Moderate sedation is produced by the administration of pharmacologic agents, by a route that results in a depressed level of consciousness, but allows the patient to independently maintain a patent airway and respond appropriately to verbal commands or physical stimulus. Sedation occurs on a continuum from minimal sedation to general anesthesia and patients progress along that line based on the medication given, the route, the dose and the patient's own current clinical status. The provider caring for the patient must be able to recognize the clinical differences between the levels of sedation, and be able to rescue the patient, should the patient progress to a deeper level than was intended. For example, the healthcare provider who is capable of monitoring or administering moderate sedation must be able to recognize when that the patient has slipped into deep sedation and provide any necessary emergency care. This care may include airway support, fluids, more frequent assessments, or an immediate consult with an anesthesia provider or other practitioner with advanced airway skills, if necessary. The sedation continuum was first coined in 1985.[1] Being a subjective based continuum, it has been recently formulated to include some objective columns to predict the on-going risks of serious adverse events.[2] However, we sought to modify the current sedation continuum to make more self-explanatory. The following table shows the levels of sedation, and their effect upon the patients’ airway, breathing, and cardiovascular system. Our modification includes defining a level which we called deeper sedation level column. Furthermore, we added the drug-induced raw on the bottom of the original table of sedation continuum. The reason of adding the drug induced raw is to bring a close focus to the so-called endoscopist-directed propofol practice, which induces the deep sedation level on the continuum; however, with a little increase of the propofol dose the patient can easily introduced to a deeper level on the continuum.[3] We believe that the “modified sedation continuum” adds a new dimension in the paradigm of defining different levels of sedation, which indefinitely will help physicians providers to distinguish between deep and deeper sedation levels and hence interfering timely and properly earlier to rescue the patient before any serious adverse events happen [Figure 1]. For better performance and understanding of the moderate sedation protocol a course using a combination of didactic and simulation education to is essential. For the purpose of course, we sought to develop a road map or what we call “moderate sedation ladder” which summarizes the four essential steps of moderate sedation practice [Figure 2]. The ladder is similar to the WHO analgesic ladder, but with different contents.[4]
Figure 1.
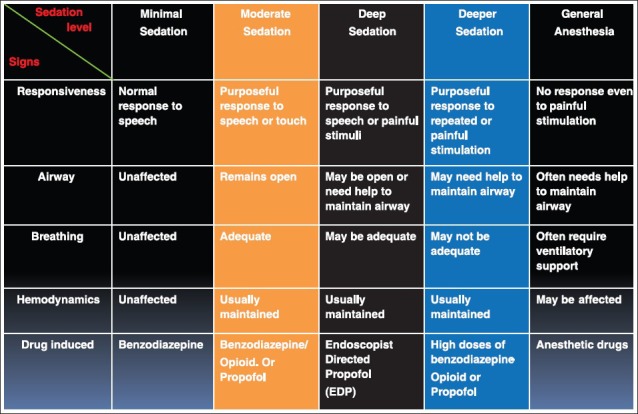
Modified sedation continuum
Figure 2.
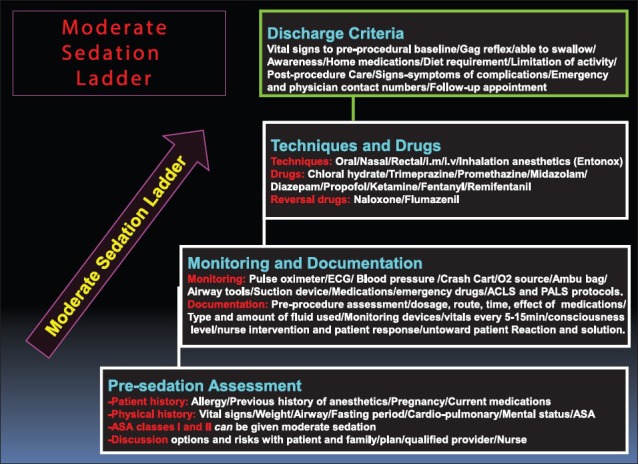
Moderate sedation ladder
We believe that understanding of the modified sedation continuum will enable providers with a clear distinction between different levels of sedation and hence proper titration of the induced drugs to avoid serious adverse events. Equally the summation of different issues of moderate sedation ladder will help providers not to miss any step of the moderate sedation protocol.
REFERENCES
- 1.Consensus conference. Anesthesia and sedation in the dental office. JAMA. 1985;254:1073–6. [PubMed] [Google Scholar]
- 2.Green SM, Mason KP. Stratification of sedation risk — A challenge to the sedation continuum. Paediatr Anaesth. 2011;21:924–31. doi: 10.1111/j.1460-9592.2011.03609.x. [DOI] [PubMed] [Google Scholar]
- 3.Sieg A, bng-Study-Group, Beck S, Scholl SG, Heil FJ, Gotthardt DN, et al. Safety analysis of endoscopist-directed propofol sedation: A prospective, national multicenter study of 24 441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29:517–23. doi: 10.1111/jgh.12458. [DOI] [PubMed] [Google Scholar]
- 4.Zeppetella G. The WHO analgesic ladder: 25 years on. Br J Nurs. 2011;20:S4. doi: 10.12968/bjon.2011.20.17.S4. S6. [DOI] [PubMed] [Google Scholar]


