Abstract
Study Objectives:
The purpose of the study was to examine whether insomnia symptoms and nightmares mediated the relation between alcohol use and suicide risk. Further, we examined whether this mediation was moderated by gender.
Design:
The study consisted of questionnaires administered online examining insomnia symptoms, nightmares, alcohol use, and suicide risk.
Setting:
University.
Patients or Participants:
375 undergraduate students at a large, public university in the southeastern United States.
Interventions:
N/A.
Measurements and Results:
Results indicated that insomnia symptoms significantly mediated the relation between alcohol use and suicide risk; however, this mediation was moderated by gender. For women, there was both a direct effect of alcohol use on suicide risk as well as an indirect effect of alcohol use through insomnia symptoms increasing suicide risk. For men, there was no direct effect of alcohol use on suicide risk, but there was a significant indirect effect of alcohol use increasing suicide risk through insomnia symptoms. Nightmares were not related to alcohol use, and the association between nightmares and suicide risk was found to be independent of alcohol use
Conclusions:
Insomnia symptoms are an important factor in explaining the mechanism by which alcohol use increases suicide risk.
Citation:
Nadorff MR, Salem T, Winer ES, Lamis DA, Nazem S, Berman ME. Explaining alcohol use and suicide risk: a moderated mediation model involving insomnia symptoms and gender. J Clin Sleep Med 2014;10(12):1317-1323.
Keywords: insomnia symptoms, suicide risk, alcohol use, gender
Suicide is a serious and growing public health concern in the United States (U.S.). In 2010 alone, 38,364 Americans died by suicide, making suicide the tenth leading cause of death in the U.S.; among 15-24 year olds it was the third leading cause of death, and was the second leading cause of death among college-age students.1 Moreover, 2010 marked the fifth consecutive year that suicide rates in the U.S. increased.1 Thus, it is crucial for clinicians and researchers to gain a better understanding of suicide risk and protective factors.
Insomnia and Suicide Risk
Numerous empirical studies have demonstrated a relation between insomnia symptoms and suicide risk,2–7 including several that have found an association above and beyond other psychopathology. In a longitudinal study of 6,504 adolescents, Wong and Brower found that sleep problems significantly predicted future suicidal ideation and attempts.7 Additionally, among young adults in the military, insomnia symptoms were positively related to suicidal ideation.6
Insomnia symptoms are also associated with death by suicide. In a chart review of U.S. Veterans who died by suicide, Pigeon and colleagues found that Veterans who had documented insomnia symptoms died within a shorter time span following their last VA appointment than did Veterans who had not reported insomnia symptoms.4 Similarly, in a large population-based study, Bjørngaard and colleagues found that, when surveyed at the outset of the study, participants who reported sleep problems “often” and “almost every night” were respectively 2.7 times and 4.3 times more likely than those who reported no sleep problems to die by suicide within the 20-year follow up.2
BRIEF SUMMARY
Current Knowledge/Study Rationale: Research has demonstrated that insomnia symptoms and nightmares are associated with suicide risk independent of many other risk factors. However, little research has examined whether insomnia symptoms or nightmares may explain how established suicide risk factors confer suicide risk.
Study Impact: The present study found that insomnia symptoms atemporally mediate the relation between alcohol use and suicide risk. Thus, insomnia symptoms are an important factor in explaining the mechanism by which alcohol increases suicide risk, and may also be an intervention target to reduce the suicide risk caused by alcohol use.
Nightmares and Suicide Risk
Nightmares have also been linked to suicidal behavior independent of other psychopathology.3,5,8–10 Nadorff and colleagues found that nightmares were significantly associated with suicidal thoughts and behaviors after controlling for symptoms of depression, anxiety, PTSD, and insomnia.5 In a prospective study, Sjöström and colleagues examined sleep disturbances, symptoms of anxiety, depressive symptoms, psychosis, and alcohol use in 163 individuals admitted to the hospital following suicide attempts, re-assessed those variables two months later, and then tracked whether or not those individuals re-attempted suicide within the next two years. Compared to those who did not report nightmares, participants who reported frequent nightmares at the outset of the study were three times more likely to re-attempt suicide, and participants who had reported frequent nightmares when reassessed two months into the study were five times more likely to re-attempt suicide.9,10
Alcohol Use, Sleep Problems, and Suicide Risk
Both alcohol use disorders and acute alcohol intoxication are associated with elevated suicidal risk.11,12 Further, controlled lab studies involving non-alcohol dependent individuals have found that the administration of alcohol is associated with greater self-administered self-injury behaviors using a novel self-injury analog.13,14
Findings across several studies demonstrate a relation between alcohol use and sleep problems. Mechanisms that contribute to this relation may be bidirectional; alcohol use contributes to sleep disturbances,15,16 and sleep disturbances may contribute to alcohol use. For example, Brower and colleagues looked at sleep problems and alcohol use in 172 individuals receiving treatment for alcohol dependence and found that 60% of participants with insomnia symptoms relapsed to alcohol use in the months following treatment, compared to 30% of participants without insomnia symptoms.17 The participants with insomnia symptoms were also more likely to report frequent use of alcohol to help them sleep.17 A daily monitoring study found that among individuals with alcohol use disorders and posttraumatic symptoms, sleep disturbances during the night were associated with increased craving for alcohol the following day.18 Further, a recent longitudinal investigation of 358 alcohol-dependent individuals showed that the number of alcoholic drinks participants had consumed over the previous 90 days was positively related to severity of insomnia symptoms when statistically accounting for baseline insomnia.19
In addition to insomnia symptoms, nightmares have also been shown to be associated with alcohol use. Munezawa and colleagues conducted a large cross-sectional study examining lifestyle, mental health, and sleep variables in relation to nightmares in Japanese adolescents, finding that respondents who reported having used alcohol in the past month were significantly more likely to report having experienced nightmares during that time.20
Due to the associations among sleep problems, alcohol use, and suicide risk, sleep problems could be a potential explanatory factor in the association between alcohol use and suicide risk. For example, empirical findings demonstrate that insomnia symptoms are significantly associated with suicide risk among those who abuse alcohol. In a study of 282 individuals in treatment for alcohol dependence, participants with insomnia symptoms were significantly more likely to report suicidal ideation.21 Further, results of a recent chart review of 161 Veterans referred for behavioral health evaluations due to evidence of heavy drinking or other substance abuse indicated that inadequate sleep quality was a significant predictor of suicidal ideation.22
Statement of the Problem
Despite literature that has found that alcohol predicts sleep problems, and that sleep problems such as insomnia and nightmares are associated with suicidal behavior, we are unaware of any studies that have examined whether the relation between alcohol use and suicidal behavior may be explained by sleep difficulties. Studies designed to directly examine the relation among these three factors, however, could have meaningful clinical implications. For example, if sleep problems mediate the relation between alcohol use and suicide risk, sleep interventions may be a particularly effective way to reduce suicide risk associated with alcohol use. College students are an important group to study these relations in for several reasons. First, suicide is the second-leading cause of death for college-aged individuals, and the suicide rate for this age group has increased in recent years.1 Second, nightmares are more prevalent among college-age students than among older adults,23 and clinically significant insomnia symptoms are prevalent,5 as is problematic alcohol use.24 Thus, these risk factors converge in the college years, making this age ideal for studying their interrelationships.
The current study aimed to fill this gap in the literature by examining whether insomnia symptoms and/or nightmares atemporally mediate the relation between alcohol use and suicide risk. We hypothesized that: (1) the relation between alcohol use and suicide risk would be partially mediated by insomnia symptoms, but that a direct effect of alcohol on suicide would remain; and (2) The relation between alcohol use and suicide risk would be partially mediated by nightmares, but a direct effect of alcohol on suicide would remain. Further, given that alcohol use and suicidal behavior differ significantly between men and women,25 we also conducted an exploratory analysis to determine whether gender moderated any mediation found.
METHODS
Participants
Participants were obtained from a survey of 375 undergraduate students from a large, public university in the Southeastern United States. All of the participants were enrolled in an undergraduate psychology course that offered course credit for research participation. The vast majority of these students were students taking a General Psychology course. Given that a large percentage of our General Psychology students are not psychology majors, our subject pool is diverse and is representative of our university.
Participants were recruited using the SONA system, an online survey manager commonly utilized to manage student participant pools. SONA presents the student with a list of all of the studies that are available and the student then is able to select the studies that he or she would like to complete. Given that students are not directly solicited, we were unable to determine the total number of students who were solicited or a response rate for the study. In the present study, the students completed all survey instruments using the SONA system. SONA then provided the research team with de-identified data while also providing the student credit for taking part in the study. Therefore, the data collection may be considered anonymous.
The sample was 60% female, with an age range of 18-36 years (mean age 19.2 years, standard deviation [SD] 1.7 years). Approximately 77% of participants identified themselves as Caucasian, 16% African American, 2.2% Asian or Pacific Islander, 2.1% other, and < 2% Hispanic and Native American. The study was approved by the institution's institutional review board (IRB), and participants were presented with a cover letter describing the study to read before participation.
Measures
The Alcohol Use Disorders Identification Test (AUDIT)
The AUDIT is a 10-item self-report measure designed to identify individuals with alcohol-related problems by assessing alcohol use and dependence over the last year.26 It is composed of 2 scales that assess both alcohol use (3 items) and alcohol dependence (7 items). A sample item is “How many drinks containing alcohol do you have on a typical day when you are drinking?” with scores ranging from 0 for “1 or 2” to 4 for “10 or more.” These scales are combined to create an index score of alcohol-related problems. Scores ≥ 8 are indicative of an alcohol use disorder.27 The AUDIT has shown concurrent validity with other alcohol use screening tests.26 In the sample, the mean was 6.76 (SD 5.83) with acceptable reliability (α = 0.83).
The Disturbing Dreams and Nightmare Severity Index (DDNSI)
The DDNSI was used as a measure of bad dream and nightmare frequency and severity. It measures nightmare frequency by asking about the number of nights with bad dreams/nightmares per week (0-7 nights) and the number of total bad dreams/ nightmares per week (up to 14).28 The DDNSI also measures the severity and intensity of the bad dreams/nightmares on a Likert scale, ranging from no problem (0) to extremely severe problem (6), as well as how often nightmares result in awakenings, ranging from never/rarely (0) to always (4). A sample item is “How would you rate the INTENSITY of your disturbing dreams and/or nightmares?” with options ranging from 0 for “Not intense” to 6 for “Extremely severe intensity.” A score > 10 may indicate the presence of a nightmare disorder.28 In the sample, the mean was 3.45 (SD 5.21) with acceptable reliability (α = 0.88).
The Insomnia Severity Index (ISI)
The ISI is a 7-item self-report measure that assesses insomnia symptoms over the last 2 weeks.29 Each item is scored on a 0-4 scale, with total scores ranging from 0-28. A sample item is “How worried/distressed are you about your current sleep problem?” with options ranging from 0 for “Not at all” to 4 for “Very much.” The ISI has been shown to have adequate test-re-test reliability over 3 months and concurrent validity with sleep diaries and polysomnography.29,30 In the sample, the mean was 8.30 (SD 4.98) and reliability was acceptable (α = 0.80).
The Suicidal Behaviors Questionnaire–Revised (SBQ-R)
The SBQ-R, revised from the Suicidal Behaviors Questionnaire,32 is a 4-item self-report measure designed to assess suicide risk.31 The SBQ-R assesses past suicidal thoughts and attempts, past suicidal ideation and threats, and future suicidal behavior. A sample item is: “Have you ever thought about or attempted to kill yourself?” with options ranging from 1 for “Never” to 4 for “I have attempted to kill myself, and really hoped to die.” A cutoff score of 7 for undergraduate populations or 8 for psychiatric inpatients may be used to determine clinically significant levels of suicide risk.31 In this sample the mean was 4.44 (SD 2.50) and reliability was acceptable (α = 0.83).
Data Cleaning and Analysis Plan
The data for the present study were obtained from a broader study. Due to the data being collected from students via online questionnaires, the data were carefully cleaned to ensure that biased responses were removed from the data set. Specifically, participants who took less than 22 minutes to complete the survey (mean duration = 46 min, SD = 21 min) were excluded from the study. Of the original 433 responses in the data set, 33 responses were removed due to completing the study too quickly (mean = 19.1, SD = 2.98, 7.6%). An additional 25 participants (5.8%) were removed due to inconsistent or potentially biased responding, such as selecting the same response for all items on a measure with reverse-coded questions, resulting in data from 375 individuals being used for the analyses.
The study measures were also examined for normality of their distributions. The SBQ-R deviated from normality (skew = 2.05, kurtosis = 3.85). A log transformation was employed to restore normality. Following the transformation, the skew (1.35) and kurtosis (0.67) were reduced. Thus, the log-transformed score for the SBQ-R was utilized for all analyses. Analyses were conducted both with the entire sample and excluding those who reported no alcohol use (N = 82). There were no differences in significance in the primary analyses. Thus, we have opted to present the data from the overall sample.
A correlation was used to examine the relation between age and suicide risk, and an ANOVA was used to test for effects of socioeconomic status, education, ethnic background, relationship status, and race on suicide risk. None of these demographic variables were significantly associated with the dependent variable, and thus they were not included in the analyses. Initial data cleaning was conducted using SAS (v. 9.3). As part of our data cleaning we found that one of our measures, the AUDIT, was missing 18% of responses due to a large number of participants declining to answer the question “How many drinks containing alcohol do you have on a typical day when you are drinking?” The missing responses were not related to the independent or dependent variables in these analyses, so the data may be assumed to be missing at random. Although list-wise deletion would be appropriate given this conclusion, we decided to impute the data using the Missing Values tool in SPSS (v.16), due to the large percentage of data that were missing. The data for the individual AUDIT items were imputed using Estimation Maximization. No other measure was missing more than 5% of data. Given that Tabachnick and Fidell suggest that in large data sets list-wise deletion is acceptable when < 5% of the data are missing,33 we utilized this method for handing missing data on all other measures. All analyses were conducted both with the imputed and non-imputed data sets and there were no differences in significance between the two. We have reported the imputed results in this manuscript.
To test our mediation hypotheses, including the exploratory hypothesis of gender moderation, we utilized the PROCESS macro.34 The PROCESS macro utilizes the bootstrapping method of testing mediation. Bootstrapping is a method of assessing direct and indirect effects of variables in a way that maximizes power and is robust against non-normality. The indirect effect represents the impact of the mediator variable on the original relation, with a value of 0 indicating no impact. Typically 95% confidence intervals are used to judge significance of the indirect effect, with ranges not including zero indicating that the two-tailed p value for the indirect effect is less than 0.05. We utilized a 95% bias-corrected bootstrap model with confidence intervals resampled 5,000 times for each analysis. We utilized a traditional mediational model to test indirect effects (Figure 1).35,36 Given that alcohol use and suicidal behavior differ significantly between men and women,25 we also conducted an experimental analysis to determine whether gender moderated the mediation (Figure 2). All analyses presented here were conducted using SPSS (v. 21) statistical software.
Figure 1. Test of mediation.
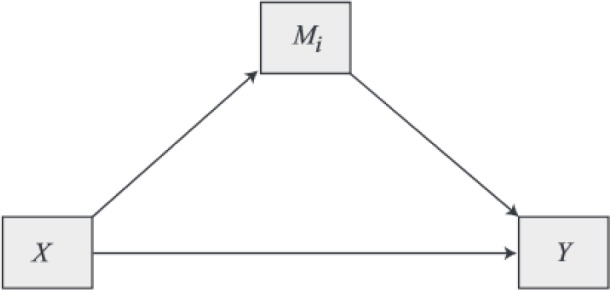
In our model alcohol use was X, insomnia symptoms were M, and suicide risk was Y.
Figure 2. Test of moderated mediation.
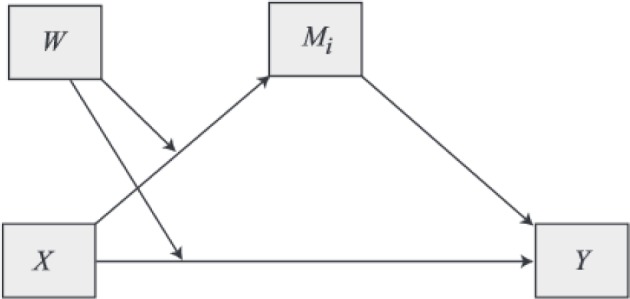
In our model alcohol use was X, insomnia symptoms were M, gender was W, and suicide risk was Y.
RESULTS
Descriptive statistics and correlations can be found in Table 1. We found that alcohol use was significantly associated with insomnia symptoms and suicide risk. We then tested whether insomnia symptoms mediated the relation between alcohol use and suicide risk. We found that alcohol use was no longer significantly associated with suicide risk after adding insomnia symptoms to the model, B = 0.004, SE = 0.004, 95% CI -0.004 to 0.013, p = 0.28, though insomnia symptoms were significantly associated with suicide risk, B = 0.025, SE = 0.0005, 95% CI 0.016 to 0.034, p < 0.01. Looking at the indirect effect, which is the impact of alcohol use on suicidal ideation through insomnia symptoms, B = 0.003, SE = 0.001, the 95% bias-corrected confidence intervals were 0.001 and 0.006. Since 0 was not in the confidence interval range, we conclude that insomnia symptoms partially mediated the relation between alcohol use and suicidal ideation.
Table 1.
Correlations and means of study variables.
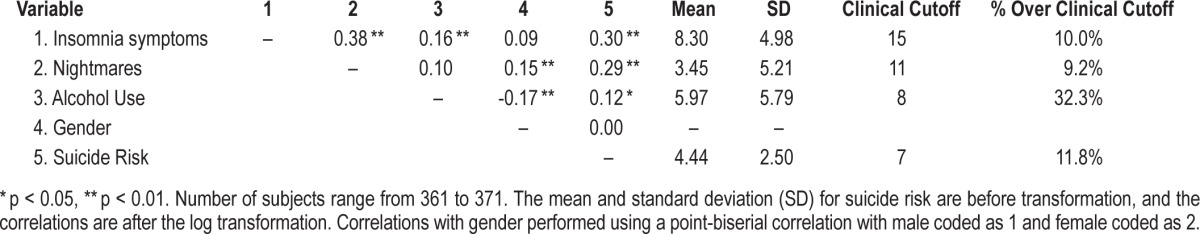
Next, we examined whether nightmares mediate the relation between alcohol use and suicide risk in the same way. Our correlation analyses revealed that alcohol use was associated with suicide risk but not with nightmares. After adding nightmares to the model alcohol use was no longer significantly associated with suicide risk, B = 0.007, SE = 0.004, 95% CI -0.0006 to 0.015, p = 0.07, though nightmares were significantly associated with suicide risk, B = 0.02, SE = 0.005, 95% CI 0.013 to 0.32, p < 0.01. Looking at the indirect effect, which is the impact of alcohol use on suicidal ideation through nightmares, B = 0.002, SE = 0.001, the 95% bias-corrected confidence intervals were -0.0003 and 0.0044. Since 0 was in the confidence interval range, we conclude that nightmares did not significantly mediate the relation between alcohol use and suicide risk.
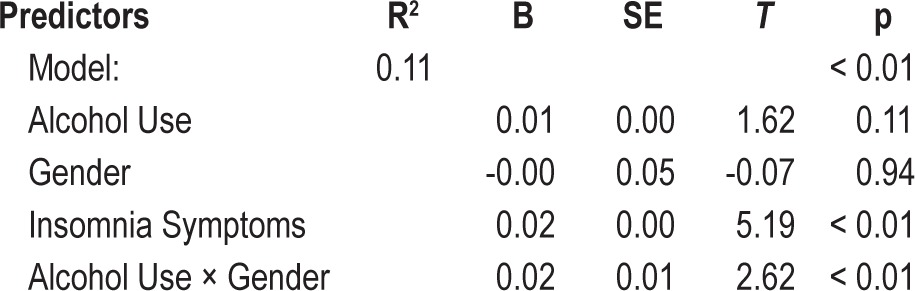
Since nightmares did not mediate the relation between alcohol use and suicide risk, we did not examine a mediated moderation. In order to examine our exploratory hypothesis that the mediational relation between insomnia symptoms, alcohol use, and suicide risk may differ by gender, we first examined study correlations for both men and women independently (Table 2), finding that although alcohol use was associated with suicide risk in women (r = 0.24), it was not associated in men (r = -0.01). To further explore these relations we conducted a moderated mediation analysis. The overall regression model was significant, with significant main effects for insomnia symptoms and the interaction between alcohol use and gender (Table 3). There were significant indirect effects of alcohol use on suicide risk through insomnia symptoms for both men (B = 0.003, SE = 0.002, 95% CI 0.0002 to 0.0074) and women (B = 0.004, SE = 0.002, 95% CI 0.0013 to 0.0085). Looking at the remaining direct effect of alcohol use on suicide risk after statistically holding insomnia symptoms constant, there was a significant direct effect of alcohol on suicide risk for women (B = 0.02, SE = 0.01, 95% CI 0.0038 to 0.0281), but not men (B = -0.01, SE = 0.01, 95% CI -0.0168 to 0.07). Thus, alcohol use was associated with suicide risk independent of insomnia symptoms for women, but not for men.
Table 2.
Correlations and means of study variables by gender.
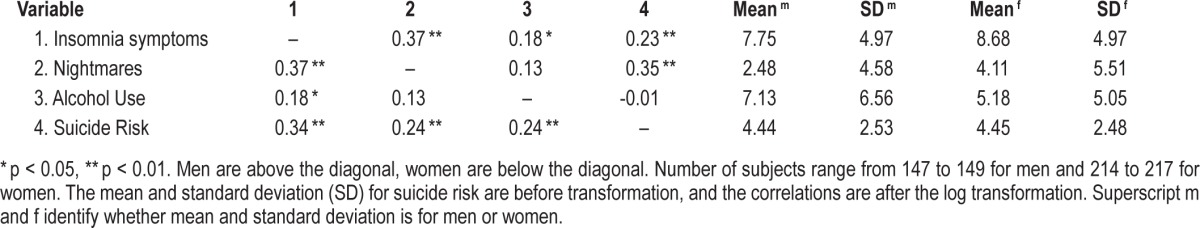
Table 3.
Gender moderating insomnia symptom's mediation of the relation between alcohol use and suicide risk.
DISCUSSION
Our findings suggest that insomnia symptoms, but not nightmares, significantly atemporally mediate the relation between alcohol use and suicide risk. Looking more closely at the insomnia symptoms mediation, we found significant indirect effects of alcohol use on suicide risk through insomnia symptoms for both men and women. Put differently, for both genders, we found that a significant amount of the effect between alcohol use and suicide risk was statistically explained by alcohol use being related with higher rates of insomnia symptoms, and these symptoms being associated with higher levels of suicide risk. This is interesting as it suggests that despite the lack of a significant correlation between alcohol use and suicide risk among men, alcohol use may still be associated with increased suicide risk due to being associated with higher levels of insomnia symptoms. Turning our attention to the direct effects, we found a direct effect of alcohol use and suicide risk for women but not for men. This result was anticipated given the correlations presented in Table 2, and suggests that if one removes the effects of insomnia symptoms, alcohol use is still associated with suicide risk in women, but not in men. These findings suggest that the positive relation of alcohol use and insomnia symptoms explains a significant amount of variance in suicide risk, and thus insomnia symptoms may be a potential target for reducing the suicide risk conferred by alcohol use.
Contrary to our prediction, nightmares failed to significantly mediate the relation between alcohol use and suicide risk. This hypothesis was based upon prior research with adolescents, which found that alcohol use in the past month was associated with significantly more nightmares.20 Although the percent of participants that had an alcohol use disorder was not reported by Munezawa and colleagues,20 it is likely that our sample of college students had more individuals with clinically significant alcohol use (32%) than the study by Munezawa and colleagues. This is important because alcohol use, particularly at higher doses, can reduce REM sleep, and thus may prevent nightmares.37 Therefore, it is possible that alcohol use may be positive associated with nightmares at lower doses and negatively associated at higher doses, obscuring the relation between the two variables. However, it is important to note that REM suppression may also lead to REM rebound, which could result in a waxing and waning of nightmares due to alcohol use. Further research, especially research utilizing polysomnography, is warranted to gain further understanding of this complex relationship.
Although we were unable to test whether nightmares mediated the relation between alcohol use and suicide risk, the present study adds to the literature regarding nightmares and suicidality. Previous studies have demonstrated that nightmares are associated with suicide risk and behavior independent of many forms of psychopathology,3,5,9,10,38–41 as well as Joiner's Interpersonal-Psychological Theory of Suicide.8,42,43 Further, research has shown that among suicide attempters, nightmares are associated with suicide risk and suicide attempts independent of alcohol use.9,10 However, to the best of our knowledge, the present study is the first to demonstrate that nightmares are associated with suicide risk independent of alcohol use among college students. Thus, consistent with previous studies, our findings suggest that nightmares are clinically relevant in predicting suicide risk.
The lack of a correlation between gender and suicide risk (r = 0.00) was surprising given that previous literature has found significant gender differences in suicide risk.31 However, gender differences are typically greater in clinical samples than in non-clinical samples, and may be one potential explanation for our lack of a gender difference.31 Thus, it is possible that the nonsignificant gender effect finding may be due to our nonclinical sample. This hypothesis is supported by the fact that when one looks at a clinical subsample, such as those individuals who reported clinically significant alcohol use, a nearly significant gender-suicide risk correlation emerges (r = 0.172, p = 0.06). It is also possible that this is a regional difference. In a re-analysis of previously reported data8 from the same university, we failed to observe a significant gender effect- suicide risk correlation in a larger sample of students (N = 730, r = -0.05, p = 0.15). Given that suicidal behavior differs widely by location and culture,44,45 it is certainly possible that gender differences found in other regions of the United States may not generalize to the Southern United States, where this study took place.
Findings from the present study are clinically relevant as it presents a new potential treatment target for reducing suicide risk in individuals with co-occurring alcohol use and insomnia symptoms. Based upon the literature demonstrating that alcohol use is associated with sleep disturbances,15,16 and this study's findings, clinical research examining whether reducing insomnia symptoms among those who abuse alcohol also results in a reduction of suicidal behaviors would be particularly interesting and would have clear clinical implications. This is important as insomnia interventions are likely to be met with greater acceptability than alcohol interventions, especially among college student populations. Thus, research evaluating whether targeted or broadly distributed sleep treatments may reduce suicide risk among college students, particularly those who also abuse alcohol, is warranted.
Based upon this study, there are several other areas of research that deserve exploration. In particular, the literature would benefit from longitudinal studies examining whether sleep problems temporally mediate the relation between alcohol use and suicide risk and behaviors. Further, research examining the association of these variables among a clinical population is needed. Lastly, research examining the mechanisms by which sleep difficulties confer suicide risk would greatly inform the literature and may result in more targeted interventions designed to reduce suicide risk.
The present study has several limitations that are worth noting. First, our study consisted of a college student sample that was predominately Caucasian (77%), which may not generalize to other populations. However, we believe that this is an important group to study as suicide is a leading cause of death among college students,1 with a suicide rate for 18- to 22-year-olds (11.94 per 100,000) being nearly as high as the suicide rate in the general population (12.4 per 100,000).1 Further, both insomnia symptoms and alcohol use are common in this population.5,46 Thus, it is an optimal population to examine this research question. Our study is also limited by its use of a cross-sectional design. To truly test mediation, which is causal, a longitudinal study is required. However, alcohol use failed to mediate the relation between insomnia symptoms and suicide risk in our sample, adding support for the potential directionality of our findings. Despite our inability to make causal attributions, the present study lays the groundwork for future longitudinal investigations that can further elucidate the relation among alcohol use, insomnia symptoms, and suicide risk. Third we utilized measures with different time frames, with the SBQ-R, examining lifetime suicide risk, the DDNSI assessing nightmares in the last year, ISI measuring insomnia symptoms in the last two weeks, and the AUDIT assessing alcohol use in the past year. Although these differences make interpretation more difficult, we believe that they introduce a conservative bias as these differences should reduce the correlation between all of these variables, but particularly insomnia symptoms since it has the shortest time frame. Thus, our faith in these findings is only strengthened by the fact that we were able to detect significant differences despite this conservative bias. Fourth, our study is limited by our participants not receiving a full psychiatric evaluation, as well as our not controlling for depressive symptoms. Not controlling for depressive symptoms is particularly notable, as depressive symptoms have been found to mediate the relation between insomnia and suicidality,5,38,47 though the literature is mixed.3,6 Thus, depressive symptoms may underlie the mediation found in the present study. However, our study still notably adds to the literature by being the first study to demonstrate that insomnia symptoms mediate the relation between alcohol use and suicide risk. The literature would greatly benefit from future examinations that extend these findings by examining these relations in clinical populations. Fifth, given that we conducted our study through the SONA systems website, and participants chose our study rather than our actively soliciting participants, we were unable to determine the response rate for the study. Lastly, our study consisted only of subjective sleep measures collected online and did not feature polysomnography or actigraphy. Polysomnography may be particularly useful in further examining the relation between REM sleep, alcohol, and nightmares. However, the ISI is a commonly used measure that has been validated against both sleep diaries and polysomnography, and thus the ISI has been established as a valid measure of subjective insomnia symptoms.29,30 That said, future research examining these relations using objective sleep measures would substantially add to the literature. Lastly, given that the focus of the present paper was to examine whether insomnia symptoms mediated the relation between alcohol use and suicide risk, examining further mediations through statistically controlling for symptoms of psycho-pathology were beyond the scope of this paper. However, we believe this is an important research area that warrants exploration in future studies.
In summary, to the best of our knowledge, our study is the first to demonstrate that insomnia symptoms mediate the relation between alcohol use and suicide risk, and that this mediation is moderated by gender. This finding has substantial potential clinical implications, as insomnia symptoms may present a treatment target to reduce suicide risk among those who use alcohol. Based upon the results of this study, we believe that additional research investigating this relation, as well as treatment studies examining whether insomnia treatments may reduce the suicide risk conferred by alcohol use, are warranted.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System. [cited 2012 February 10] Available from: http://www.cdc.gov/injury/wisqars/index.html.
- 2.Bjørngaard JH, Bjerkeset O, Romundstad P, Gunnell D. Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. Sleep. 2011;34:1155–9. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43:139–49. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pigeon WR, Britton PC, Ilgen MA, Chapman B, Conner KR. Sleep disturbance preceding suicide among veterans. Am J Public Health. 2012;102:S93–S7. doi: 10.2105/AJPH.2011.300470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–8. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136:743–50. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 7.Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the national longitudinal study of adolescent health. J Psychiatr Res. 2012;46:953–9. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nadorff MR, Anestis MD, Nazem S, Harris HC, Winer ES. Sleep disorders and the interpersonal-psychological theory of suicide: independent pathways to suicidality? J Affect Disord. 2014;152–154:505–12. doi: 10.1016/j.jad.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Sjöström N, Wærn M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–5. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 10.Sjöström N, Hetta J, Wærn M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatr Res. 2009;170:208–11. doi: 10.1016/j.psychres.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Ali S, Nathani M, Jabeen S, et al. Alcohol: the lubricant to suicidality. Innov Clin Neurosci. 2013;10:20–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Sher L. Alcoholism and suicidal behavior: a clinical overview. Acta Psych Scan. 2006;113:13–22. doi: 10.1111/j.1600-0447.2005.00643.x. [DOI] [PubMed] [Google Scholar]
- 13.Berman ME, Bradley TP, Fanning JR, McCloskey MS. Self-focused attention reduces self-injurious behavior in alcohol-intoxicated men. Subst Use Misuse. 2009;44:1280–97. doi: 10.1080/10826080902961328. [DOI] [PubMed] [Google Scholar]
- 14.McCloskey MS, Berman ME, Echevarria DJ, Coccaro EF. Effects of acute alcohol intoxication and paroxetine on aggression in men. Alcohol Clin Exp Res. 2009;33:581–90. doi: 10.1111/j.1530-0277.2008.00872.x. [DOI] [PubMed] [Google Scholar]
- 15.Roehrs T, Roth T. Sleep, sleepiness, and alcohol use. Alcohol Res Health. 2001;25:101–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Subst Abuse. 2005;26:1–13. doi: 10.1300/j465v26n01_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry. 2001;158:399–404. doi: 10.1176/appi.ajp.158.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simpson TL, Stappenbeck CA, Varra AA, Moore SA, Kaysen D. Symptoms of posttraumatic stress predict craving among alcohol treatment seekers: results of a daily monitoring study. Psychol Addict Behav. 2012;26:724–33. doi: 10.1037/a0027169. [DOI] [PubMed] [Google Scholar]
- 19.Zhabenko O, Krentzman AR, Robinson EAR, Brower KJ. A longitudinal study of drinking and depression as predictors of insomnia in alcohol-dependent individuals. Subst Use Misuse. 2013;48:495–505. doi: 10.3109/10826084.2013.781182. [DOI] [PubMed] [Google Scholar]
- 20.Munezawa T, Kaneita Y, Osaki Y, et al. Nightmare and sleep paralysis among Japanese adolescents: a nationwide representative survey. Sleep Med. 2011;12:56–64. doi: 10.1016/j.sleep.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 21.Klimkiewicz A, Bohnert ASB, Jakubczyk A, Ilgen MA, Wojnar M, Brower K. The association between insomnia and suicidal thoughts in adults treated for alcohol dependence in Poland. Drug Alcohol Depen. 2012;122:160–3. doi: 10.1016/j.drugalcdep.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chakravorty S, Grandner MA, Mavandadi S, Perlis ML, Sturgis EB, Oslin DW. Suicidal ideation in veterans misusing alcohol: relationships with insomnia symptoms and sleep duration. Addict Behav. 2014;39:399–405. doi: 10.1016/j.addbeh.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salvio MA, Wood JM, Schwartz J, Eichling PS. Nightmare prevalence in the healthy elderly. Psychol Aging. 1992;7:324–5. doi: 10.1037//0882-7974.7.2.324. [DOI] [PubMed] [Google Scholar]
- 24.Velazquez CE, Pasch KE, Laska MN, Lust K, Story M, Ehlinger EP. Differential prevalence of alcohol use among 2-year and 4-year college students. Addict Behav. 2011;36:1353–6. doi: 10.1016/j.addbeh.2011.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kenney SR, LaBrie JW. Use of protective behavioral strategies and reduced alcohol risk: examining the moderating effects of mental health, gender, and race. Psychol Addict Behav. 2013;27:997–1009. doi: 10.1037/a0033262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 27.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. 2nd ed. Geneva, Switzerland: The World Health Organization; 2001. The Alcohol Use Disorders Identification Test: Guidelines for Primary Care. [Google Scholar]
- 28.Krakow B, Melendrez DC, Johnston LG, et al. Sleep dynamic therapy for Cerro Grande Fire evacuees with posttraumatic stress symptoms: a preliminary report. J Clin Psychiatry. 2002;63:673–84. doi: 10.4088/jcp.v63n0804. [DOI] [PubMed] [Google Scholar]
- 29.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 30.Savard M, Savard J, Simard S, Ivers H. Empirical validation of the Insomnia Severity Index in cancer patients. Psycho-Oncology. 2005;14:429–41. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]
- 31.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire--Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8:443–54. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- 32.Linehan MM. The Suicidal Behaviors Questionnaire (SBQ) University of Washington. 1981 [Google Scholar]
- 33.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013. [Google Scholar]
- 34.Hayes AF. New York, NY: Guilford Press; 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- 35.Baron RM, Kenny DA. The moderator—mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 36.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: effects on normal sleep. Alcohol Clin Exp Res. 2013;37:539–49. doi: 10.1111/acer.12006. [DOI] [PubMed] [Google Scholar]
- 38.Cukrowicz KC, Otamendi A, Pinto JV, Bernert RA, Krakow B, Joiner TE., Jr The impact of insomnia and sleep disturbances on depression and suicidality. Dreaming. 2006;16:1–10. [Google Scholar]
- 39.Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–41. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 40.McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCall WV, Batson N, Webster M, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. J Clin Sleep Med. 2013;9:135–40. doi: 10.5664/jcsm.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joiner T. Why People Die By Suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 43.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McIntosh JL, Drapeau CW. U.S.A. Suicide 2011: Official Final Data. [cited November 1, 2013]. Available from: http://www.suicidology.org.
- 45.Canetto SS, Sakinofsky I. The gender paradox in suicide. Suicide Life Threat Behav. 1998;28:1–23. [PubMed] [Google Scholar]
- 46.Chiauzzi E, DasMahapatra P, Black RA. Risk behaviors and drug use: a latent class analysis of heavy episodic drinking in first-year college students. Psychol Addict Behav. 2013;27:974–85. doi: 10.1037/a0031570. [DOI] [PubMed] [Google Scholar]
- 47.Nadorff MR, Fiske A, Sperry JA, Petts R, Gregg JJ. Insomnia symptoms, nightmares and suicidal ideation in older adults. J Gerontol Psychol Sci. 2013;68:145–52. doi: 10.1093/geronb/gbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]


