Abstract
Although propofol has been the backbone for sedation in gastrointestinal endoscopy, both anesthesiologists and endoscopists are faced with situations where an alternative is needed. Recent national shortages forced many physicians to explore these options. A midazolam and fentanyl combination is the mainstay in this area. However, there are other options. The aim of this review is to explore these options. The future would be, invariably, to move away from propofol. The reason is not in any way related to the drawbacks of propofol as a sedative. The mandate that requires an anesthesia provider to administer propofol has been a setback in many countries. New sedative drugs like Remimazolam might fill this void in the future. In the meantime, it is important to keep an open eye to the existing alternatives.
Keywords: GI endoscopy sedation, non-anesthetist administered propofol, propofol complications in sedation, propofol Remimazolam
INTRODUCTION
During the recent national shortages of propofol, physicians started to look for alternatives with similar properties. A major setback to the use of propofol for sedation by physicians globally is the legal binding as a result of the directive released by the American Society of Anesthesiologists (ASA) and the Royal College of Anesthetists (Great Britain) that “Propofol must only be used by healthcare provider with specialized training in airway management.” As per a recent survey from Canada, it was realized that more than 90% of gastroenterologists use sedation for facilitating procedures in a GE suite.[1] An interesting survey involving gastroenterologists from 29 European countries found that non-anesthesiologist administration of propofol (NAAP) was used by 29.9% of the respondents in nine countries, and approximately two-thirds of other endoscopists would consider implementing steps against the use of propofol by non-anesthesiologists. They also found that in the present scenario, the main reasons for pressing the use of an anesthesiologist for based propofol sedation were medico-legal issues and cost.[2] Most of the physicians beyond anesthesiologists and emergency physicians do not actually receive any specific additional training in management of airway and thus they end up into complications upon the use of propofol and are likely to face legal actions. Additionally, it is not uncommon to find an occasional patient with an allergy to egg or soya that form components of propofol formulations available in the market. It is difficult to categorize the type of allergy or the possible dangers of propofol administration in these patients. Although mild allergy may not be an absolute contraindication to the administration of propofol, one has to make a decision to proceed with this anesthetic or resort to an alternative.[3] Outside of endoscopy anesthesia, the need for an alternative is mainly for induction, as anesthesia can be maintained with inhalational anesthetics. Thiopentone or etomidate readily fills this gap as long as maintenance is performed by alternative means. This invariably involves the administration of inhalational agents, which requires tracheal intubation for an upper GI endoscopy. Also, as most GI procedure suites do not have adequate scavenging systems, inhalational anesthetic administration can be environmentally hazardous. GI endoscopy demands a still or cooperative patient to tolerate procedures of short to intermediate duration. For upper GI procedures, this entails airway sharing. The expectation is always a level of sedation and analgesia that allows the insertion of an endoscope with no coughing/retching/gagging. The modern GI endoscope practice involves many diagnostic and therapeutic procedures that could be intensely stimulating for brief periods of time. Many of these procedures (endoscopic retrograde cholangiopancreatography, endoscopic mucosal resection, endoscopic ultrasound, double balloon enteroscopy) are of a long duration, and sometimes unpredictable. Colonoscopy alone will not pose the same problems as upper GI endoscopy. The exclusive control of the airway by the anesthesiologist allows traditional inhalational anesthesia administration using a facemask preceded by induction using many propofol alternatives. The following review, however, discusses intravenous alternatives to propofol in endoscopy anesthesia (both upper and colon) and their modalities of administration. We assume that this will be especially useful for patients who need anesthesia for the procedures where conscious sedation is seen as impractical or impossible only because of limitations to propofol use. Additionally, the drugs discussed here can also be used as adjuvants to reduce the total amount of propofol consumed.
GENERAL PHARMACOLOGY OF INTRAVENOUS ANESTHETIC/SEDATION AGENTS
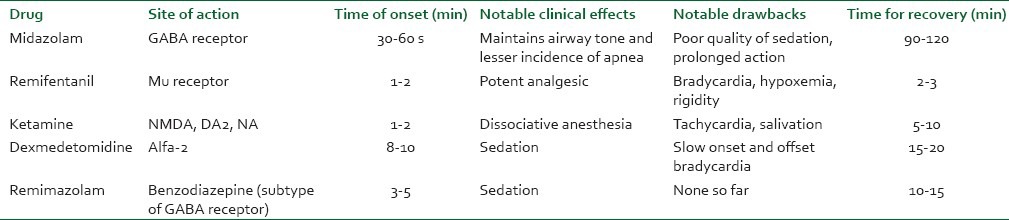
The drugs discussed in this review [Table 1] follow either a two- or a three-compartmental pharmacokinetic model. From a gastroenterologist's perspective, this means drugs momentarily distributing into the central compartment and almost instantly leaving to the muscle (so-called vessel-rich compartment) and fat. This distribution-induced fall in the plasma concentration allows awakening after a bolus administration. In order to keep the patients asleep after a bolus-induced sleep, it is important to follow with additional smaller boluses or, ideally, an infusion. Organ-dependent, and sometimes independent (in case of Remifentanil), elimination of the administered drug also begins almost instantly. This process of distribution and elimination applies to all the intravenous drugs used by both gastroenterologists and anesthesiologists. Although the intent of this paper is to discuss alternatives, a discussion of propofol itself is essential. As more gastroenterologists attempt to use it, it is important to be aware of the pitfalls of using this drug especially in combination with opioids. The major advantage of propofol is the unparalleled quality of recovery, especially after short anesthetics. In the hands of experts, deep levels of sedation can be maintained for short — intermediate endoscopic procedures and yet ensure timely termination of the infusions, where the patient can wake up in a short time (usually 5-7 min). The clear-headed nature of recovery usually allows rapid discharge however to produce effective sedation that allows insertion of an endoscope (especially gastroscope requires doses that border on apnea). Relatively small doses can lead to coughing (rarely laryngospasm) and larger doses can cause partial (or complete if untreated) airway obstruction. Any physician attempting to use propofol should be able to recognize and treat laryngospasm, if necessary, by tracheal intubation. Fospropofol was recently tried as an effective sedation for GI endoscopy. It is a prodrug of propofol.[4] However, the pharmacological variability and ability to cause apnea were difficult to address. In the absence of a pharmacological antagonist, it will be difficult for a non-anesthesia trained practitioner to use either of these compounds safely, except for very short procedures and in small titrated doses. It must be realized that evidence clearly suggests that use of sedation during procedures significantly improves the gastroenterologist's satisfaction scores toward procedural conditions and thus if the use of propofol is limited (legal binding for airway training), one must look for other valid alternatives.[5]
Table 1.
Comparison of propofol alternatives in endoscopy anesthesia
ALTERNATIVES TO PROPOFOL
Midazolam and fentanyl are the mainstay of conscious sedation in GI endoscopy. However, they have their drawbacks and certainly cannot fill the place of propofol. They can at best supplement the anesthesia/deep sedation provided by the other drugs discussed here.
Midazolam
Midazolam is a short-acting benzodiazepine developed in the 1970s by Hoffmann-La Roche. Midazolam has a rapid onset of action, high effectiveness and low toxicity level. Compared with propofol, it is significantly less likely to cause apnea or loss of airway. It primarily acts on centrally located GABA receptors and is unique in ability to be reversed pharmacologically using flumazenil. Before the propofol era, it gained significant popularity and was attributed as the drug of choice for short gastroenterology procedures.[6] Compared with propofol, the quality of sedation provided by midazolam in GI endoscopic procedures has been reported to be relatively less comfortable for the patient.[7] Combinations of midazolam with opioids like meperidine have been tried for sedation in a GI suite and the procedural conditions were comparable to propofol combined with low-dose midazolam. Being longer acting than propofol, the recovery times are likely to be prolonged. Paspatis et al. also highlighted this in their trial evaluating the midazolam combination with meperidine in comparison with midazolam and propofol for patients undergoing colonoscopies under sedation.[8] Another distinct advantage of midazolam that has been utilized in pediatric patients undergoing upper GI endoscopies is midazolam utility as oral pre-medication. This pre-medication dose allows enhancing the child's cooperation and lowers the eventual doses of intravenous sedation required for the procedure. Despite the quality of sedation not being as “optimal” as that of propofol, it offers distinct safety advantages over propofol. The primary cause of the ASA directive against NAAP-based sedation is the ability of propofol to cause profound apnea and loss of airway tone. Both these events ultimately lead to compromise of patient safety unless appropriate measures to secure the airway are instituted.[9,10] Recently, Cooper et al. in their extensive analysis comparing propofol-based sedation in colonoscopy to earlier sedation practices in the pre-propofol era found that propofol-based sedation had significantly higher airway-related complications.[11] Midazolam, even in relatively high doses, is not associated with apnea or loss of airway tone; thus, the airway-related complication rates are much lower even in the hands of physicians not experienced in airway management.[12] Additionally, midazolam-based sedation is not associated with hypotension, which is invariably a complication related to the propofol infusions. The above fact has significant clinical importance for sicker patients and patients with GI bleed requiring endoscopic procedures under sedation, where propofol can lead to deleterious hypotension but midazolam is much safer. Literary evidence suggests that intermittent boluses of midazolam can be successfully and safely used for patients undergoing upper GI endoscopic procedures.[13]
Remifentanil
This is an ultra-short acting opioid with unique pharmacokinetic properties. Its pharmacodynamic properties are similar to the other commonly used opioids. It is a mu receptor agonist with profound analgesic properties. Pharmacokinetically, however, unlike all other opioids, Remifentanil is metabolized by esterases. Esterases are ubiquitous, being present in many tissues including plasma and red blood cells. Its fixed context-sensitive halftime stems from this unique metabolism. Because of rapid elimination, its context-sensitive half-life time is short, about 2-4 min, and fixed. The context-sensitive half-life time is the time for the plasma concentration to drop by 50% after a period of infusion. All anesthetic drugs exhibit an increase in this time with increasing the durations of infusion. For example, with propofol, after 10 min of infusion, this is about 2 min while that after 5 h of infusion is 30 min. With Remifentanil, this is constant irrespective of the duration of infusion. For the perspective of gastroenterology, the pharmacological properties offer unique advantages. It may not be uncommon for patients undergoing GI procedures under sedation to have hepatic compromise. Thus, most sedatives will have significant alterations in their pharmacokinetics, prolonging their clinical actions and recovery times unpredictably. Remifentanil by virtue of its metabolism being independent of hepatic function offers the advantage of being predictable in its clinical actions. Along with all other commonly used opioids in anesthesia, Remifentanil is also a pure mu receptor agonist at clinical doses. To be clinically useful, this drug needs to be administered as a small bolus followed by an infusion. When the drug was first introduced into clinical practice in the late 90s, there were case reports of intense bradycardia and briefs periods of sinus pause. It is not uncommon to see this with rapid and larger boluses. Sinus pause lasting 10-15 s can be unnerving. For this reason, it is important to administer it as a small bolus (1-2 mcg/kg) infused over a period of at least 2 min. This is to be followed by an infusion at 0.06-0.2 mcg/kg/min. Administration of 0.5-2 mg midazolam 2-3 min before is useful for amnesia, although Remifentanil itself has an amnesic effect. It can be repeated again in small doses during the procedure. After 4-5 min of Remifentanil infusions, patients tolerate GI endoscopy quite well.[14] Bouvet and colleagues evaluated Remifentanil as an alternative to propofol for patient-controlled analgesia during digestive endoscopic procedures and concluded that self-administration of Remifentanil for sedation during GI endoscopies is as effective as the self-administration of propofol, and can be offered to patients especially when it is desirable that they remain conscious during the procedure.[15] The role of Remifentanil in combination etomidate infusion has been evaluated in patients scheduled for colonoscopy, and the combination has shown significantly stable hemodynamics when compared with propofol-based sedation.[16] Thus, in patients with hemodynamic compromise or on inotropes, the use of Remifentanil in combination with another hypnotic may help to maintain sedation in high-risk patients. Although Remifentanil is not an anesthetic, it does suppress the cortical EEG and many patients do not have a recollection of the procedure even when used as a single drug.[17,18] The same technique can be used for colonoscopies and will be easier due to the ability to administer oxygen via a face mask and, if necessary, assist ventilation. In our own experience, appropriately titrated Remifentanil infusion for GI endoscopy is associated with minimal complications and, eventually, can lower the “operating room time based costs” associated with procedures by promoting quick recovery.[19,20] Manolarki et al. found that Remifentanil when used for sedation during colonoscopy was effective in providing sufficient pain relief with better hemodynamic stability, less respiratory depression and significantly faster recovery and hospital discharge than moderate sedation with midazolam and meperidine.[21]
Ketamine
Ketamine is a phencyclidine derivative first used clinically in 1965. If not for emergence phenomena and unusual kind of (dissociative) anesthesia, it acts on a variety of receptors including N-methyl D-aspartate, Dopamine 2 and noradrenalin. From a gastroenterologist's perspective, ketamine scores over propofol significantly in its ability to maintain airway reflexes and preserving spontaneous respiration. Its ability to provide additional analgesia without apnea during gastroenterological procedures due to its high therapeutic index makes it one of the frontline choices to replace propofol for practitioners not specialized in airway procedures. Pharmacokinetically, the drug is ideal for endoscopy procedures. It fits into a two-compartment model. This means that after a bolus administration, the elimination curve is bi-exponential. The plasma concentration initially declines rapidlyfollowed by a slower phase due to elimination and slow distribution. Attributable to redistribution, it also has a context-sensitive half-life similar to Remifentanil, especially in short procedures like GI endoscopy. From this standpoint, it is quite useful as an infusion. However, frequently, it can be used as intermittent boluses when very short procedures are to be performed. There is limited data regarding the use of ketamine as either a single agent or with midazolam in endoscopy anesthesia/sedation. It is more popular as a mixture with propofol among a few anesthesiologists in our institution. Ketamine in sedative doses does not cause apnea and maintains airway reflexes. Miqdady et al. reported ketamine-based sedation to be particularly safe for pediatric patients undergoing upper GI endoscopy.[22] Contrary to this, Lightdale and colleges found that ketamine sedation for upper GI endoscopy was associated with an increased incidence of laryngospasm and patient movement during the procedures.[23] It must be realized that these events can however be prevented by adequate pre-medication of patients with anti-sialagogue in addition to small doses of midazolam prior to using ketamine. More experience of use of ketamine exists in pediatric patients, as ketamine is the least likely agent to cause apnea in this patient population when compared with the other sedatives available.[24]
Emergence phenomenon is a major problem with ketamine use in adults. It is an established practice to co-administer ketamine with either diazepam or midazolam. However, not all patients administered midazolam will benefit from this. There is still an 8% chance of these reactions occurring after midazolam administration.[25] Varadarajulu et al. studied the use of ketamine in patients who failed meperidine, midazolam and diazepam.[26] However, their study has certain drawbacks. Their dose of 20 mg every 5 min is not the anesthetic dose we commonly use. We did not understand the purpose of using two benzodiazepines with different times of onset and significantly different durations of action. Knowing the pharmacodynamic variability of benzodiazepines, this seems to be an unsafe practice. The incidence of desaturation was surprisingly low with no apneic events. Still, they had a very high success rate. In a large case — control analysis with ketamine anesthesia, the incidence of laryngospasm was 0.3%.[27]
Dexmedetomidine
Dexmedetomidine has unique pharmacodynamic properties (unlike Remifentanil that has unique pharmacokinetic properties). It is a selective alfa 2 agonist.[28]. Its action is similar to another alfa-2 receptor agonist called clonidine; however, it is six-times more selective. As the drug is now approved for sedation[29] in un-intubated patients, its inclusion in GI endoscopy armory is both relevant and important. Dexmedetomidine is unique in that it has properties unlike any other commonly used anesthetic drugs. Almost all studies agree on one thing, its ability to maintain spontaneous ventilation with almost no assistance required apart from occasional chin lift. In that case, why is it not as popular as one expects? The foregoing discussion relates mainly to its potential use in GI endoscopy anesthesia/sedation. There are very few studies looking at the role of dexmedetomidine in GI endoscopy.[30,31,32,33] While using dexmedetomidine in the setting of GI endoscopy, the following points should be borne in mind:
The evidence for its use in this setting is weak at best.
The optimal loading dose is unknown and evidence indicates that a bolus of 1 μg/kg over 6-10 min followed by 0.5-0.8 mcg/kg/h seems to be reasonable. However, it is important to remember that supplements of midazolam in increments of 0.5-1 mg are necessary for completion of the procedure.
As can be expected from its pharmacokinetics, the drug has a prolonged induction time and even more prolonged recovery time. Most upper GI endoscopies will not take more than 10 min, which questions the role of this drug in endoscopy altogether.
It is frequently noted that dexmedetomidine has an excellent hemodynamic profile. It suppresses intubation response and maintains heart rate and blood pressure, but it can also cause severe bradycardia and hypotension, which caused the cessation of at least one study.[31]
Even if a simple diagnostic upper GI endoscopy and a colonoscopy can be done with reasonable success, it might be difficult to carry out complicated therapeutic and advanced endoscopic procedures with dexmedetomidine even with the addition of midazolam and fentanyl.
In our opinion, dexmedetomidine might be useful for diagnostic upper endoscopy and colonoscopy in experienced hands. Use of midazolam and short-acting opioid is essential to achieve a higher success rate.
Remimazolam (CNS 7056)
From the point of a gastroenterologist, the search is always on for a suitable alternative to propofol. The drawback of Remifentanil is its propensity to cause apnea and chest wall (and even jaw muscle) rigidity. Respiratory depression with resultant hypoxemia and need for constant supervision would make its use challenging even for an experienced anesthesiologist. Its context-insensitive half-life time, although useful from an infusion standpoint, is of no benefit for bolus administration. It is midazolam with an ester moiety introduced, such that the molecule can become a substrate for esterases. As a result, it can be metabolized in the plasma and tissues quickly without needing any specific organ. The patients are likely to wake up fast as a result after a bolus administration. Like midazolam, it acts on the benzodiazepine part of GABA receptors. In a Phase IIa clinical trial on patients undergoing upper GI endoscopy, its onset of action was similar to midazolam and recovery was slightly shorter.[34] It is highly unlikely to replace propofol or be a realistic sole alternative to propofol as apnea will still be an issue and the depth of sedation that can be safely provided will be insufficient to undertake anything more than simple diagnostic endoscopy. Remimazolam is more likely to be part of future total intravenous anesthesia because of its more predictable recovery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Porostocky P, Chiba N, Colacino P, Sadowski D, Singh H. A survey of sedation practices for colonoscopy in Canada. Can J Gastroenterol. 2011;25:255–60. doi: 10.1155/2011/783706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Riphaus A, Macias-Gomez C, Devière J, Dumonceau JM. Propofol, the preferred sedation for screening colonoscopy, is underused. Results of an international survey. Dig Liver Dis. 2012;44:389–92. doi: 10.1016/j.dld.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Baombe JP, Parvez K. Towards evidence-based emergency medicine: Best BETs from the Manchester Royal Infirmary. BET 1: Is propofol safe in patients with egg anaphylaxis? Emerg Med J. 2013;30:79–80. doi: 10.1136/emermed-2012-202183.2. [DOI] [PubMed] [Google Scholar]
- 4.Garnock-Jones KP, Scott LJ. Fospropofol. Drugs. 2010;70:469–77. doi: 10.2165/11204450-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM, Durkalski V, et al. Endoscopic sedation in the United States: Results from a nationwide survey. Am J Gastroenterol. 2006;101:967–74. doi: 10.1111/j.1572-0241.2006.00500.x. [DOI] [PubMed] [Google Scholar]
- 6.Al-Qurain A. Comparative study of diazepam and midazolam for sedation during upper gastrointestinal endoscopy. Curr Ther Res. 1993;53:375–80. [Google Scholar]
- 7.Koshy G, Nair S, Norkus EP, Hertan HI, Pitchumoni CS. Propofol versus midazolam and meperidine for conscious sedation in GI endoscopy. Am J Gastroenterol. 2000;95:1476–9. doi: 10.1111/j.1572-0241.2000.02080.x. [DOI] [PubMed] [Google Scholar]
- 8.Paspatis GA, Manolaraki M, Xirouchakis G, Papanikolaou N, Chlouverakis G, Gritzali A. Synergistic sedation with midazolam and propofol versus midazolam and pethidine in colonoscopies: A prospective, randomized study. Am J Gastroenterol. 2002;97:1963–7. doi: 10.1111/j.1572-0241.2002.05908.x. [DOI] [PubMed] [Google Scholar]
- 9.Practice guidelines for sedation and analgesia by nonanesthesiologists. Anesthesiology. 2002;96:1004–17. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 10.Goudra BG, Singh PM. Cardiac arrests during endoscopy with anesthesia assistance. JAMA Intern Med. 2013;173:1659–60. doi: 10.1001/jamainternmed.2013.8756. [DOI] [PubMed] [Google Scholar]
- 11.Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia Assistance-A population-based analysis complications after colonoscopy with anesthesia. JAMA Intern Med. 2013;173:551–6. doi: 10.1001/jamainternmed.2013.2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reeves ST, Havidich JE, Tobin DP. Conscious sedation of children with propofol is anything but conscious. Pediatrics. 2004;114:e74–6. doi: 10.1542/peds.114.1.e74. [DOI] [PubMed] [Google Scholar]
- 13.Smith MR, Bell GD, Quine MA, Spencer GM, Morden AE, Jones JG. Small bolus injections of intravenous midazolam for upper gastrointestinal endoscopy: A study of 788 consecutive cases. Br J Clin Pharmacol. 1993;36:573–8. doi: 10.1111/j.1365-2125.1993.tb00417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alexander R, Fardell S. Use of remifentanil for tracheal intubation for caesarean section in a patient with suxamethonium apnoea. Anesthesia. 2005;60:1036–8. doi: 10.1111/j.1365-2044.2005.04281.x. [DOI] [PubMed] [Google Scholar]
- 15.Bouvet L, Allaouchiche B, Duflo F, Debon R, Chassard D, Boselli E. Remifentanil is an effective alternative to propofol for patient-controlled analgesia during digestive endoscopic procedures. Can J Anaesth. 2004;51:122–5. doi: 10.1007/BF03018769. [DOI] [PubMed] [Google Scholar]
- 16.Toklu S, Iyilikci L, Gonen C, Ciftci L, Gunenc F, Sahin E, et al. Comparison of etomidate-remifentanil and propofol-remifentanil sedation in patients scheduled for colonoscopy. Eur J Anaesthesiol. 2009;26:370–6. doi: 10.1097/EJA.0b013e328318c666. [DOI] [PubMed] [Google Scholar]
- 17.Koitabashi T, Johansen JW, Sebel PS. Remifentanil dose/electroencephalogram bispectral response during combined propofol/regional anesthesia. Anesth Analg. 2002;94:1530–3. doi: 10.1097/00000539-200206000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Vennila R, Hall A, Ali M, Bhuiyan N, Pirotta D, Raw DA. Remifentanil as single agent to facilitate awake fibreoptic intubation in the absence of premedication. Anesthesia. 2011;66:368–72. doi: 10.1111/j.1365-2044.2011.06687.x. [DOI] [PubMed] [Google Scholar]
- 19.Goudra BG, Singh PM, Sinha AC. Anesthesia for ERCP: Impact of anesthesiologist's experience on outcome and cost. Anesthesiol Res Pract. 2013;2013:570518. doi: 10.1155/2013/570518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goudra BG, Singh PM, Sinha A. Outpatient endoscopic retrograde cholangiopancreatography: Safety and efficacy of anesthetic management with a natural airway in 653 consecutive procedures. Saudi J Anaesth. 2013;3:259–65. doi: 10.4103/1658-354X.115334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manolaraki MM, Theodoropoulou A, Stroumpos C, Vardas E, Oustamanolakis P, Gritzali A, et al. Remifentanil compared with midazolam and pethidine sedation during colonoscopy: A prospective, randomized study. Dig Dis Sci. 2008;53:34–40. doi: 10.1007/s10620-007-9818-0. [DOI] [PubMed] [Google Scholar]
- 22.Miqdady MI, Hayajneh WA, Abdelhadi R, Gilger MA. Ketamine and midazolam sedation for pediatric gastrointestinal endoscopy in the Arab world. World J Gastroenterol. 2011;17:3630–5. doi: 10.3748/wjg.v17.i31.3630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lightdale JR, Mitchell PD, Fredette ME, Mahoney LB, Zgleszewski SE, Scharff L, et al. A pilot study of ketamine versus midazolam/fentanyl sedation in children undergoing GI endoscopy. Int J Pediatr. 2011;2011:623710. doi: 10.1155/2011/623710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papoff P, Mancuso M, Caresta E, Moretti C. Effectiveness and safety of propofol in newborn infants. Pediatrics. 2008;121:448. doi: 10.1542/peds.2007-3132. [DOI] [PubMed] [Google Scholar]
- 25.Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: A randomized controlled trial. Ann Emerg Med. 2011;57:109–14. doi: 10.1016/j.annemergmed.2010.09.010. e2. [DOI] [PubMed] [Google Scholar]
- 26.Varadarajulu S, Eloubeidi MA, Tamhane A, Wilcox CM. Prospective randomized trial evaluating ketamine for advanced endoscopic procedures in difficult to sedate patients. Aliment Pharmacol Ther. 2007;25:987–97. doi: 10.1111/j.1365-2036.2007.03285.x. [DOI] [PubMed] [Google Scholar]
- 27.Green SM, Roback MG, Krauss B Emergency Department ketamine meta-analysis study group. Laryngospasm during emergency department ketamine sedation: A case-control study. Pediatr Emerg Care. 2010;26:798–802. doi: 10.1097/PEC.0b013e3181fa8737. [DOI] [PubMed] [Google Scholar]
- 28.Scheinin H, Aantaa R, Anttila M, Hakola P, Helminen A, Karhuvaara S. Reversal of the sedative and sympatholytic effects of dexmedetomidine with a specific alpha2-adrenoceptor antagonist atipamezole: A pharmacodynamic and kinetic study in healthy volunteers. Anesthesiology. 1998;89:574–84. doi: 10.1097/00000542-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Kaur M, Singh P. Current role of dexmedetomidine in clinical anesthesia and intensive care. Anesth Essays Res. 2011;5:128. doi: 10.4103/0259-1162.94750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demiraran Y, Korkut E, Tamer A, Yorulmaz I, Kocaman B, Sezen G, et al. The comparison of dexmedetomidine and midazolam used for sedation of patients during upper endoscopy: A prospective, randomized study. Can J Gastroenterol. 2007;21:25–9. doi: 10.1155/2007/350279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jalowiecki P, Rudner R, Gonciarz M, Kawecki P, Petelenz M, Dziurdzik P. Sole use of dexmedetomidine has limited utility for conscious sedation during outpatient colonoscopy. Anesthesiology. 2005;103:269–73. doi: 10.1097/00000542-200508000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Dere K, Sucullu I, Budak ET, Yeyen S, Filiz AI, Ozkan S, et al. A comparison of dexmedetomidine versus midazolam for sedation, pain and hemodynamic control, during colonoscopy under conscious sedation. Eur J Anaesthesiol. 2010;27:648–52. doi: 10.1097/EJA.0b013e3283347bfe. [DOI] [PubMed] [Google Scholar]
- 33.Muller S, Borowics SM, Fortis EA, Stefani LC, Soares G, Maguilnik I, et al. Clinical efficacy of dexmedetomidine alone is less than propofol for conscious sedation during ERCP. Gastrointest Endosc. 2008;67:651–9. doi: 10.1016/j.gie.2007.09.041. [DOI] [PubMed] [Google Scholar]
- 34.Kilpatrick GJ, McIntyre MS, Cox RF, Stafford JA, Pacofsky GJ, Lovell GG, et al. CNS 7056: A novel ultra-short-acting Benzodiazepine. Anesthesiology. 2007;107:60–6. doi: 10.1097/01.anes.0000267503.85085.c0. [DOI] [PubMed] [Google Scholar]


