Abstract
BACKGROUND
Surgery resident education is based on experiential training, which is influenced by changes in clinical management strategies, technical and technologic advances, and administrative regulations. Trauma care has been exposed to each of these factors, prompting concerns about resident experience in operative trauma. The current study analyzed the reported volume of operative trauma for the last two decades; to our knowledge, this is the first evaluation of nationwide trends during such an extended time line.
METHODS
The Accreditation Council for Graduate Medical Education (ACGME) database of operative logs was queried from academic year (AY) 1989–1990 to 2009–2010 to identify shifts in trauma operative experience. Annual case log data for each cohort of graduating surgery residents were combined into approximately 5-year blocks, designated Period I (AY1989–1990 to AY1993–1994), Period II (AY1994–1995 to AY1998–1999), Period III (AY1999–2000 to AY2002–2003), and Period IV (AY2003–2004 to AY2009–2010). The latter two periods were delineated by the year in which duty hour restrictions were implemented.
RESULTS
Overall general surgery caseload increased from Period I to Period II (p < 0.001), remained stable from Period II to Period III, and decreased from Period III to Period IV (p < 0.001). However, for ACGME-designated trauma cases, there were significant declines from Period I to Period II (75.5 vs. 54.5 cases, p < 0.001) and Period II to Period III (54.5 vs. 39.3 cases, p < 0.001) but no difference between Period III and Period IV (39.3 vs. 39.4 cases). Graduating residents in Period I performed, on average, 31 intra-abdominal trauma operations, including approximately five spleen and four liver operations. Residents in Period IV performed 17 intra-abdominal trauma operations, including three spleen and approximately two liver operations.
CONCLUSION
Recent general surgery trainees perform fewer trauma operations than previous trainees. The majority of this decline occurred before implementation of work-hour restrictions. Although these changes reflect concurrent changes in management of trauma, surgical educators must meet the challenge of training residents in procedures less frequently performed.
LEVEL OF EVIDENCE
Epidemiologic study, level III; therapeutic study, level IV.
Keywords: Surgical residents, trauma, ACGME, resident work-hour restrictions, education
Trauma is a leading cause of morbidity and mortality worldwide.1 General surgery residents learn to manage trauma through broad exposure, including operative experience. However, there is concern that changes in surgical education, changes in the epidemiology of trauma, and the evolution toward a nonoperative approach to blunt solid organ trauma may have reduced educational experience. We sought to quantify these changes through a review of the Accreditation Council for Graduate Medical Education (ACGME) database of graduating residents’ operative case logs, which represent the aggregated nationwide experience of all graduating surgery residents. Previous reviews of resident experience in operative trauma have been based on single-institution data or have focused on the era before implementation of work-hour restrictions. This analysis was designed to answer the following questions: Has national surgery resident operative trauma volume changed during the last two decades? Are there discernible differences following the introduction of work-hour restrictions? Has the experience of chief residents (CRs) changed during the last two decades? Findings from this review have implications on current trainees’ preparation for entry into the workforce.
MATERIALS AND METHODS
Description of the Database
Case log databases were provided from the ACGME as PDF documents (academic year [AY] 1989–1990 through AY2009–2010) and transcribed into an Excel spreadsheet (Microsoft, Redmond, WA) for analysis. Residents submit individual case logs containing their cumulative 5-year operative experience at the completion of residency. The ACGME then aggregates these data for the entire graduating cohort, generates summary statistics, and issues national reports. For certain ‘‘defined categories’’ (including trauma), subcategories, and individual procedures, the ACGME reports the total number of cases for the entire cohort, average cases per resident, SDs, and average cases performed as CR. The median number of cases is available for certain categories. The average “total major cases” (TMCs) per resident are typically reported but were not included in the AY2004–2005 and AY2005–2006 reports. For these 2 years, subtotals of all major subcategories were combined to generate the TMC (this produced the same numbers for TMC published by authors from the ACGME Applications and Data Analysis Department2). Consequently, SDs are not available for TMC in AY2004–2005 and AY2005–2006.
During the 21 years documented in this review, there have been changes in the format of information submission and changes in minimum case requirements. Specific changes were summarized through extensive personal communication with ACGME staff, review of all available Surgery Residency Review Committee (RRC) newsletters (1998–2010), and evaluation of changes in case log reports. The case logs have continually distinguished between trauma-related and nontrauma exploratory laparotomy, spleen, and liver cases. For most of the period reviewed, fractures, burns, and vascular injuries were included in the “trauma” category; however, starting in AY2009–2010, these were moved into separate subcategories. For AY2009–2010, subtotals for fracture, vascular trauma, and burn procedures were added to the total trauma category to generate a number consistent with the previous 20 years; consequently, no SD is available for total trauma in AY2009–2010. Where SDs were not available for individual years, they were imputed from adjacent years (if necessary for analysis).
Because the ACGME-designated trauma category includes such a broad array of procedures, including burn care, fracture repair, and urologic procedures, an “Intra-abdominal Trauma” category was generated that included subtotals of esophageal, gastric, duodenal, small bowel, colon, splenic, hepatic, kidney, and pancreatic operations for trauma, as well as repair of the abdominal aorta or vena cava and cases coded as trauma laparotomy or laparoscopy. Because the intra-abdominal trauma category was generated from summary statistics, no SDs are available.
Some aspects of trauma operations were coded inconsistently. In some years, the reports distinguished between spleen repair and splenectomy, and open versus laparoscopic, but in other years, these were combined. Laparoscopic procedures for solid organ trauma were rare, so laparoscopic spleen operations were disregarded in those years in which the reports were subdivided (AY1993–1994 to AY2000–2001). A sensitivity analysis showed that this exclusion changed the mean by less than 0.05 cases per resident during the most affected period. Coding categories for traumatic liver cases were more inconsistent, so all trauma liver cases were combined into a single yearly average; consequently, published SDs could not be used.
Analytic Strategy
To reduce the impact of any single year on the analysis, annual resident cohorts were combined into approximately 5-year blocks, designated Period I (AY1989–1990 to AY1993–1994), Period II (AY1994–1995 to AY1998–1999), Period III (AY1999–2000 to AY2002–2003), and Period IV (AY2003–2004 to AY2009–2010). The latter two periods were delineated by the year in which duty-hour restrictions were first implemented (July 1, 2003), with Period III representing the pre–80-hour work-week era and Period IV representing the post–80-hour work-week era. Annual means were combined into a period mean; where SDs were available for annual means, they were combined into a period SD.
Using STATA (StataCorp, College Station, TX), a oneway analysis of variance (ANOVA) was performed for Periods I, II, III, and IV using the “aovsum” command, which can generate a statistical model from summary statistics. We chose the conservative Bonferroni adjustment for multiple comparisons, and significance was set at α = 0.05. For data in which annual SDs were unavailable (intra-abdominal trauma and liver cases), ANOVA of the annual means within each period followed by the Bonferroni adjustment was performed (in this case, variance is generated by differences in the annual means and not variance among individual residents, as estimated by the original annual SDs).
Data are also presented in a year-by-year format. Each category or type of operation is presented in graphic form. Statistical analysis included simple linear regression (SLR) of the annual means against graduating year to produce linear coefficients and 95% confidence intervals (95% CIs). To assess whether the rate of change was different from the first decade (AY1989–AY1999) to the second (AY2000–AY2009), SLR was stratified by decade.
Finally, the percentage of trauma cases logged by each graduating cohort specifically during the chief year was calculated for total trauma and intra-abdominal trauma, spleen, and liver operations. SLR was performed to generate coefficients and CIs.
RESULTS
Total Major Cases
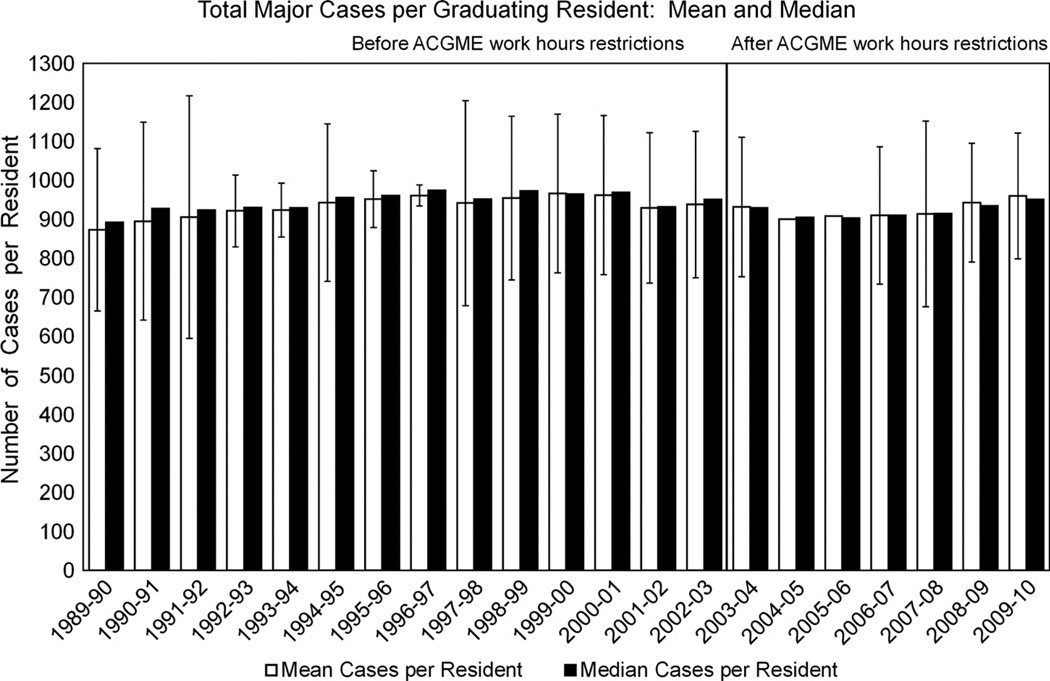
The average number of TMCs increased during the two decades of our study (Fig. 1). However, there was substantial yearly variation, and SLR during the entire two decades did not reveal a significant trend. TMC increased throughout most of the 1990s. This was followed by multiple slight decreases in the early 2000s. (Some of these declines are attributable to coding changes introduced by the RRC in AY2001–2002.3) When the data were analyzed by cumulative periods (Table 1), TMC increased from Period I to Period II, remained stable from Period II to Period III, and decreased from Period III to Period IV (ANOVA, p < 0.001). Pairwise analysis detected significant differences between TMCs for each period (all p < 0.001) except for Period II and Period III.
Figure 1.
Total major cases per graduating resident: Mean and median. Bars indicate SD. No SD available for AY2004–2005 and AY2005–2006.
TABLE 1.
Mean Number of Cases Per Graduating Resident by Period
| Period I | Period II | Period III | Period IV | |
|---|---|---|---|---|
| Procedure Type | AY1989–1999 to AY1993–1994 |
AY1994–1995 to AY1998–1999 |
AY1999–2000 to AY2002–2003 |
AY2003–2004 to AY2009–2010 |
| TMCs | 904.1 (210.0) | 950.6 (178.9) | 949.2 (198.0) | 924.1 (167.6) |
| ACGME-designated trauma operations | 72.5 (45.7) | 54.5 (34.0) | 39.3 (18.9) | 39.4 (21.3) |
| Operations for intra-abdominal trauma | 30.9 | 23.5 | 18.0 | 16.8 |
| Operations for splenic trauma | 4.7 (4.0) | 3.7 (3.7) | 3.1 (2.8) | 3.0 (2.9) |
| Operations for liver trauma | 3.9 | 3.1 | 2.1 | 1.9 |
SDs for the period means are reported in parentheses and were only able to be calculated for TMCs, ACGME-designated total trauma cases, and operations for splenic trauma. The “Intra-abdominal Trauma” category was generated from subtotals of operations for esophageal, gastric, duodenal, small bowel, colon, splenic, hepatic, kidney, and pancreatic trauma, as well as repair of the abdominal aorta or vena cava and cases coded as trauma laparotomy or laparoscopy. One-way ANOVA p < 0.001 for each category or type of operation; results of pairwise comparisons (Bonferroni adjustment) are reported in the text.
ACGME-Designated Total Trauma Cases
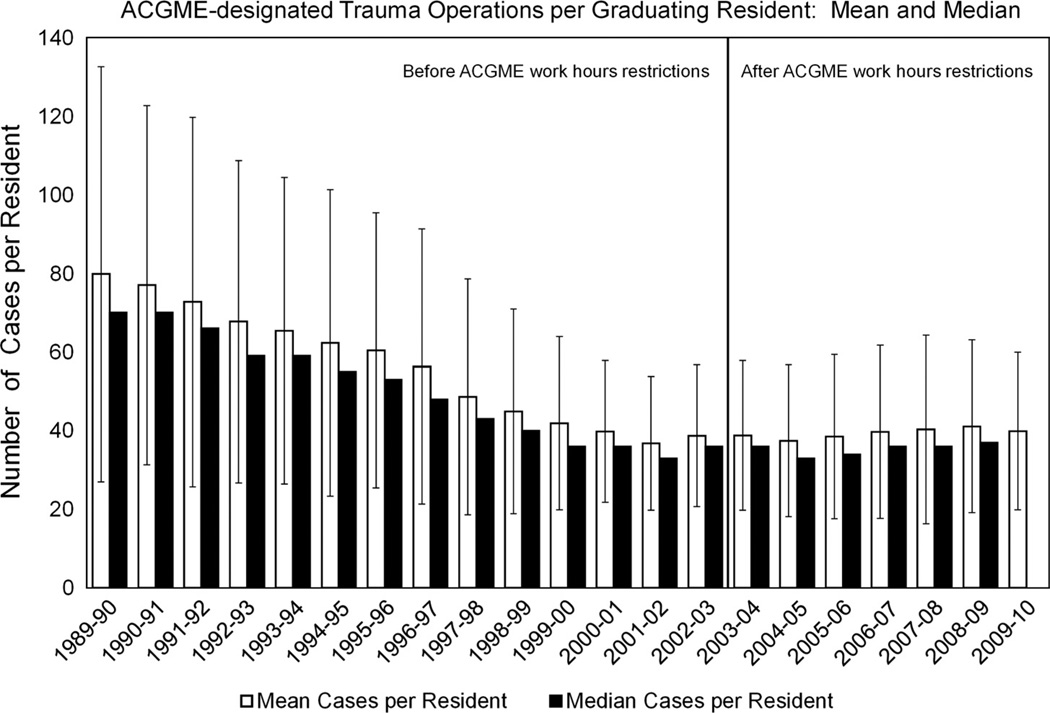
Table 1 shows an overall decline in ACGME-designated total trauma cases. Pairwise analysis demonstrated a significant decline from Period I to Period II (75.5 vs. 54.5 cases, p < 0.001), Period II to Period III (54.5 vs. 39.3 cases, p < 0.001) but no difference between Period III and Period IV (39.3 vs. 39.4 cases). Year-by-year analysis showed a similar trend (Fig. 2). SLR of the annual averages demonstrated that residents performed 2.11 fewer trauma cases each year (95% CI, −2.61 to −1.63) during the two-decade period. When SLR was stratified by decade, a change in slope was evident: during the first decade of data, average operative trauma declined by approximately 3.8 operations per year (95% CI, −4.16 to −3.35); in the second decade, there was no significant yearly change in number of trauma operations performed (95% CI, −0.27 to 0.40).
Figure 2.
ACGME-designated trauma operations per graduating resident: Mean and median. Bars indicate SD. No median available for AY2009–2010.
Specific Trauma Operations
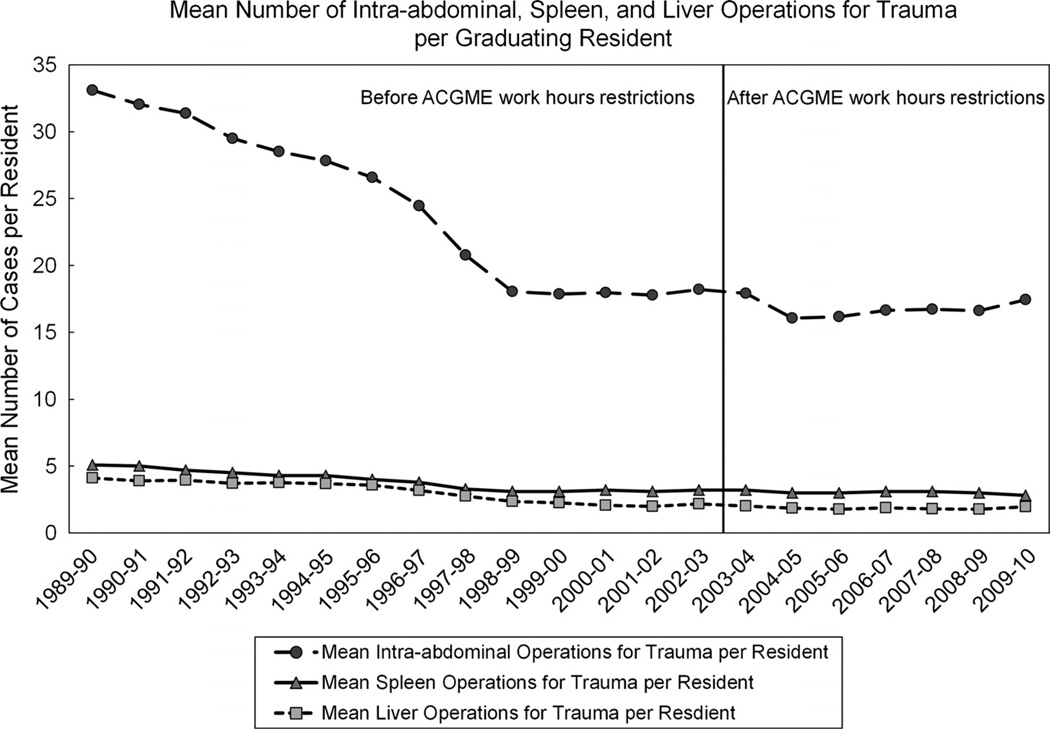
Trends for changes in individual procedures (all intra-abdominal trauma, spleen, and liver operations) were similar to ACGME-designated total trauma. Mean number of each declined significantly from Periods I to II to III (all p < 0.005) but not between Periods III and IV. Year-by-year analysis for individual operations revealed the same pattern. Figure 3 shows that graduating residents performed an average of 33 intra-abdominal trauma cases in AY1989–1999, which declined to 18 by the end of the first decade; the second decade was relatively unchanged, with an average of 16 to 17 cases performed per resident. SLR stratified by decade revealed a decline of 1.6 cases per resident per year for all intra-abdominal trauma during the first decade (95% CI, −1.9 to −1.2) but no significant decline during the second decade. Figure 3 also demonstrates reductions in spleen and liver cases. For spleen cases, stratified SLR showed a decline of 0.21 cases per year (95% CI, −0.25 to −0.18) during the first decade and an almost negligible decline of 0.02 cases per year (95% CI, −0.04 to −0.01) during the second decade. The pattern was nearly identical for liver cases.
Figure 3.
Mean number of intra-abdominal, spleen, and liver operations for trauma per graduating resident. The “Intra-abdominal Trauma” category was generated from subtotals of operations for esophageal, gastric, duodenal, small bowel, colon, splenic, hepatic, kidney, and pancreatic trauma, as well as repair of the abdominal aorta or vena cava and cases coded as trauma laparotomy or laparoscopy.
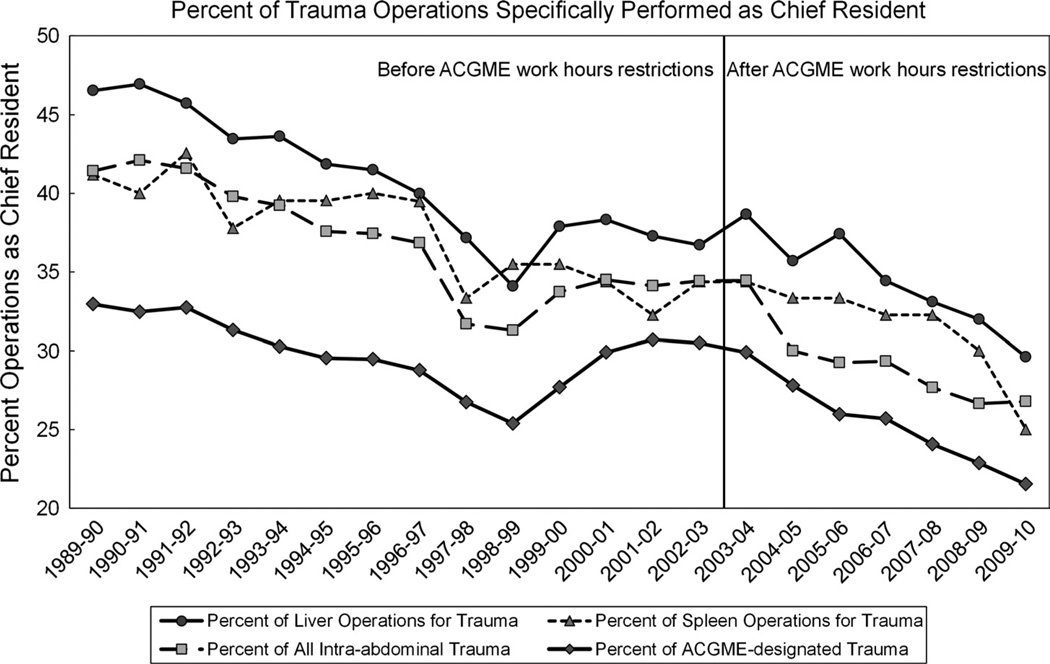
Trauma Cases in CR Year
Figure 4 shows the percent of trauma cases that were performed specifically during the CR year. During the 20 years of analysis, the percentage of trauma operative volume performed as CR declined. In the early 1990s, approximately 40% to 45% of intra-abdominal trauma operations were performed by residents in the chief year. By the late 2000s, this had declined to 25% to 30%. For each category or type of trauma case, SLR revealed a consistent and statistically significant decline in the percent of cases performed as CR.
Figure 4.
Percent of trauma operations specifically performed as CR. For each annual cohort of graduating residents, this figure displays the trauma cases specifically performed during the CR year as a percentage of all trauma cases performed during that cohort’s 5 years of residency.
DISCUSSION
Findings in a Historical Context
General surgery resident education in the United States is based on the Halstedian model of experiential training: residents are exposed to a broad range of experiences in operative and perioperative care, critical care, and nonoperative management of injury and illness. Whereas efforts are being made to alter this training model to one of benchmarks or milestones, the two decades covered by this review saw a training system largely based on the classic experiential model.
In 1982, Trunkey4 voiced concern over the adequacy of training in operative trauma in an address to the Society of University Surgeons. He noted that residents graduating in 1980 reported, on average, 22 trauma cases to the American Board of Surgery. Later that decade, resident exposure to operative trauma was demonstrated to have increased by Rotondo et al.,5 who showed that residents graduating in the late 1980s reported, on average, between 83 and 87 total trauma cases and 11 trauma laparotomies. However, by the late 1990s, single-center and national data were emerging that demonstrated a new decline in resident operative trauma experience.6–12
This review of ACGME case logs evaluated two decades of national data beginning at about the same time as the increases demonstrated by the Rotondo et al.5 study. The current study demonstrates that recently graduating surgical trainees performed an average of 39.4 ± 21 ACGME-designated trauma operations, which is about one half the number (72.5 ± 46) performed by graduates from two decades ago. This decline is concerning because several investigators have identified experience as one factor in the development toward competency.13,14 Limitations in trauma competency have important implications for the surgical workforce, and by identifying factors that influenced the decline in experience, adjustments may be made to increase experience. This study was designed to evaluate the relative contributions of changes in management strategies versus changes in resident work-hour rules.
At the beginning of this analysis, standard management of solid organ injury was still predominantly operative.15 However, beginning in 1989, favorable results from multicenter studies on blunt splenic injury prompted increasing acceptance of nonoperative management.15,16 By 1993 and 1997, a nationwide study found that 48% and 61%, respectively, of blunt splenic trauma was admitted for nonoperative management, and more recent analysis of the National Trauma Data Bank (2000–2004) found operative rates of only 26.6% for splenic injuries and 14.8% for liver injuries.17,18 This increasing adoption of a nonoperative approach is reflected in the resident-level data from the ACGME. Significant declines were seen in all intra-abdominal trauma operations, most sharply throughout the 1990s.
Another potential contributor to the overall decline in trauma operations for surgical residents may have been implementation of work-hour restrictions. Substantial discussion has been generated over the potential effects that duty-hour restrictions would have on training. There was widespread apprehension by surgical educators and trainees alike that time reductions would lead to reductions in surgical experience.19–21 There have been conflicting conclusions, with some articles showing no change2,3,22–26 and others showing a decline in operative experience of almost 20%.27,28,29
In this review of ACGME data, a marked difference is apparent when trauma operations are compared with TMC. Between Periods I and II, while TMC increased, each category or type of trauma operation decreased. Between Periods II and III, while TMC remained constant, the decline in trauma operations continued. Most notably, between Periods III (pre–work-hour restriction) and IV (post–work-hour restrictions), TMC decreased, but there was no decline in any of the trauma operations reviewed. These data support the conclusion that duty-hour restrictions have not contributed substantially to the overall decline in trauma cases.
In light of the overall decline, the current study was also designed to evaluate whether there were discernable changes in the distribution of operative experience between the junior and senior years of residency. The underlying assumption was that surgery programs might have compensated for the overall drop in operative trauma by making it possible for senior residents (R3–R5) to perform a greater percentage of cases. Although the ACGME case logs do not distinguish the year of residency in which procedures are performed, the number of cases performed specifically during the CR year is recorded. The ACGME data suggest that the percentage of trauma cases performed by CRs has in fact declined. There are several potential reasons for this finding. First, rotations may have been adjusted so that CRs spend less time on trauma teams. Moreover, now that “night-float” systems are common, CRs may take less (or no) overnight in-house call, reducing the number of potential cases. In both of these scenarios, trauma rotations in the third or fourth clinical year (considered “senior” in many programs) would produce operative trauma experience not captured by the “CR” designation in the ACGME case logs. However, this decrease in chief-year experience compounds concerns raised by the overall decline in trauma experience and may justify consideration of restructuring resident rotations: CRs perform cases with more autonomy than their junior colleagues, which may optimize learning during these increasingly infrequent operations.
Limitations
There are several limitations to bear in mind when evaluating these data. The current online case logging system went live in July 2001. Surgical trainees frequently enter cases as they complete them, which may produce a log that closely matches trainee operative experience. Before this, trainees accumulated and stored their data until completion of residency, which may have increased inaccurate reporting. Both systems rely on human input, and presumably, some level of misclassification has happened continuously, but there may be differences attributable to the type of case logging system. In addition, residents can log only one operation per patient per day; other procedures during the same case are not counted and other procedures during reoperation on the same day are not counted. Since AY2003–2004, the RRC has required surgery residents to log 30 trauma cases (10 operative and 20 nonoperative cases). Before that, the requirement was 16 trauma cases.30 As residents may stop logging cases after they reach the required numbers, this may lead to an underrepresentation of operative experience for residents after 2004; however, trauma operations beyond the required minimum still count toward TMC, which would encourage residents to log all cases.
Summary statistics for a cohort of 1,000 graduating surgery residents cannot be used to accurately predict the operative volume of any individual resident or any individual program; however, the summary statistics analyzed and presented here do have use in evaluating trends over time for surgical education in the United States.
Finally, although case numbers may be useful in assessing technical competence, operative volume alone does not define surgical competence.31 Educators should not lose sight that the true goal of surgical training is a well-rounded surgical professional with good judgment and the ability to manage patients both inside and outside the operating room.32 We assume that performance of nearly 80 trauma operations (as for graduates in 1990) is better preparation for future operative trauma than performance of 40 operations (as for 2010 graduates); this difference is not only difficult to quantify but also it is likely highly variable among individual trainees.32 Despite this caveat, and in the absence of data correlating patient outcomes to era of training, resident case numbers are perhaps the only viable tool for assessing operative competence of the new surgical workforce relative to their predecessors.
CONCLUSIONS
ACGME case log data suggest that as blunt trauma and solid organ injury became an increasingly nonoperative condition, resident experience in operative trauma has also diminished. Work-hour restrictions did not contribute substantially to the changes seen during the last two decades, although they may complicate efforts to increase resident experience in operative trauma. This reduction in experience may represent a limitation in preparedness for general surgeons who care for trauma patients, which may be especially pertinent to those who will practice in areas remote from high-level trauma centers.
It has been increasingly recognized that case numbers and years spent in residency are insufficient for measuring competence. But experience in the operative room is essential, and the data presented in this review suggest that creative solutions are required to improve experience in operative trauma; some have proposed the use of simulators10,33 or the development of a structured skills and benchmark-based curriculums.34,35 Surgical educators and leaders in trauma surgery must meet the challenge of training residents in procedures less frequently performed.
Footnotes
This study was presented at the 42nd annual meeting of the Western Trauma Association, February 26–March 2, 2012, in Vail, Colorado.
AUTHORSHIP
All authors contributed to this study’s design. F.T.D., S.A., and C.R.H. collected the data. F.T.D. and C.R.H. analyzed the data, which all authors interpreted. All authors participated in writing and revising the manuscript.
DISCLOSURE
The authors declare no conflicts of interest.
REFERENCES
- 1.National Center for Injury Prevention and Control: WISQARS (Web-Based Injury Statistics Query and Reporting System). Centers for Disease Control and Prevention National Center for Injury Prevention and Control (NCIPC) [Accessed September 2011];2011 Available at: www.cdc.gov/injury.
- 2.Simien C, Holt KD, Richter TH, et al. Resident operative experience in general surgery, plastic surgery, and urology 5 years after implementation of the ACGME duty hour policy. Ann Surg. 2010;252:383–389. doi: 10.1097/SLA.0b013e3181e62299. [DOI] [PubMed] [Google Scholar]
- 3.Bland KI, Stoll DA, Richardson JD, Britt LD. Members of the Residency Review Committee-Surgery. Brief communication of the residency review committee-surgery (RRC-S) on residents’ surgical volume in general surgery. Am J Surg. 2005;190:345–350. doi: 10.1016/j.amjsurg.2005.06.036. [DOI] [PubMed] [Google Scholar]
- 4.Trunkey DD. Society of University Surgeons. Presidential address: on the nature of things that go bang in the night. Surgery. 1982;92:123–132. [PubMed] [Google Scholar]
- 5.Rotondo MF, McGonigal MD, Schwab CW, Kauder DR, Angood PB. On the nature of things still going bang in the night: an analysis of residency training in trauma. J Trauma. 1993;35:550–553. doi: 10.1097/00005373-199310000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins ML, Wynn JJ, Schmacht DC, Medeiros RS, Gadacz TR. Nonoperative management of liver and/or splenic injuries: effect on resident surgical experience. Am Surg. 1998;64:552–556. [PubMed] [Google Scholar]
- 7.Jennings GR, Poole GV, Yates NL, Johnson RK, Brock M. Has nonoperative management of solid visceral injuries adversely affected resident operative experience? Am Surg. 2001;67:597–600. [PubMed] [Google Scholar]
- 8.Bulinski P, Bachulis B, Naylor DF, Jr, Kam D, Carey M, Dean RE. The changing face of trauma management and its impact on surgical resident training. J Trauma. 2003;54:161–163. doi: 10.1097/00005373-200301000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Engelhardt S, Hoyt D, Coimbra R, Fortlage D, Holbrook T. The 15-year evolution of an urban trauma center: what does the future hold for the trauma surgeon? J Trauma. 2001;51:633–637. doi: 10.1097/00005373-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Bittner JG, 4th, Hawkins ML, Medeiros RS, et al. Nonoperative management of solid organ injury diminishes surgical resident operative experience: is it time for simulation training? J Surg Res. 2010;163:179–185. doi: 10.1016/j.jss.2010.05.044. [DOI] [PubMed] [Google Scholar]
- 11.Lukan JK, Carrillo EH, Franklin GA, Spain DA, Miller FB, Richardson JD. Impact of recent trends of noninvasive trauma evaluation and nonoperative management in surgical resident education. J Trauma. 2001;50:1015–1019. doi: 10.1097/00005373-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Fakhry SM, Watts DD, Michetti C, Hunt JP EAST Multi-Institutional Blunt Hollow Viscous Injury Research Group. The resident experience on trauma: declining surgical opportunities and career incentives? Analysis of data from a large multi-institutional study. J Trauma. 2003;54:1–7. doi: 10.1097/00005373-200301000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Compeau C, Tyrwhitt J, Shargall Y, Rotstein L. A retrospective review of general surgery training outcomes at the university of Toronto. Can J Surg. 2009;52:E131–E136. [PMC free article] [PubMed] [Google Scholar]
- 14.Suwanabol PA, McDonald R, Foley E, Weber SM. Is surgical resident comfort level associated with experience? J Surg Res. 2009;156:240–244. doi: 10.1016/j.jss.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Peitzman AB, Richardson JD. Surgical treatment of injuries to the solid abdominal organs: a 50-year perspective from the journal of trauma. J Trauma. 2010;69:1011–1021. doi: 10.1097/TA.0b013e3181f9c216. [DOI] [PubMed] [Google Scholar]
- 16.Cogbill TH, Moore EE, Jurkovich GJ, et al. Nonoperative management of blunt splenic trauma: a multicenter experience. J Trauma. 1989;29:1312–1317. doi: 10.1097/00005373-198910000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Peitzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: multi-institutional study of the eastern association for the surgery of trauma. J Trauma. 2000;49:177–187. doi: 10.1097/00005373-200008000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Tinkoff G, Esposito TJ, Reed J, et al. American association for the surgery of trauma organ injury scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg. 2008;207:646–655. doi: 10.1016/j.jamcollsurg.2008.06.342. [DOI] [PubMed] [Google Scholar]
- 19.Drolet BC, Spalluto LB, Fischer SA. Residents’ perspectives on ACGME regulation of supervision and duty hours–a national survey. N Engl J Med. 2010;363:e34. doi: 10.1056/NEJMp1011413. [DOI] [PubMed] [Google Scholar]
- 20.Pape HC, Pfeifer R. Restricted duty hours for surgeons and impact on residents quality of life, education, and patient care: a literature review. Patient Saf Surg. 2009;3:3. doi: 10.1186/1754-9493-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antiel RM, Thompson SM, Hafferty FW, et al. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86:185–191. doi: 10.4065/mcp.2010.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jamal MH, Rousseau MC, Hanna WC, Doi SA, Meterissian S, Snell L. Effect of the ACGME duty hours restrictions on surgical residents and faculty: a systematic review. Acad Med. 2011;86:34–42. doi: 10.1097/ACM.0b013e3181ffb264. [DOI] [PubMed] [Google Scholar]
- 23.Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243:864–871. doi: 10.1097/01.sla.0000220042.48310.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin S, Britt R, Britt LD. Effect of the 80-hour work week on resident case coverage: corrected article. J Am Coll Surg. 2008;207:148–150. doi: 10.1016/j.jamcollsurg.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Shin S, Britt R, Doviak M, Britt LD. The impact of the 80-hour work week on appropriate resident case coverage. J Surg Res. 2010;162:33–36. doi: 10.1016/j.jss.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Spencer AU, Teitelbaum DH. Impact of work-hour restrictions on residents’ operative volume on a subspecialty surgical service. J Am Coll Surg. 2005;200:670–676. doi: 10.1016/j.jamcollsurg.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 27.Fairfax LM, Christmas AB, Green JM, Miles WS, Sing RF. Operative experience in the era of duty hour restrictions: is broad-based general surgery training coming to an end? Am Surg. 2010;76:578–582. [PubMed] [Google Scholar]
- 28.Sadaba JR, Urso S. Does the introduction of duty-hour restriction in the united states negatively affect the operative volume of surgical trainees? Interact Cardiovasc Thorac Surg. 2011;13:316–319. doi: 10.1510/icvts.2011.270363. [DOI] [PubMed] [Google Scholar]
- 29.Damadi A, Davis AT, Saxe A, Apelgren K. ACGME duty-hour restrictions decrease resident operative volume: a 5-year comparison at an ACGME-accredited university general surgery residency. J Surg Educ. 2007;64:256–259. doi: 10.1016/j.jsurg.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 30.Residency Review Committee (RRC) Newsletter. 2002 Aug [Google Scholar]
- 31.Margenthaler JA. The impact of duty hours on surgical resident education: are operative logs appropriate surrogates for surgical competence? J Surg Res. 2010;164:216–217. doi: 10.1016/j.jss.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Grasberger RC, McMillian TN, Yeston NS, Williams LF, Hirsch EF. Residents’ experience in the surgery of trauma. J Trauma. 1986;26:848–850. doi: 10.1097/00005373-198609000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Knudson MM, Khaw L, Bullard MK, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma. 2008;64:255–263. doi: 10.1097/TA.0b013e31816275b0. [DOI] [PubMed] [Google Scholar]
- 34.Gunst M, O’Keeffe T, Hollett L, et al. Trauma operative skills in the era of nonoperative management: the trauma exposure course (TEC) J Trauma. 2009;67:1091–1096. doi: 10.1097/TA.0b013e3181bc77ba. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs LM, Burns KJ, Kaban JM, et al. Development and evaluation of the advanced trauma operative management course. J Trauma. 2003;55:471–479. doi: 10.1097/01.TA.0000059445.84105.26. [DOI] [PubMed] [Google Scholar]