Abstract
Caregiving for ill loved ones can affect sleep quality and quantity. Insufficient sleep has been associated with worse physical and mental health outcomes, and it is known to affect work performance and ability to accomplish necessary tasks. While some research has looked at the sleep of caregivers of loved ones with chronic illness and found that they experience poorer sleep, little is known about the impact of caring for a child with asthma on the caregiver’s sleep and the ways in which their sleep may be affected. Community Action Against Asthma, a community-based participatory research partnership, conducted interviews with semistructured and open-ended questions with 40 caregivers of children with asthma who live in Detroit. Findings showed that caregivers regularly experience poor quality sleep because of sleeping lightly in order to listen for the child’s symptoms, wake multiple times to check on the child because of worry, and provide care for child when he or she experiences symptoms in the middle of the night. Results of the Epworth Sleepiness Scale indicate that 12.5% of caregivers received a score of 16 or more, the score on the scale used to indicate likely presence of a sleep disorder, and 42.5% had a score of 10 or more, indicating excessive sleepiness. Sleep disturbance in caregivers is an underrecognized consequence of childhood asthma, with implications for providers caring for children with asthma.
Keywords: ashma, children, caregivers, sleep disruption
More than 7.1 million school-aged children currently have asthma,1 a leading chronic disease among children.2 African Americans, Hispanics, and people living in low-income and inner-city communities experience worse asthma outcomes, including disproportionate emergency department visits, hospitalizations, and deaths.1–3
Asthma symptoms can cause disruptions to sleep.4–11 Patients with respiratory symptoms are more likely to present to emergency rooms between the hours of midnight and 8:00 am or call physicians between 11:00 pm and 7:00 am, indicating increased severe respiratory symptoms at night.7 Researchers have concluded that asthma symptoms at night are due to unstable asthma,4,12 in response to asthma triggers.10 The guidelines of the National Asthma Education and Prevention Program (NAEPP)13 specify that not sleeping well because of asthma symptoms is an indicator of lack of control and need for increased medications. Although some studies have seen a decrease in sleep disruption with changes in medication regimen,6 others have found that these night symptoms persist despite physician care and using medications commonly prescribed to control nocturnal symptoms.4,10 Pediatric asthma patients have described difficulty falling asleep because of their asthma medication.14 Additionally, one study found that even of those who perceive their asthma as being mild some still experienced sleep disruption.10
Caring for an ill spouse, parent, or child impairs sleep quality of the caregiver, including sleep duration, sleep latency, sleep efficiency, and daytime dysfunction.15–17 These sleep disturbances are due to care recipient’s behavior, performing caregiving duties, and stress related to care recipient’s health.15,16,18 However, caregivers may resist prescribed sleep medications because of the concern that they may inhibit their ability to carry out caregiving responsibilities.19 Caregivers also stated that even when sleeping, they felt they were only “half-asleep” to be vigilant to the needs of the care recipient.16 Research has shown similar sleep disruption among caregivers of children with chronic illness—with parents who care for children who have severe chronic nonasthma respiratory disease getting less sleep than parents of healthy children.18
Providing care for a family member with a chronic illness can have a profound impact on the caregiver’s emotional health.18,20,21 Although little is known about the impact on the caregiver of a child with asthma, previous studies have demonstrated that providing care for a sick loved one can affect the emotional health of caregivers of adults with dementia15 or cancer16 or children with cerebral palsy22 or other disabilities.18,21 Williams et al20 found that 95% of caregivers of children with asthma considered their child’s asthma among the top third of their daily problems.
Studies of caregivers of ill adults have found a relationship between caregiver sleep and symptoms of depression or anxiety.15,16 A study that compared the sleep and mental health of caregivers of children with (nonasthma) chronic respiratory diseases with caregivers of healthy children demonstrated similar connections between sleep disturbance and distress. Forty percent of parents of children with cystic fibrosis or children who are on a ventilator report waking due to stress related to their child’s breathing. Although researchers found an association between the child’s health and levels of both depression and fatigue of the caregiver, this association may have been due to sleep disturbance, as the relationship disappeared when the researchers controlled in their analysis for sleep quality.18
Sleep disturbances can also affect physiological health and the ability to carry out life and caregiving responsibilities. In addition to affecting mood and quality of life, there is an association between sleep loss and cardiovascular disease, diabetes mellitus, and respiratory disorders.5 In a study by Diette et al,6 parents of children who woke due to their child’s asthma reported missing work or usual activities. Caregivers’ physical health, sleepiness, and emotional health may affect their ability to care for their ill relative,5 thus increasing health care costs, decreasing productivity earnings, and increasing costs associated with provision of services for care recipient.22
Although previous research has demonstrated that caregiving for ill loved ones can affect sleep quality and quantity, as well as physical and emotional health, little is known about the effect of caring for a child with asthma on the caregiver’s sleep. The purpose of this study was to examine whether the caregivers of children with asthma living in Detroit experience sleep disruptions, the ways in which their sleep is interrupted, and the impact of any sleep disruption.
Methods
Community Action Against Asthma (CAAA)23 is an ongoing community–academic partnership examining environmental triggers of childhood asthma in Detroit. The research conducted by CAAA includes an epidemiological component,24 examining the effects of indoor and outdoor air quality on childhood asthma exacerbations, and neighborhood and household-level intervention components.25,26 In the summer of 2009, CAAA conducted a mixed methods study to examine the effects of a child’s asthma on family members, his or her caregiver’s health and stress, and the ways in which caregivers’ skills for managing their child’s asthma translate into management of their own health. This study used a community-based participatory research approach, where the design and questions asked were developed with the steering committee of CAAA, which includes academic and community partners. The principal investigator (PI) and trained graduate students conducted a total of 40 interviews with caregivers of children with asthma in Detroit. A translator was present at 2 interviews where the caregiver preferred to conduct the interview in Spanish. A convenience sample of participants from 2 other concurrent studies of CAAA was recruited for this study. The inclusion criteria for these studies was that the child should sleep most nights a week in the caregiver’s home, be between the ages of 6 and 12, have symptoms consistent with persistent asthma, and reside in the Michigan cities of Detroit, Dearborn, Highland Park, or Hamtramck. Each interview took approximately 2 hours. Each caregiver received a $30 incentive. The institutional review board of the University of Michigan approved the interview process, and all interviewees gave consent to participate in the study. All but one interviewee gave permission to be audio recorded.
The interviews consisted of 27 semistructured, open-ended questions and a structured questionnaire with 148 items. A sample of the semistructured, open-ended questions is included in Table 1. The structured questionnaire included demographic information for the caregiver and the child(ren) with asthma and measures that have been tested and validated, such as the Epworth Sleepiness Scale and the Center for Epidemiologic Studies–Depression (CES-D) Scale. The Epworth Sleepiness Scale, a simple 8-item questionnaire with a high level of internal consistency (α = .88), uses a Likert-type scale to assess the degree to which an individual has the propensity to fall asleep. The individual is asked how likely it is that he or she will fall asleep in 8 different situations or activities that most people engaged in as part of their lives. Possible scores range from 0 to 24. To create a dichotomous variable, threshold value of 16 was used to indicate a sleep disorder27 and a score ≥10 indicated excessive sleepiness.28 The CES-D is a 20-item questionnaire, with a range of scores from 0 to 60, designed to measure depressive symptoms in the general population, using validated questions and has been demonstrated to have high validity and reliability. A higher score indicates more symptoms.29
Table 1.
Sample Semistructured, Open-Ended Questions and Probes
| 1. On a day that [child’s name] has asthma symptoms, what is that like? |
| 2. Tell me about how things are going with [child’s name]’s asthma. |
| (a) Daytime symptoms |
| (b) Nighttime symptoms |
| (c) ER visits |
| (d) Hospitalizations |
| (e) In the day-to-day, have you seen changes over time? |
| 3. How does [child’s name]’s asthma affect your everyday life? |
| (a) Anything else? |
| (b) Worry |
| (c) Sleep |
| (d) Work |
| (e) School |
| (f) Play |
| (g) Routine tasks |
| (h) Managing symptoms |
| If no effect, |
| (i) Well, what is the hardest part? |
| 4. Can you tell me about your health? |
The open-ended portion of each interview was audio-recorded and transcribed, except for the interview for one participant who declined to be audio-recorded. The interviewer took extensive notes during this interview. The transcripts and notes were analyzed by the PI and graduate students using open coding. NVivo 8.0 was used to facilitate the management of the data. After coding several interviews, a codebook was generated that represented key concepts that were arising from the data. These concepts included a series of codes and subcodes. Additional codes were added to the codebook, as necessary, during analysis. Members of the research team each coded a sample of interviews. The PI and the graduate students met to discuss coding decisions for these interviews. Any disagreement was discussed until consensus was reached. After it was determined that members were coding consistently across team members, one research team member coded each of the remaining interviews. Table 2 includes examples of codes and subcodes used. Quantitative descriptive data were entered into one database and analyzed using SPSS. Descriptive tests were used for all demographic variables. Although we had a small sample (40 caregivers with a total of 57 children) with insufficient power to draw conclusions, to identify suggestive trends we conducted χ2 test for independence to look for associations between a rating of excessive sleepiness or sleepiness scores indicative of sleep disorder and various measures of the child’s asthma. Regression analysis was used to examine the relationship between CES-D and Epworth Sleepiness Score. A P value of .05 was used to indicate statistical significance.
Table 2.
Sample Codes
| Sample Code 1: Child’s general experience with asthma or clinical experiences |
| Sample Code 1 subcodes: |
| (1) Emotional responses to asthma |
| (2) Behavioral responses to asthma (parent or child initiated) |
| (3) Learning about asthma |
| (4) Using meds with or without assistance |
| (5) Awareness of symptoms or emerging attack |
| (6) Dealing with multiple chronic illnesses |
| (7) Communication of asthma needs |
| (8) Social activities and asthma (eg, won’t do sleepovers, activities not bothered by asthma) |
| (9) Sleep-related issues |
| Sample Code 2: family life |
| Sample Code 2 subcodes: |
| (1) Siblings’ needs and experiences |
| (2) Asthma’s impact (or nonimpact) on day-to-day family or caregiver’s life (from J1) |
| (3) Others care (or lack of care) for child |
| (4) Others with asthma in family (may be dbl-coded as D2.a.) |
| (5) Caregiving/parenting experiences with asthma (was Q.) |
| a. Organizing or changing life patterns due to asthma (eg, keeps child at home more than other children, increased monitoring, establishing a routine) |
| b. Parent or family coping strategies to address emotional/mental effects of asthma (eg, meditation, prayer) |
| c. Teaching or modeling attitudes for children (about life or asthma) |
| Sample Code 3: about the caregiver |
| Sample Code 3 subcodes: |
| (1) Physical health |
| a. Personal asthma experiences |
| (2) Emotional/mental health (in general, code here J2.) |
| a. Worry/stress/fear specific to asthma (eg, hard to watch child have attack) |
| (3) Learning about personal health |
| (4) Health-seeking behaviors (ie, action, delay or avoidance of these; prioritizing or putting aside) |
| (5) Experience with medical professionals, medical encounters (re: caregiver, not re: child) |
| (6) Social support |
| (7) Family problems |
| (8) Other family responsibilities (eg, caregiving for parent) |
| (9) Other stressors |
| (10) Work Life |
| (11) Sleep |
Results
Quantitative Results
The 40 caregivers in this study cared for a total of 57 children diagnosed with asthma. Some of those interviewed cared for more than one child with asthma symptoms: 12 caregivers cared for 2 children with asthma and 2 cared for 3 or more children with asthma. Table 3 provides information about the asthma symptoms of the 57 children who exhibited symptoms of asthma.
Table 3.
Children’s Asthma Symptoms
| % (n) | |
|---|---|
| Diagnosed with asthma by doctor, nurse, or other health professional (n = 57) | 89.5 (51) |
| Caregiver reports that their child (or children) has (have) health insurance (n = 40) | 85.0 (34) |
| During the 12 months before the interview | |
| Child woke up at least one time per week from sleep due to wheezy, dry cough, tightness in the chest, or shortness of breath (n = 57) | 38.7 (22) |
| Child had taken medication, inhalers, or nebulizers prescribed by a doctor (n = 57) | 93.0 (53) |
| Child had taken doctor-prescribed medications for breathing problems every day even when he/she was not having trouble (n = 57) | 47.4 (27) |
| Child stayed overnight in the hospital for wheezing, dry cough, tightness of the chest, or shortness of breath (n = 56) | 12.3 (7) |
| Number of days child missed school because of breathing problems in 12 months before the interview (n = 54) | |
| Between 1 and 5 school days | 48.1 (26) |
| Between 6 and 10 school days | 16.7 (9) |
| More than 10 days | 11.1 (6) |
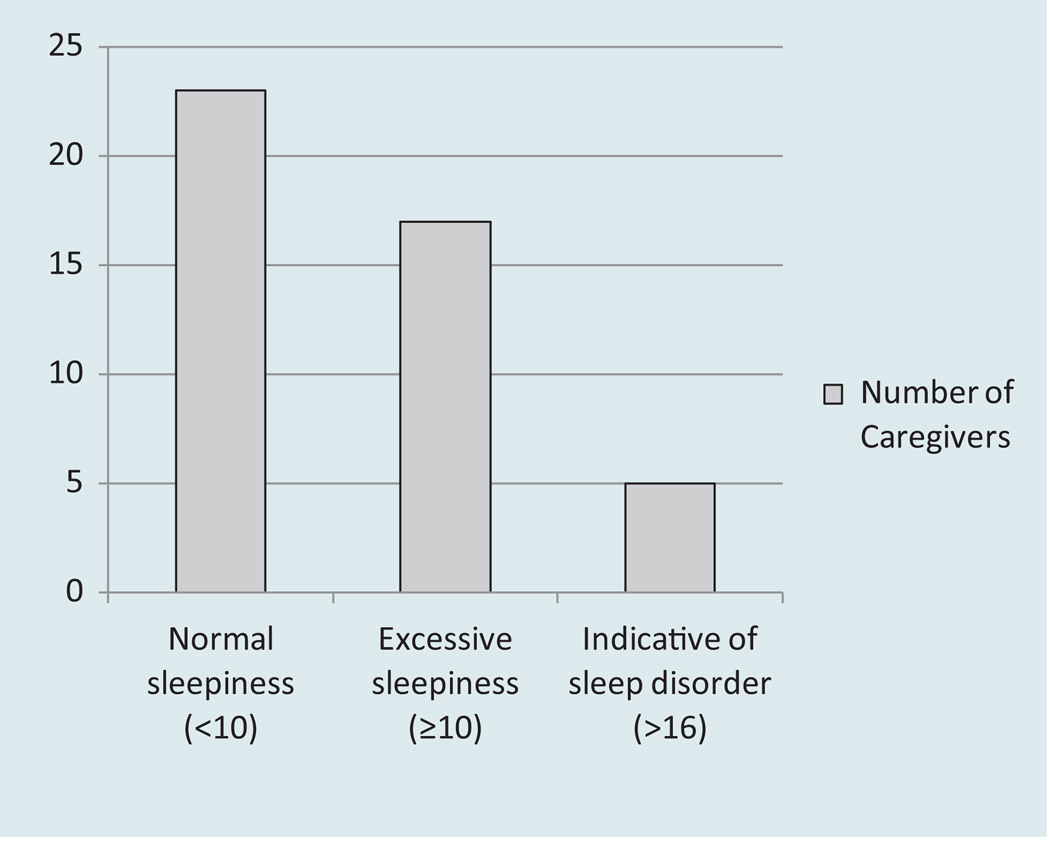
The demographic characteristics of the caregivers can be seen in Table 4. Overall, the caregivers were predominantly female (92.5%, n = 37), African American or Black (80%, n = 32), and not married (67.5%, n = 27), with nearly three quarters (73.7%, n = 28) reporting an annual income of $20 000 or less per year. Scores for the Epworth Sleepiness Scale indicated that 12.5% (n = 5) of participants had possible sleep disorder, and 42.5% (n = 17) had excessive daytime sleepiness at the threshold for clinical referral (Figure 1).
Table 4.
Demographics of Caregivers (N = 40)
| % (n) | |
|---|---|
| Gender (n = 40) | |
| Female | 92.5 (37) |
| Race/ethnicity (n = 37) | |
| Black | 80.0 (32) |
| White | 0.0 (0) |
| Multiracial | 8.1 (3) |
| Other | 5.4 (2) |
| Hispanic | 7.5 (3) |
| Education (n = 40) | |
| Less than high school | 5.0 (2) |
| Some high school | 22.5 (9) |
| High school graduate/GED | 22.5 (9) |
| Some college | 35.0 (14) |
| Associate’s or bachelor’s degree | 15.0 (6) |
| Annual income ($) (n = 38) | |
| <10 000 | 50.0 (19) |
| 10 001–20 000 | 23.7 (9) |
| 20 001–30 000 | 10.5 (4) |
| >30 001 | 15.8 (6) |
| Marital status (n = 40) | |
| Married | 32.5 (13) |
| Domestic partner | 5.0 (2) |
| Single—never married | 52.5 (21) |
| Divorced or separated | 10.0 (4) |
| Age (n = 39; mean = 39.4) | |
| ≤30 | 12.8 (5) |
| 31–40 | 43.6 17) |
| 41–50 | 30.8 (12) |
| ≥51 | 12.8 (5) |
Figure 1.
Epworth Sleepiness Scores for Caregivers
There were no significant relationships between whether the caregiver had more than one child with asthma, had at least one child who in the last year woke at least one time a week with asthma symptom, had a child hospitalized for asthma in the last year, or had a child who was taking daily medication, and Epworth scores that indicated either excessive sleepiness (≥10) or likely sleep disorder (>16; Table 5). The only relationship that approached levels of significance was the one between caregivers reporting more than one child with asthma and an Epworth score greater than 10 (P = .091). Regression analysis indicated that there was a significant relationship between depression and sleepiness with a significance level of P = .023.
Table 5.
Relationships Between Sleepiness Scores and Other Caregiver Variables
| Variables | χ2 | df | Asymp Sig. |
|---|---|---|---|
| Having more than one child with asthma and Epworth score of at least 10 | 2.857 | 1 | .091 |
| Regression analysis to examine the relationship between CES-D and Epworth Sleepiness Score | |||
| CES-D score as independent variable and Epworth Sleepiness as dependent variable | CES-D score predicted sleepiness scores: β = .146, t = 2.662, P = .023 | ||
| CES-D score accounted for a significant proportion of the variance of Epworth Sleepiness score: R2 = .140, F(1, 35) = 5.688, P = .023 | |||
Abbreviations: df, degrees of freedom; CES-D, Center for Epidemiologic Studies–Depression Scale.
Qualitative Results
The children with asthma cared for by study participants experienced nighttime asthma symptoms
At night, when he lays down, you can hear [him coughing]. And I can hear him through the wall. As he’s sleeping, you can hear it.
Caregivers attributed the night symptoms to various triggers, such as “the night air,” change in weather, exposure to smoke, or “playing too hard.” Parents tried to reduce these triggers to avoid nighttime symptoms by modifying behaviors of the child and others in the family or by reducing environmental triggers. Behavioral modifications included restricting the child’s physical activity or prohibiting smoking inside their house. Efforts to address environmental triggers in the child’s bedroom included opening the window, having a fan, or using a vaporizer.
He don’t like to sleep at night. … He’ll say, “I can’t breathe.” He will come in and, “I don’t feel good” or “I can’t breathe” or this and that. And I’ll get up and see what’s going on with him and stuff, and it’s OK. Let’s see what’s what. We’ll, crack the window. One time I put a little vaporizer in there, or whatever, because I know the heat here is dry and stuff.
Caregivers reported 3 ways in which the child’s asthmatic symptoms affected their sleep: caregivers were awakened and/or kept awake by the sound of the child’s symptoms, they were awake to care for their symptomatic child when he or she exhibited nighttime symptoms, and they slept lightly or awoke several times to check on their child throughout the night.
Caregivers reported being awakened by the sound of their child’s symptoms, such as coughing, wheezing, or snoring or by the child telling them that they were experiencing symptoms. In some cases, the child did not experience symptoms for long, and the caregiver was able to resume sleeping.
Well, if it’s in the middle of the night and I hear him, … I tell him to blow his nose. … He just go back to sleep. So, it’s nothing I have to rush in and give asthma treatment or stuff like that.
Other caregivers reported remaining awake to provide care or address triggers or to monitor the child’s symptoms.
Caregivers also explained that their sleep was disrupted because they were frequently checking on the child. Some caregivers checked on the child to see if he or she was experiencing asthmatic symptoms, in order to prevent the worsening of symptoms.
[When I check on him at night], I’m looking to see how he’s breathing and stuff, and if he knows that he’s coughing, you know. And so a lot of times, I’ll wake him up.
Other caregivers checked on the child each night out of worry, regardless of whether the child was exhibiting symptoms. Parents mentioned specifically checking on their child to make sure that he or she was still breathing.
You know what? I sleep light now. I used to sleep hard, but I don’t now because I’m always having my ears open for [Child]. All the time. It do, it bothers my sleep a lot. I don’t sleep a lot. I sleep maybe four, five hours at the most every night because I just be listening. The house quiet, I’m listening. I get up. I’ll go in there to check on him to make sure he’s still breathing. I do that a lot.
I really, really have to watch them throughout the night, literally, if I want to keep them around for the air to help them breathe because it really bothers them … [in] the middle of the night.
I worry. I got to get up and watch him. Sometimes I feel like he’s going to stop breathing when he sleep, so you know what I mean? That’s my biggest fear with him. I watch him like a hawk.
Caregivers expressed how the worry related to their child’s asthma contributed to their overall stress.
The part that bothers [me] is the worrying because I’m scared, you know? What if they have an attack and I’m not there?
I’m a little panicky, at times, especially when he sleeps. The fact that, for some reason, I have this big, strange fear of this boy’s going to stop breathing, and I’m trying to get myself out of that. It’s like the more he can get to the healthy side, the better I’ll be.
Caregivers described experiencing depression and or stress. Although some of this stress was worry related to the child’s asthma, other stress was due to other stressors, including financial concerns, neighborhood factors, health problems, or the death of family members.
It’s just the depression. That’s a hard thing, too. … I’m usually upstairs in my room. When I’m up in my room, I just cry all the time. And I don’t know why. I just cry. I know this comes from me being without an income, because I was so used to taking care of myself.
I lost my mother in 2007, so I go through little issues as far as, you know, I cry at night. … I just pray about it. That’s pretty much that. But I mean, you know, everyday life is stressful, you know, as far as the jobs and the stuff you have to deal with every day.
Caregivers expressed often feeling fatigued. This fatigue may affect their ability to perform their other family duties. The fatigue may cause them to feel overwhelmed by their many competing responsibilities.
I had a busy day with working and everything and then coming home and the homework and all of that and he all of a sudden have an attack, and I’m exhausted. I’m very exhausted, and I just want to say, “Forget it. I don’t care. I don’t want to be bothered with it.” But yet, still I know, “OK, come on, son. We got to do it.” But I’m just, I literally be falling asleep if I’m too exhausted while he’s on the machine, but he’s right there. … It’s some work. It’s work.
I’m learning how to network it in away where I can take care of the needs of everybody and I crash at nighttime because it’s so hard taking care of the needs of everybody during the day and then at night. Sometimes you’re too tired to take care of your own needs, like you don’t feel like … doing anything. All you want to do is sleep at the end of the day.
Despite the fatigue and stressors, caregivers’ sense of responsibility propelled them to continue taking care of their children with asthma and other responsibilities.
Sometimes as a parent, you are going to be tired throughout the day, but that is something you have to deal with, parents, you know what I’m saying? … Well, you can’t get upset, you know what I’m saying? We know the consequences before we had children. We know things are going to happen.
Discussion
In this study, we examined the degree to which caregivers of children with asthma living in Detroit experienced sleep disruptions, the ways in which their sleep is interrupted, and the impact of any sleep disruption on their lives. Caregivers in the sample exhibited sleep disruption for many of the same reasons as those described previously in the research on caregivers of other ill family members.15,16,18 Caregivers reported waking to perform caregiving duties, as 38.7% of the children with asthma woke up at least once per week because of asthma symptoms. This rate exceeds the criteria for poorly controlled asthma as defined by the NAEPP guidelines: waking 2 times per month.13 The method that caregivers in this study described to alleviate the impact of their child’s asthma on their sleep was trying to address the asthma nighttime symptoms or reduce asthma triggers. However, some of the actions (eg, using a humidifier) are not in line with treatment recommendations,13 and may be inappropriate responses to asthma symptoms, and unlikely to provide the child relief. This research indicates the need to expand the information provided to caregivers of children with asthma to include effective ways to address asthma symptoms when they occur.
Caregivers’ sleep was affected even when the child was not actually experiencing symptoms. Parents slept lightly to remain vigilant to listen for their child’s symptoms. A striking finding in this study was that caregivers wake frequently to make sure the child is still breathing and did not die due to asthmatic symptoms. To our knowledge, this has not been described in literature on caregiving that we found, including that of caregivers providing care to those in last stages of illness.15,16
Caregivers’ Epworth sleepiness scores indicated that more than the half (55%) of the caregivers were either experiencing excessive sleepiness or were likely to have a sleep disorder. Quantitative analysis did not elucidate why some caregivers experienced sleepiness, whereas others did not, as there was no significant relationship between whether the caregiver had more than one child with asthma, had at least one child who woke at least one time a week with asthma symptom, had a child hospitalized for asthma symptoms over the last year and either excessive or a sleepiness score indicative of sleep disorder, or had a child who was taking daily medication and sleepiness. These quantitative results must be viewed with caution, as the sample size was quite low.
The excessive sleepiness experienced by participants may not only be due only to caring for a child with asthma. It is possible that being a caregiver for a child (independent of the child’s asthma), being African American, and/or a single parent can increase the likelihood of sleep disruption independent of having a child with asthma. Previous studies of the general population have shown parents’ sleep to be disrupted after they become parents. The National Sleep Foundation30 found that 48% of parents and caregivers reported much more insomnia and 27% reported experiencing somewhat more insomnia than before they became a parent or caregiver. Most caregivers in this sample were African American or Black (80%) and single parents (67.5%). Previous studies have shown an association between being non-White31 or a member of a minority population (Maori population in New Zealand)32 and having higher Epworth Sleepiness Score. We were unable to find published research on the sleep of single parents, so we do not know how the Epworth Sleepiness Score of this sample compares with those of single parents of healthy children. This would be an interesting area for future research.
Although it is possible that these other factors (being a parent, being African American or Black, or being a single parent) may also contribute to sleep disruption, participants in this study reported specific reasons for sleep disruption that are unique to caring for a child with asthma: caring for asthmatic symptoms, sleeping lightly so they would hear their child’s symptoms, and checking to make sure their child did not die. Participants articulated that their sleep was affected by stressors—related to the child’s asthma and broader life factors, including financial stress, neighborhood stressors, the death of loved ones, or other family responsibilities. An in-depth examination of these stressors is beyond the scope of this article but can be found elsewhere.33
Several of the respondents described experiencing symptoms of depression or anxiety. These findings echo previous research on caregivers that have found an association between sleep disturbance and emotional health and mental health.18,20,21 Quantitative analysis, though consisting of a small sample, supported this relationship. Regression analysis indicated that depression accounted for a significant proportion of sleepiness variance and was also a significant predictor of sleepiness. Although caregivers in this study articulated some of the ways in which these concepts are related (eg, stress causing the caregiver to check to make sure the child was breathing), the relationship between sleep disturbance and stress is complex and a potential area for future research.
Strengths and Limitations
Participants in this study were enrolled in other studies of childhood asthma. The recruitment methods for these studies selected for children with poorly controlled asthma. Thus, the results presented here must be considered in this context and may not be representative of the general population of children with asthma and their caregivers, but represents the level of sleep disturbance among a group of caregivers of children with moderate to severe asthma.
This study provides a unique view into the lives of caregivers of children with asthma in Detroit. Although the inclusion of standard scales in the structured interview section provides a glimpse at their realities, the size of the sample limited the power of these scales and conclusions that can be drawn from regression analysis. However, the inclusion of these measures in the study complements the qualitative findings of this study and provides initial exploration of areas that can be expanded in future research. The in-depth, open-ended questions provided a more nuanced understanding of the lived experiences of these caregivers and elucidated specifically how caring for an asthmatic child causes sleep disturbance and the impact this lack of sleep has on the caregiver’s other responsibilities and emotional health.
The Epworth Sleepiness Scale, while useful for diagnostic purposes, may not capture the sleep problems faced by caregivers of children with asthma. Caregivers described feeling fatigued during the day. However, the items in this scale ask about the likelihood of sleeping in restful situations (like lying down or watching TV). These scenarios may not be relevant to the lives of those who are constantly caring for others. It is possible that the results underestimated the true level of sleepiness experienced by participants. Finally, because this study only collected data at one time point, we cannot specify the relationship between sleep disruption and stress or other mental illness.
Conclusion
Health care providers caring for children with asthma can ask targeted questions to ascertain the night symptoms that the child may be experiencing. Although some researchers4,10 found that sleep disruptions persisted despite medication, Diette et al6 state that sleep disruption due to asthma can be reduced with an appropriate medication regimen. According to the NAEPP guidelines,13 the absence of nighttime symptoms is one important component of the definition of controlled asthma and should be a goal of treatment. Health care providers must also consider the physiologic and psychological health needs of the caregiver to ensure that the caregiver can provide the best possible care to the child. This care may include an assessment of sleepiness, stress levels, and mental health issues, such as depression and anxiety, and may require working with the caregiver to seek assistance for these issues from his or her own health care provider. Additionally, health care providers should reinforce education about best responses to asthma symptoms and work with caregivers to address barriers to providing prescribed medication, such as concerns about the medication, lack of insurance or others in the household who may share medication, or availability of supervision to ensure the child takes his or her medication correctly. Additional research is needed to further elucidate the complex relationship between sleep and stress and to identify appropriate places and mechanisms for intervention.
Acknowledgments
The authors appreciate the contributions to the work described in this article of all members of the Community Action Against Asthma Steering Committee: Arab Community Center for Economic and Social Services (ACCESS), Community Health and Social Services Center (CHASS), Community member-at-large, Detroit Department of Health and Wellness Promotion, Detroit Hispanic Development Corporation (DHDC), Detroiters Working for Environmental Justice, Friends of Parkside, Henry Ford Health System, Latino Family Services, Southwest Detroit Environmental Vision, Warren Conner Development Coalition, University of Michigan School of Public Health (Departments of Environmental Health Sciences, Health Behavior and Health Education, Biostatistics), and University of Michigan School of Medicine. The work presented here was funded by Robert Wood Johnson Clinical Scholars Program, RWJF Award #56940 and Award #64332 and the Health Behavior and Health Education Summer Writing Award funded through the Faculty Allies Program at Rackham. Participants were recruited from the following studies: NIEHS Grant R01-ESO14566-01A1, “A Community Based Participatory Research Intervention for Childhood Asthma Using Air Filters and Air Conditioners” and NIEHS Grant R01-ESO14677, “Role of Diesel and Other Vehicular Exhaust in Exacerbation of Childhood Asthma.”
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
This article was previously presented as a poster at the Annual Meeting of the American Public Health Association, November 2, 2011, Washington, DC.
References
- 1.Akinbami OJ, Moorman JE, Liu X. Asthma prevalence, health care use, mortality: United states, 2005–2009. Natl Health Stat Report. 2011;(32):1–14. [PubMed] [Google Scholar]
- 2.Centers for Disease Control. Adolescent and school health: asthma and schools. [Accessed January 31, 2013]; http://www.cdc.gov/HealthyYouth/asthma/. Updated March 13, 2012.
- 3.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 4.Mastronarde JG, Wise RA, Shade DM, Olopade CO, Scharf SM. Sleep quality in asthma: results of a large prospective clinical trial. J Asthma. 2008;45:183–189. doi: 10.1080/02770900801890224. [DOI] [PubMed] [Google Scholar]
- 5.Zee PC, Turek FW. Sleep and health: everywhere and in both directions. Arch Intern Med. 2006;166:1686–1688. doi: 10.1001/archinte.166.16.1686. [DOI] [PubMed] [Google Scholar]
- 6.Diette GB, Markson L, Skinner EA, Nguyen TTH, Algatt-Bergstrom P, Wu AW. Nocturnal asthma in children affects school attendance, school performance, and parents’ work attendance. Arch Pediatr Adolesc Med. 2000;154:923–928. doi: 10.1001/archpedi.154.9.923. [DOI] [PubMed] [Google Scholar]
- 7.D’Ambrosio CM, Mohsenin V. Sleep in asthma. Clin Chest Med. 1998;19:127–137. doi: 10.1016/s0272-5231(05)70437-8. [DOI] [PubMed] [Google Scholar]
- 8.Schmier JK, Chan KS, Leidy NK. The impact of asthma on health-related quality of life. J Asthma. 1998;35:585–597. doi: 10.3109/02770909809048961. [DOI] [PubMed] [Google Scholar]
- 9.Fitzpatrick M, Engleman H, Whyte K, Deary I, Shapiro C, Douglas N. Morbidity in nocturnal asthma: sleep quality and daytime cognitive performance. Thorax. 1991;46:569–573. doi: 10.1136/thx.46.8.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner-Warwick M. Epidemiology of nocturnal asthma. Am J Med. 1988;85:6–8. doi: 10.1016/0002-9343(88)90231-8. [DOI] [PubMed] [Google Scholar]
- 11.Kier C, Hom S, Qureshi F. Asthma and sleep. J Asthma Allergy Educ. 2012;33:99–105. [Google Scholar]
- 12.Montplaisir J, Walsh J, Malo JL. Nocturnal asthma: features of attacks, sleep and breathing patterns. Am Rev Respir Dis. 1982;125:18–22. doi: 10.1164/arrd.1982.125.1.18. [DOI] [PubMed] [Google Scholar]
- 13.National Asthma Education and Prevention Program Expert Panel. Guidelines for the Diagnosis and Management of Asthma. Washington, DC: U.S. Department of Health and Human Services; 2007. (Report No. 3; NIH Publication No. 08–5846). [Google Scholar]
- 14.Townsend M, Feeny D, Guyatt G, Furlong W, Seip A, Dolovich J. Evaluation of the burden of illness for pediatric asthmatic patients and their parents. Ann Allergy. 1991;67:403–408. [PubMed] [Google Scholar]
- 15.Creese J, Bédard M, Brazil K, Chambers L. Sleep disturbances in spousal caregivers of individuals with Alzheimer’s disease. Int Psychogeriatr. 2008;20:149–161. doi: 10.1017/S1041610207005339. [DOI] [PubMed] [Google Scholar]
- 16.Flaskerud JH, Carter PA, Lee P. Distressing emotions in female caregivers of people with AIDS, age related dementias, and advanced stage cancers. Perspect Psychiatr Care. 2000;36:121–130. doi: 10.1111/j.1744-6163.2000.tb00600.x. [DOI] [PubMed] [Google Scholar]
- 17.Wilcox S, King AC. Sleep complaints in older women who are family caregivers. J Gerontol B Psychol Sci Soc Sci. 1999;54:P189–P198. doi: 10.1093/geronb/54b.3.p189. [DOI] [PubMed] [Google Scholar]
- 18.Meltzer LJ, Mindell JA. Impact of a child’s chronic illness on maternal sleep and daytime functioning. Arch Intern Med. 2006;166:1749–1755. doi: 10.1001/archinte.166.16.1749. [DOI] [PubMed] [Google Scholar]
- 19.Carter PA, Chang BL. Sleep and depression in cancer caregivers. Cancer Nurs. 2000;23:410–415. doi: 10.1097/00002820-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Williams S, Sehgal M, Falter K, et al. Effect of asthma on the quality of life among children and their caregivers in the Atlanta empowerment zone. J Urban Health. 2000;77:268–279. doi: 10.1007/BF02390538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hauenstein EJ. The experience of distress in parents of chronically ill children: potential or likely outcome? J Clin Child Psychol. 1990;19:356–364. [Google Scholar]
- 22.Brehaut JC, Kohen DE, Raina P, et al. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004;114:e182–e191. doi: 10.1542/peds.114.2.e182. [DOI] [PubMed] [Google Scholar]
- 23.Parker EA, Israel BA, Williams M, et al. Community action against asthma: examining the partnership process of a community-based participatory research project. J Gen Intern Med. 2003;18:558–567. doi: 10.1046/j.1525-1497.2003.20322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis TC, Robins TG, Dvonch JT, et al. Air pollution–associated changes in lung function among children with asthma in Detroit. Environ Health Perspect. 2005;113:1068–1075. doi: 10.1289/ehp.7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parker EA, Chung LK, Israel BA, Reyes A, Wilkins D. Community organizing network for environmental health: using a community health development approach to increase community capacity around reduction of environmental triggers. J Prim Prev. 2010;31:41–58. doi: 10.1007/s10935-010-0207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parker EA, Israel BA, Robins TG, Mentz G. Evaluation of community action against asthma: a community health worker intervention to improve children’s asthma-related health by reducing household environmental triggers for asthma. Health Educ Behav. 2008;35:376–395. doi: 10.1177/1090198106290622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994;17:703–710. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- 28.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D scale: a self report depression scale for research in the general. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 30.National Sleep Foundation. [Accessed December 12, 2012];2004 Sleep in America Poll: summary of findings. http://www.sleepfoundation.org/sites/default/files/FINAL%20SOF%202004.pdf. [Google Scholar]
- 31.Whitney CW, Enright PL, Newman AB, Bonekat W, Foley D, Quan SF. Correlates of daytime sleepiness in 4578 elderly persons: the Cardiovascular Health Study. Sleep. 1998;21:27–36. doi: 10.1093/sleep/21.1.27. [DOI] [PubMed] [Google Scholar]
- 32.Gander PH, Marshall NS, Harris R, Reid P. The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth Sleepiness scores of adults in New Zealand. Sleep. 2005;28:249–253. doi: 10.1093/sleep/28.2.249. [DOI] [PubMed] [Google Scholar]
- 33.Sampson NR, Parker EA, Cheezum RR, et al. Stress and health among caregivers of children with asthma in Detroit. Fam Community Health. 2013;36:51–62. doi: 10.1097/FCH.0b013e31826d7620. [DOI] [PMC free article] [PubMed] [Google Scholar]