Abstract
Background
General surgery resident training has changed dramatically over the past 2 decades, with likely impact on specialty exposure. We sought to assess trends in general surgery resident exposure to thoracic surgery using the Accreditation Council for Graduate Medical Education (ACGME) case logs over time.
Methods
The ACGME case logs for graduating general surgery residents were reviewed from academic year (AY) 1989–1990 to 2011–2012 for defined thoracic surgery cases. Data were divided into 5 eras of training for comparison: I, AY89 to 93; II, AY93 to 98; III, AY98 to 03; IV, AY03 to 08; V, AY08 to 12. We analyzed quantity and types of cases per time period. Student t tests compared averages among the time periods with significance at a p values less than 0.05.
Results
A total of 21,803,843 general surgery cases were reviewed over the 23-year period. Residents averaged 33.6 thoracic cases each in period I and 39.7 in period V. Thoracic cases accounted for nearly 4% of total cases performed annually (period I 3.7% [134,550 of 3,598,574]; period V 4.1% [167,957 of 4,077,939]). For the 3 most frequently performed procedures there was a statistically significant increase in thoracoscopic approach from period II to period V.
Conclusions
General surgery trainees today have the same volume of thoracic surgery exposure as their counterparts over the last 2 decades. This maintenance in caseload has occurred in spite of work-hour restrictions. However, general surgery graduates have a different thoracic surgery skill set at the end of their training, due to the predominance of minimally invasive techniques. Thoracic surgery educators should take into account these differences when training future cardiothoracic surgeons.
Surgery training has evolved over time, with dramatic changes occurring over the past 2 decades. Not only has the scope of disease treated by the general surgeon narrowed and shifted, but residency training paradigms themselves are radically different. One of the most significant changes that have occurred is the implementation of the 80 hour work week restriction in 2003. Concerns have arisen about the impact of work hour restrictions on resident education and operative training, including both quantity and variety of cases being performed during residency. On an institutional level, many program directors have responded to new work hour restrictions by limiting general surgery resident clinical time on subspecialty services.
There is a perception that with changes in residency training there has been less exposure to cardiothoracic surgery for the general surgery trainee. This is concerning for many educators as exposure to thoracic surgery is considered important to attracting the best and brightest to the field. The objective of this study was to analyze trends in resident operative experience within the defined category of thoracic surgery. We sought to evaluate both trends in overall operative experience and the types of general thoracic cases being performed by general surgical residents.
Material and Methods
Description of the Data Source
A request was made to the Accreditation Council for Graduate Medical Education (ACGME) for all available case log data for general surgery residents. General surgery residents log individual operative experience in the ACGME database during all 5 years of clinical training. The ACGME compiles this individual data and generates summary statistics annually. For our study, we obtained the summary reports of all graduating general surgery residents from academic year (AY) 1989 to 1990 through AY 2011 to 2012. Focusing on the defined category of Thoracic Surgery, we analyzed the data by dividing into 5 cohorts: period I (AY1989–90 to AY1992–93); period II (AY1993–94 to AY1997–98); period III (AY1998–99 to AY2002–03); period IV (AY2003–04 to AY2007–08); and period V (AY2008–09 to AY2011–2012). Period IV was delineated by implementation of work hour restrictions in 2003, representing the era of trainees with some portion of their training prior to restrictions. Period V comprised the first era of residents trained entirely within the 80-hour work week.
Analytic Methods
Yearly averages of total major thoracic surgery cases performed by graduating general surgery residents were calculated for each academic year, as well as the percentage of total surgical cases that were in the defined category of thoracic surgery. Trends were assessed with respect to case numbers over time in the defined eras of training both for total major surgical cases and for total thoracic surgical cases. Examining data in the context of era of training helped to eliminate the impact of any 1 year of training skewing overall trends. An unpaired Student t test was used to compare annual averages within each period to the next period of training, with statistical significance set at a p value less than 0.05. An exploratory assessment of cardiac surgery experience was performed as well. Over the time period of the study, the number of cardiac surgery cases per resident was so small (less than 4 on average) that there were no observable trends in these data. Thus, we focused on general thoracic cases only for the purposes of this study.
In order to evaluate specific trends over time in operative exposure, we looked at the most frequently performed thoracic operations for comparison. Exploratory procedures (thoracotomy or thoracoscopy), wedge resections, and lobectomies or segmentectomies were the 3 most frequently performed procedures over the years of study. Within these 3 categories specifically, we divided the case numbers into those performed in an open manner versus those performed thoracoscopically. This could only be completed for periods II to V, as there was not a specific code to log thoracoscopic procedures prior to 1993. Total numbers of cases performed in either an open or thoracoscopic fashion were then assessed from period II through period V, and the unpaired Student t test utilized to compare eras of training (significance p < 0.05).
Results
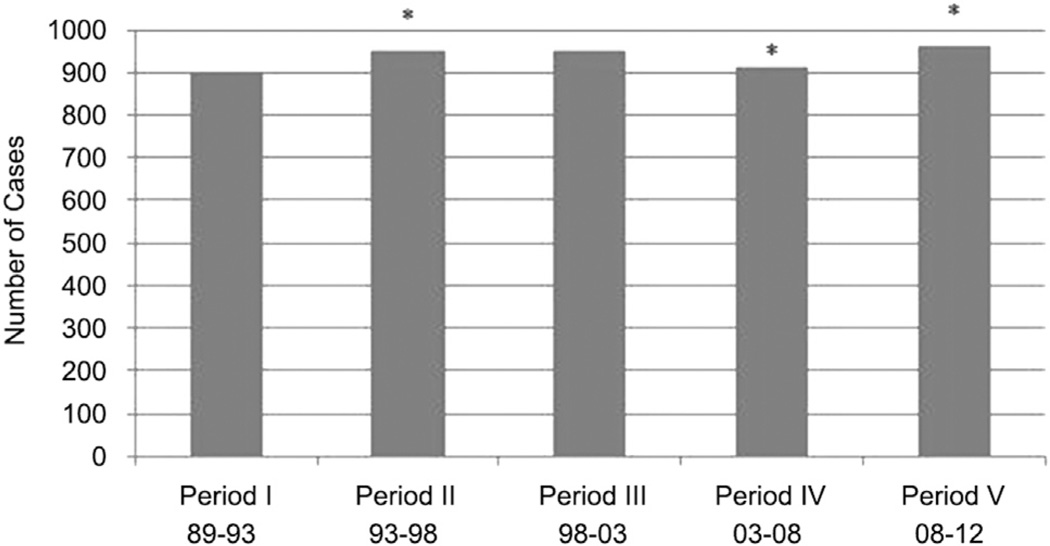
The 21,803,843 surgery cases logged by 23,334 graduating residents were reviewed over the 23 year time period of study (AY 1989–1990 through AY 2011–2012). Analysis of total major cases performed per resident (Fig 1) showed a significant decline in period IV with the implementation of work hours followed by a significant increase the following period. The maximum number of cases per resident was in period V at 962 cases per resident, and the lowest number was in period I at 899 cases per resident.
Fig 1.
Total major cases per resident on average within defined time periods of training. Asterisks (*) denote significant changes in mean case numbers compared with the immediately previous period.
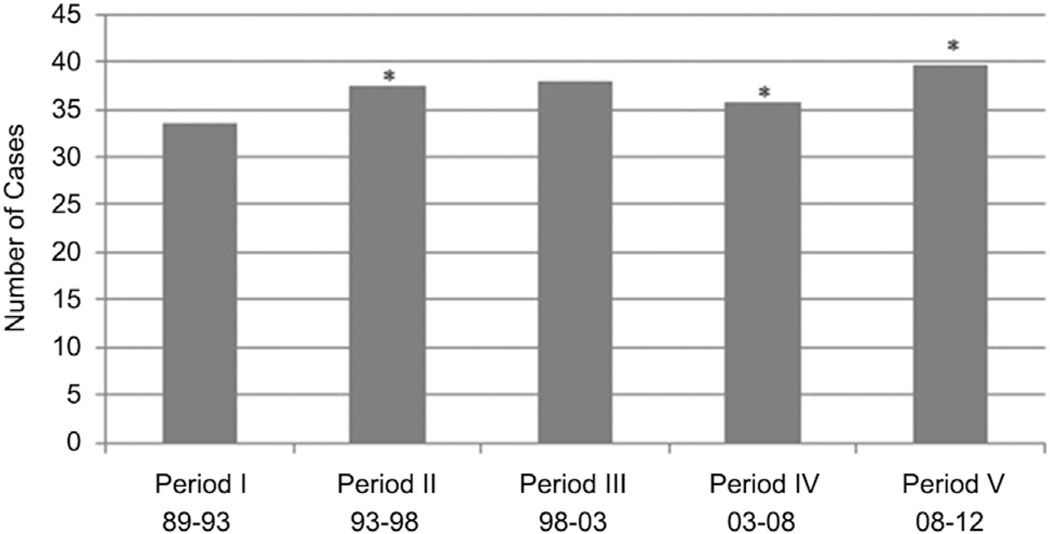
A similar trend in major thoracic surgery cases was seen (Fig 2). Although there was a decline in period IV soon after implementation of work-hour restrictions, the average number of thoracic operations completed by each graduating resident over their 5-year period of training increased from 33.6 cases in period I to 39.7 cases in period V (Table 1). For each period of training, thoracic major cases comprised a similar proportion of total resident operative experience, approximately 4% of the overall case log.
Fig 2.
Total major cases within the defined category of thoracic surgery per resident defined by era of training. Asterisks (*) denote significant changes in mean case numbers compared with the immediately previous period.
Table 1.
Average Thoracic and Total Major Cases per Resident for Each Period of Training
| Period | Thoracic Cases | Total Major Cases | % Thoracic/ Total Cases |
||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| I | 32.5 | 34.8 | 33.60 ± 1.04 | 873.4 | 921.9 | 899.1 ± 20.33 | 3.74% |
| II | 35.5 | 38.4 | 37.36 ± 1.17 | 923.9 | 961.3 | 943.68 ± 14.15 | 3.96% |
| III | 36.7 | 39.3 | 37.86 ± 1.05 | 929.7 | 966.5 | 950.22 ± 15.75 | 3.98% |
| IV | 34.4 | 36.9 | 35.74 ± .90 | 900.2 | 931.9 | 912.98 ± 11.74 | 3.91% |
| V | 37.2 | 41.9 | 39.70 ± 1.99 | 943 | 980 | 962.43 ± 15.30 | 4.12% |
Max = maximum number of cases; Min = minimum number of cases.
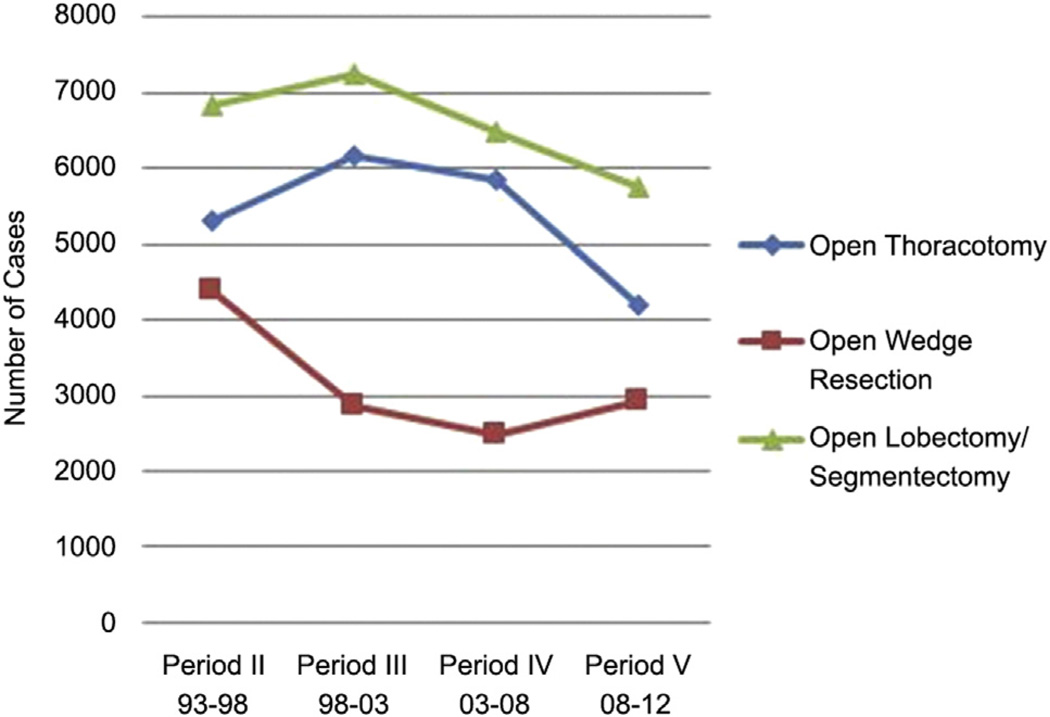
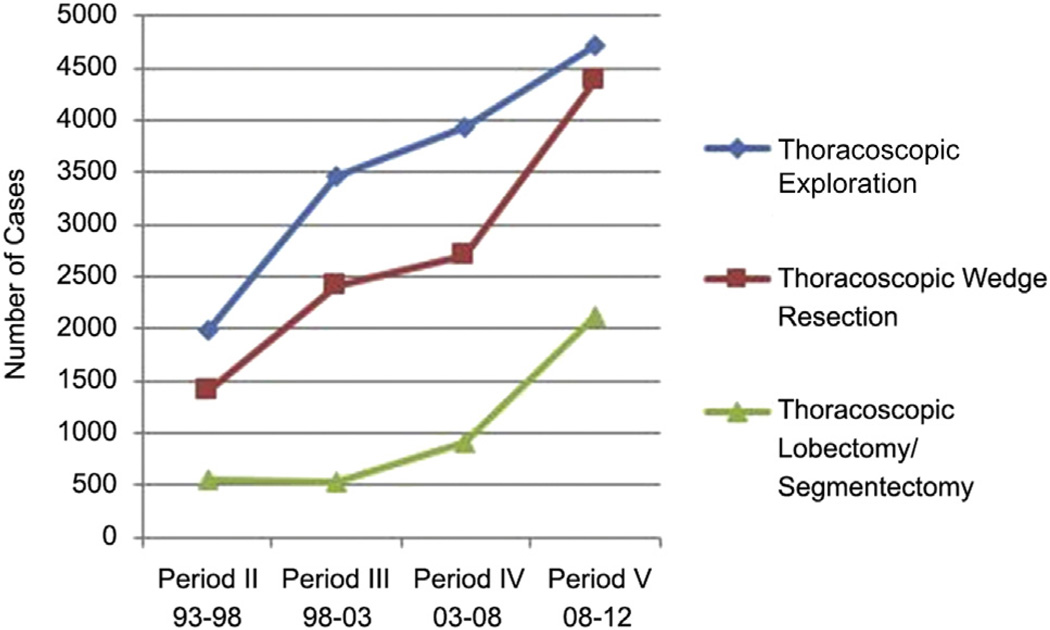
When looking specifically at the types of procedures performed within the defined category of thoracic surgery, the 3 most frequently performed operations were exploratory (thoracotomy or thoracoscopy), wedge resections, and lobectomies or segmentectomies. A comparison of approach (open versus minimally invasive) for the 3 most commonly performed procedures was completed. As there were no specific codes for open and thoracoscopic approach during period I, results from this time period were excluded from further analysis. In period II the open approach was the most commonly used for all 3 of these procedures. Figure 3 illustrates the decline in open surgical approach over the time period of study. In contrast to Figure 3, Figure 4 demonstrates increasing utilization of minimally invasive techniques (thoracoscopy) over time. On an individual resident level, these trends were also mirrored. Table 2 shows a comparison of the average number of these specific procedures each resident performed in period II and period V. There was a significant increase in the number of thoracoscopic approaches for the 3 procedure subtypes on an individual resident basis. There were significantly less open approaches for exploratory thoracotomies and lobectomies or segmentectomies. While there was also a decrease in open wedge resections, the difference was not significant.
Fig 3.
Trends in performance of open thoracotomy, open wedge resections, and open lobectomies or segmentectomies from period II to V.
Fig 4.
Trends in thoracoscopic exploratory procedures, thoracoscopic wedge resections, and thoracoscopic lobectomies or segmentectomies from period II–V.
Table 2.
Individual Resident Experience With Specific Procedure Types: Period II Versus Period V
| Procedure Type | Period II AY93–94 to AY97–98 |
Period V AY08–09 to AY11–12 |
p Value | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| Open thoracotomy | 4.9 | 5.9 | 5.3 ± .4 | 4.1 | 4.8 | 4.3 ± .4 | 0.0144 |
| Thoracoscopic exploration | 1.1 | 2.7 | 2.0 ± .7 | 4.4 | 4.8 | 4.7 ± .17 | 0.0001 |
| Open wedge resection | 3.3 | 6.9 | 4.3 ± 1.5 | 1.2 | 4.5 | 2.5 ± 1.8 | 0.1551 |
| Thoracoscopic wedge resection | 0.2 | 1.9 | 1.4 ± .7 | 2.8 | 4.8 | 4.1 ± 1.1 | 0.0050 |
| Open lobectomy/segmentectomy | 4.9 | 7.7 | 6.8 ± 1.1 | 1.2 | 5.6 | 4.2 ± 2.1 | 0.0435 |
| Thoracoscopic lobectomy/segmentectomy | 0.4 | 0.7 | 0.6 ± .1 | 1.8 | 4.8 | 2.9 ± 1.3 | 0.0047 |
AY = academic year; Max = maximum number of cases; Min = minimum number of cases.
Comment
General surgery residency training has undergone important changes over the last 2 decades. In the midst of these changes, the goal continues to be the training of well-rounded surgeons who may either enter general surgery practice or successfully transition to the subspecialty of choice [1]. To provide the foundation to train learners in a broad range of skills continues to challenge surgical educators, especially with external influences such as duty-hour restrictions [2, 3], introduction of minimally invasive surgery [3, 4], and the dramatic rise in subspecialty fellowships. One area that has not been previously studied is the education of general surgery residents in thoracic surgery. As there is a general perception that there is declining exposure during general surgery training to the field of cardiothoracic surgery [5], we sought to define the changes that have occurred with the operative experience over the last 2 decades.
The major finding from this review is that the average total thoracic cases performed by general surgery residents has remained stable, comprising approximately 4% of the overall operative experience. When viewed in the context of the duty-hours restrictions that were introduced in period IV the thoracic cases did drop for this period, but by period V had rebounded. Therefore, we along with others [6, 7] conclude that duty-hour restrictions have had minor effects on the thoracic surgery operative experience. This maintenance of thoracic operative experience may be attributable to having an unchanged ACGME requirement of 15 thoracic surgical cases prior to graduation. However, over this same time, despite a similar requirement, there has been a marked decline in the operative experience for pediatric surgery [8]. This may imply that thoracic surgery is perceived as a core rotation and has been maintained during the changes that followed implementation of the duty-hour restrictions [2]. However, while these figures are reassuring, the overall numbers do not tell the entire story.
An analysis of the specific types of thoracic cases that general surgery residents performed showed that exploratory thoracic procedures and lung resections (wedge resections and lobectomies or segmentectomies) comprised over half of all the cases performed. On average, a general surgery resident will have performed about 20 of these cases during their training. Whether this is considered adequate to achieve competence is difficult to answer and is likely resident specific and experience dependent. Additional operative experience can be gained as a first assistant as well. Unfortunately, we do not have the number of first-assist cases within this dataset and thus cannot determine the overall amount of time residents spend within the operating room observing versus participating in thoracic surgical procedures. The overall experience level could only be enhanced by participation in more first-assist cases in addition to those performed as primary surgeon.
The ACGME case logs began providing information on the approach used for thoracic surgery cases starting in AY93 to 94 (the beginning of period II). The rise of minimally invasive cases has been accompanied by a fall in the open counterpart, which mirrors the entire field of surgery [4]. The introduction of thoracoscopy has been a benefit to patients but a challenge to surgical educators [9]. Specifically, while the minimally invasive surgical (MIS) procedures may be similar, they do call for a different skill set from open surgery. Indeed some would argue that MIS skills are more challenging to acquire than open procedures [10]. The procedures require the learner to build a sufficient foundation before undertaking more challenging MIS cases [11, 12]. This has led to a shift in which performance of challenging MIS cases occurs during the senior years of residency [13]. Also, with the addition of thoracoscopic procedures, residents must now learn 2 different approaches to the same operation [14]. Ultimately, it has been shown that with the advent of MIS, residents feel less competent after completing general surgery training [6, 15], which bodes poorly as far as the ability to offer these services in practice.
There are many reasons for general surgery residents to continue to train in thoracic surgery. One reason is to provide general surgery residents with the requisite skills to be able to perform those operations in practice. Indeed, studies continue to show that thoracic procedures are being performed by practicing general surgeons, although only accounting for less than 2% of cases [16, 17]. However, if residents continue to feel uncomfortable with their operative skills at the end of residency, the now declining numbers of thoracic surgery cases being offered by general surgeons may continue to fall [18]. This will thereby compound the predicted shortage of a thoracic surgery workforce due to retiring surgeons and an aging population [19–21]. A recent study [21] predicts that in the near future there will be a shortage of almost 2,000 cardiothoracic surgeons in the US. As such, thoracic surgery should remain a component of general surgery practice to some degree.
Another reason to train general surgery residents in thoracic surgery is to attract new trainees into the field [22–25]. There has been much written recently regarding the decline in popularity of cardiothoracic surgery as a career [23] due to a perceived poor job outlook [19, 26], lack of job security, excessive length of training, and concerns over perceived poor work-life balance [24, 27, 28]. However, about a tenth of general surgery residents currently are considering cardiothoracic surgery as a career [29]. Exposure to thoracic surgery as a general surgical resident may foster interest, especially when the case selection is broad and there is good mentorship [29].
Another training initiative that has been recently introduced is the 6-year integrated thoracic surgery residency, where medical students may match directly into thoracic surgery, thereby shortening the years of training by 1 or 2 years [25, 30]. Recent studies have shown that there has been a rise in applicants [31] and that the quality of applicant has been excellent [32], thereby providing hope that the field will continue to attract the best and brightest. However, the operative experience of the integrated thoracic surgery resident needs to be monitored for possible siphoning of cases away from general surgery residents. Because this new pathway to thoracic surgery has only recently begun, it is too early to see any effects in the ACGME case logs. An additional avenue to provide more cardiothoracic surgery exposure to resident trainees is the 7-year program combining both general surgery and thoracic surgery with the end result of both General and Thoracic Surgery Board Certification. While this is an approved training pathway, there are few programs adopting this paradigm as of yet.
In the midst of the above changes in training paradigms, our study shows that current general surgical resident trainees are participating in the same amount of cardiothoracic surgery cases as their predecessors over the past 20 years. The main strength of our study is that the time period examined was large enough to include a significant number of trainees both pre- and post-work-hour restriction implementation. Furthermore, rather than focusing on an individual institution’s experience, we looked at the national trends, which are more applicable to fellowship directors and surgical educators at the post-residency level. Unfortunately there are inherent limitations in using a database such as the ACGME case log for data analysis. First, trainees began entering data online in July 2001, which likely contributed to real-time data entry rather than retrospective. This change may have resulted in increased documentation and potential increase in case numbers. Similarly another ACGME policy change in July 2011 allowed more than 1 resident to log components of a single procedure, which could have contributed to inflated case numbers in that academic year alone. Fortunately, this likely had no influence on the numbers reported in our study as this was only applicable to 1 year of data (2011 to 2012). It is unlikely chief residents in that year performed a significant number of thoracic cases that were recorded by other residents as well.
Despite these overall limitations in a large national database, the numbers are reassuring that work-hour implementation has not completely redefined resident operative experience both as a general surgeon trainee and as a potential cardiothoracic fellowship applicant. For the past 23 years, there has been a stable proportion of overall operative experience devoted to cardiothoracic surgery (roughly 4% of total major cases). This cardiothoracic exposure has changed greatly from only open techniques to an approximately equal amount of exposure to both thoracoscopic and open techniques. This in turn may lead to challenges as trainees try to achieve competence in 2 different approaches to the same type of procedure. Fellowship educators should take into account the changing experience of the general surgery residency graduate, so as to adequately approach their post-residency education.
DISCUSSION
DR SIDHU P. GANGADHARAN (Boston, MA): Great presentation. Would you comment on the effect of the total number of cases available to residents and the fact that thoracic cases may be considered a highly desirable case to do. Meaning if you had to pick between doing your fiftieth gallbladder and your second lobe, you would preferentially sort of skew towards the thoracic cases, and that may inform some of the preservation of case numbers despite the work-hour restrictions.
DR KANSIER: Thank you for your question. On an anecdotal level, I certainly would choose a lobectomy as opposed to doing a fiftieth gallbladder, and so would many residents at our institution. However, at least at the University of Washington, the way the rotations are structured, you are only on cardiothoracic at a certain time period, and, as such, cannot choose different procedures during the time that you are on that subspecialty rotation. I believe the opportunity to participate in these cases is more or less the same, as most residency programs are likely structured in a similar manner.
DR SCOTT I. REZNIK (Temple, TX): Do you think your numbers would have been the same had you included some of the laparoscopic foregut surgeries, like Heller myotomy or Nissen? Both of those operations have proliferated, and with minimally invasive general surgery training and fellowships fewer thoracic surgeons or a larger percentage of general surgeons may be doing those operations.
DR KANSIER: Thank you for your question. Yes, I anticipate that those have likely increased, maybe even more dramatically than the thoracoscopic approaches to these operations, and that likely would have inflated the thoracic case numbers even further if these were logged under this category, which they are not.
DR ELENA ZIARNIK (Nashville, TN): Did you look at the breakdown regarding how they delineated what their role was in the surgery regarding a first assistant, surgeon junior, teaching, what participation they had as residents?
DR KANSIER: Thank you for your question. All of the cases that we presented here are either surgeon junior or surgeon senior. First assistant and teaching assistant are not included in this data. Some of our other colleagues have looked at the breakdown between surgeon junior and surgeon senior and for the cardiothoracic data predominantly the juniors are the ones performing these operations. But we have to remember that with the ACGME [Accreditation Council for Graduate Medical Education] case log, surgeon junior means any resident years 1 through 4. The only people who are allowed to log surgeon senior cases are a chief resident/R5, and they are much less likely to be participating on a subspecialty service such as cardiothoracic. That is likely why those residents are not logging a lot of these cases.
DR ANTHONY L. ESTRERA (Houston, TX): That was a very nice presentation.
What would be intriguing, if you have the detail, is to see if the results differed with general surgery programs that had affiliated or associated thoracic programs. This would be interesting to see.
DR KANSIER: Absolutely. I definitely agree. Thank you.
DR RYAN MACKE (Madison, WI): Did you look at the cardiac numbers? I know during my training, there was this kind of shift where cardiac rotations disappeared. PAs (physician assistants) were doing a lot of the work and general surgery residents were getting less of a cardiac experience. In those time periods, did you see a trend in decreasing cardiac cases?
DR KANSIER: Thank you for your question. We did look at that. Unfortunately, the number of cardiac procedures that general surgery residents log is so low, on upwards of 3 or 4 cases total, and the way that they are logged is just under the heading “Cardiac Procedures.” So there is not a lot of leeway for interpreting what residents are actually doing. Over the time course of our study, they were doing 3 or 4 cases each, but it is hard to tell exactly what they were doing. Either way you look at it, numbers are low.
DR LISA M. BROWN (St. Louis, MO): Do you think there would be a difference if you examined the experience that a resident would obtain on thoracic surgery rotations during general surgery based upon where you trained? There are some surgery programs with high volume thoracic surgery divisions. It is likely that general surgery residents at these programs still get a fair amount of exposure to thoracic surgery. In other programs, the exposure to thoracic surgery is minimal. Other general surgery subspecialties have filled in these gaps and thoracic surgery is taking more of a back seat. Have you thought about comparing the number of thoracic cases done, time spent on service, and at what level of training between programs with high volume thoracic surgery versus those without?
DR KANSIER: Thank you. Absolutely that is a great idea. With this national data set, it is impossible to differentiate numbers on an institutional level, but it would be very interesting to separate the ones with fellowship training programs and those without.
DR GANGADHARAN: I think a great corollary to this study would be to look at the incoming cardiothoracic trainees and find out how they matched compared to the numbers that you generated from the big pool of that fifth time period. It seems to me that one of the things that trainees are doing, like you suggest, is picking and choosing their cases much more carefully when they have the opportunity, and people who are motivated to go into a particular field are very aware of the limitations now because the 80-hour work week is a much more mature concept, and so with that in mind, they direct their learning; ie, their case selection with that.
DR KANSIER: Absolutely. Thank you.
DR ANDREA J. CARPENTER (San Antonio, TX): I think it would also be of interest to look at the case breakdown being logged; exploration, wedge, lobectomy, or pneumonectomy. Has there been a shift over time there with more tendency towards exploration versus more complex procedures. The American Board of Surgery still has the same case number requirement for exposure to thoracic cases, so those cases will somehow be met by the residents. I wonder whether you will find many more of the cases are exploration, and that the residents are not doing formal thoracic cases on a thoracic service, but are logging trauma cases where they went into the chest and logged the cases as thoracic exploration to make their numbers. Do you have a sense of that breakdown of formal resections versus chest explorations?
DR KANSIER: Right now, currently, they are still logging exploratory trauma separately under Trauma Operative Surgery, for which the requirement is 10 cases. For thoracic surgery, as you mentioned, the requirement is 15 cases, which has not changed over the time period of study. I think residents are actually having a harder time meeting their operative trauma requirements and may end up logging those open exploratory thoracotomies under the trauma category instead. But, yes, you could in theory fudge your logging based on which cases you needed to acquire.
DR JOSEPH B. SHRAGER (Stanford, CA): I would just make the happy point that the applicants at thoracic-track programs this year seem to be very good, and there are lots of them. Maybe that has something to do with the fact that the experience in thoracic surgery for general surgery residents has remained at least relatively stable. I think we all have to be involved with our general surgery program directors at the academic institutions and make sure that we do not lose exposure for general surgery residents, because it is clearly during those rotations people decide that they are going to go into thoracic, at least noncardiac thoracic, and it is an experience that has to be maintained or the subspecialty will be in big trouble.
DR KANSIER: Absolutely. Thank you.
Footnotes
Presented at the Fiftieth Annual Meeting of The Society of Thoracic Surgeons, Orlando, FL, Jan 25–29, 2014.
References
- 1.Pellegrini CA. Surgical education in the United States: navigating the white waters. Ann Surg. 2006;244:335–342. doi: 10.1097/01.sla.0000234800.08200.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung R, Ahmed N, Chen P. Meeting the 80-hour work week requirement: what did we cut? Curr Surg. 2004;61:609–611. doi: 10.1016/j.cursur.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Lewis FR, Klingensmith ME. Issues in general surgery residency training- 2012. Ann Surg. 2012;256:553–559. doi: 10.1097/SLA.0b013e31826bf98c. [DOI] [PubMed] [Google Scholar]
- 4.Eckert M, Cuadrado D, Steele S, Brown T, Beekley A, Martin M. The changing face of the general surgeon: national and local trends in resident operative experience. Am J Surg. 2010;199:652–656. doi: 10.1016/j.amjsurg.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Vaporciyan AA, Yang SC, Baker CJ, Fann JI, Verrier ED. Cardiothoracic surgery residency training: past, present and future. J Thorac Cardiovasc Surg. 2013;146:759–767. doi: 10.1016/j.jtcvs.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR., Jr Operative experience of surgery residents: trends and challenges. J Surg Educ. 2013;70:783–788. doi: 10.1016/j.jsurg.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 7.Mendoza KA, Britt LD. Resident operative experience during the transition to work-hour reform. Arch Surg. 2005;140:137–145. doi: 10.1001/archsurg.140.2.137. [DOI] [PubMed] [Google Scholar]
- 8.Gow KW, Drake FT, Aarabi S, Waldhausen JH. The ACGME case log: general surgery resident experience in pediatric surgery. J Pediatr Surg. 2013;48:1643–1649. doi: 10.1016/j.jpedsurg.2012.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reed MF, Lucia MW, Starnes SL, Merrill WH, Howington JA. Thoracoscopic lobectomy: Introduction of a new technique into a thoracic surgery training program. J Thorac Cardiovasc Surg. 2008;136:376–381. doi: 10.1016/j.jtcvs.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258:440–449. doi: 10.1097/SLA.0b013e3182a191ca. [DOI] [PubMed] [Google Scholar]
- 11.Hedrick T, Turrentine F, Sanfey H, Schirmer B, Friel C. Implications of laparoscopy on surgery residency training. Am J Surg. 2009;197:73–75. doi: 10.1016/j.amjsurg.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 12.Namias N, McKenney MG, Sleeman D, Hutson DG. Trends in resident experience in open and laparoscopic cholecystectomy. Surg Laparosc Endosc. 1997;7:245–247. [PubMed] [Google Scholar]
- 13.Drake FT, Horvath KD, Goldin AB, Gow KW. The general surgery chief resident operative experience: 23 years of national ACGME case logs. JAMA Surg. 2013;148:841–847. doi: 10.1001/jamasurg.2013.2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unawane A, Kamyab A, Patel M, Flynn JC, Mittal VK. Changing paradigms in minimally invasive surgery training. Am J Surg. 2013;205:284–288. doi: 10.1016/j.amjsurg.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Park A, Kavic SM, Lee TH, Heniford BT. Minimally invasive surgery: the evolution of fellowship. Surgery. 2007;142:505–513. doi: 10.1016/j.surg.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Decker MR, Dodgion CM, Kwok AC, et al. Specialization and the current practices of general surgeons. J Am Coll Surg. 2014;218:8–15. doi: 10.1016/j.jamcollsurg.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritchie WP, Jr, Rhodes RS, Biester TW. Workloads and practice patterns of general surgeons in the United States, 1995–1997: a report from the American board of surgery. Ann Surg. 1999;230:533–542. doi: 10.1097/00000658-199910000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valentine RJ, Jones A, Biester TW, Cogbill TH, Borman KR, Rhodes RS. General surgery workloads and practice patterns in the United States, 2007 to 2009: a 10-year update from the American board of surgery. Ann Surg. 2011;254:520–525. doi: 10.1097/SLA.0b013e31822cd175. [DOI] [PubMed] [Google Scholar]
- 19.Salazar JD, Lee R, Wheatley GH, III, Doty JR. Are there enough jobs in cardiothoracic surgery? The thoracic surgery residents association job placement survey for finishing residents. Ann Thorac Surg. 2004;78:1523–1527. doi: 10.1016/j.athoracsur.2004.05.068. [DOI] [PubMed] [Google Scholar]
- 20.Shemin RJ, Ikonomidis JS. Thoracic surgery workforce: report of STS/AATS thoracic surgery practice and access task force–snapshot 2010. J Thorac Cardiovasc Surg. 2012;143:39–46. e31–e36. doi: 10.1016/j.jtcvs.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 21.Williams TE, Jr, Satiani B, Thomas A, Ellison EC. The impending shortage and the estimated cost of training the future surgical workforce. Ann Surg. 2009;250:590–597. doi: 10.1097/SLA.0b013e3181b6c90b. [DOI] [PubMed] [Google Scholar]
- 22.Baumgartner WA. Retooling thoracic surgery education for the 21st century. Ann Thorac Surg. 1998;65:13–16. doi: 10.1016/s0003-4975(97)01312-x. [DOI] [PubMed] [Google Scholar]
- 23.Pousatis SM, Marshall MB. Trends in applications for thoracic fellowship in comparison with other subspecialties. Ann Thorac Surg. 2014;97:624–632. doi: 10.1016/j.athoracsur.2013.08.073. [DOI] [PubMed] [Google Scholar]
- 24.Allen JG, Weiss ES, Patel ND, et al. Inspiring medical students to pursue surgical careers: outcomes from our cardiothoracic surgery research program. Ann Thorac Surg. 2009;87:1816–1819. doi: 10.1016/j.athoracsur.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Rusch VW, Calhoon JH, Allen MS, Baumgartner W. The American board of thoracic surgery: update. J Thorac Cardiovasc Surg. 2012;143:519–521. doi: 10.1016/j.jtcvs.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 26.Cooke DT, Kerendi F, Mettler BA, et al. Update on cardiothoracic surgery resident job opportunities. Ann Thorac Surg. 2010;89:1853–1858. doi: 10.1016/j.athoracsur.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 27.Kim AW, Reddy RM, Higgins RS. Joint Council for Thoracic Surgical Education Subcommittee Best and Brightest “Back to the future”: recruiting the best and brightest into cardiothoracic surgery. J Thorac Cardiovasc Surg. 2010;140:503–504. doi: 10.1016/j.jtcvs.2010.05.028. [DOI] [PubMed] [Google Scholar]
- 28.Vaporciyan AA, Reed CE, Erikson C, et al. Factors affecting interest in cardiothoracic surgery: survey of North American general surgery residents. J Thorac Cardiovasc Surg. 2009;137:1054–1062. doi: 10.1016/j.jtcvs.2009.03.044. [DOI] [PubMed] [Google Scholar]
- 29.Sarkaria IS, Carr SR, MacIver RH, et al. The 2010 Thoracic Surgery Residents Association workforce survey report: a view from the trenches. Ann Thorac Surg. 2011;92:2062–2070. doi: 10.1016/j.athoracsur.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 30.Verrier ED. Joint Council on Thoracic Surgical Education: an investment in our future. J Thorac Cardiovasc Surg. 2011;141:318–321. doi: 10.1016/j.jtcvs.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 31.Chikwe J, Brewer Z, Goldstone AB, Adams DH. Integrated thoracic residency program applicants: the best and the brightest? Ann Thorac Surg. 2011;92:1586–1591. doi: 10.1016/j.athoracsur.2011.05.107. [DOI] [PubMed] [Google Scholar]
- 32.Gasparri MG, Tisol WB, Masroor S. Impact of a six-year integrated thoracic surgery training program at the Medical College of Wisconsin. Ann Thorac Surg. 2012;93:592–595. doi: 10.1016/j.athoracsur.2011.11.005. [DOI] [PubMed] [Google Scholar]