Abstract
The aim of this review is to evaluate the effectiveness and safety of acupuncture for poor semen quality in infertile men. We searched for relevant trials registered up to May 2013 in 14 databases. We selected randomized controlled trials (RCTs) that compared acupuncture, with or without additional treatment, against placebo, sham, no treatment, or the same additional treatment. Two reviewers independently performed the study selection, data extraction, risk of bias and reporting quality appraisal. Risk of bias and reporting quality were appraised by the Cochrane risk of bias tool, the consolidated standards of reporting trials and Standards for Reporting Interventions in Clinical Trials of Acupuncture. The outcomes were sperm motility, sperm concentration, pregnancy rate, and adverse events. Pregnancy was defined as a positive pregnancy test. Four RCTs met the eligibility criteria. Acupuncture increased the percentage of sperm with rapid progression (mean difference - 6.35, 95% confidence interval (CI): 4.38–8.32, P< 0.00001) and sperm concentration (mean difference - 6.42, 95% CI: 4.91–7.92, P< 0.00001), but these two outcomes were substantially heterogeneous among the studies (I2 = 72% and 58%, respectively). No differences in pregnancy rate were found between acupuncture and control groups (odds ratio 1.60, 95% CI: 0.70–3.69, P= 0.27, I2 = 0%). No participants experienced adverse events. The current evidence showing that acupuncture might improve poor semen quality is insufficient because of the small number of studies, inadequacy of procedures and/or insufficient information for semen analysis, high levels of heterogeneity, high risk of bias, and poor quality of reporting. Further large, well-designed RCTs are required.
Keywords: acupuncture, asthenozoospermia, male infertility, oligozoospermia, sperm quality
INTRODUCTION
Parenthood is one of the most prevalent desires among humans. However, many couples suffer from infertility despite regular unprotected intercourse. Male factors account for about half of all causes of infertility.1,2,3 Poor semen quality is the main male factor.1,2,3 Idiopathic oligoasthenoteratozoospermia is the most common medical diagnosis of abnormal semen quality.2
Various empirical drugs have been used to improve abnormal semen quality in infertile men. Androgens, gonadotropins, and corticosteroids are not effective, but follicle-stimulating hormone might be effective in some patients.4 Systematic reviews have shown that antioxidants such as vitamin E and L-carnitine could be effective for improving semen quality and the pregnancy rate of couples.5,6
Acupuncture also has been used to improve semen quality. A Norwegian study reported that approximately 20% of infertile men preferred an alternative treatment like acupuncture.7 However, the therapeutic effects of acupuncture on poor semen quality remain uncertain.1 Therefore, systematic review on the effects of acupuncture on poor semen quality is required.
This systematic review evaluated current evidence from available randomized controlled trials (RCTs) on the effectiveness and safety of acupuncture with regard to semen parameters and the pregnancy rate of couples with male factor infertility.
MATERIALS AND METHODS
The protocol describing the methods for this review was registered prospectively (CRD 42013004930; http://www.crd.york.ac.uk/PROSPERO).
Literature search
The following digital databases were searched for relevant studies in May 2013: the Cochrane Central Register of Controlled Trials (up to the Cochrane Library Issue 5, 2013), Medline (from 1946 to May 15 2013), Embase (from 1974 to May 15 2013), the Cumulative Index to Nursing Allied Health Literature, the Allied Complementary Medicine Database, eight Korean databases (KoreaMed, Korean Medical Database, Korean Studies Information Service System, Korea Education and Research Information Service, National Discovery for Science Leaders, Database Periodical Information Academic, Korea National Assembly Digital Library, and Oriental Medicine Advanced Searching Integrated System) and one Chinese database (China National Knowledge Infrastructure). We established search terms related to three areas (male infertility, semen, and acupuncture). The detailed search strategies used for each database are shown in Supplement 1 (6.5MB, tif) . Reference texts (e.g. andrology/gynecology textbooks, integrative/complementary and alternative medicine textbooks, clinical guidelines, and other review articles) in the relevant publications were manually checked to find missing eligible trials.
SEARCH STRATEGIES
Study selection and data extraction
This study scrutinized all RCTs evaluating the effects of acupuncture on semen parameters in infertile males. In randomized cross-over trials, we only analyzed the data measured before cross-over to remove the carryover effect. Non-randomized trials, quasi-experimental studies, and all observational studies were excluded. We selected trials using manual acupuncture and/or electrically stimulated acupuncture in which needles were inserted in classical acupuncture points. We excluded trials of other treatments using acupuncture points without needle insertion, such as moxibustion, acupressure, laser acupuncture, and electrical acupuncture point stimulation. The control group could have received placebo/sham acupuncture, conventional therapy, or no treatment. Trials that evaluated the effect of acupuncture combined with other treatments, in comparison with the same other treatments alone, were also included. We included these studies because the additional therapeutic effects of acupuncture could be estimated in these trials. Trials without a clear description of at least one of the semen parameters, including semen ejaculate volume, sperm concentration, sperm motility, or sperm morphology, were excluded.
The titles and abstracts retrieved from the electronic databases or relevant publications were examined closely, and the whole content of articles that were considered to meet the eligibility criteria was analyzed. We selected relevant studies only after the close examination of full manuscripts.
Two independent reviewers (UMJ and JYJ) performed a literature search, study selection, and data extraction using a standard form. All disagreements were resolved by consensus between the two reviewers or arbitration by another reviewer (SL). If the data in an article were insufficient or ambiguous, one reviewer (UMJ) contacted the corresponding author by E-mail to request additional information.
Data assessment and synthesis
Two reviewers (UMJ and JYJ) independently assessed the risk of bias and the reporting quality of the included studies. The risk of bias was evaluated using the “risk of bias” tool developed by the Cochrane collaboration. The Consolidated Standards of Reporting Trials (CONSORT), and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA)8,9 were used to evaluate reporting quality.
Statistical analyses were performed with RevMan 5.0 (Cochrane collaboration, Oxford, UK). We calculated odds ratios (ORs) for the dichotomous variable (number of pregnancies), and mean differences for the continuous variables (sperm motility and sperm concentration) using a random-effects model with 95% confidence intervals (CI). We utilized a random-effects model because of the clinical and/or methodological heterogeneity of the included trials. Based on the Cochrane guidelines, Cochrane's Q test results with P < 0.01 and I2 ≥ 75% indicated considerable heterogeneity. If the considerable heterogeneity could be explained by differences in study features, we conducted subgroup analysis.
RESULTS
The searches yielded 801 articles, 700 of which were excluded based on the title and abstract. Ninety-seven studies were excluded after full contents of these studies had been analyzed or the corresponding authors had been contacted: 75 were non-RCTs, three were review articles, 17 used inadequate interventions, one lacked semen analysis10 and the other11 was the same trial in a study12 that had already been included. Four eligible RCTs12,13,14,15 including a total of 500 male participants were chosen (Figure 1). The characteristics of the included studies are presented in Table 1.
Figure 1.
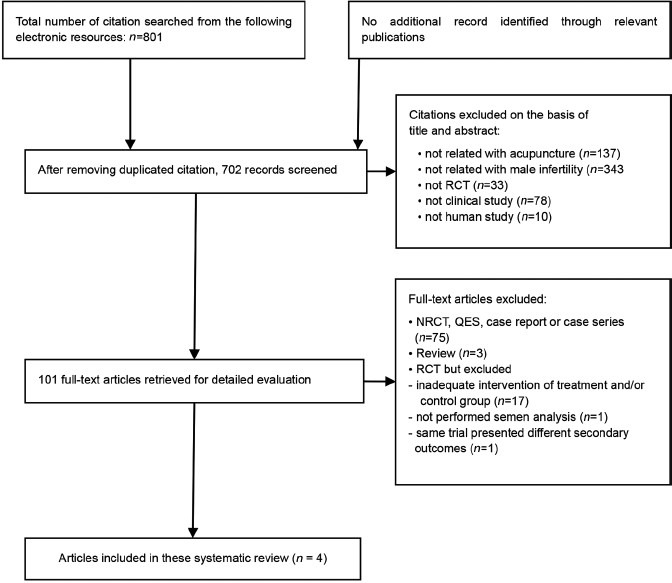
Study selection flow chart. NRCT: non-randomized controlled trial; QES: quasi-experimental study; RCT: randomized controlled trial.
Table 1.
Summary of the results of the randomized controlled trials of acupuncture for male infertility
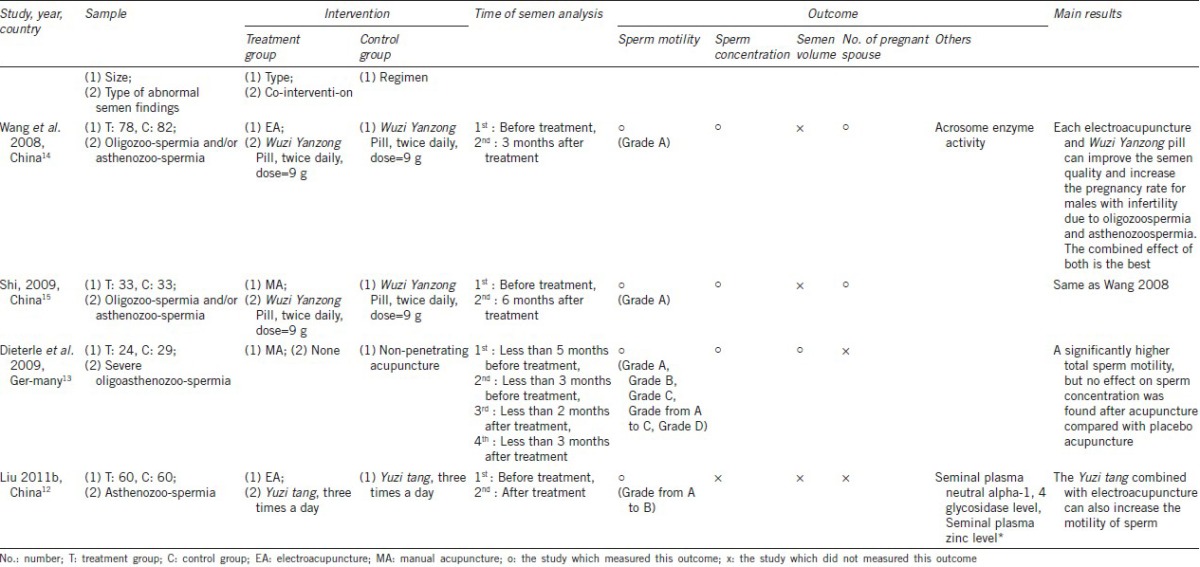
Population
The trials were performed in two different countries; one was conducted in Germany,13 and the others were conducted in China.12,14,15 Two trials14,15 recruited patients with oligozoospermia or asthenozoospermia that had been diagnosed according to the World Health Organization (WHO) criteria. One trial12 recruited only patients with asthenozoospermia that had been diagnosed according to the WHO criteria. The remaining trial13 reported that severe oligoasthenozoospermia patients were recruited, but in actuality, only oligozoospermia patients were recruited (<106 sperm per ml). No studies recruited teratozoospermia patients. Three trials12,14,15 excluded men who could not have children due to female factors. Three trials13,14,15 also excluded men who were infertile due to organic diseases.
Interventions
One trial13 used one manual acupuncture treatment group and one control group, which received a nonpenetrating placebo acupuncture, to evaluate the efficacy of acupuncture. The others12,14,15 established three treatment groups: the first group received acupuncture therapy combined with an oral herb mixture, the second group were only administered the herb mixture, and the third group received the acupuncture therapy alone. We considered the first group to be the treatment group and the second group to be the control group in these trials12,14,15 to evaluate the additional effects of acupuncture.
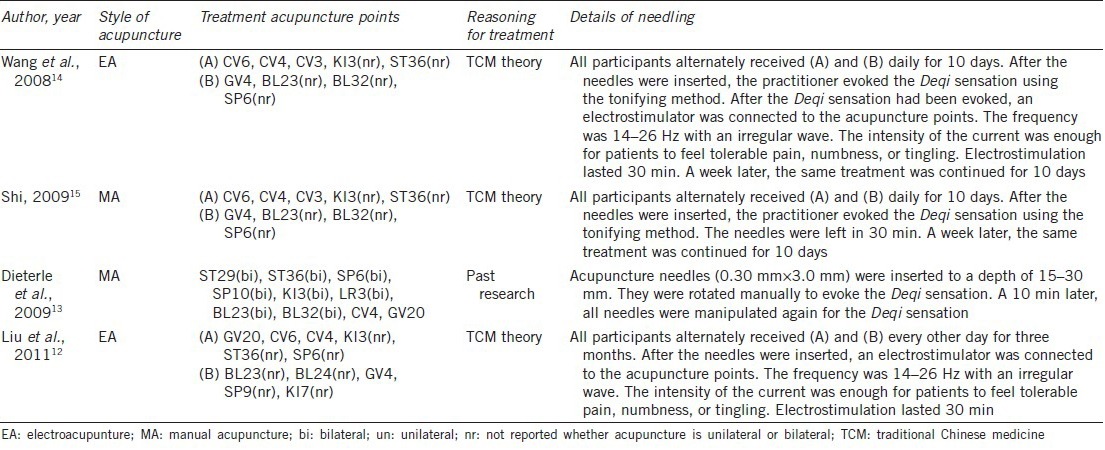
The selected acupuncture points, administrative procedures, and treatment regimens were highly variable among the studies. Only two trials14,15 used the same acupuncture points and treatment regimens, and they used similar procedures (except for acupuncture style). All of the trials induced De qi sensation, which is a type of sensation following acupuncture placement and manipulation.16 The duration of therapy ranged from 27 days14,15 to 3 months.12 Each acupuncture regimen is summarized in Table 2.
Table 2.
Summary of the acupuncture points and techniques used in the randomized controls trials
Outcomes
Semen samples were evaluated according to the WHO standard in all the trials. Three trials12,14,15 measured abnormal semen quality determined according to the WHO criteria published in 1999, while the other trial13 did not report the year when the adopted WHO criteria was published. The frequency and time of semen analysis are described in Table 1.
All of the trials assessed sperm motility but reported different reference points according to the WHO classification of the grades of motility: one trial12 reported the percentage of progressively motile sperm (grade A + B), and the other three trials13,14,15 reported the percentage of sperm with rapid progression (grade A). One trial13 also reported the percentage of sperm with slow or sluggish progression (grade B), the percentage of nonprogressively motile sperm (grade C), and the percentage of motile (grade A + B + C) sperm. Three trials13,14,15 assessed sperm concentration and only one13 trial assessed semen volume. None of the studies assessed sperm morphology.
The diagnostic criterion for pregnancy was a positive pregnancy test. None of the studies documented the pregnancy rate using this criterion. Although two trials14,15 reported the pregnancy rate of couples with male factor infertility, the diagnostic criterion for pregnancy was not clearly documented. We attempted to contact the authors of the two trials to determine which diagnostic criterion for pregnancy they had used. The author of one study14 only replied that the diagnostic criterion for pregnancy was a positive pregnancy test. All of the included trials reported that none of the participants experienced adverse events.
Risk of bias
Among the four RCTs, three12,14,15 adopted poor randomization procedures with an allocation concealment method based on hospital visitation order, while only one13 described adequate methods of random sequence generation and allocation concealment. One trial13 blinded patients and outcome assessors. The other three trials12,14,15 did not report any information on blinding. Although all the trials reported how many participants dropped out or withdrew, three trials12,14,15 were estimated to have a high risk of bias because they did not include any information on whether drop-outs or withdrawals occurred before or after randomization. Risk of bias from selective outcome reporting or from other sources was unclear in all of the included trials (Figure 2).
Figure 2.
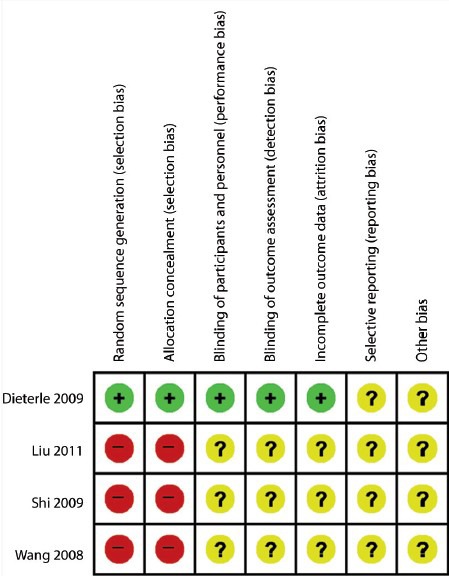
“Risk of bias” summary: review of authors’ judgments about each risk of bias item for each included study.
Reporting quality
Even though the CONSORT statement and STRICTA recommendations were updated in 2010, the 2001 versions were used to assess reporting quality because all four trials were conducted before 2010. Based on the CONSORT statement, all the RCTs described the eligibility criteria, sequence generation, adverse events, and a general interpretation of the results. Three RCTs12,13,14 documented the statistical methods used to compare outcomes between groups. Two RCTs14,15 presented the baseline demographic and clinical characteristics of the participants. All of the RCTs either improperly reported or did not report items such as specific objectives and hypothesis, clearly defined outcome measures, methods of random allocation concealment, the precision of each outcome, ancillary analysis, and generalizability. The detailed results are presented in Supplement 2 (3.2MB, tif) .
Reporting quality of randomized controlled trials based on the consolidated standard of reporting trials (CONSORT)
One study13 mentioned that it had been conducted in accordance with STRICTA, but it did not report the rationale for treatment, needle type, practitioner's training duration, or practitioner's years of clinical experience. Three RCTs12,14,15 were evaluated as having equal reporting quality based on STRICTA. They had good reporting quality in 11 sub-items (style of acupuncture, rationale for treatment, acupuncture response elicited, type of needle stimulation, needle retention time, number of treatment sessions, frequency of treatment, co-interventions, intended effect of control intervention, precise description of control intervention, and sources that justified the choice of control). The detailed results are presented in Supplement 3 (1.5MB, tif) .
Effects of interventions
Sperm motility
The percentages of grade A and grade A + B motile sperm were pooled because these outcomes were used to diagnose asthenozoospermia.17,18 Three trials13,14,15 measured the percentage of grade A sperm motility, and the other trial12 measured the percentage of grade A + B sperm motility. Overall, the pooled data indicated considerable heterogeneity (χ2 = 122.19, P < 0.00001, I2 = 98.0%), so subgroup analysis was conducted. The pooled data for the percentage of grade A sperm motility showed large differences between acupuncture and control groups (mean difference 6.35, 95% CI: 4.38–8.32, P < 0.00001), but the results across the trials were substantially heterogeneous (χ2 = 7.09, P = 0.03, I2 = 72%). Subgroup analysis was not performed for the percentage of grade A + B sperm motility because it was only evaluated in one trial (Figure 3).
Figure 3.
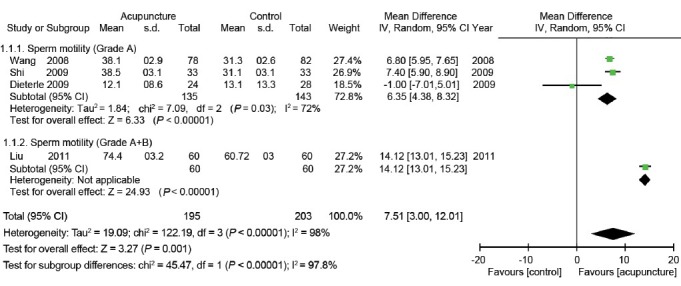
Forest plot for comparison: acupuncture with/without additional treatment versus placebo or same additional treatment. Outcome: sperm motility.
Sperm concentration
Three trials13,14,15 evaluated sperm concentration. The pooled results showed a significant difference between acupuncture and control groups (mean difference 6.42, 95% CI: 4.91–7.92, P < 0.00001), but substantial heterogeneity among the trials was observed (χ2 = 4.71, P = 0.09, I2 = 58%) (Figure 4).
Figure 4.
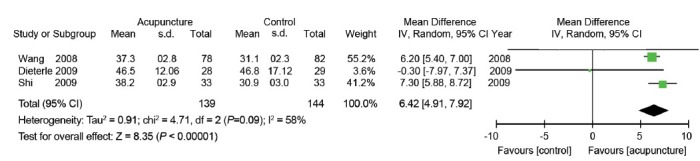
Forest plot for comparison: acupuncture with/without additional treatment versus placebo or same additional treatment. Outcome: sperm concentration.
Pregnancy rate (positive pregnancy test rate)
We determined that one trial14 reported the rate of having a female partner with a positive pregnancy test from contacting the author. No significant difference was found between the acupuncture and control groups in the study (OR: 1.52, 95% CI: 0.46–5.00). Another trial, which reported pregnancy without clear diagnostic criteria, also showed no significant difference between the two groups (OR: 1.69, 95% CI: 0.52–5.44). Despite an unconfirmed definition of pregnancy in one study, we attempted to pool the results. The results showed no significant differences between the acupuncture and control groups (OR: 1.60, 95% CI: 0.70–3.69, P = 0.27). There was also no significant heterogeneity between these trials (χ2 = 0.02, P =0.90, I2 = 0%) (Figure 5).
Figure 5.
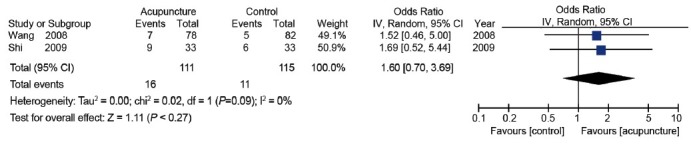
Forest plot for comparison: acupuncture with/without additional treatment versus placebo or same additional treatment. Outcome: pregnancy rate.
Adverse events
All the RCTs reported that no participants experienced adverse events.
DISCUSSION
This systematic review included a total of four RCTs that evaluated acupuncture with or without an additional oral herb mixture, in comparison with placebo or the herb mixture alone. We found that acupuncture might significantly improve sperm motility and sperm concentration, but has no significant additional impact on the pregnancy rate of couples with male infertility. No adverse events were reported in all the trials.
The pooled data on sperm motility and concentration suggest that acupuncture could be applied to oligozoospermia and/or asthenozoospermia patients. Various mechanisms could explain the effectiveness of acupuncture. Pei et al.19 have reported that acupuncture could be beneficial for acrosome position and shape, nuclear shape, axonemal pattern and shape, and accessory fibers. Gurfinkel et al.20 suggested that neural stimulation by acupuncture might affect testicle and epididymis vasodilation. Siterman et al.21,22 proposed that acupuncture might reduce lipid peroxidation in human spermatozoa or genital inflammatory reaction by enhancing immune responses. Future studies confirming these mechanisms are needed.
Although acupuncture might seem beneficial for improving semen quality, the evidence in favor of acupuncture is not compelling. Discrepancy in the effectiveness of acupuncture among the studies is one of the factors that make it difficult to draw definite conclusions. Three studies12,14,15 in our meta-analysis reported positive results on semen quality, while one study13 did not. Different studies that were excluded in this review also indicate mixed results.20,21,22,23,24 We suggest that the following factors possibly caused these discrepant results. First, the outcomes could be affected by whether placebo acupuncture was applied in the control groups. Placebo acupuncture can evoke therapeutic effects25,26 or expectancy effects.27,28 Thus, the differences which were found between the treatment and control groups in one study13 might be underestimated, while the differences in the other three studies12,14,15 might be overestimated. Second, inadequate procedures and/or insufficient information for semen analysis could affect outcomes. The WHO states that two semen samples should be collected after a minimum of 2 days to a maximum of 7 days of sexual abstinence and that the interval between the two collections should range from 7 days to 3 weeks to ensure reliable results.17,29 Although semen samples were collected after a sufficient period of abstinence in the three RCTs, semen sample collection was only conducted once before and once after treatment.12,14,15 Although the remaining RCT13 collected two samples at every assessment, the shortest interval between semen collections was 1 month, and there was no report of whether semen collections were conducted after abstinence. These inadequate procedures and the insufficient information provided for semen analysis made it difficult to validate these results. Finally, high risk of bias and poor reporting quality could cause inconsistent effects. Three RCTs12,14,15 used inadequate methods for sequence generation and allocation concealment, which could have caused selection bias. In addition, most items in CONSORT and STRICTA were not described in the three studies.12,14,15 This means that the studies might not have been conducted according to a predefined plan; therefore, outcomes could have been biased. Furthermore, it is known that there can be an inherent tendency for the treatment group to show more positive results than its control group in a study with poor reporting quality.30
Substantial heterogeneity among the three included studies13,14,15, which reported the percentage of sperm with rapid progression and sperm concentration, is another factor that makes it difficult to draw definite conclusions. Feature differences among the three studies could have led to substantial heterogeneity. First, different treatment protocols might have induced heterogeneity. The participants in two RCTs14,15 received two different acupuncture regimens. After receiving one regimen daily for 10 days, the participants had a rest for 7 days, and then another regimen was also applied daily for 10 days (Table 2). The participants in another study13 received one acupuncture regimen twice a week for 6 weeks without a resting period. Second, differences in the objectives among the studies might have caused heterogeneity. Two RCTs14,15 evaluated the combined effects of acupuncture and herbs compared with herbs alone, while another study13 evaluated the effects of acupuncture compared with placebo acupuncture. Third, different target populations among infertile men could have resulted in heterogeneity. Two RCTs14,15 recruited oligozoospermia and/or asthenozoospermia patients, whereas one study13 recruited only severe oligozoospermia patients. Finally, inconsistency regarding the risk of bias and reporting quality could have led to heterogeneity. Two14,15 of the three studies were identical in all items related to the risk of bias. The other study13 and the above two studies14,15 were identical in only two items related to the risk of bias. A similar tendency was observed in our assessment of reporting quality. Two studies14,15 had similar results for each item on STRICTA and CONSORT, but the other study13 differed from the above two studies in more than 50% of the items.
The pooled result for pregnancy rate of couples with male infertility showed no significant difference between the treatment and control groups. However, we could not conclude that acupuncture in infertile men has no effect on the pregnancy rate from this result. The herbal co-intervention could have contributed to the nonsignificant differences in pregnancy outcomes. Two studies14,15 used the Wuzi Yanzong herb mixture, which is often administered to improve semen quality in traditional Chinese medicine, as a co-intervention in the treatment and control groups. This medication might have enhanced semen quality in both groups and thus resulted in the lack of a difference in pregnancy rate. Insufficient treatment sessions and short duration of the intervention could also have caused the lack of significant difference between the groups. Acupuncture in two included studies14,15 was performed only 20 times over 27 days, whereas other therapies to improve semen quality and spontaneous pregnancy, including clomiphene citrate and antioxidants, were taken daily for 56 days to 6 months.31,32,33,34 Therefore, the treatment period might have been too short to significantly enhance the pregnancy rate of couples. Other factors associated with spontaneous pregnancy might also have led to the nonsignificant pregnancy results. Age of the spouse and duration of infertility are associated with pregnancy rate.35,36 The proportion of sperm with normal morphology is also strongly associated with time to pregnancy.37 Two included studies14,15 did not report any information on these factors and hence there could have been an imbalance in these factors between groups.
All the studies reported no adverse events, but it is uncertain whether acupuncture is a safe treatment for poor semen quality. To reduce publication bias, Ioannidis and Lau38 recommend that authors describe the information on patients who withdrew because of adverse effects. One included study13 mentioned that five patients in the total population discontinued the intervention because of a lack of time. However, the other three studies12,14,15 did not describe why participants withdrew or discontinued during the study. Therefore, there is a possibility of missing data on adverse events. Future clinical trials are required to understand why and when participants withdraw or discontinue.
CONCLUSIONS
This review suggests that current evidence regarding whether acupuncture in infertile men improves sperm motility, sperm concentration, and the pregnancy rate of couples is insufficient. The poor quality of the evidence is attributable to the small number of studies, inadequate procedures and/or insufficient information for semen analysis, high risk of bias, methodological heterogeneity, and poor reporting quality. Large-scale RCTs with elaborate designs are needed to rigorously test the effectiveness and safety of acupuncture on semen quality. Appropriate target populations and sufficient treatment periods should also be considered in future studies.
AUTHOR CONTRIBUTIONS
UMJ and JYJ planned and designed the study, searched for articles from the databases, selected relevant studies, extracted the data, analyzed the data, and drafted the manuscript. SL and JML made substantial contributions to the study design. SL arbitrated contradictory assessments. SL helped to draft the manuscript. SL and OK participated in the critical revision of the manuscript. OK had the final responsibility for the submission decision for publication. All of the authors read and approved the final manuscript.
COMPETING INTERESTS
The authors declare that they have no conflict of interest.
ACKNOWLEDGMENTS
This study was supported by the “New Donguibogam” Compilation Project for the expansion of Korean Medical Knowledge (No. K13380) of the Korea Institute of Oriental Medicine.
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
REFERENCES
- 1.Ng EH, So WS, Gao J, Wong YY, Ho PC. The role of acupuncture in the management of subfertility. Fertil Steril. 2008;90:1–13. doi: 10.1016/j.fertnstert.2008.02.094. [DOI] [PubMed] [Google Scholar]
- 2.Hirsh A. Male subfertility. BMJ. 2003;327:669–72. doi: 10.1136/bmj.327.7416.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tremellen K. Oxidative stress and male infertility – A clinical perspective. Hum Reprod Update. 2008;14:243–58. doi: 10.1093/humupd/dmn004. [DOI] [PubMed] [Google Scholar]
- 4.Jungwirth A, Diemer T, Dohle GR, Giwercman A, Kopa Z, et al. Arnhem: European Association of Urology; 2013. Guidelines on Male Infertility; p. 40. [Google Scholar]
- 5.Ross C, Morriss A, Khairy M, Khalaf Y, Braude P, et al. A systematic review of the effect of oral antioxidants on male infertility. Reprod Biomed Online. 2010;20:711–23. doi: 10.1016/j.rbmo.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Showell MG, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2011;(1):CD007411. doi: 10.1002/14651858.CD007411.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Oldereid NB, Rui H, Purvis K. Male partners in infertile couples. Personal attitudes and contact with the Norwegian health service. Scand J Soc Med. 1990;18:207–11. doi: 10.1177/140349489001800309. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. J Evid Based Med. 2010;3:140–55. doi: 10.1111/j.1756-5391.2010.01086.x. [DOI] [PubMed] [Google Scholar]
- 10.Lun X. Effects of electroacupuncture on nitric oxide and trace elements in patient of male immune infertility. Zhongguo Zhen Jiu. 2004;24:854–6. [Google Scholar]
- 11.Liu L, Yue Z-X, Fu W, Hou Q, He X. Effect of Yu-Zi tang combined with electric acupuncture on seminal plasma zinc in patients with weak sperm. J Mod Clin Med. 2011;37:251–2. [Google Scholar]
- 12.Liu L, Yue ZX, Fu W, Zhang LJ, He X. The effect of Traditional Chinese Drug combined with electric acupuncture on seminal plasma neutral alpha-1, 4 glycosidase enzymes in patients with male infertility due to weak sperm. Chin J Fam Plann Gynecotokology. 2011;3:32–4. [Google Scholar]
- 13.Dieterle S, Li C, Greb R, Bartzsch F, Hatzmann W, et al. A prospective randomized placebo-controlled study of the effect of acupuncture in infertile patients with severe oligoasthenozoospermia. Fertil Steril. 2009;92:1340–3. doi: 10.1016/j.fertnstert.2009.02.041. [DOI] [PubMed] [Google Scholar]
- 14.Wang ZQ, Huang YQ, Liang B. Clinical observation on electroacupuncture and Chinese drug for treatment of oligospermia and asthenospermia of the male infertility patient. Zhongguo Zhen Jiu. 2008;28:805–7. [PubMed] [Google Scholar]
- 15.Shi XF. Effects of acupuncture and traditional Chinese medicinal for oligozoospermia and/or asthenozoospermia in male infertility (Chinese) China Mod Med. 2009;16:115–6. [Google Scholar]
- 16.Leung AY, Park J, Schulteis G, Duann JR, Yaksh T. The electrophysiology of de qi sensations. J Altern Complement Med. 2006;12:743–50. doi: 10.1089/acm.2006.12.743. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. 4th ed. Cambridge: Cambridge University Press; 1999. WHO Laboratory Manual for the Examination and Processing of Human Semen; pp. 4–10. [Google Scholar]
- 18.World Health Organization. 5th ed. Geneva: World Health Organization; 2010. WHO Laboratory Manual for the Examination and Processing of Human Semen; pp. 10–226. [Google Scholar]
- 19.Pei J, Strehler E, Noss U, Abt M, Piomboni P, et al. Quantitative evaluation of spermatozoa ultrastructure after acupuncture treatment for idiopathic male infertility. Fertil Steril. 2005;84:141–7. doi: 10.1016/j.fertnstert.2004.12.056. [DOI] [PubMed] [Google Scholar]
- 20.Gurfinkel E, Cedenho AP, Yamamura Y, Srougi M. Effects of acupuncture and moxa treatment in patients with semen abnormalities. Asian J Androl. 2003;5:345–8. [PubMed] [Google Scholar]
- 21.Siterman S, Eltes F, Wolfson V, Zabludovsky N, Bartoov B. Effect of acupuncture on sperm parameters of males suffering from subfertility related to low sperm quality. Arch Androl. 1997;39:155–61. doi: 10.3109/01485019708987914. [DOI] [PubMed] [Google Scholar]
- 22.Siterman S, Eltes F, Wolfson V, Lederman H, Bartoov B. Does acupuncture treatment affect sperm density in males with very low sperm count? A pilot study. Andrologia. 2000;32:31–9. [PubMed] [Google Scholar]
- 23.Siterman S, Eltes F, Schechter L, Maimon Y, Lederman H, et al. Success of acupuncture treatment in patients with initially low sperm output is associated with a decrease in scrotal skin temperature. Asian J Androl. 2009;11:200–8. doi: 10.1038/aja.2008.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang M, Huang G, Lu F, Paulus WE, Sterzik K. Influence of acupuncture on idiopathic male infertility in assisted reproductive technology. J Huazhong Univ Sci Technolog Med Sci. 2002;22:228–30. doi: 10.1007/BF02828187. [DOI] [PubMed] [Google Scholar]
- 25.Enblom A, Johnsson A, Hammar M, Onelöv E, Steineck G, et al. Acupuncture compared with placebo acupuncture in radiotherapy-induced nausea – A randomized controlled study. Ann Oncol. 2012;23:1353–61. doi: 10.1093/annonc/mdr402. [DOI] [PubMed] [Google Scholar]
- 26.Schneider A, Weiland C, Enck P, Joos S, Streitberger K, et al. Neuroendocrinological effects of acupuncture treatment in patients with irritable bowel syndrome. Complement Ther Med. 2007;15:255–63. doi: 10.1016/j.ctim.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Kong J, Kaptchuk TJ, Polich G, Kirsch I, Vangel M, et al. Expectancy and treatment interactions: a dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage. 2009;45:940–9. doi: 10.1016/j.neuroimage.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colagiuri B, Smith CA. A systematic review of the effect of expectancy on treatment responses to acupuncture. Evid Based Complement Alternat Med 2012. 2012:857804. doi: 10.1155/2012/857804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leushuis E, van der Steeg JW, Steures P, Repping S, Bossuyt PM, et al. Reproducibility and reliability of repeated semen analyses in male partners of subfertile couples. Fertil Steril. 2010;94:2631–5. doi: 10.1016/j.fertnstert.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 30.Clifford TJ, Barrowman NJ, Moher D. Funding source, trial outcome and reporting quality: are they related? Results of a pilot study. BMC Health Serv Res. 2002;2:18. doi: 10.1186/1472-6963-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Závaczki Z, Szöllõsi J, Kiss SA, Koloszár S, Fejes I, et al. Magnesium-orotate supplementation for idiopathic infertile male patients: a randomized, placebo-controlled clinical pilot study. Magnes Res. 2003;16:131–6. [PubMed] [Google Scholar]
- 32.Rolf C, Cooper TG, Yeung CH, Nieschlag E. Antioxidant treatment of patients with asthenozoospermia or moderate oligoasthenozoospermia with high-dose vitamin C and vitamin E: a randomized, placebo-controlled, double-blind study. Hum Reprod. 1999;14:1028–33. doi: 10.1093/humrep/14.4.1028. [DOI] [PubMed] [Google Scholar]
- 33.Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, et al. Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial. Fertil Steril. 2009;91:1785–92. doi: 10.1016/j.fertnstert.2008.02.119. [DOI] [PubMed] [Google Scholar]
- 34.Ghanem H, Shaeer O, El-Segini A. Combination clomiphene citrate and antioxidant therapy for idiopathic male infertility: a randomized controlled trial. Fertil Steril. 2010;93:2232–5. doi: 10.1016/j.fertnstert.2009.01.117. [DOI] [PubMed] [Google Scholar]
- 35.Hunault CC, Habbema JD, Eijkemans MJ, Collins JA, Evers JL, et al. Two new prediction rules for spontaneous pregnancy leading to live birth among subfertile couples, based on the synthesis of three previous models. Hum Reprod. 2004;19:2019–26. doi: 10.1093/humrep/deh365. [DOI] [PubMed] [Google Scholar]
- 36.Sripada S, Townend J, Campbell D, Murdoch L, Mathers E, et al. Relationship between semen parameters and spontaneous pregnancy. Fertil Steril. 2010;94:624–30. doi: 10.1016/j.fertnstert.2009.02.085. [DOI] [PubMed] [Google Scholar]
- 37.Slama R, Eustache F, Ducot B, Jensen TK, Jørgensen N, et al. Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Hum Reprod. 2002;17:503–15. doi: 10.1093/humrep/17.2.503. [DOI] [PubMed] [Google Scholar]
- 38.Ioannidis JP, Lau J. Improving safety reporting from randomised trials. Drug Saf. 2002;25:77–84. doi: 10.2165/00002018-200225020-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SEARCH STRATEGIES
Reporting quality of randomized controlled trials based on the consolidated standard of reporting trials (CONSORT)


