Abstract
Summary:
Mastopexy and reduction mammoplasty share techniques of pedicle formation and skin excision patterns, with the main difference being the amount of breast tissue resected. Various types of excision patterns and orientation of pedicles were developed throughout the years, each with flares of popularity at different times. This article reviews the multiple techniques of pedicle orientation and skin excision patterns separately and gives the advantages and disadvantages of each.
Mastopexy and reduction mammoplasty are similar operations but with further parenchymal resection in reductions and have been described in a great variety of methods. The 2 basic questions are (1) Where is the pedicle oriented? and (2) Which skin resection pattern should I use? The pedicle formation can be independent of the skin pattern chosen (Figs. 1A–C), but some combinations are performed more frequently than others, such as the inferior pedicle inverted T pattern, reasons for which will be elucidated below. The 3 main steps in the procedures are to:
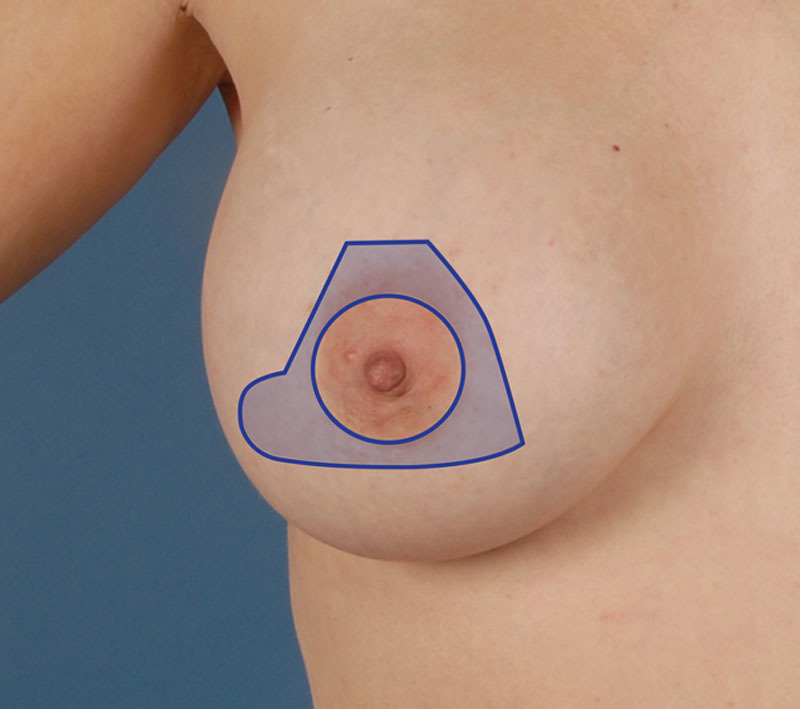
Fig. 1.
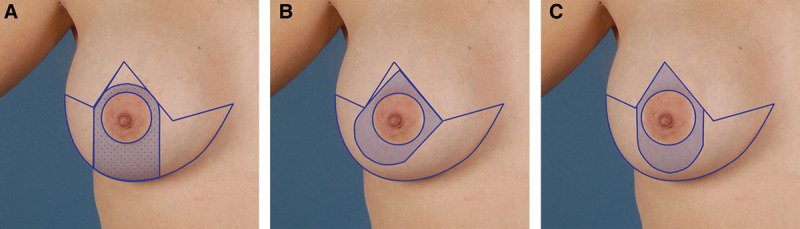
A, Wise (inverted T) pattern, inferior pedicle; B, Wise pattern, superomedial pedicle; and C, Wise pattern, superior pedicle.
resect excessive breast tissue if needed;
excise excessive skin; and
maintain the viability and reposition of the nipple-areolar complex.
The breast receives its vascular supply from the branches of the internal mammary artery, lateral thoracic artery, thoracodorsal artery, intercostal perforators, and thoracoacromial artery, with the largest suppliers being the former two. Innervation of the nipple is by the anterior and lateral cutaneous branches of the third through fifth intercostal nerves, most frequently the fourth lateral cutaneous branch.1 Orientation of the pedicle attempts to maximize both vascularity and sensation to the nipple while optimizing aesthetic outcome. Pedicle formation is balanced between being as wide as possible to maximize vascularity and being narrow enough to allow sufficient tissue reduction.
SUPERIOR PEDICLE
The superior pedicle was described by Weiner et al2 in 1973 and has traditionally been associated with smaller resections, best used in resections of less than 1000 g, as it becomes difficult to inset with larger resections.3 Although not ideal for larger resections, there is a role for the superior pedicle in severely ptotic breasts as it leaves upper-pole fullness and maintains breast projection. It has been demonstrated to be a safe option in women with sternal notch to nipple distances >40 cm.4 A major disadvantage of the superior pedicle technique is the higher risk for sensory loss at the nipple-areolar complex postoperatively.5 This is found to be independent of the amount of tissue resected and is thought to be due to the tissue resection at the base of the breast this pedicle requires. Numbers as high as 70% of women have diminished sensation at the nipple-areolar complex 1 year postoperative with the superior pedicle, irrespective of the amount of tissue resected.6
INFERIOR PEDICLE
Introduced in 1975 by Ribeiro,7 and popularized by Robbins,8 Courtiss and Goldwyn,9 and Georgiade et al,10 the inferior pedicle is very reliable in both viability and retention of sensation.11 It is therefore a strong option for larger resections, having been described in resections as large as 3000 g with no increase in complications compared with smaller resections.12,13 A 3:1 ratio for length:width of pedicle was recommended by Georgiade et al.10 It has similar rates of postoperative lactation as the superior and medial pedicles, around 60% of women, regardless of pedicle choice.14 It has been advocated for use in younger patients given its reliability in maintaining sensation, even in larger resections. In a 2002 American Society for Aesthetic Plastic Surgery survey, 56% of surgeons reported using only the inferior pedicle and inverted T skin pattern.15 A major criticism of the inferior pedicle is the development of the “bottoming out” phenomenon.
CENTRAL MOUND
In this technique, popularized by Hester, 17 thick skin and subcutaneous flaps are dissected off around the nipple, leaving a central mound. Breast tissue is reduced as needed around this central mound (ensuring it does not become too narrow). Nipple-areola viability does not depend on a dermal pedicle, but on the parenchymal circulation.16–18 Vascularity was found to be excellent. In their series of 153 patients, Grant and Rand19 had no nipple losses. Sensation is also well preserved,20 and this technique allows small to large reductions to be carried out.
MEDIAL PEDICLE
The medial pedicle orients its base along the sternal border so that it is based off internal mammary perforators and anteromedial intercostal nerves. The medial pedicle is modified from the superomedial pedicle described by Orlando and Guthrie.21 Nahabedian et al22 modifies the original superomedial pedicle for severe mammary hypertrophy, by narrowing the base and eliminating the superior attachment, therefore allowing a wider arc of rotation. It is a good option in cases of severe mammary hypertrophy with preserved sensation and viability in 94% of patients.23,24 It has been shown to be safe in resections >1500 g, with rates of postoperative lactation similar to inferior and superior pedicle techniques. Importantly, it has not been associated with the same degree of pseudoptosis as the inferior pedicle technique. In resections of 500–1200 g and >1200 g, the medial pedicle technique saw increases of the nipple to inframammary fold distances postoperatively of 11% and 34%, respectively.25 This is in contrast to the inferior pedicle technique, in which prior studies have shown respective increases of nipple to IMF distances of 48% and 72%.26 Many authors including Hall-Findlay3 use the medial pedicle as it was found to be easy to inset and had excellent perfusion and sensation.
LATERAL PEDICLE
The lateral pedicle was originally described by Skoog27 in 1963. Most of the reduction is in the inferior and medial quadrants. Many assert that this procedure is basically a modified Strombeck (horizontal bipedicle) reduction. The lateral pedicle is reliable, allows for breast feeding, and has excellent preservation of sensation at the nipple-areolar complex.28,29 However, it is a less popular technique because it does not allow for optimal shaping, as the dense tissue of the upper outer quadrant cannot be resected with resultant lateral fullness.3
VERTICAL BIPEDICLE
The vertical bipedicle was described by McKissock30 in 1976. Although reliable and aesthetically pleasing, it does have a higher rate of sensation loss when compared with the inferior pedicle. It can also lead to broad breasts although subsequent modifications including narrowing of the pedicle have addressed this problem. Although still used today, it was widely replaced with the introduction of the inferior pedicle.31
HORIZONTAL BIPEDICLE
The horizontal bipedicle, described by Strombeck,32 uses both a medial and a lateral pedicle to supply the nipple-areolar complex. It is safe and reliable, even in resections >1000 g. It was popular in the 1960s, until it began to be largely replaced by McKissock’s vertical bipedicle technique. The Strombeck reduction was criticized on the basis of an awkward nipple inset, difficult maneuvering of the pedicle intraoperatively, and a high rate of loss of nipple sensation.
SKIN EXCISION PATTERNS
Wise (Inverted T) Pattern
This extremely popular technique can be used on most pedicles and is most commonly associated with an inferior pedicle (Figs. 1A–C).33 It is a good option for very large reductions as it allows for the largest amount of skin excision and is the most versatile technique; therefore, it is the best skin pattern for poor-quality skin. It is also useful in correcting severely ptotic breasts. Many surgeons find this pattern to be more predictable and relatively easier to learn/teach. The major disadvantage of the Wise pattern is the high scar burden, so may be a point of consideration in patients who have a tendency for keloid or hypertrophic scarring. It also runs the risk of giving a boxy breast appearance if the medial and lateral incisions do not curve up against the breast enough.34
Vertical Skin Pattern
Vertical skin patterns are more commonly used for smaller reductions and for managing mild to moderate ptosis (Fig. 2). This pattern is usually associated with superior, superomedial, or medial pedicle techniques. Advantages include improved projection for a longer period of time. The glandular reshaping gives a more aesthetic mound as suturing of the medial and lateral pillars narrows the breast and gives the desired projection. Scar burden is reduced and advocates for the vertical pattern maintain that although the scar is on a prominent part of the breast, it fades and does not bother the patient much. It requires good-quality skin with adequate elasticity for remodeling. Disadvantages include a steeper learning curve and the necessity of overcorrection on table. This gives a less aesthetic immediate outcome as it results in “bunched-up” tissue from the vertical incision, and the breast appears overly uplifted. However, as the breast settles over time, it gives a more aesthetic breast compared with the inverted T pattern. Although patients rate the vertical skin pattern higher in the scars and aesthetics scales, it may require more surgical revisions compared with the inverted T pattern.35
Fig. 2.
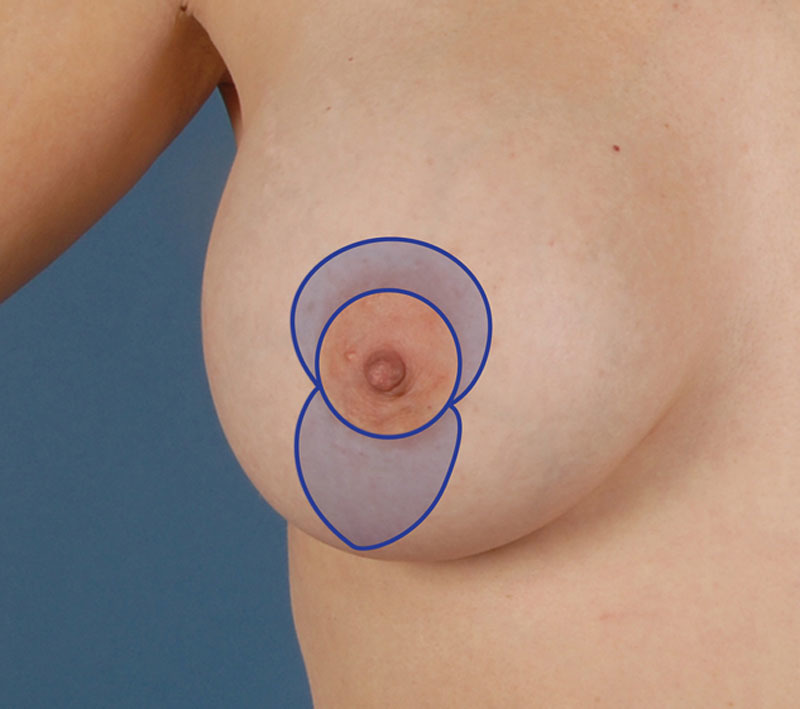
Vertical pattern.
Periareolar Pattern
This approach results in the shortest possible scar pattern (Fig. 3). Movement of the nipple is limited to 2 cm; therefore, only useful in patients with very minor ptosis. This pattern is more for mastopexy as opposed to reduction because minimal or no resection of gland is performed. Benelli36 uses a crisscrossing of pillars for his mastopexy technique, with nonabsorbable suture around the areolar incision. Complaints about this technique include distortion of areola, scar widening, and flattening of the breast. Spear et al37 have developed 3 principles regarding the diameters of the outside, inside, and original circles, which minimize these risks of misshapen areola and poor scars. Additionally, there is a role for the periareolar pattern in explantation patients, who have large areola and minimal ptosis, as this allows reduction of the areolar size.38
Fig. 3.
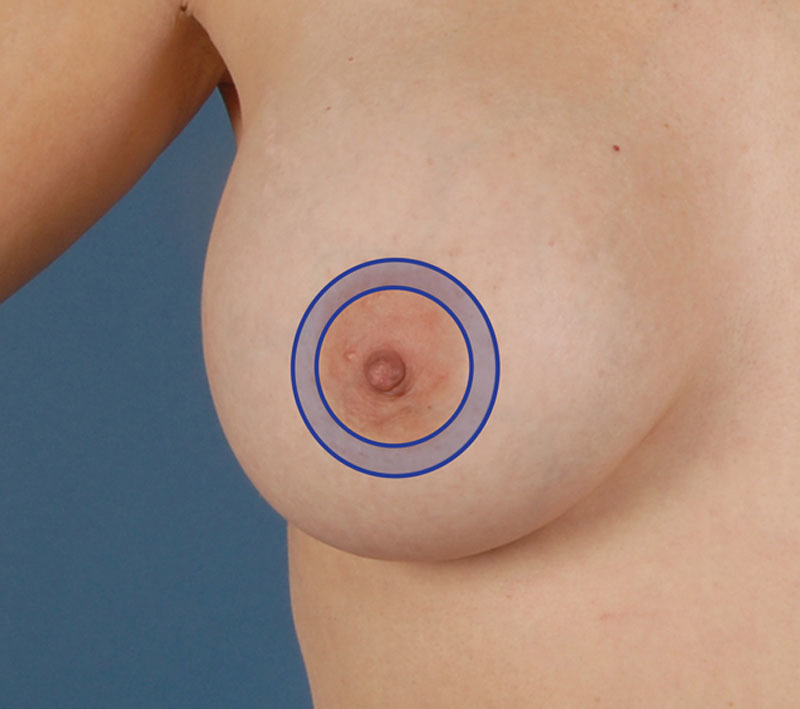
Periareolar pattern.
L-shaped Pattern
This skin pattern eliminates medial limb of inverted T and shortens lateral limb, and it is useful for breasts with ptosis grades I and II. The Regnault B technique (Fig. 4) is derived from a B-shaped incision, involving resection and de-epithelialization, which ends up in an L-shaped wound.39,40 Peranteau and Regnault41 maintain it to be “very adaptable to various deformities and is easy to use. The percent of complications is thought to be no greater than that of other techniques.” Chiari’s42 pattern (Fig. 5) has a triangle based above the inframammary fold, with a lower lateral extension. The incision is based on geometric planning, using key measurements, and involves de-epithelialization of the skin.
Fig. 4.
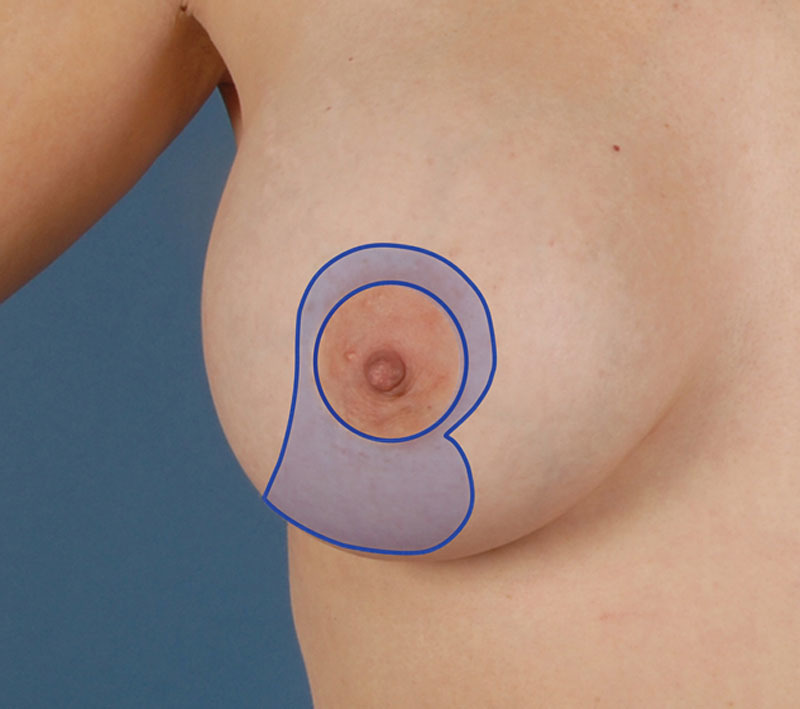
Regnault B technique.
Fig. 5.
Chiari technique.
Short-scar Peri-areolar Inferior Pedicle Reduction (Results in J-shaped Incision)
Described by Hammond,43,44 this skin pattern allows that surgeons are able to perform from simple mastopexies to reductions up to 2000 g (Fig. 6). It overcomes the annoying disadvantage of vertical skin resections of having to overcorrect and waiting for it to settle as it results in an excellent shape immediately. Like other short-scar techniques, it gives a reduced scar burden compared with inverted T pattern. In small reductions up to 500 g, the vertical incision may stop at the inframammary fold. In larger reductions of >500 g, it becomes a J-shaped incision as the resection is carried out laterally along the inframammary fold.
Fig. 6.

J-shaped incision.
DISCUSSION
Reduction mammoplasty is still one of the most gratifying procedures in terms of patient satisfaction.45–48 As demonstrated, there is a multitude of variations of this procedure, and many a time, one could use a couple of different ways to achieve roughly the same thing. Main considerations are the size of reduction needed and the comfort level of the surgeon performing the procedure. Ideally, each patient case should have the specific reduction technique individualized to their needs, but as demonstrated by the 2002 ASAPS survey, more than half the surgeons reported using only the inferior pedicle and inverted T skin pattern,15 so this is not always possible. Mastopexy patients are likely to have greater aesthetic concerns compared with reduction patients; therefore, scar placement will have greater emphasis in these cases. Breasts to be reduced or pexied come in a great variety of sizes, shapes, and skin quality, so plastic surgery trainees should learn at least a few of these techniques so as to be able to tailor the operation required to optimize patient results.
Footnotes
Disclosure: Dr. Rohrich receives instrument royalties from Micrins Instruments and book royalties from Quality Medical Publishing. The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Schlenz I, Kuzbari R, Gruber H, et al. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105:905–909. doi: 10.1097/00006534-200003000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Weiner DL, Aiache AE, Silver L, et al. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty, or mastopexy. Plast Reconstr Surg. 1973;51:115–120. doi: 10.1097/00006534-197302000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29:379–391. doi: 10.1016/s0094-1298(02)00008-1. [DOI] [PubMed] [Google Scholar]
- 4.Wettstein R, Christofides E, Pittet B, et al. Superior pedicle breast reduction for hypertrophy with massive ptosis. J Plast Reconstr Aesthet Surg. 2011;64:500–507. doi: 10.1016/j.bjps.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Chiummariello S, Angelisanti M, Arleo S, et al. Evaluation of the sensitivity after reduction mammoplasty. Our experience and review of the literature. Ann Ital Chir. 2013;84:385–388. [PubMed] [Google Scholar]
- 6.Schlenz I, Rigel S, Schemper M, et al. Alteration of nipple and areola sensitivity by reduction mammaplasty: a prospective comparison of five techniques. Plast Reconstr Surg. 2005;115:743–751; discussion 752–754. doi: 10.1097/01.prs.0000152435.03538.43. [DOI] [PubMed] [Google Scholar]
- 7.Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55:330–334. [PubMed] [Google Scholar]
- 8.Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59:64–67. doi: 10.1097/00006534-197701000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500–507. [PubMed] [Google Scholar]
- 10.Georgiade NG, Serafin D, Morris R, et al. Reduction mammaplasty utilizing an inferior pedicle nipple-areolar flap. Ann Plast Surg. 1979;3:211–218. doi: 10.1097/00000637-197909000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Sandsmark M, Amland PF, Abyholm F, et al. Reduction mammaplasty. A comparative study of the Orlando and Robbins methods in 292 patients. Scand J Plast Reconstr Surg Hand Surg. 1992;26:203–209. doi: 10.3109/02844319209016013. [DOI] [PubMed] [Google Scholar]
- 12.Chang P, Shaaban AF, Canady JW, et al. Reduction mammaplasty: the results of avoiding nipple-areolar amputation in cases of extreme hypertrophy. Ann Plast Surg. 1996;37:585–591. [PubMed] [Google Scholar]
- 13.O’Grady KF, Thoma A, Dal Cin A. A comparison of complication rates in large and small inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2005;115:736–742. doi: 10.1097/01.prs.0000152428.43300.19. [DOI] [PubMed] [Google Scholar]
- 14.Cruz NI, Korchin L. Lactational performance after breast reduction with different pedicles. Plast Reconstr Surg. 2007;120:35–40. doi: 10.1097/01.prs.0000263371.37596.49. [DOI] [PubMed] [Google Scholar]
- 15.Rohrich RJ, Gosman AA, Brown SA, et al. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114:1724–1733; discussion 1734–1736. doi: 10.1097/01.prs.0000142480.27748.9e. [DOI] [PubMed] [Google Scholar]
- 16.Balch CR. The central mound technique for reduction mammaplasty. Plast Reconstr Surg. 1981;67:305–311. doi: 10.1097/00006534-198103000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Hester TR, Jr, Bostwick J, III, Miller L, et al. Breast reduction utilizing the maximally vascularized central breast pedicle. Plast Reconstr Surg. 1985;76:890–900. doi: 10.1097/00006534-198512000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Hester TR, Jr, Cukic J. Central breast pedicle and “free-hand” technique for alteration of volume and skin envelope of the breast. Clin Plast Surg. 1988;15:613–625. [PubMed] [Google Scholar]
- 19.Grant JH, III, Rand RP. The maximally vascularized central pedicle breast reduction: evolution of a technique. Ann Plast Surg. 2001;46:584–589. doi: 10.1097/00000637-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Hagerty RC, Nowicky DJ. Integration of the central mound technique with the vertical skin takeout reduction mammaplasty. Plast Reconstr Surg. 1998;102:1182–1187. doi: 10.1097/00006534-199809040-00042. [DOI] [PubMed] [Google Scholar]
- 21.Orlando JC, Guthrie RH., Jr The superomedial dermal pedicle for nipple transposition. Br J Plast Surg. 1975;28:42–45. doi: 10.1016/s0007-1226(75)90149-6. [DOI] [PubMed] [Google Scholar]
- 22.Nahabedian MY, McGibbon BM, Manson PN. Medial pedicle reduction mammaplasty for severe mammary hypertrophy. Plast Reconstr Surg. 2000;105:896–904. doi: 10.1097/00006534-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Mofid MM, Dellon AL, Elias JJ, et al. Quantitation of breast sensibility following reduction mammaplasty: a comparison of inferior and medial pedicle techniques. Plast Reconstr Surg. 2002;109:2283–2288. doi: 10.1097/00006534-200206000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Nahabedian MY, Mofid MM. Viability and sensation of the nipple-areolar complex after reduction mammaplasty. Ann Plast Surg. 2002;49:24–31; discussion 31–32. doi: 10.1097/00000637-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Abramson DL, Pap S, Shifteh S, et al. Improving long-term breast shape with the medial pedicle wise pattern breast reduction. Plast Reconstr Surg. 2005;115:1937–1943. doi: 10.1097/01.prs.0000165085.23537.a7. [DOI] [PubMed] [Google Scholar]
- 26.Reus WF, Mathes SJ. Preservation of projection after reduction mammaplasty: long-term follow-up of the inferior pedicle technique. Plast Reconstr Surg. 1988;82:644–652. doi: 10.1097/00006534-198810000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Skoog T. A technique of breast reduction; transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453–465. [PubMed] [Google Scholar]
- 28.Hefter W, Lindholm P, Elvenes OP. Lactation and breast-feeding ability following lateral pedicle mammaplasty. Br J Plast Surg. 2003;56:746–751. doi: 10.1016/s0007-1226(03)00368-0. [DOI] [PubMed] [Google Scholar]
- 29.Hamdi M, Blondeel P, Van de Sijpe K, et al. Evaluation of nipple-areola complex sensitivity after the latero-central glandular pedicle technique in breast reduction. Br J Plast Surg. 2003;56:360–364. doi: 10.1016/s0007-1226(03)00190-5. [DOI] [PubMed] [Google Scholar]
- 30.McKissock PK. Reduction mammaplasty by the vertical bipedicle flap technique. Rationale and results. Clin Plast Surg. 1976;3:309–320. [PubMed] [Google Scholar]
- 31.Ramon Y, Sharony Z, Moscona RA, et al. Evaluation and comparison of aesthetic results and patient satisfaction with bilateral breast reduction using the inferior pedicle and McKissock’s vertical bipedicle dermal flap techniques. Plast Reconstr Surg. 2000;106:289–295; discussion 295–297. doi: 10.1097/00006534-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Strombeck JO. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79–90. doi: 10.1016/s0007-1226(60)80014-8. [DOI] [PubMed] [Google Scholar]
- 33.Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17:367–375. doi: 10.1097/00006534-195605000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Hidalgo DA. Improving safety and aesthetic results in inverted T scar breast reduction. Plast Reconstr Surg. 1999;103:874–886; discussion 887–889. [PubMed] [Google Scholar]
- 35.Cruz-Korchin N, Korchin L. Vertical versus Wise pattern breast reduction: patient satisfaction, revision rates, and complications. Plast Reconstr Surg. 2003;112:1573–1578; discussion 1579–1581. doi: 10.1097/01.PRS.0000086736.61832.33. [DOI] [PubMed] [Google Scholar]
- 36.Benelli L. A new periareolar mammaplasty: the “round block” technique. Aesthetic Plast Surg. 1990;14:93–100. doi: 10.1007/BF01578332. [DOI] [PubMed] [Google Scholar]
- 37.Spear SL, Kassan M, Little JW. Guidelines in concentric mastopexy. Plast Reconstr Surg. 1990;85:961–966. doi: 10.1097/00006534-199006000-00023. [DOI] [PubMed] [Google Scholar]
- 38.Rohrich RJ, Beran SJ, Restifo RJ, et al. Aesthetic management of the breast following explantation: evaluation and mastopexy options. Plast Reconstr Surg. 1998;101:827–837. doi: 10.1097/00006534-199803000-00039. [DOI] [PubMed] [Google Scholar]
- 39.Regnault P. Breast reduction: B technique. Plast Reconstr Surg. 1980;65:840–845. doi: 10.1097/00006534-198006000-00023. [DOI] [PubMed] [Google Scholar]
- 40.Regnault P. Breast reduction and mastopexy, an old love story: B technique update. Aesthetic Plast Surg. 1990;14:101–106. doi: 10.1007/BF01578333. [DOI] [PubMed] [Google Scholar]
- 41.Parenteau JM, Regnault P. The Regnault “B” technique in mastopexy and breast reduction: a 12-year review. Aesthetic Plast Surg. 1989;13:75–79. doi: 10.1007/BF01571472. [DOI] [PubMed] [Google Scholar]
- 42.Chiari A., Jr The L short-scar mammaplasty. Clin Plast Surg. 2002;29:401–409, vi. doi: 10.1016/s0094-1298(02)00004-4. [DOI] [PubMed] [Google Scholar]
- 43.Hammond DC. The short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Semin Plast Surg. 2004;18:231–243. doi: 10.1055/s-2004-831910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hammond DC. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103:890–901; discussion 902. doi: 10.1007/3-540-27218-6_6. [DOI] [PubMed] [Google Scholar]
- 45.Serletti JM, Reading G, Caldwell E, et al. Long-term patient satisfaction following reduction mammoplasty. Ann Plast Surg. 1992;28:363–365. doi: 10.1097/00000637-199204000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Boschert MT, Barone CM, Puckett CL. Outcome analysis of reduction mammaplasty. Plast Reconstr Surg. 1996;98:451–454. doi: 10.1097/00006534-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Brühlmann Y, Tschopp H. Breast reduction improves symptoms of macromastia and has a long-lasting effect. Ann Plast Surg. 1998;41:240–245. doi: 10.1097/00000637-199809000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Spector JA, Karp NS. Reduction mammaplasty: a significant improvement at any size. Plast Reconstr Surg. 2007;120:845–850. doi: 10.1097/01.prs.0000277660.49802.76. [DOI] [PubMed] [Google Scholar]


