Abstract
After preliminary assessment of virulence in AKR/J, DBA/1, BALB/c, and C57BL/6 mice, we investigated histopathologic changes in BALB/c and C57BL/6 mice infected with type A (strain SCHU S4) or type B (strain 425) Francisella tularensis by aerosol exposure. In mice exposed to type A infection, changes in histologic presentation were not apparent until day 3 after infection, when pyogranulomatous inflammation was detected in spleens and livers of BALB/c mice, and in lungs and spleens of C57BL/6 mice. Histopathologic changes were most severe and widespread in both mouse strains on day 5 after infection and seemed to completely resolve within 22 d of challenge. BALB/c mice were more resistant than C57BL/6 mice in lethal-dose calculations, but C57BL/6 mice cleared the infection more rapidly. Mice similarly challenged with type B F. tularensis also developed histopathologic signs of infection beginning on day 3. The most severe changes were noted on day 8 and were characterized by granulomatous or pyogranulomatous infiltrations of the lungs. Unlike type A infection, lesions due to type B did not resolve over time and remained 3 wk after infection. In type B, but not type A, infection we noted extensive inflammation of the heart muscle. Although no microorganisms were found in tissues of type A survivors beyond 9 d after infection, mice surviving strain 425 infection had a low level of residual infection at 3 wk after challenge. The histopathologic presentation of tularemia caused by F. tularensis types A and B in BALB/c and C57BL/6 mice bears distinct similarities to tularemia in humans.
Abbreviations: LVS, live vaccine strain; SUBLN, submandibular lymph node; MESLN, mesenteric lymph node
Tularemia is an infectious disease caused by the gram-negative bacterium Francisella tularensis. Clinical disease was first seen in Japan in 1837, when people who ate meat from rabbits developed fever, chills, and glandular tumors.27 In the United States, the disease was first described in 1911 by Dr Edward Francis, who observed a plague-like illness in ground squirrels. In 1914, the first human case in the United States was described in a butcher.48 Dr Francis, for whom the microorganism was named, characterized the clinical signs, symptoms, and the mode of transmission after infection.
Tularemia is one of the most pathogenic diseases known, causing disease after inoculation or inhalation of as few as 10 microorganisms.27 The microorganism is infectious by many routes, including ingestion of contaminated food or water, through microabrasions or bites from various arthropods, or inhalation of the infectious agent. The species F. tularensis includes several subspecies including tularensis, holarctica, novidia, and mediaasiatica. The type A F. tularensis subspecies tularensis is highly virulent in humans and is the dominant species in North America. Type B F. tularensis subspecies holarctica (also called palearctica) is usually found in European countries and is less virulent.45 Humans infected with either subspecies can develop an acute febrile illness.
F. tularensis is a facultative intracellular pathogen and multiplies in macrophages. Target organs are associated with the reticuloendothelial system and include lymph nodes, lungs, spleen, liver, and kidneys. In human pneumonic tularemia, infection progresses systemically from the lungs to other organs and causes pathologic changes, primarily to the liver and spleen.9,11,19,38 Humans infected by aerosol exposure also show hemorrhagic inflammation of the airways, which can progress to bronchopneumonia.43 Alveolar spaces become filled with a mononuclear cell infiltrate. Pleuritis with adhesions and effusion and hilar lymphadenopathy are commonly found.33 The fatality rate for untreated pneumonic infections is approximately 30% to 60% for type A F. tularensis and approximately 10% for infections with type B F. tularensis.42 Because of its high infectivity, morbidity, and mortality, this microorganism is classified as a Category A Select Agent. F. tularensis can cause natural infections in a variety of animals, including rabbits, cats, prairie dogs, voles, raccoons, squirrels, rats, lemmings, wild mice, and other species.1,3,4,12,30,35,40,49 Although the source of infection can be inapparent, outdoor-housed rhesus macaques can acquire tularemia.15,37
Animal models using virulent (for humans) strains are essential for the development of efficacious vaccines and evaluation of antimicrobials against pathogenic diseases affecting humans. Due to the virulence of this microorganism, most experimental infections in rodent model systems use the Live Vaccine Strain (LVS) to minimize the risk to laboratory workers,17 although many recent studies use the more virulent type B and type A strains. LVS can be lethal to mice but is attenuated in humans. LVS is lethal in naïve mice and causes pathologic reactions similar to those seen with virulent strains in humans.8 However, using an LVS model of infection is not without potential problems. First, dose lethality varies widely, depending on the route of LVS infection. Naïve mice are most sensitive to intraperitoneal challenge, followed by intravenous, intranasal, aerosol, and intradermal challenge. Furthermore, the LD50 for LVS administered by aerosol is greater than 103 microorganisms, whereas the LD50 for virulent F. tularensis strains is less than 10 microorganisms.8
To better understand the pathogenesis of this important Category A pathogen, we determined the virulence and investigated the histopathogenesis of type A and type B F. tularensis in mice challenged by small-particle aerosol. We compared the histopathogenesis of infection over a period of 3 wk in BALB/c and C57BL/6 mice challenged with 1468 microorganisms or 100 microorganisms of F. tularensis SCHU S4 (type A). Type B (strain 425) infection was similarly investigated in BALB/c mice challenged with 102 microorganisms. Bacterial burdens in spleens, livers, lungs, and blood were determined.
Materials and Methods
Microorganisms.
Type A F. tularensis strain SCHU S4 was obtained from an archived culture collection (Diagnostic Systems Division, USAMRIID). Initial testing in BALB/c mice demonstrated that the virulence of SCHU S4 via aerosol was lower than expected (LD50 approximately 1660 microorganisms). Therefore, this strain was passed through a single mouse and reisolated from the spleen, propagated overnight in Mueller Hinton II broth (Difco, Detroit, MI) containing 2% Isovitalex (Becton Dickinson, Franklin Lakes, NJ), and microorganisms were collected by centrifugation and frozen (−70 °C) in 20% glycerol as a stock culture for use in this and other experiments. This strain was designated FT4 in our archive. Prior to use in infectious aerosol, Mueller Hinton II broth was inoculated with stock culture and incubated overnight in a shaking incubator at 37 °C. Prior to whole-body aerosol infection, the microorganisms were adjusted to the appropriate concentration according to optical density (660 nm) and confirmed by plate counts. This bacterial strain has been widely used in studies of bacterial pathogenesis and countermeasure evaluation10,13,28,31 and has been sequenced.22
Type B F. tularensis strain 425 was obtained from an archived culture collection (Diagnostic Systems Division, USAMRIID). Due to its uncertain history regarding in vitro passage, this strain was passed through a single mouse, reisolated, propagated overnight, and stored at −70 °C in 20% glycerol. This strain was designated FT15 in our archive. Strain 425 was previously used in pathogenesis studies and was the only type B virulent strain available to us.39
Microorganisms were administered to mice via small-particle aerosol as described.36 The aerosol stream was passed through culture medium in all-glass impingers. Doses were calculated by using the concentrations of bacteria in the culture medium and typical respiratory volumes of mice of similar weights.
LD50 determination.
Female mice (10 mice per group; age, 6 to 8 wk) of the strains AKR/J (H-2k, Jackson Laboratory, Bar Harbor, ME), DBA/1J (H-2q, Harlan Laboratories, Indianapolis, IN), BALB/c (H-2d), and C57BL/6 (H-2b, both strains from Charles River–NCI, Fort Detrick, MD) were exposed by small-particle aerosol (diameter, 1 to 5 µm) to log dilutions of the SCHU S4 strain. Mice were monitored twice daily to observe clinical condition, record deaths, and ensure that moribund mice were identified and euthanized by using CO2 (gaseous) followed by cervical dislocation or thoracotomy to conform with AVMA guidelines.24 Euthanized mice were included in the daily tally. Three weeks after aerosol challenge, surviving mice were euthanized. The LD50 for each mouse strain was determined by probit analysis.16 The LD50 of F. tularensis strain 425 was determined similarly in 6- to 8-wk-old female BALB/c mice.
Histopathogenesis study.
BALB/c and C57BL/6 female mice (age, 6 to 8 wk) were infected with type A F. tularensis SCHU S4 (1468 microorganisms; 5 LD50 BALB/c; 17 LD50 C57BL/6).36 Beginning at 4 h and on days 1, 2, 3, 5, 6, and 22 after aerosol exposure, 4 BALB/c and 4 C57BL/6 mice were euthanized with CO2. At each time point, one uninfected control mouse of each mouse strain was euthanized also. Due to the high type A challenge dose, few mice survived beyond 1 wk. To examine the histopathogenesis of type A infection at later time points, a second cohort of BALB/c and C57BL/6 was challenged by using a lower infectious dose (100 microorganisms; 0.3 LD50 BALB/c; 1 LD50 C57BL/6). Mice were euthanized on days 6, 9, 12, 15, and 20 after challenge.
BALB/c female mice (age, 6 to 8 wk) were infected with type B F. tularensis strain 425 (102 microorganisms; 1 LD50) by infectious aerosol. Beginning 6 h after exposure and on days 2, 3, 6, 8, 12, 15, and 20, 4 mice (plus 1 control mouse) were euthanized by using CO2.
Infected mice were monitored twice daily to remove dead mice and ensure that moribund mice were identified and euthanized. Only euthanized mice were used in this study.
Spleens, livers, and lungs were excised from infected mice and weighed. Sections of the tissue used for bacterial counting were weighed and dissociated in 5 mL HBSS by mechanical disruption in a tissue grinder and plated at dilutions of 10−1, 10−2, and 10−3 (or other dilutions, as required) on Modified Thayer Martin culture plates. Plates were incubated at 37 °C for 5 d, and the concentration of bacteria in the original tissue suspensions was calculated. The number of bacteria present in spleens, livers, and lungs was then calculated. Heart blood (0.1 mL) was obtained from euthanized mice and plated on Modified Thayer Martin agar plates. The number of bacteria present in 1 mL of blood was then calculated.
Fixed samples of all major organs and tissues from each mouse were routinely processed as previously described.18 Tissues examined histopathologically included nasal cavity, oropharyngeal cavity, eye, haired skin, pituitary gland, brain, inner ear, middle ear, external ear canal, esophagus, mediastinal lymph node, lung, heart, trachea, thyroid gland, thymus, gall bladder, pancreas, liver, spleen, stomach, mesenteric lymph node, small intestine, large intestine, kidney, adrenal gland, urinary bladder, uterus, oviduct, ovary, salivary gland, submandubular lymph node, and mammary gland.
Husbandry.
Mice were obtained from Jackson Laboratory, Bar Harbor, ME, Harlan Laboratories, Indianapolis, IN, and from Charles River – NCI, Ft. Detrick, MD and were SPF, signifying that environmental samples from rodent production rooms were evaluated by PCR assay for a variety of known murine pathogens.6 In addition, groups of animals in the production facility were routinely serologically tested by the supplier for pathogens known to adversely affect the heath of mice, including mouse hepatitis virus, murine norovirus, mouse parvovirus, mouse polio virus, mouse rotavirus, ectromelia virus, mouse cytomegalovirus, mouse pneumonitis virus, polyoma virus, and lactate dehydrogenase elevating virus.
Mice were housed at 10 per cage, maintained on a 12:12-h light:dark cycle, and were provided food and water ad libitum. Anesthesia and analgesia were not given in these studies. BALB/c and C57BL/6 mice have previously been used in experiments involving F. tularensis.19
Results
Virulence of F. tularensis in mice.
We assessed the relative virulence of F. tularensis type A (strain SCHU S4) and type B (strain 425) by determining the aerosol LD50 in different strains of mice. The LD50s of F. tularensis SCHU S4 in AKR/J, DBA/1, BALB/c, and C57BL/6 mice were calculated as 79, 801, 308, and 88 microorganisms, respectively. The LD50 of F. tularensis strain 425 in BALB/c mice was 102 microorganisms.
F. tularensis in tissues and blood.
In BALB/c and C57BL/6 mice given the high-count challenge with type A organisms, no tissues were found to be infected at 4 h after challenge. However, on days 1 and 2 after challenge, we noted increasing numbers of microorganisms in the lungs, reaching approximately 3 × 105 microorganisms per lung in both mouse species, but no microorganisms were detected in the spleens, livers, or blood. By day 3, microorganisms were present in all tissues examined, including blood. On day 6, spleens, livers, and lungs of all BALB/c mice were heavily infected. In BALB/c mice, spleens and livers an average of approximately 107 microorganisms, and approximately 106 microorganisms were found in lungs. Blood contained approximately 104 microorganisms per milliliter. The highest numbers of microorganisms were found in tissues of C57BL/6 mice on day 3 of infection, when an average of approximately 4 × 104, 2 × 105, and 1 × 106 microorganisms were found in spleens, livers, and lungs, respectively. Three of the 4 C57BL/6 mice at this time point were infected. On day 6, microorganisms were cultured from the spleen, liver, and lungs of a single C57BL/6 mouse. No residual microorganisms were noted in tissues from the BALB/c and C57BL/6 mice obtained from days 9 through 22 after infection (one mouse from each mouse strain on day 22).
In mice given the low-challenge dose of type A F. tularensis, low levels of infection (approximately 107 microorganisms in spleens and liver; 106 microorganisms in lungs) were present in 3 of 4 BALB/c mice on day 6, but all C57BL/6 tissues were sterile. All examined tissues from both mouse species were sterile on days 9, 12, 15, and 20 after challenge. We did not observe bacteremia at any time point.
In BALB/c mice challenged with type B microorganisms, we initially detected approximately 105 microorganisms per lung in all mice on day 3 of infection. On day 6, all mice had evidence of bacteremia. On day 8, all tissues examined were heavily infected (approximately 6 × 106 microorganisms per spleen, 6 × 107 microorganisms per liver, and 2 × 107 microorganisms per lung), including blood (approximately 6 × 105 microorganisms per mL). On day 12, all tissues from 2 mice remained infected, although bacterial counts were approximately 1 log lower per tissue than was measured on day 8. Spleens and livers from the other 2 mice had no culturable bacteria, but the lungs were not sterile. All mice at this time point were bacteremic. On day 15, all tissues were sterile, including blood, but 2 of 4 lungs were lightly infected (<2 × 106 microorganisms per lung). At the last time point, day 20, examined tissues from all mice were lightly infected (fewer than 6 × 103 microorganisms per tissue), but no microorganisms were found in blood.
Histopathogenesis.
Type A.
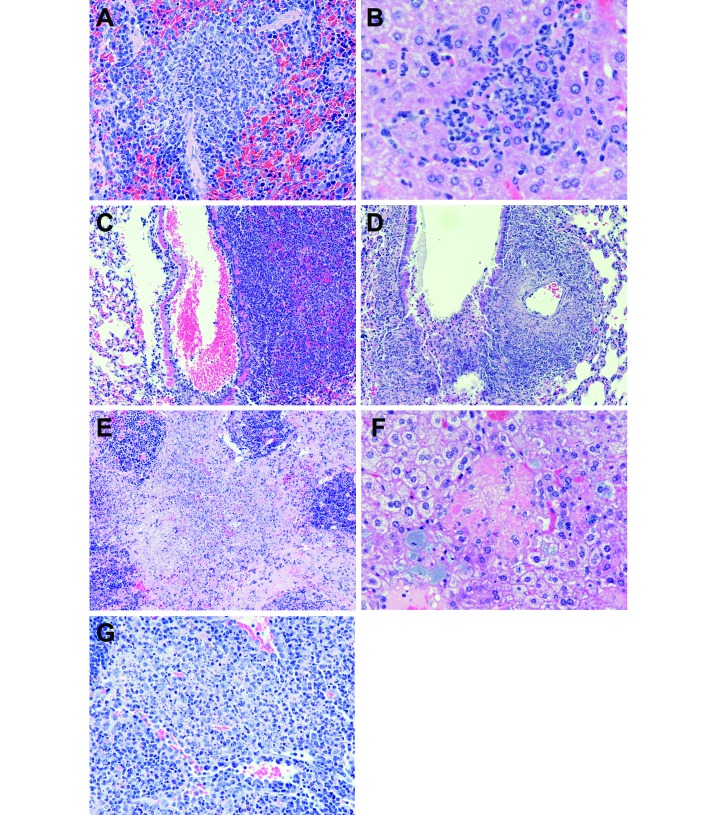
In the first study (mice given 1468 microorganisms of type A F. tularensis), we found no evidence of infection until day 3 after challenge. On day 3, 2 of 4 mice from each mouse strain showed histologic evidence of infection (Tables 1 and 2). In BALB/c mice, sites of infection on day 3 included the spleen (Figure 1 A) and liver (Figure 1 B). The liver of one mouse showed mild leukocyte necrosis, whereas the other demonstrated mild hepatocellular degeneration and necrosis. In C57BL/6 mice, sites of infection included the lung (Figure 1 C) and spleen. The histologic character of inflammation in the tissues from both mouse strains was pyogranulomatous (approximately equal numbers of macrophages and neutrophils). Although no bacilli were evident, given our previous experience that F. tularensis can be difficult to visualize in routine histologic sections, we believe that bacilli are within these lesions.
Table 1.
Presence of histopathologic changes in BALB/c mice (n = 4, except day 22 [n = 1])) after aerosol exposure to a high dose of type A F. tularensis
| Evidence of infection | Bone marrow | Lymph nodes |
|||||||
| Lung | Spleen | Liver | Mediastinum | Mediastinal | Sublingual | Mesenteric | |||
| Day 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 3 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 |
| Day 5 | 4 | 2 | 1 | 4 | 4 | 4 | 1 | 0a | 0 |
| Day 6 | 4 | 3 | 3 | 4 | 4 | 0 | 0 | 1 | 0b |
| Day 22 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Data are given as the number of mice affected.
n = 3
n = 1
Table 2.
Presence of histopathologic changes in C57BL/6 mice (n = 4, except day 22 [n = 1]) after aerosol exposure to a high dose of type A F. tularensis
| Evidence of infection | Bone marrow | Lymph nodes |
||||||
| Lung | Spleen | Liver | Mediastinum | Sublingual | Mesenteric | |||
| Day 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 3 | 2 | 0 | 2 | 1 | 0 | 0 | 0 | 0 |
| Day 5 | 4 | 4 | 4 | 4 | 4 | 1 | 4 | 2 |
| Day 6 | 1 | 1 | 0 | 1 | 1 | 0 | 1a | not done |
| Day 22 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Data are given as the number of mice affected.
n = 3
Figure 1.
(A) Spleen from a BALB/c mouse (no. 060231) d after aerosol infection with Francisella tularensis type A. There is a focus of pyogranulomatous inflammation (equal numbers of macrophages and neutrophils) present in the red pulp. Original magnification, 40 ×. (B) Liver from a BALB/c mouse (no. 060231) 3 d after aerosol infection with Francisella tularensis type A. There is a focus of pyogranulomatous inflammation (equal numbers of macrophages and neutrophils) with a few degenerated hepatocytes, evidenced by their bright pink cytoplasm. Original magnification, 60×. (C) Lung from a C57BL/6 mouse (no. 060239) 3 d after aerosol infection with Francisella tularensis type A. There is an area of pneumonia to the right of a blood-filled (artifact) bronchiole, and it is evident that inflammatory cells have invaded the wall of the bronchiole. There is relatively normal lung to the left of the bronchiole. Original magnification, 20×. (D) Lung from a C57BL/6 mouse (no. 060247) 5 d after aerosol infection with Francisella tularensis type A. This field is similar to that in panel C. Note the necrosis of most of the inflammatory cells at this time point. Original magnification, 20×. (E) Spleen from a C57BL/6 mouse (no. 060248) 5 d after aerosol infection with Francisella tularensis type A. Most of the red pulp of this spleen is filled with necrotic inflammatory cells and fibrin (pink material). The blue cellular clusters are remnants of white pulp that has been markedly depleted. Original magnification, 40 ×. (F) Liver from a C57BL/6 mouse (no. 060248) 5 d after aerosol infection with Francisella tularensis type A. Centrally is a group of necrotic hepatocytes with no evidence of attending inflammatory cells. Surrounding this focus, note enlarged cells with blue granular cytoplasm. These are Kupffer cells (and possibly some hepatocytes) that contain Francisella. Original magnification, 40×. (G) Submandibular lymph node from a C57BL/6 mouse (no. 060246) 3 d after aerosol infection with Francisella tularensis type A. There are coalescing foci of inflammation in this lymph node and the inflammation is comprised mostly of macrophages. Many of the macrophages are necrotic as evidenced by the blue nuclear debris. Original magnification, 40×.
Histopathologic changes were most severe and most widespread in both mouse strains on day 5 after infection (Tables 1 and 2). We noted the first evidence of inflammation of small areas of bone marrow of the head in 2 of 4 BALB/c mice and in all 4 C57BL/6 mice. All mice had lesions in the maxillary bone, whereas one C57BL/6 mouse also had lesions in the calvaria (brain case). The bone marrow of the maxilla of 2 BALB/c mice had an acute, mild to moderate necrotizing inflammatory cell infiltrate. In one mouse, we noted a multifocal moderate necrotizing pyogranulomatous inflammation. Inflammation was present in the lung of 1 of the 4 BALB/c (a mild, multifocal necrotizing pyogranulomatous pneumonia) and in all 4 C57BL/6 mice. At this time point, the inflammation had become necrotizing (Figures 1 D through F), meaning that many of the inflammatory cells were dead and lytic, most likely due to leukocytic enzymes or bacterial toxic products. Of interest is the extension of inflammation in 2 of 4 C57BL/6 mice from areas of pneumonia in the alveoli completely into the walls of adjacent bronchioles (Figure 1 D), sometimes causing ulceration of these bronchioles. The mediastinal tissue surrounding the lungs had pyogranulomatous inflammation in all 4 BALB/c mice but only one C57BL/6 mouse. The infiltrate was necrotizing and pyogranulomatous in nature and mild to moderate in severity.
By day 5 of infection, histologic changes in the spleens were more severe than were changes observed on day 3 (Figure 1 E). All BALB/c and C57BL/6 mice had histologic changes in the spleens. There was a moderate to marked pyogranulomatous infiltrate in the red pulp, and this inflammation was necrotizing in 3 of the 4 BALB/c mice. Likewise, the livers of all mice had involvement at day 5. Whereas the principle lesion on day 3 in BALB/c mice was inflammation accompanied by devitalized hepatocytes (Figure 1 B), the principle lesion on day 5 contained degenerated or dead hepatocytes, with accompanying inflammation of lesser severity (Figure 1 F). Small clusters of bacilli were frequently evident, always within host cells (Figure 1 F). Although some of the host cells resembled hepatocytes, most, if not all, are likely Kupffer cells, resident macrophages lining the sinuses. On day 5, there was involvement of the submandibular lymph nodes in all 4 C57BL/6 mice and of the mesenteric lymph nodes in 2 of the 4 C57BL/6 mice, while there was no involvement of either tissue in BALB/c mice. The character of inflammation differed between mesenteric lymph nodes and other tissues. Inflammation in other tissues was characteristically pyogranulomatous but was characteristically granulomatous (mostly macrophages with few or no neutrophils) in mesenteric lymph nodes (Figure 1 G).
On day 6 after infection with the type A strain, the primary difference noted between the mouse strains was in numbers of mice from each strain with histologic evidence of infection. The numbers of histologically affected mice from each strain was approximately equal at previous time points. However, on day 6, histopathologic evidence of infection was decreasing in C57BL/6 mice but constant in BALB/c mice. On day 6, we noted that all 4 BALB/c mice as compared with one of the 4 C57BL/6 mice had histologic changes (Tables 1 and 2). We hypothesize that increasing numbers of C57BL/6 mice without histologic changes is suggestive that they were able to clear the infection, a feature that can be difficult to determine histologically. In general, after bacterial infection, tissues such as lung and liver can have a great deal of lymphoid tissue in them, but in 3 of the 4 C57BL/6 mice, there was no such evidence. Otherwise, there was very little qualitative difference between mice of both strains that did have histologic evidence of infection at 6 d after infection. Whereas there was lung involvement in all 4 C57BL/6 and only one of the 4 BALB/c mice on day 5, 3 of 4 BALB/c lungs and no C57BL/6 lungs were involved on day 6. BALB/c lungs had moderate necrotizing pneumonia, and 2 had mild bronchiolar leukocytic exudates. Day 6 lesions in the bone marrow, spleen, liver were qualitatively the same as at day 5. The bone marrow of the maxilla in 3 of 4 BALB/c mice demonstrated mild, acute necrotizing inflammation. There were variable numbers of bacterial clusters in the hepatic sinusoids. All spleens had moderate to marked necrotizing pyogranulomatous inflammation in the red pulp, with moderate deposition of fibrin. In addition, there was moderate lymphoid depletion of the white pulp. Submandibular lymph nodes were affected in one of 4 BALB/c and in one of 3 C57BL/6 mice on day 6. The inflammation in these nodes was granulomatous. The one mouse from each strain that was examined at day 22 showed no histologic evidence of infection.
Overall, these findings indicate that until day 5 after infection, BALB/c and C57BL/6 mice show approximately equal resistance to infection with F. tularensis, although there are some differences in which organs become involved early on. After day 5, the histologic findings suggest that C57BL/6 mice are showing some resistance and clearing the infection. This scenario is not corroborated by the culture data, which show approximately equal numbers microorganisms in the lungs of both mouse strains at day 5, for example, at which point there was histologic evidence of involvement in lungs of all 4 C57BL/6 mice but only one of 4 BALB/c.
In the mice challenged with the low dose of type A F. tularensis, we noted histopathologic changes in tissues of only a minority of BALB/c mice (2 of 5) collected on day 6 after challenge (Table 3). Tissues affected were spleen, liver, and lung. We did not find histopathologic changes at other time points in BALB/c mice, nor did we find evidence of infection in C57BL/6 mice at any time point. Affected BALB/c lungs showed evidence of granulomatous focally to multifocally extensive moderate pneumonia with leukocyte necrosis. Occasional clusters of bacilli were seen also. Thymuses had mild to moderate diffuse lymphoid depletion in the cortex. The livers showed evidence of moderate, multifocal, granulomatous to pyogranulomatous hepatitis with occasional bacilli. Splenic red pulp had moderate, multifocal and coalescing splenitis that was granulomatous to pyogranulomatous. Splenic white pulp showed evidence of mild, diffuse, lymphoid depletion. No specific lesions were found in other tissues. The 2 affected mice had evidence of active bacterial infection in multiple tissues.
Table 3.
Presence of histopathologic changes in BALB/c mice (n = 5) after aerosol exposure to a low dose of type A F. tularensis
| Evidence of infection | Lung | Liver | Spleen | |
| Day 6 | 2 | 2 | 2 | 2 |
| Day 9 | 0 | 0 | 0 | 0 |
| Day 12 | 0 | 0 | 0 | 0 |
| Day 15 | 0 | 0 | 0 | 0 |
| Day 20 | 0 | 0 | 0 | 0 |
Data are given as the number of mice affected.
Type B.
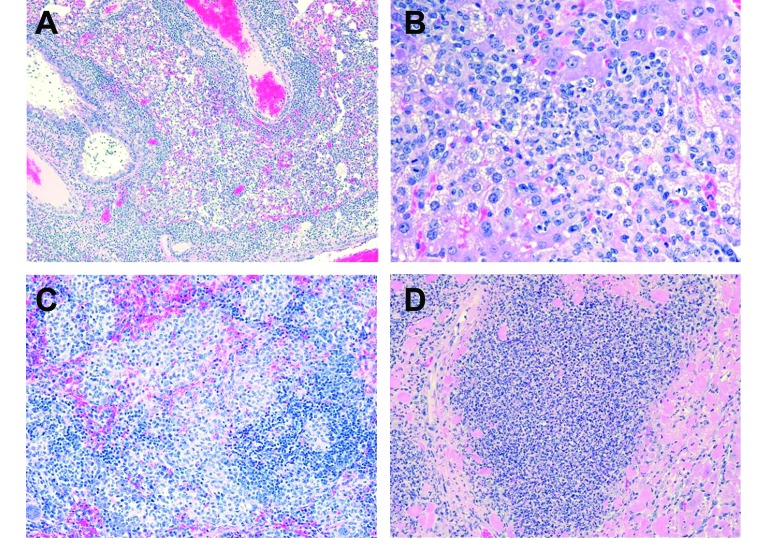
When BALB/c mice were infected by aerosol with type B F. tularensis, we did not see evidence of infection until day 3, when a mild pneumonia was present in the lung of one mouse (Table 4). On day 6, one of 5 mice had pathologic evidence of infection in lungs, liver, spleen, and mediastinum. However, the most severe changes were seen beginning at day 8 and were characterized by granulomatous or pyogranulomatous infiltrations of the lungs. Infiltrate in the spleens was primarily granulomatous, as was inflammation in the mediastinum and mediastinal, submandibular, and mesenteric lymph nodes. We also noted extensive inflammation of the heart muscle. On day 12, lungs exhibited alveolar infiltrates of either mostly macrophages or a mixture of macrophages and neutrophils. Interestingly, surrounding bronchioles and blood vessels often had cuffs consisting of lymphocytes and plasma cells (Figure 2 A). The more severe lesions in the liver and spleen consisted of multifocal moderate to marked infiltrates of macrophages with variable numbers of neutrophils (Figure 2 B). In spleen, the infiltrate was mostly macrophages accompanied by mild extramedullary hematopoiesis (Figure 2 C). Similar inflammation was sometimes present in the mediastinum and mediastinal, submandibular, and mesenteric lymph nodes.
Table 4.
Presence of histopathologic changes in BALB/c mice following aerosol exposure to Francisella tularensistype B.
| Evidence of infection | Lymph nodes |
|||||||
| Heart | Lung | Spleen | Liver | Mediastinum | Sublingual | Mesenteric | ||
| Day 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Day 3 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Day 6 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 |
| Day 8 | 5 | 1 | 5 | 5 | 5 | 1 | 1 | 1 |
| Day 12 | 4 | 4 | 4 | 4 | 4 | 0 | 0 | 0 |
| Day 15 | 4 | 4 | 4 | 4 | 4 | 0 | 0 | 1 |
| Day 20 | 4 | 1 | 4 | 4 | 4 | 0 | 0 | 0 |
Data are given as the number of mice affected.
Figure 2.
A. Lung from a BALB/c mouse 12 d following aerosol infection with Francisella tularensis type B. Note the cuffs of lymphoid cells surrounding the blood vessel (near top center) and the bronchiole (to the left of it). Alveoli contain variable numbers of macrophages and neutrophils, and small amounts of pink material which is edema fluid. H and E stain. Original magnification = 10 × . Mouse path # = 061531-3. B. Liver from a BALB/c mouse 12 d following aerosol infection with Francisella tularensis type B. The infiltrate in this liver consists mostly of macrophages in multiple clusters. Note the number of hepatocytes with clear vacuoles in them; this is a degenerative change. Very few normal hepatocytes are evident within this field. H and E stain. Original magnification = 40 × . Mouse path # = 061530-5. C. Spleen from a BALB/c mouse 12 d following aerosol infection with Francisella tularensis type B. There are numerous small granulomas consisting of compacted macrophages, within the red pulp, and to a lesser degree, the white pulp of this spleen. H and E stain. Original magnification = 20 × . Mouse path # = 061529-5.D. Heart from a BALB/c mouse 15 d following aerosol infection with Francisella tularensis type B. Within this section of myocardium there is an extensive infiltrate of macrophages and neutrophils. There is significant loss of cardiac muscle cells within this area, and some degenerating or necrotic muscle cells (bright pink) are evident around the periphery of the inflammation. H and E stain. Original magnification = 20 × . Mouse path # = 061534-4.
Beginning about day 15, the histopathologic features began to change from being those of active infection to those of resolving infection. In the lung, the peribronchiolar lymphoid cuffs remained, but the active pneumonia was generally absent. The liver had little evidence of infiltrates of macrophages; instead, extramedullary hematopoiesis was present multifocally. The spleen contained mostly extramedullary hematopoiesis. Many of the lymphoid areas of the mice, including lymph nodes and thymus, were variably depleted of lymphocytes, attributable to systemic corticosteroids. In addition, the heart was affected occasionally. There were mild, sometimes moderate infiltrates of lymphocytes and macrophages in the epicardium. Several mice, particularly at day 15, demonstrated extensive inflammation of the heart muscle itself (Figure 2 D).
Clinical observations revealed that BALB/c mice displayed signs, such as lethargy, hunched back, and anorexia at least 48 h before death, whereas C57BL/6 mice did not exhibit clinical signs until only a few hours before death.
Discussion
Mice can be useful as models of human disease for many reasons, including the wide availability of inbred strains, genetic knockout, and well-characterized immunodeficient strains. In this study, we established murine models of type A and type B F. tularensis infection for use in evaluating vaccines and therapeutics against tularemia. Although AKR/J, DBA/1, BALB/c, and C57BL/6 mice were all susceptible to the lethal effects of type A F. tularensis, we chose to use BALB/c and C57BL/6 mice because these inbred laboratory strains are commonly used for studies involving biothreat agents.5,20,23,25,41 Although LD50 determinations using type A microorganisms suggested that C5BL/6 mice were more susceptible to lethal infection, surviving C57BL/6 mice tended to shed the infection more rapidly than did BALB/c mice. Histopathogenic lesions were less severe in C57BL/6 mice than in BALB/c mice. We also noted differences when BALB/c mice were infected with type A compared with type B microorganisms. Although the lethality of infection was similar between types A and B according to LD50 values, type A-infected survivors shed the infection within 9 d of challenge, whereas mice that survived type B infection exhibited a low level of residual infection for 3 wk. In addition, time to death of mice given similar doses was shorter for the type A infection than the type B disease (data not shown). This result is similar to the findings of others, who found that mice died sooner after type A (day 6) than type B (day 8) infection.7 Overall, although less susceptible to lethal infection, BALB/c mice appeared more clinically ill for a longer duration than did C57BL/6 mice.
In addition, the pathogenesis of infection differed between mice challenged with type A or type B F. tularensis. Mice challenged with type B bacteria developed moderate leukopenia beginning 15 d after challenge, whereas mice given the type A bacteria developed severe leukopenia at 4 d after challenge. The histopathologic reactions were more severe in mice given the type A microorganism, with lesions frequently exhibiting necrosis. Gross changes in internal organs were not noted until day 4 after challenge, and inflammatory necrosis could be seen in the livers, with hepatocytes containing microorganisms. Type A-associated changes in the lungs were apparent by 4 d after infection. Lungs contained severe pulmonary necrosis and pleuritis. Pulmonary tissue surrounding small and medium blood vessels was infiltrated by macrophages and neutrophils. Histopathologic changes were of lower magnitude in the spleen than the liver. Within 2 d of infection, the populations of neutrophils and macrophages in the spleen increased. The splenic white pulp contained basophilic granules, necrotic debris, and bacteria. This histopathogenic presentation in type A-infected mice is similar to that of humans infected with type A F. tularensis. The hallmark of tissue change was pyogranulomatous inflammation. No histopathologic changes were noted in the hearts of type-A-infected mice.
In addition, rabbits were severely affected after aerosol exposure to type A F. tularensis.33 Lymphocyte depletion and tissue necrosis seem to be shared characteristics between the rabbit and mouse models.
Type B-infected mice tended to have more macrophage infiltrates than did those infected with type A, which had heavy infiltrates of neutrophils with the macrophages. In type B infection, there were lymphoid cuffs surrounding blood vessels and bronchioles in the lung. With routine histologic stains, neither strain of bacteria was readily evident microscopically, except type A organisms appeared to be clustered within hepatocytes. Changes in the liver were less severe in mice given the type B microorganism than type A bacteria.
Although we have found evidence of cardiac involvement after infection with type B F. tularensis, other investigators found no correlation with another type B strain in BALB/c mice.29 The ability to affect cardiac tissue may not be a universal characteristic of type B strains. In another study, F. tularensis was isolated from the heart blood of a fatal human case of tularemia presumably acquired by aerosol,32 but the infecting microorganisms were not classified regarding type, nor were pathologic changes in the heart addressed.
The usefulness of animal models depends on how closely they mimic human disease. Histopathologic changes reported after F. tularensis infection in humans include pyogranulomatous pneumonia, interstitial pneumonia, organ necrosis, thrombosis, giant cell formation, lung edema, and the migration of neutrophils and macrophages into tissue.2,21,26,43 The most commonly reported infiltrating cell type in human tularemia is the neutrophil.21 The degeneration of the neutrophils was associated with the presence of microabscesses, particularly in liver and spleen, which were common features in human and animal infection.21 The histopathogenesis in mice infected with F. tularensis was similar to that seen in human patients with tularemia pneumonia.2,21,43 In our study, we did not note symptoms similar to ulceroglandular disease, the most common clinical manifestation of tularemia. However, we did find similarities in common with nonspecific febrile systemic illness (typhoidal tularemia). In an outbreak on Martha's Vineyard during the summer of 2000, 11 patients developed pneumonic tularemia, and 1 person died.14 Aerosol exposure led to infection in the lungs, which progressed to a systemic infection in other organs.14 The disease in humans can result in deterioration of the spleen and liver accompanied by lesions in the lung.44 Widespread dissemination of bacteria has also been reported to occur in human tularemia.21
We noted the presence of bacteria in blood and tissue of infected mice beginning on day 3 after infection and continuing until day 9. In addition, our mice displayed a lack of residual infection after resolution of acute infection with type A F. tularensis. We do not know whether tularemia in humans behaves similarly or whether the duration of illness typically is longer after type B infection. Other microorganisms, such as B. mallei and B. pseudomallei, have a propensity for prolonged infection in both humans and experimental animals.5,47
The histopathologic features we noted in mouse models of tularemia caused by type A and type B organisms were similar to the findings from an African green monkey model of tularemia.46 In both models, infection was characterized by necrotizing pyogranulomatous lesions targeting the lungs and lymphoid tissues. These changes also are found in human disease. Other similarities between the African green monkey and mouse models and human disease are: necrotizing inflammation in the lungs and lymphoid tissue, and lymphoid depletion (African green monkey, mediastinal lymph nodes; mouse, splenic white pulp). Multinucleated giant cells or histologic changes in the kidney, both of which have been reported to occur in human disease, were not found in our mice or in the African green monkey model.46 Another difference between the mouse models and human disease is that type B infection in humans is rarely fatal, whereas type B infection in mice is as virulent (in terms of observed lethality) as type A infection. However, type B infection had less severe histopathologic consequences in mice.
Our findings from mice were similar to the histologic presentation in rhesus macaques naturally infected with type B F. tularensis.15 The macaques were found to have pyogranulomatous inflammation in several lymphoid tissues, including splenic white and red pulp.15 Inflammation progressed to necrosis, whereas necrotic lesions were not as pronounced in the mouse.15 A major difference in findings between mice and macaques is that mice surviving acute infection eventually shed the infection, whereas the macaques in the case study tended not to respond well to supportive care and therapy and were euthanized.
Our study demonstrated that mouse models of tularemia caused by type A or type B F. tularensis show many similarities to human tularemia and the African green monkey model of tularemia. These mouse models may be useful for evaluating the efficacy of medical countermeasures against tularemia.
Acknowledgments
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the US Army.
This research was conducted under an IACUC-approved protocol in compliance with the Animal Welfare Act, PHS Policy, and other federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is accredited by the AAALAC and adheres to principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 2011.
This research was funded by the Defense Threat Reduction Agency under USAMRIID project number 05-4-5P-001.
References
- 1.Avashia SB, Petersen JM, Lindley CM, Schriefer ME, Gage KL, Cetron M, DeMarcus TA, Kim DK, Buck J, Montenieri JA, Lowell JL, Antolin MF, Kosoy MY, Carter LG, Chu MC, Hendricks KA, Dennis DT, Kool JL. 2004. First reported prairie dog-to-human tularemia transmission, Texas, 2002. Emerg Infect Dis 10:483–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avery FW, Barnett TB. 1967. Pulmonary tularemia. A report of 5 cases and consideration of pathogenesis and terminology. Am Rev Respir Dis 95:584–591. [DOI] [PubMed] [Google Scholar]
- 3.Bell JF, Stewart SJ. 1983. Quantum differences in oral susceptibility of voles, Microtus pennsylvanicus, to virulent Francisella tularensis type B in drinking water: implications to epidemiology. Ecol Dis 2:151–155. [PubMed] [Google Scholar]
- 4.Bigler WJ, Jenkins JH, Cumbie PM, Hoff GL, Prather EC. 1975. Wildlife and environmental health: raccoons as indicators of zoonoses and pollutants in southeastern United States. J Am Vet Med Assoc 167:592–597. [PubMed] [Google Scholar]
- 5.Carr BG, Waag DM. 2008. Glanders, p 121–146 In: Dembek ZF. Textbooks of military medicine: medical aspects of biological warfare. Washington (DC): Office of the Surgeon General, US Army. [Google Scholar]
- 6.Clifford CB. [Internet]. Routine health monitoring of Charles River rodent barrier production colonies in Europe and North America. Charles River Research Models. [Cited Mar 25, 2014]. Available at: http://www.criver.com/files/pdfs/rms/hmsummary.aspx.
- 7.Conlan JW, Chen W, Shen H, Webb A, KuoLee R. 2003. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb Pathog 34:239–248. [DOI] [PubMed] [Google Scholar]
- 8.Conlan JW, KuoLee R, Shen H, Webb A. 2002. Different host defenses are required to protect mice from primary systemic vs pulmonary infection with the facultative intracellular bacterial pathogen, Francisella tularensis LVS. Microb Pathog 32:127–134. [DOI] [PubMed] [Google Scholar]
- 9.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Tonat K. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763–2773. [DOI] [PubMed] [Google Scholar]
- 10.Eigelsbach HT, Hunter DH, Janssen WA, Dangerfield HG, Rabinowitz SG. 1975. Murine model for study of cell-mediated immunity: protection against death from fully virulent Francisella tularensis infection. Infect Immun 12:999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans ME, Gregory DW, Schaffner W, McGee ZA. 1985. Tularemia: a 30-year experience with 88 cases. Medicine (Baltimore) 64:251–269. [PubMed] [Google Scholar]
- 12.Evans ME, McGee ZA, Hunter PT, Schaffner W. 1981. Tularemia and the tomcat. JAMA 246:1343. [PubMed] [Google Scholar]
- 13.Eyles JE, Hartley MG, Laws TR, Oyston PC, Griffin KF, Titball RW. 2008. Protection afforded against aerosol challenge by systemic immunisation with inactivated Francisella tularensis live vaccine strain (LVS). Microb Pathog 44:164–168. [DOI] [PubMed] [Google Scholar]
- 14.Feldman KA, Enscore RE, Lathrop SL, Matyas BT, McGuill M, Schriefer ME, Stiles-Enos D, Dennis DT, Petersen LR, Hayes EB. 2001. An outbreak of primary pneumonic tularemia on Martha's Vineyard. N Engl J Med 345:1601–1606. [DOI] [PubMed] [Google Scholar]
- 15.Ferrecchia CE, Colgin LM, Andrews KR, Lewis AD. 2012. An outbreak of tularemia in a colony of outdoor-housed rhesus macaques (Macaca mulatta). Comp Med 62:316–321. [PMC free article] [PubMed] [Google Scholar]
- 16.Finney DJ. 1971. Probit analysis. Cambridge (UK): Cambridge University Press. [Google Scholar]
- 17.Fortier AH, Slayter MV, Ziemba R, Meltzer MS, Nacy CA. 1991. Live vaccine strain of Francisella tularensis: infection and immunity in mice. Infect Immun 59:2922–2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fritz DL, Vogel P, Brown DR, Waag DM. 1999. The hamster model of intraperitoneal Burkholderia mallei. Vet Pathol 36:276–291. [DOI] [PubMed] [Google Scholar]
- 19.He Y, Rush HG, Liepman RS, Xiang Z, Colby LA. 2007. Pathobiology and management of laboratory rodents administered CDC category A agents. Comp Med 57:18–32. [PubMed] [Google Scholar]
- 20.Heine HS, Chuvala L, Riggins R, Hurteau G, Cirz R, Cass R, Louie A, Drusano GL. 2013. Natural history of Yersinia pestis pneumonia in aerosol-challenged BALB/c mice. Antimicrob Agents Chemother 57:2010–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamps LW, Havens JM, Sjostedt A, Page DL, Scott MA. 2004. Histologic and molecular diagnosis of tularemia: a potential bioterrorism agent endemic to North America. Mod Pathol 17:489–495. [DOI] [PubMed] [Google Scholar]
- 22.Larsson P, Oyston PC, Chain P, Chu MC, Duffield M, Fuxelius HH, Garcia E, Halltorp G, Johansson D, Isherwood KE, Karp PD, Larsson E, Liu Y, Michell S, Prior J, Prior R, Malfatti S, Sjostedt A, Svensson K, Thompson N, Vergez L, Wagg JK, Wren BW, Lindler LE, Andersson SG, Forsman M, Titball RW. 2005. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat Genet 37:153–159. [DOI] [PubMed] [Google Scholar]
- 23.Leakey AK, Ulett GC, Hirst RG. 1998. BALB/c and C57Bl/6 mice infected with virulent Burkholderia pseudomallei provide contrasting animal models for the acute and chronic forms of human melioidosis. Microb Pathog 24:269–275. [DOI] [PubMed] [Google Scholar]
- 24.Leary S, Underwood W, Anthony R, Cartner S, Corey D, Grandin T, Greenacre CB, Gwaltney-Bran S, McCrackin MA, Meyer R, Miller D, Shearer J, Yanong R. 2013. AVMA guidelines for the euthanasia of animals: 2013 edition. September 16, 2014. Available at: http://works.bepress.com/cheryl_greenacre/14
- 25.Lever MS, Nelson M, Ireland PI, Stagg AJ, Beedham RJ, Hall GA, Knight G, Titball RW. 2003. Experimental aerogenic Burkholderia mallei (glanders) infection in the BALB/c mouse. J Med Microbiol 52:1109–1115. [DOI] [PubMed] [Google Scholar]
- 26.Martin GJ, Marty AM. 2001. Clinicopathologic aspects of bacterial agents. Clin Lab Med 21:513–548 [ix.]. [PubMed] [Google Scholar]
- 27.McCrumb FR. 1961. Aerosol infection of man with Pasteurella tularensis. Bacteriol Rev 25:262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McLendon MK, Apicella MA, Allen LA. 2006. Francisella tularensis: taxonomy, genetics, and Immunopathogenesis of a potential agent of biowarfare. Annu Rev Microbiol 60:167–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pavlis O, Kusakova E, Novotny L, Pohanka M. 2013. Organs of BALB/c mice can be injured in course of tularemia. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.Petersen JM, Schriefer ME, Carter LG, Zhou Y, Sealy T, Bawiec D, Yockey B, Urich S, Zeidner NS, Avashia S, Kool JL, Buck J, Lindley C, Celeda L, Monteneiri JA, Gage KL, Chu MC. 2004. Laboratory analysis of tularemia in wild-trapped, commercially traded prairie dogs, Texas, 2002. Emerg Infect Dis 10:419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piercy T, Steward J, Lever MS, Brooks TJ. 2005. In vivo efficacy of fluoroquinolones against systemic tularaemia infection in mice. J Antimicrob Chemother 56:1069–1073. [DOI] [PubMed] [Google Scholar]
- 32.Pittman B, Shaw EB, Jr, Cherry WB. 1977. Isolation of Francisella tularensis from infected frozen human blood. J Clin Microbiol 5:621–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pullen RL, Stuart BM. 1945. Tularemia: analysis of 225 cases. JAMA 129:495–500. [Google Scholar]
- 34.Reed DS, Smith L, Dunsmore T, Trichel A, Ortiz LA, Cole KS, Barry E. 2011. Pneumonic tularemia in rabbits resembles the human disease as illustrated by radiographic and hematological changes after infection. PLoS ONE 6:e24654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reintjes R, Dedushaj I, Gjini A, Jorgensen TR, Cotter B, Lieftucht A, D'Ancona F, Dennis DT, Kosoy MA, Mulliqi-Osmani G, Grunow R, Kalaveshi A, Gashi L, Humolli I. 2002. Tularemia outbreak investigation in Kosovo: case control and environmental studies. Emerg Infect Dis 8:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roy CJ, Hale M, Hartings JM, Pitt L, Duniho S. 2003. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal Toxicol 15:619–638. [DOI] [PubMed] [Google Scholar]
- 37.Sammak RL, Rejmanek DD, Roth TM, Christe KL, Chomel BB, Foley JE. 2013. Investigation of tularemia outbreak after natural infection of outdoor-housed rhesus macaques (Macaca mulatta) with Francisella tularensis. Comp Med 63:183–190. [PMC free article] [PubMed] [Google Scholar]
- 38.Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. 1961. Tularemia vaccine study. II. Respiratory challenge. Arch Intern Med 107:702–714. [DOI] [PubMed] [Google Scholar]
- 39.Schricker RL, Eigelsbach HT, Mitten JQ, Hall WC. 1972. Pathogenesis of tularemia in monkeys aerogenically exposed to Francisella tularensis 425. Infect Immun 5:734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shoemaker D, Woolf A, Kirkpatrick R, Cooper M. 1997. Humoral immune response of cottontail rabbits naturally infected with Francisella tularensis in southern Illinois. J Wildl Dis 33:733–737. [DOI] [PubMed] [Google Scholar]
- 41.Sinha K, Bhatnagar R. 2010. GroEL provides protection against Bacillus anthracis infection in BALB/c mice. Mol Immunol 48:264–271. [DOI] [PubMed] [Google Scholar]
- 42.Stuart BM, Pullen RL. 1945. Tularemic pneumonia: review of American literature and report of 15 additional cases. Am J Med Sci 210:223–236. [Google Scholar]
- 43.Syrjala H, Sutinen S, Jokinen K, Nieminen P, Tuuponen T, Salminen A. 1986. Bronchial changes in airborne tularemia. J Laryngol Otol 100:1169–1176. [DOI] [PubMed] [Google Scholar]
- 44.Tarnvik A. 1989. Nature of protective immunity to Francisella tularensis. Rev Infect Dis 11:440–451. [PubMed] [Google Scholar]
- 45.Tarnvik A, Eriksson M, Sandstrom G, Sjostedt A. 1992. Francisella tularensis—a model for studies of the immune response to intracellular bacteria in man. Immunology 76:349–354. [PMC free article] [PubMed] [Google Scholar]
- 46.Twenhafel NA, Alves DA, Purcell BK. 2009. Pathology of inhalational Francisella tularensis spp. tularensis SCHU S4 infection in African green monkeys (Chlorocebus aethiops). Vet Pathol 46:698–706. [DOI] [PubMed] [Google Scholar]
- 47.Vietri NJ, Deshazer D. 2008. Melioidosis, p 147–166 In: Dembek ZF. Textbooks of military medicine: medical aspects of biological warfare. Washington (DC): Office of the Surgeon General, US Army. [Google Scholar]
- 48.Wherry WB, Lamb BH. 2004. Infection of man with Bacterium tularense. 1914. J Infect Dis 189:1321–1329. [DOI] [PubMed] [Google Scholar]
- 49.Woods JP, Crystal MA, Morton RJ, Panciera RJ. 1998. Tularemia in 2 cats. J Am Vet Med Assoc 212:81–83. [PubMed] [Google Scholar]