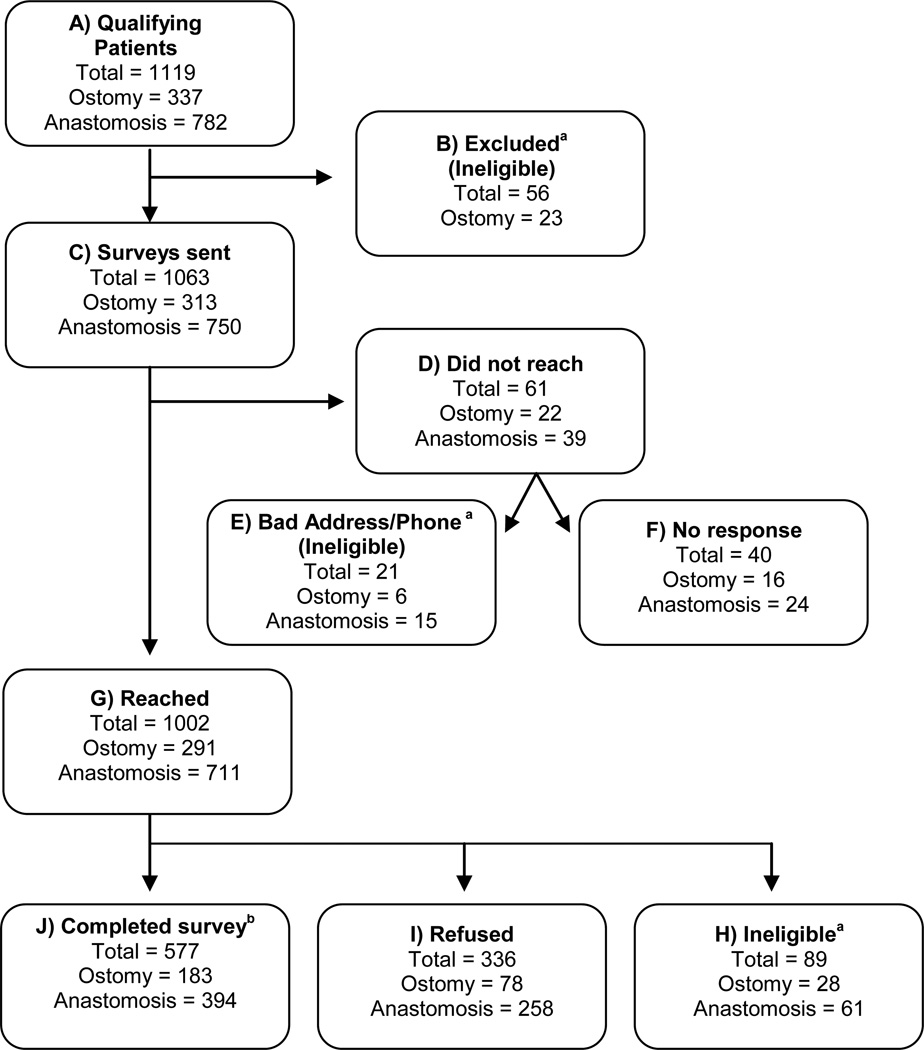
We mailed questionnaires to 1,063 rectal cancer survivors (≥5 years post-diagnosis) during 2010–2011. Eligible patients were identified in tumor registry in September 2009. Dates of enrollment into the study ranged from January 2010 to December 2011.. Figure 1 shows the Consort Diagram flow of our recruitment. Our overall response rate was 60.5% (577 respondents/953 eligible).
Fig. 1.
Recruitment Flow Diagram
a Found to be ineligible (dead, not rectal cancer, etc.) after initial search (B), those who had a wrong address and phone number (E) or found to be ineligible (not rectal cancer, no intra-abdominal surgery, etc.) after return of survey (H)
b Response rates (completed/eligible): 58.6% ostomy, 66.8% anastomosis, 60.5% total
Response bias assessment
We conducted an evaluation of potential response bias in our sample. Selected measures were approved by the three IRBs for aggregate analysis comparing respondents to non-respondents. Table 1 shows that those who refused or could not be reached were older by an average of 2.2 years (p=0.01), were less likely to be non-Hispanic white (p<0.001), were more likely to be enrolled in Kaiser Permanente as an individual versus through a group (p=0.02), and were more likely to live in a census tract designated “educationally deprived” (p=0.04). Participants and nonresponders did not differ significantly on time since diagnosis, sex, Hispanic ethnicity, tumor stage, Medicare and Medicaid eligibility, and census tract indicators of low income or poverty.
Table 1.
Characteristics of Participants versus Non-participants
| Characteristics | Participants (N=577) |
Refused/Not Reached (N=397) |
P-value |
|---|---|---|---|
| Age (yr), mean (SD) | 72.8 (10.9) | 74.6 (11.8) | 0.02 |
| Years since diagnosis, mean (SD) | 13.0 (6.2) | 13.0 (6.0) | 0.94 |
| Male (%) | 59.1 | 55.4 | 0.25 |
| Hispanic (%) | 5.2 | 7.7 | 0.12 |
| Non-Hispanic White (%) | 81.8 | 71.5 | <0.001 |
| Stage (%) | |||
| Localized | 70.8 | 73.9 | 0.15 |
| Regional | 26.4 | 22.1 | |
| Distant | 1.1 | 2.6 | |
| Unknown | 1.8 | 1.5 | |
| Medicare eligible (%) | 74.3 | 78.2 | 0.17 |
| Medicaid eligible (%) | 0.35 | 0.77 | 0.37 |
| Individual KP enrollmenta (%) | 28.2 | 35.1 | 0.02 |
| Neighborhood education deprivedb (%) | 17.5 | 22.8 | 0.04 |
| Neighborhood income deprivedb (%) | 11.5 | 14.9 | 0.13 |
| Neighborhood poverty indicatorb (%) | 21.3 | 24.6 | 0.23 |
KP = Kaiser Permanente
Membership enrolled individually, in contrast to through a group
Based on census tract summaries.
Sample characteristics
Table 2 shows participant demographic and clinical characteristics, comparing ostomy and anastomosis groups. The ostomy group was significantly older, more likely to be male, and less likely to have completed college. The ostomy group had significantly longer mean time since diagnosis and surgery, were more likely to have a Charlson-Deyo comorbidity index greater than 2, and had a shorter mean tumor distance from the anal verge. The distribution of SEER general summary stage was not significantly different between groups. The ostomy group was significantly more likely to have received radiation and chemotherapy.
Table 2.
Demographic and Clinical Characteristics of Ostomy and Anastomosis Groups
| Characteristics | Ostomy (N=183) |
Anastomosis (N=394) |
P-value |
|---|---|---|---|
| Age (yr), mean (SD) | 74.7 (11.1) | 72.5 (10.5) | .02 |
| Male (%) | 65.6 | 56.0 | .03 |
| Race/Ethnicity | |||
| Non-Hispanic White | 80.3 | 77.7 | .28 |
| Hispanic | 7.7 | 4.6 | |
| African American | 2.7 | 3.5 | |
| Asian | 6.6 | 9.1 | |
| Other/unknown/mixed | 2.7 | 5.1 | |
| Education: college degree (%) | 27.6 | 43.3 | <.001 |
| Income over $50,000/yr (%) | 39.4 | 46.4 | .13 |
| Married/Partnered (%) | 66.1 | 64.1 | .64 |
| Years since diagnosis, mean (SD) | 15.0 (7.4) | 12.6 (5.5) | <.0001 |
| Years since surgery, mean (SD) | 14.6 (7.7) | 12.4 (5.5) | .0001 |
| Charlson-Deyo comorbidity score > 2 (%) | 29.5 | 18.0 | .002 |
| Tumor distance from anal verge (cm), mean (SD) | 5.9 (3.8) | 11.4 (4.9) | <.0001 |
| Stage (%) | |||
| Localized | 45.9 | 51.1 | .21 |
| Regional | 47.5 | 45.8 | |
| Distant | 1.6 | 0.76 | |
| Unknown | 4.9 | 2.3 | |
| Received chemotherapy (%) | 57.9 | 47.9 | .02 |
| Received radiation treatment (%) | 49.2 | 34.9 | .001 |
Adaptations to BFI for ostomy group
Table 3 shows the wording of items from the three subscales of the MSKCC Bowel Function Instrument, as well as the adaptations made by our team for administration to RC survivors living with an ostomy. Two Frequency questions regarding time to get to the toilet, as well as the number of bowel movements per day, were deemed not applicable for ostomy survivors. We changed “bowel function” and the number of bowel movements to the number of times the respondent changed or emptied their ostomy bag. Finally, because of ostomy location, we reworded Soilage questions regarding undergarments to garments in general.
Table 3.
MSKCC Bowel Function Instrumenta
| Item | Question | Ostomy adaptation |
|---|---|---|
| Urgency/Soilage | ||
| Soilage day | Have you had soilage (leakage of stool) of your undergarments during the day? | Substitute “garments” for “undergarments” |
| Soilage bed | Have you had soilage (leakage of stool) of your undergarments when you go to bed? | Substitute “garments” for “undergarments” |
| Tissue/padb | Have you used a tissue, napkin, and/or pad in your undergarments during the day in case of stool leakage? | Substitute “garments” for “undergarments” |
| Alter activities | How often have you had to alter your activities because of your bowel function? | Substitute “because of the number of times you changed or emptied your bag” |
| Frequency | ||
| Medicines | Have you used medicines to decrease the number of bowel movements (drugs like Imodium®, Lomotil®)? | Substitute “decrease the number of times did you change or empty your bag” |
| Diarrhea | Have you had diarrhea (no form, watery stool)? | No change |
| Loose stool | Have you had loose stool (slight form, but mushy)? | No change |
| Able to wait | Have you been able to wait 15 minutes to get to the toilet when you feel like you are going to have a bowel movement? | Not included |
| Toilet on time | Do you get to the toilet on time? | Not included |
| Number of BMs | How many bowel movements do you generally have in 24 hours? | How many times did you change or empty your bag in a typical 24-hour period? |
| Dietary | ||
| Food increases BM | Do certain solid foods increase the number of bowel movements in a day? | Substitute “increase the number of times did you change or empty your bag in a day” |
| Liquids increase BM | Do certain liquids that you drink increase the number of bowel movements in a day? | Substitute “increase the number of times did you change or empty your bag in a day” |
| Limited food | Have you limited the types of solid food you eat to control your bowel movements? | No change |
| Limited liquids | Have you limited the types of liquids you drink to control your bowel movements? | No change |
BM = bowel movement
Questions have stem “Over the past 4 weeks, how often…” Responses are 5 choices from “always” to “never” (except for number of BMs)
The nature of pad would differ between groups: diaper or underwear insert for anastomosis versus abdominal pad for ostomy.
Reliability for previously validated instruments
The mCOH-QOL-O, SF-12v2, and FSSQ were found to be consistently highly reliable in both the ostomy and the anastomosis groups. Cronbach’s alphas for the mCOH-QOL-O subscales ranged from 0.83 to 0.93, with the exception of lower scores for the Spiritual Well-being subscale in the ostomy group (0.76) and the anastomosis group (0.77). SF-12v2 subscale alphas were: Physical Function (0.77), Role Physical (0.86), Role Emotional (0.75), and Mental Health (0.71). Cronbach’s alpha for the FSSQ was 0.88.
BFI Reliability
Table 4 shows the results of reliability evaluation and factor analysis of the BFI. In the anastomosis group, the three subscales Urgency/Soilage, Frequency, and Dietary were found to be internally consistent with Cronbach’s alphas of 0.72 or higher. In the ostomy group, however, Urgency/Soilage (alpha = 0.74) and Dietary (alpha = 0.83) were found to be internally consistent, but Frequency (alpha = 0.50) was not. The item “Alter Activities," on the Urgency/Soilage subscale had the lowest correlation with the other Urgency/Soilage items for the anastomosis and ostomy groups (0.44 and 0.38, respectively). However, it did not substantially decrease the overall alpha for the subscale (0.77 when item was excluded).
Table 4.
Reliability and Validity of MSKCC Bowel Function Instrument
| Anastomosis (N=394) |
Ostomy (N=183) |
Ostomy Factor Analysisa | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Correlation with rest |
Alpha without item |
Alpha | Correlation with rest |
Alpha without item |
Alpha | Urgency/ Soilage |
Frequency | Dietary | |
| Urgency/Soilage | .81 | .74 | |||||||
| Soilage day | .74 | .70 | .64 | .62 | .75d | .10 | .13 | ||
| Soilage bed | .69 | .72 | .64 | .63 | .73d | .10 | .16 | ||
| Tissue/pad | .62 | .76 | .52 | .69 | .54d | .21 | .09 | ||
| Alter activities | .44 | .84b | .38 | .77b | .31 | .32 | .37 | ||
| Frequency | .72 | .50c | |||||||
| Medicines | .43 | .68 | .24 | .52 | .07 | .29 | .03 | ||
| Diarrhea | .55 | .65 | .42 | .22 | .20 | .59 | .16 | ||
| Loose stool | .55 | .65 | .30 | .43 | .21 | .50 | .20 | ||
| Able to wait | .37 | .70 | N/A | N/A | N/A | N/A | N/A | ||
| Toilet on time | .41 | .69 | N/A | N/A | N/A | N/A | N/A | ||
| Number BM | .37 | .70 | N/A | N/A | N/A | N/A | N/A | ||
| Dietary | .79 | .83 | |||||||
| Food increase BM | .51 | .78 | .60 | .81 | .17 | .24 | .634 | ||
| Liquids increase BM | .59 | .74 | .62 | .79 | .16 | .45 | .654 | ||
| Limited food | .61 | .73 | .66 | .78 | .08 | −.04 | .784 | ||
| Limited liquids | .67 | .70 | .70 | .76 | .10 | .09 | .804 | ||
Urgency/Soilage, Frequency, and Dietary explained 24%, 19%, and 27% of variance, respectively
Alpha somewhat stronger without item.
Subscale not internally consistent (“reliable”).
Items appear to measure the same latent construct.
BFI construct validity in ostomy group
In factor analysis of the ostomy group, Urgency/Soilage, Frequency, and Dietary explained 24%, 19%, and 27% of variance, respectively. The four items that correlated with the Dietary scale in the original questionnaire loaded on the same subscale (Table 4). Daytime soilage, bedtime soilage, and use of a tissue/pad loaded clearly on the Urgency/Soilage subscale. The alter activities item, however, correlated essentially equally with all three factors. Because the alter activities item did not substantially decrease the overall alpha for the subscale, it was retained in the Urgency/Soilage subscale for the ostomy group. The three applicable items that correlated with the Frequency subscale in the original questionnaire appeared to be distributed on the same subscale for the ostomy group, although the use of medicines did not reach the 0.30 threshold. However, in light of poor reliability of the Frequency subscale in the ostomy group, we did not further explore its construct or discriminant validity.
BFI concurrent validity in ostomy group
The BFI questionnaire demonstrated good concurrent validity in the ostomy group, through significant correlations with several domains from the mCOH-QOL-O and SF-12v2, including several comparable items. Table 5 shows significant correlations for both Dietary and Urgency/Soilage with the subscales and selected items from the mCOH-QOL-O. The Dietary subscale was correlated with mCOH-QOL-O items Adjusted diet due to ostomy (r=0.19, p<.05) and Comfort with diet within 1 month (r=0.27, p<.001). The Urgency/Soilage subscale was correlated with mCOH-QOL-O scaled items Leakage from pouch (r=0.50, p<.001) and Skin surrounding the ostomy (r=0.35, p<.001). In addition, both BFI subscales were significantly correlated with SF-12v2 subscales Role physical, Bodily pain, Social function, Role Emotional, and Mental Health.
Table 5.
Concurrent Validity with mCOH-QOL-O and SF12v2 in Ostomy Group
| Measures | Dietary | Urgency/ Soilage |
Total (2 subscales) |
|---|---|---|---|
| COH-QOL | |||
| Total QOL | 0.31*** | 0.45*** | .45*** |
| Physical well-being | 0.28*** | 0.32*** | .38*** |
| Psychological well-being | 0.25*** | 0.32*** | .34*** |
| Social well-being | 0.32*** | 0.53*** | .48*** |
| Spiritual well-being | 0.01 | 0.10 | 0.06 |
| Adjusted diet due to ostomy | −0.19* | .04 | −.16* |
| Comfort with diet within 1 month | 0.27*** | 0.18* | .29*** |
| SF-12v2 | |||
| Physical Function | −0.03 | .04 | .00 |
| Role Physical | 0.16* | .23** | .21** |
| Bodily Pain | 0.27*** | .28*** | .32*** |
| General Health | 0.12 | .13 | .17* |
| Vitality | 0.03 | .05 | .05 |
| Social Function | 0.27*** | .39*** | .38*** |
| Role Emotional | 0.36*** | .33*** | .41*** |
| Mental Health | 0.34*** | .31*** | .39*** |
p<.05;
p<.01;
p<.001
BFI discriminant validity in the ostomy group
The BFI Dietary scale demonstrated a significant difference according to time since surgery in survivors living with an ostomy. The mean (SD) Dietary score was 15.5 (3.4) in 98 subjects who were 12 or more years since surgery compared to 14.3 (3.2) in 80 subjects with fewer than 12 years since surgery (p=0.02). The Urgency/Soilage difference by duration since surgery did not reach statistical significance [17.4 (2.6) vs 16.5 (3.3), p=0.06]. There was no significant difference found by age in Urgency/Soilage [17.3 (2.6) age ≥ 75 vs 16.8 (3.1) age<75, p=0.33] or Dietary [15.5 (3.2) age ≥ 75 vs 14.5 (3.5) age<75, p=0.06] subscales. There was a significant difference found comparing those who reported sexual satisfaction versus dissatisfaction in Urgency/Soilage [17.6 (2.4) vs 16.2 (3.2), respectively, p=0.03] but not for Dietary [14.9 (3.6) vs 13.8 (3.0), respectively, p=0.17] subscales.
Discussion
As the number of cancer survivors grows each year, cancer survivorship research is increasingly recognized as an important area of study. Survey instruments have been widely used to explore the many issues related to the effects of cancer and its treatment. Therefore, it is imperative to ensure valid and reliable instruments are available and utilized. In the current study we found that instruments we had used in the past continued to provide valid information. Our study of nearly 600 RC survivors used a combination of existing survey instruments to examine multiple facets of HRQOL. These surveys (mCOH-QOL-O, SF-12v2, FSSQ, and BFI in anastomosis) remained reliable in this composite instrument and across groups of RC survivors with varied post-operative challenges. In addition, we validated a survey instrument that enables us to assess bowel function in RC survivors with ostomies, an area that was previously underexplored. The BFI will allow us to identify aspects of patient care across all types of RC survivors, subjects that should be included in patient education. Future reports will include analysis of the QOL and function instruments, describing differences found in the ostomy versus the anastomosis groups of rectal cancer survivors.
Our overall response rate of 60.5% was higher than our previous survey of a similar population [8], which is likely due in part to a protocol of more telephone contact attempts sustained over a longer period, our aggressively reminding survivors, and allowing completion via telephone interviews for those that requested it. Respondents to our survey were similar in most regards to those who did not participate in the survey. While our results are generalizable for most RC survivors in our population, the participants were statistically significantly younger (by 2.2. years on average) and more likely to be non-Hispanic white, reside in educationally nondeprived areas, and had KP membership through a group. Although we were inclusive of the entire KP population in Northern California and Oregon, it is not uncommon in survey studies to encounter lower participation rates among older and minority status individuals. The ecological association between participation and education deprivation is based on census tract designation, which may be a surrogate for other sociodemographic characteristics.
When comparing respondents, those with ostomies had several demographic and clinical differences from those without ostomies. While the ostomy population was slightly older (74.7 vs. 72.5 years, p=0.02), the two-year mean difference may not be clinically relevant, despite being statistically significant. Anastomosis survivors were better educated than those with permanent ostomies, and it is reasonable to further explore this difference in future studies. Ostomy survivors had greater co-morbidity burden during year prior to survey which may be related to their being slightly older and having a greater number of years since diagnosis and surgery. The one expected difference is that participants with anastomoses had tumors with a greater distance on average from the anal verge. There are several likely factors to explain why many survivors in both groups, especially the anastomosis group, did not receive radiation therapy. Such factors include the fact that patients with more superficial tumors, as well as those with tumors high in the rectum or the rectosigmoid junction, are unlikely to receive radiation. Other reasons why patients may not have received radiation include patient refusal, older age, or greater co-morbidities. Additionally, in a complex system where patients may receive a portion of their care outside of the system and/or in the more distant past, a history of radiation therapy may occasionally not be captured in the patient records.
We found that two of the three subscales of the BFI --previously validated for use with RC survivors with anastomosis--could with minor revisions be used reliably in those living with ostomies. This has not previously been reported. Both the Dietary and Urgency/Soilage subscales demonstrated reliability and validity. In the ostomy group, four Dietary items and three of four Urgency/Soilage items clearly loaded on the same factors that had been shown previously for anastomosis survivors, while one Urgency/Soilage item loaded equally with all three factors. The Frequency subscale did not demonstrate reliability, which is not unexpected, as this domain has limited relevance to ostomy survivors who use a bag and two of the original items could not be adapted to the ostomy version.
The Dietary and Urgency/Soilage subscales demonstrated concurrent validity through high correlation with several HRQOL and functional scales in the survey, including all mCOH-QOL scales except Spiritual well-being and five of the eight subscales from the SF12v2. Furthermore these two BFI scales correlated highly with closely related individual items from the mCOH-QOL We also showed that subscales of the BFI could discriminate duration of time since surgery and post-surgical level of sexual satisfaction.
Limitations to this study included: 1) the need to modify certain BFI questions for use in the ostomy population, which may have made them not entirely analogous in meaning to the anastomosis versions and 2) limited clinical measures available that were relevant to discriminant validity analysis.
Conclusions
The BFI has relevance not only as a research instrument, but also as a clinical utility measure to help identify survivorship issues, and assist with the implementation of resources. It provides evidence needed for development of the survivorship care plan, including information about the presence of late and long term bowel effects [18]. When information from the BFI is combined with the MCOH-QOL-O, the SF-12v2, the FSSQ, the broad picture of colon cancer survivorship needs becomes evident, and potential resources can be identified. With this information, interventions can be identified and tested, expanding the quality of care needed for rectal cancer survivors [11]. Based on our psychometric analysis, the BFI can be used for these survivors and augments general information gathered from quality of life, social and physical function assessments. As the Frequency items of the BFI do not display adequate reliability, it is reasonable to omit these questions for an ostomy population.
Acknowledgements
The authors thank Raymond Skeps, Study Coordinator, and Mary Wagner, Administrative Assistant, University of Arizona Cancer Center, Tucson, AZ, for help with this work.
Funding
This research was supported by National Cancer Institute Grant R01 CA106912, an unrestricted donation from the Sun Capital Partners Foundation, and Arizona Cancer Center Support Grant CA023074. Resources and facilities were provided at the Southern Arizona Veterans Affairs Health Care System, Tucson, AZ.
Dr. Herrinton has had research contracts in the past three years with Proctor and Gamble, Centocor, Genentech, and Medimmune.
Footnotes
Publisher's Disclaimer: Disclaimer
The views expressed in this report are those of the authors and do not necessarily represent the views of Kaiser Permanente or the University of Arizona.
Conflicts of Interest
The other authors have no conflicts of interest to disclose.
References
- 1.Haggar FA, Boushey RP. Colorectal Cancer Epidemiology: Incidence, Mortality, Survival, and Risk Factors. Clinics in Colon and Rectal Surgery. 2009;22(4):191–197. doi: 10.1055/s-0029-1242458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Implementing Cancer Survivorship Care Planning. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 3.Grant M, McMullen CK, Altschuler A, Mohler MJ, Hornbrook MC, Herrinton LJ, et al. Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncology Nursing Forum. 2011;38(5):587–596. doi: 10.1188/11.ONF.587-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krouse RS, Herrinton LJ, Grant M, Wendel CS, Green SB, Mohler MJ, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. Journal of Clinical Oncology. 2009;27(28):4664–4670. doi: 10.1200/JCO.2008.20.9502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMullen CK, Wasserman J, Altschuler A, Grant ML, Hornbrook MC, Liljestrand P, et al. Untreated peristomal skin complications among long-term colorectal cancer survivors with ostomies. Clinical Journal of Oncology Nursing. 2011;15(6):644–650. doi: 10.1188/11.CJON.644-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Altschuler A, Ramirez M, Grant M, Wendel C, Hornbrook MC, Herrinton L, Krouse RS. The influence of husbands' or male partners' support on women's psychosocial adjustment to having an ostomy resulting from colorectal cancer. Journal of Wound Ostomy and Continence Nursing. 2009;36(3):299–305. doi: 10.1097/WON.0b013e3181a1a1dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bulkley J, McMullen CK, Hornbrook MC, Grant M, Altschuler A, Wendel CS, Krouse RS. Spiritual well-being in long-term colorectal cancer survivors with ostomies. Psychooncology. 2013;22(11):2513–2521. doi: 10.1002/pon.3318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohler MJ, Coons SJ, Hornbrook MC, Herrinton LJ, Wendel CS, Grant M, Krouse RS. The health-related quality of life in long-term colorectal cancer survivors study: objectives, methods and patient sample. Current Medical Research and Opinion. 2008;24(7):2059–2070. doi: 10.1185/03007990802118360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krouse RS, Mohler MJ, Wendel CS, Grant M, Baldwin CM, Rawl SM, et al. The VA Ostomy Health-Related Quality of Life Study: objectives, methods, and patient sample. Current Medical Research and Opinion. 2006;22(4):781–791. doi: 10.1185/030079906X96380. [DOI] [PubMed] [Google Scholar]
- 10.Mols F, Beijers T, Lemmens V, van den Hurk CJ, Vreugdenhil G, van de Poll-Franse LV. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. Journal of Clinical Oncology. 2013;31(21):2699–2707. doi: 10.1200/JCO.2013.49.1514. [DOI] [PubMed] [Google Scholar]
- 11.McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, Hudson MM. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. Journal of Clinical Oncology. 2013;31(5):631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nikoletti S, Young J, Levitt M, King M, Chidlow C, Hollingsworth S. Bowel problems, self-care practices, and information needs of colorectal cancer survivors at 6 to 24 months after sphincter-saving surgery. Cancer Nursing. 2008;31(5):389–398. doi: 10.1097/01.NCC.0000305759.04357.1b. [DOI] [PubMed] [Google Scholar]
- 13.Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP. A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Annals of Surgical Oncology. 2007;14(7):2056–2068. doi: 10.1245/s10434-007-9402-z. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt CE, Bestmann B, Kuchler T, Longo WE, Kremer B. Prospective evaluation of quality of life of patients receiving either abdominoperineal resection or sphincter-preserving procedure for rectal cancer. Annals of Surgical Oncology. 2005;12(2):117–123. doi: 10.1245/ASO.2005.12.036. [DOI] [PubMed] [Google Scholar]
- 15.Krouse R, Grant M, Ferrell B, Dean G, Nelson R, Chu D. Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. Journal of Surgical Research. 2007;138(1):79–87. doi: 10.1016/j.jss.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 16.Pittman J, Rawl SM, Schmidt CM, Grant M, Ko CY, Wendel C, Krouse RS. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. Journal of Wound Ostomy and Continence Nursing. 2008;35(5):493–503. doi: 10.1097/01.WON.0000335961.68113.cb. [DOI] [PubMed] [Google Scholar]
- 17.Horner DJ, Wendel CS, Skeps R, Rawl SM, Grant M, Schmidt CM, et al. Positive correlation of employment and psychological well-being for veterans with major abdominal surgery. American Journal of Surgery. 2010;200(5):585–590. doi: 10.1016/j.amjsurg.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Temple LK, Bacik J, Savatta SG, Gottesman L, Paty PB, Weiser MR, et al. The development of a validated instrument to evaluate bowel function after sphincter-preserving surgery for rectal cancer. Diseases of the Colon and Rectum. 2005;48(7):1353–1365. doi: 10.1007/s10350-004-0942-z. [DOI] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.Grant M, Ferrell B, Dean G, Uman G, Chu D, Krouse R. Revision and psychometric testing of the City of Hope Quality of Life-Ostomy Questionnaire. Quality of Life Research. 2004;13(8):1445–1457. doi: 10.1023/B:QURE.0000040784.65830.9f. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36)I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 22.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Medical Care. 1988;26(7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Neuman HB, Schrag D, Cabral C, Weiser MR, Paty PB, Guillem JG, Minsky BD, et al. Can differences in bowel function after surgery for rectal cancer be identified by the European Organization for Research and Treatment of Cancer quality of life instrument? Annals of Surgical Oncology. 2007;14(5):1727–1734. doi: 10.1245/s10434-006-9283-6. [DOI] [PubMed] [Google Scholar]
- 24.Morrison DF. Multivariate Statistical Methods. Fourth Edition. Independence, KY: Cengage Learning; 2004. [Google Scholar]
- 25.Zotti P, Del Bianco P, Serpentini S, Trevisanut P, Barba MC, Valentini V, et al. Validity and reliability of the MSKCC Bowel Function instrument in a sample of Italian rectal cancer patients. European Journal of Surgical Oncology. 2011;37(7):589–596. doi: 10.1016/j.ejso.2011.04.002. [DOI] [PubMed] [Google Scholar]