Abstract
Previous studies investigating the relationship between affective state and community integration have focused primarily on the influence of depression and anxiety. Additionally, they have focused on frequency of participation in various activities, failing to address an individual's subjective satisfaction with participation. The purpose of this study was to examine how affective state, contributes to frequency of participation and satisfaction with participation after TBI among participants with and without a current major depressive episode. Sixty-four community-dwelling participants with a history of complicated mild to severe TBI participated in this cross-sectional cohort study. High positive affect contributed significantly to frequency of participation (β=.401, p=.001), and both high positive affect and low negative affect significantly contributed to better satisfaction with participation (F2,61=13.63, p<.001). Further investigation to assess the direction of these relationships may better inform effective targets for intervention. These findings highlight the importance of assessing affective state after TBI and incorporating a subjective measure of participation when considering community integration outcomes.
Keywords: Brain Injuries, Community Integration, Affect
INTRODUCTION
Individuals with traumatic brain injuries (TBI) often experience poor community integration, including decreased participation, social integration, and satisfaction with life, even in the absence of significant physical and cognitive impairment1–3. Numerous studies have reported the relationship between depression, anxiety, or psychosocial distress and poor psychosocial and community integration outcomes after TBI4–11. Additionally, community integration is directly associated with self-esteem and coping12,13. Both positive and negative affect have been considered as important components of subjective well-being14 and have been found to contribute to quality of life15 after TBI. Combined, this prior evidence highlights the importance of considering both positive and negative affect when assessing long-term outcomes after TBI.
Affect refers to emotional reactions to specific experiences16. Negative affect includes irritability, fear, and distress, and poor negative affect may manifest in depression or anxiety. Positive affect includes interest, energy, and pride, and poor positive affect may manifest in depression, low self-esteem, or poor coping. While poor (low positive, high negative) affect is a component of depressive disorders, evidence suggests that it may persist even when depressive disorders are treated and in current remission17. Therefore, while overlapping with clinical mood disorders, like depression, poor affect is a distinct construct that may contribute independently to community integration after TBI.
Previous studies investigating the relationship between affective state and community integration have focused primarily on depression or anxiety. However, high negative affect (e.g. feelings of nervousness, guilt, fear, irritability) may be present after TBI, even in the absence of these clinical syndromes17. Low positive affect may also represent early depressive symptoms, prior to the development to a clinical syndrome, as low positive affect is the hallmark symptom of depression18. Additionally, community integration after TBI has traditionally been measured through objective outcomes, such as return to work19,20. More recent research strongly suggests that measuring the individual's perspective of community integration19–23, by assessing satisfaction with participation in household, family, community, and societal activities. Thus, by examining both the objective (frequency) and subjective (satisfaction) perspectives, we gain a more holistic understanding of the relationships between affective state and community integration after TBI.
The purpose of this study was to assess the relationship between affective state, incorporating both positive affect and negative affect and community integration, measured by the frequency of participation in household, social, and productive activities, and satisfaction with this participation. We hypothesized that positive affect would be significantly positively associated with frequency of participation and satisfaction with participation and that negative affect would be significantly negatively associated with satisfaction with participation (but not frequency of participation). A clearer understanding of these relationships may inform clinical practice and provide meaningful and effective targets for client-centered and personalized interventions.
METHODS
This was a cross-sectional cohort study of adults with a history of complicated mild to severe traumatic brain injury (TBI). Sixty-five participants provided written informed consent and completed interviews and assessments to describe the sample and to measure community integration and positive and negative affect.
Participants
Individuals were recruited through existing collaborations with previous research studies, through a University Medical Center Research Registry, and through local agencies and support groups for individuals with TBI. All research procedures were approved by a University Institutional Review Board.
Individuals were included if they demonstrated evidence of a complicated mild to severe traumatic brain injury (Glasgow Coma Scale score of 3-12 or >13 with positive neuroradiologic findings or admission to inpatient rehabilitation or specialized rehabilitative services (TBI Day Program)) sustained longer than 6 months ago, were 18 years old or older, and lived in a private or group residential setting. Individuals were excluded if they had a history of any other condition resulting in progressive cognitive decline (e.g. dementia), current active psychotic or bipolar disorder, or were currently involved in injury-related litigation.
Measures
Descriptive Measures
We collected demographic and injury-related data to describe the sample, through interviews with participants and their family members and medical record review. Depression status was assessed with the Primary Care Evaluation of Mental Disorders (PRIME-MD) depression module24, which includes the same nine items as Patient Health Questionnaire-9, a tool which has been validated in TBI25. Participants were categorized, based on previously established criteria after TBI11,25, into four groups: Current Major Depressive Episode, Current Minor Depression Episode, History but No Current Depressive Episode, and No History of Depressive Episode. We assessed self-awareness with the Self Regulation of Skills Interview (SRSI) Awareness subscale, to control for the potential contribution of impairments in self-awareness. The SRSI has been validated as a measure of self-awareness for individuals with TBI26. Finally, we measured cognition using a cognitive composite score calculated by taking an average of T-scores from the following neuropsychological tests: California Verbal Learning Test II total trials 1-5, Trail Making Test A time, Trail Making Test B time, Symbol Digit Modalities Test total, FAS and Animals total fluency, and Wisconsin Card Sorting Test perseverative errors. Higher T-scores indicated better cognitive functioning. These tests are part of the neuropsychological battery validated by the TBI Model System Centers27, and they represent distinct domains of cognitive functioning commonly affected by TBI. Creation of a cognitive composite score as an single measure of cognition has been previously validated in TBI28–30.
Community Integration
Community Integration was measured using the Participation Assessment of Recombined Tools, Objective (PART-O; Frequency of Participation) and Satisfaction (PART-S; Satisfaction with Participation). The PART-O consists of 24 items that measure frequency of engagement in various activities of the household, family, community, and wider society. A total score is calculated measuring a person's level of participation. The PART-S addresses the subjective importance of 11 domains of participation. Domains are rated first as low, medium, or high importance, and then level of satisfaction is rated on a 0-10 point scale for domains of medium or high importance. An average weighted satisfaction score is calculated based on these ratings. The PART-O is an established measure that has been validated and is being used as the gold standard participation measure in the TBI Model Systems31,32. The PART-S is included as a measure of subjective community integration, to capture the individual perspective with regard to participation33.
Positive Affect and Negative Affect
Affect was measured using the Positive and Negative Affect Schedule (PANAS), a valid and reliable measure of affect, which has been previously used in TBI14,15, that consists of two 10-item affect scales: Positive Affect and Negative Affect34. Each subscale includes 10 items rated on a five-point scale and yielding total scores for Positive Affect and for Negative Affect (ranges 10-50). Higher scores on the Positive Affect scale indicate high energy, concentration, and pleasurable engagement, whereas low scores indicate sadness and lethargy. Higher scores on the Negative Affect scale indicate high anger, disgust, guilt, fear, or nervousness, whereas low scores indicate calmness and serenity34.
Statistical Analyses
Statistical analyses were performed using SPSS20.0™ for Windows. We first examined descriptive statistics, including means and standard deviations for continuous variables and frequencies and percentiles for categorical variables. We then examined correlations among the variables of interest to determine what factors should be controlled for in the final regression models. Finally, we conducted consecutive linear regressions to determine the contribution of affective state (positive affect and negative affect) to community integration (frequency of participation and satisfaction with participation).
RESULTS
Recruitment
Of 115 individuals who initially responded to advertisement or were contacted to participate in the study, 71 were found to be eligible after initial telephone screening; 26 individuals were not interested in research, five did not meet injury severity criteria, 3 had passed away, 2 were currently involved in litigation, and 8 were not eligible for other reasons. Seventy participants provided informed consent, of which 65 were found to be eligible and completed study assessments. Two individuals had untreated active psychotic symptoms and three did not meet the injury severity criterion. One participant failed to complete the PANAS. Therefore, 64 participants were included in the final analyses.
Descriptive Data
Descriptive data for this sample are presented in Table 1.
Table 1.
Descriptive data
| n | % | |
|---|---|---|
| Gender (male) | 51 | 78 |
| Race (white) | 62 | 97 |
| Injury Severityξ | ||
| Complicated Mild (GCS=13-15) | 20 | 31.3 |
| Moderate (GCS=9-12) | 13 | 20.3 |
| Severe (GCS < = 3) | 31 | 48.4 |
| Time Since Injury | ||
| < 2 years | 24 | 37.5 |
| 2-5 years | 11 | 17.2 |
| >5 years | 29 | 45.3 |
| Depression Status | ||
| No History of Depression | 21 | 32.8 |
| History of Depressive Episode | 29 | 45.3 |
| Current Major/Minor Depressive Episode | 14 | 21.9 |
| Mean (SD) | Range | |
| Age (years) | 46.14 (16.56) | 18-86 |
| Education (years) | 14.67 (2.63) | 10-20 |
| Frequency of Participation (PART-O) | 1.97 (0.51) | 0.70-3.26 |
| Satisfaction with Participation (PART-S) | 11.38 (3.45) | 1.22-17.55 |
| Affective State (PANAS) | ||
| Positive Affect | 32.67 (7.77) | 10-48 |
| Negative Affect* | 18.80 (6.77) | 10-35 |
| Self Awareness (SRSI) Awareness Subscale* | 7.56 (4.79) | 0-20 |
| Cognition (cognitive composite T-score) | 44.73 (12.04) | -9-60 |
Higher scores indicate poorer functioning
Based on Glasgow Coma Scale (GCS) score at time of injury †Median, inter-quartile range GCS=Glasgow Coma Scale; PART-O=Participation Assessment with Recombined Tools –Objective; PART-S=Participation Assessment with Recombined Tools -Subjective; PANAS=Positive and Negative Affect Schedule; SRSI=Self Regulation Skills Interview
With regard to affective state, compared to a sample from the general population (n=1,003) who demonstrated average positive affect of 31.31 (7.65) and negative affect of 16 (5.9; Crawford & Henry, 2004), the present sample had similar positive affect (M=32.67, SD=7.77) and slightly higher negative affect (M=18.80, SD=6.77).
Correlations
All correlations are presented in Table 2. Of note, frequency of participation was significantly correlated with positive affect (r=.372, p<.001), self-awareness (r=-.277, p=.027), and cognition (r=.397, p=.001). Satisfaction with participation was significantly correlated with positive affect (r=.504, p<.001) and negative affect (r=−.391, p=.001). Frequency of participation and satisfaction with participation were significantly correlated with each other (r=.438, p<.001).
Table 2.
Pearson Correlations (Spearman Correlations**)
| 2. | 3. | 4. | 5. | 6.** | 7.** | 8.** | ||
|---|---|---|---|---|---|---|---|---|
| 1. | Frequency of Participation - PART-O | .438‡ | .372‡ | −.043 | −.277* | .394† | .063 | −.028 |
| 2. | Satisfaction with Participation – PART-S | .504‡ | −.391† | .119 | .072 | −.013 | −.226 | |
| 3. | Positive Affect – PANAS | −.337* | .036 | .071 | .100 | .037 | ||
| 4. | Negative Affect – PANAS | −.283* | .110 | −.112 | .071 | |||
| 5. | Awareness – SRSI | −.432 | .027 | .212 | ||||
| 6. | Cognition Composite Score** | −.091 | −.331† | |||||
| 7. | Time Since Injury** | .193 | ||||||
| 8. | Injury Severity at time of injury** |
p <.05 ;
p < .01 ;
p <.001 PART-O=Participation Assessment with Recombined Tools – Objective; PART-S=Participation Assessment with Recombined Tools – Satisfaction; PANAS=Positive and Negative Affect Schedule; SRSI=Self Regulation Skills Interview
Regressions
Two separate consecutive linear regressions were conducted to examine the contribution of affective state (positive affect and negative affect) to community integration (frequency of participation and satisfaction with participation). Given that frequency of participation was also significantly correlated with self-awareness and cognition, these variables were controlled for in the final model. Satisfaction with participation was not significantly correlated with any other factor measured, but did differ by depression status (F2,62=6.70, p=.002); therefore, depression status was included as a potential covariate. The contributions of positive affect and negative affect to frequency of participation and to satisfaction with participation are summarized in Tables 3 and 4, respectively.
Table 3.
The contributions of positive affect and negative affect to frequency of participation
| Frequency of Participation | Model 1: Positive Affect (n=64) | Model 2: Negative Affect (n=64) | Model 3: Positive Affect x Cognition Interaction (n=64) | |||||
|---|---|---|---|---|---|---|---|---|
| Bstand | P | BStand | P | B | P | |||
| Intercept | - | - | Intercept | - | - | - | - | |
| Self-awareness | –.109 | .375 | Self-awareness | –.106 | .409 | Self-awareness | –.018 | .186 |
| Cognition | .366 | .004 | Cognition | .367 | .004 | Cognition Group | .848 | .109 |
| Positive Affect | .398 | .000 | Positive Affect | .401 | .001 | Positive Affect | .034 | .001 |
| Negative Affect | .011 | .026 | Positive Affect x Cognition Group* | .034 | .034 | |||
| R2=.32 | <.001 | R2=.32 | <.001 | R2=.29 | .001 | |||
| R2Adj=.29 | R2Adj=.28 | R2Adj=.24 | ||||||
Cognition Group: For the interaction, cognition was dichotomized at >1standard deviation below the mean on the cognitive composite score. Those with cognitive impairment (>1SD below the mean) are the referent group.
Table 4.
The contributions of positive affect and negative affect to satisfaction with participation
| Satisfaction with Participation | Model 1: Positive Affect (n=64) | Model 2: Negative Affect (n=64) | Model 3: Depression Status (n=64) | |||||
|---|---|---|---|---|---|---|---|---|
| Bstand | P | Bstand | P | Bstand | P | |||
| Intercept | - | - | Intercept | - | - | Intercept | - | |
| Positive Affect | .504 | <.001 | Positive Affect | .420 | <.001 | Positive Affect | .375 | .002 |
| Negative Affect | –.249 | .031 | Negative Affect | –.185 | .129 | |||
| Depression status | –.180 | .144 | ||||||
| R2=.25 | <.001 | R2=.31 | <.001 | R2=.33 | <.001 | |||
| R2Adj=.24 | R2Adj=.29 | R2 Adj =.30 | ||||||
Overall, positive affect, negative affect, self-awareness, and cognition together explained 28% of the variance in frequency of participation (F4,59=7.06, p<.001). Of this 28%, positive affect alone accounted for 16% of the variance in frequency of participation (F1,60 Δ=13.97,p<.001), based on the change in the R2 value from a base model (data not shown) to Model 1 (see Table 3). Positive affect (standardized β=.401, p=.001) and cognition (standardized β=.367, p=.004) were the only significant independent predictors of frequency of participation, when controlling for all other factors. To further explore this relationship, the interaction between positive affect and cognition was assessed in Model 3 (see Table 3). Cognition was dichotomized into those with and without cognitive impairment, based on a cut-off of 1 standard deviation below the mean for the cognitive composite score. The interaction was found to be significant after controlling for self-awareness (β=.034, p=.034). The relationship between positive affect and frequency of participation was only present among those with no cognitive impairment (R2=0.24) and not among those with cognitive impairment (R2=.001).
Positive affect and negative affect explained 29% of the variance in satisfaction with participation (F2,61=13.63, p<.001), and both were significant independent predictors of satisfaction with participation (standardized β=.420, p<.001 and standardized β=−.249, p=.031, respectively; see Table 4). Adding depression status to the model negated the statistical significant of negative affect (p=.129), and depression status was also not a statistically significant contributing factor (p=.144). However, this may be an effect of the sample size and should be validated in a larger sample. Positive affect remained a statistically significant contributor to satisfaction with participation (p=.002). Participants with a current major depressive episode reported higher negative affect and lower positive affect than those with no history of depression, but the distribution of affect scores varied greatly in the group of participants with a history of depression with no current depressive episode (see Figure 1).
Figure 1.
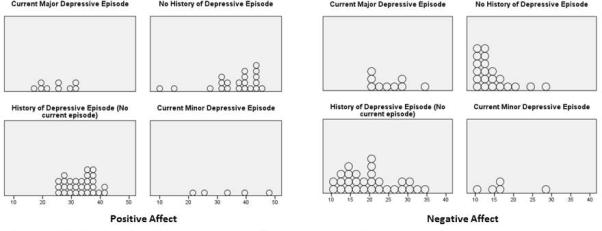
Distribution of positive and negative affect across depressive statis groups
DISCUSSION
The purpose of this study was to examine the association between positive affect and negative affect and community integration, defined as frequency of participation in activities of the household, community, and wider society, and satisfaction with participation.
High positive affect was significantly associated with high frequency of participation, after controlling for negative affect, self-awareness, and cognition. High positive affect, as measured by the PANAS34, includes emotions such as interest, pride, alertness, and determination. Individuals experiencing these emotions may be more motivated to participate in activities and may push through barriers to participation. Conversely, it is possible that participating more frequently in activities may lead to increased positive affect. Given that cognition was also a significant predictor of frequency of participation, the interaction between positive affect and cognition was also explored. It was found that, even after controlling for self-awareness, the relationship between positive affect and frequency of participation was only present among those without cognitive impairment. This is an important consideration for future research and clinical practice related to participation. Again, the direction of the relationship between positive affect and frequency of participation could not be assessed, limited the ability to interpret the effects of cognitive impairment – whether having cognitive impairment prevented those with high positive affect from participating more or whether having cognitive impairment negated the effects of participation on positive affect. Additionally, the effect sizes were small; therefore, validation of this finding in future studies is necessary.
Negative affect was not an independent predictor of frequency of participation. This indicates that neither feelings of anger, nervousness, or guilt, nor feelings of calmness or serenity34 were associated with how frequently individuals participated in community-based activities. Previous literature suggests that frequency-based measures of community integration are associated with depression, anxiety, and poor psychosocial functioning.4–10,35The absence of an association between negative affect and frequency of participation in this study supports previous findings that negative affect represents a distinct construct from anxiety and depression17,18. Furthermore, individuals may be participating frequently in community-based activities, while still experiencing high levels of negative affect, or may be participating infrequently and experiencing low levels of negative affect. This highlights the need to include a subjective measure of community integration, as objective frequency-based measures do not adequately account for an individual's subjective experience.
Both positive affect and negative affect independently contributed to satisfaction with participation. As would be expected, high satisfaction was associated with an optimal affective state. Again, the direction of these relationships – whether higher positive affect and lower negative affect lead to high satisfaction or are a result of high satisfaction – needs to be explored. Inclusion of depression status did not alter the effects of positive affect, but did wash out the effects of negative affect in the model. Furthermore, while individuals with a current major depressive episode generally report the poorest affect, there is significant overlap in the distribution of affect scores across all depression status groups. Given the sample size and the number of covariates in the model, these findings should be validated further prior to definitive interpretation. What is clear from these findings is that affective state is important to the subjective experience of community integration for individuals who have sustained a TBI.
How satisfied individuals are with their participation may be of greater importance to their overall affective state than how frequently they are participating in activities. As a result, satisfaction with participation should not only be assessed, but it also should be viewed as a viable – if not preferred – outcome measure for both rehabilitation research and practice. Satisfaction with participation is not only a more client-centered outcome, but given its association with affective state, may also be a more important outcome for preventing the development of depression, anxiety disorders, or poor health outcomes associated with these clinical syndromes.
Limitations
One limitation of the study was the assessment of affect at single time point. Affect – unlike psychiatric diagnoses – may fluctuate significantly from day to day, or even hour to hour. Multiple measurements of affect across a span of time may produce a more meaningful measure of affective traits of an individual. This is a possibility to be explored in future longitudinal studies. Given that this was a cross sectional study, no causal relationships could be determined. It remains unclear whether high positive affect leads to high frequency of participation, or whether high frequency of participation results in high positive affect. Future research should investigate the direction of the relationship between positive affect and frequency of participation. Additionally, potential confounding factors that may be related to community integration should be addressed and controlled for, such as fatigue35 and self-efficacy36 Third, the construct of community integration is complex and difficult to measure. While a significant innovation of this study was its incorporation of a subjective perspective of community integration (satisfaction with participation), the measurement of this construct is still early in its development. Though currently undergoing validation, the PART-S has not yet demonstrated its level of validity and reliability as a measure of satisfaction with participation after TBI. While powered for the research questions of interest, the sample size in this study did not allow for complex modeling including numerous covariates, such as community resources, social and family functioning, and goal attainment to be considered. These factors have been previously found to influence affect and community integration14,37–41, and therefore should be explored before these results can be generalized across multiple groups and settings.
This project is particularly timely, due to the large number of community-dwelling individuals with TBI and the growing body of research about poor community integration outcomes even in the absence of significant physical or cognitive impairment. It provides a deeper understanding of factors that contribute to community integration by investigating alternative explanations for poor outcomes, such as positive and negative affect. More importantly, these findings support the argument for including a broad conceptualization of community integration and the idea that contextual factors – both personal and environmental – are necessary to account for in community integration research.
Significance.
The prevalence of TBI continues to grow, with an ever-increasing number of individuals experiencing long-term negative consequences as a result. As the goals of rehabilitation and healthcare continue to shift towards community-based and client-centered interventions and services, understanding community integration from both an objective and subjective perspective becomes increasingly important. The findings of this study highlight the need to develop effective interventions to improve affective state and community integration after TBI and to evaluate effectiveness from both objective and subjective perspectives.
Acknowledgments
This study was supported in part through funding received from the School of Health and Rehabilitation Science Research Development Fund, School and Health of Rehabilitation Science, University of Pittsburgh, by the NIH NCMRR/NINDS K12 HD 055931, and by the U.S. Army Medical Research and Material Command under Award No. W81XWH-10-1-0920. Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the U.S. Army.
Footnotes
Disclosures:
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
REFERENCES
- 1.Cicerone KD, Azulay J. Perceived self-efficacy and life satisfaction after traumatic brain injury. J Head Trauma Rehabil. 2007;22(5):257–266. doi: 10.1097/01.HTR.0000290970.56130.81. doi:10.1097/01.HTR.0000290970.56130.81. [DOI] [PubMed] [Google Scholar]
- 2.Temkin NR, Corrigan JD, Dikmen SS, Machamer J. Social functioning after traumatic brain injury. J Head Trauma Rehabil. 2009;24(6):460–467. doi: 10.1097/HTR.0b013e3181c13413. doi:10.1097/HTR.0b013e3181c13413. [DOI] [PubMed] [Google Scholar]
- 3.Stålnacke B-M, Elgh E, Sojka P. One-year follow-up of mild traumatic brain injury: cognition, disability and life satisfaction of patients seeking consultation. J Rehabil Med Off J UEMS Eur Board Phys Rehabil Med. 2007;39(5):405–411. doi: 10.2340/16501977-0057. doi:10.2340/16501977-0057. [DOI] [PubMed] [Google Scholar]
- 4.Anson K, Ponsford J. Coping and emotional adjustment following traumatic brain injury. J Head Trauma Rehabil. 2006;21(3):248–259. doi: 10.1097/00001199-200605000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Felmingham KL, Baguley IJ, Crooks J. A comparison of acute and postdischarge predictors of employment 2 years after traumatic brain injury. Arch Phys Med Rehabil. 2001;82(4):435–439. doi: 10.1053/apmr.2001.21985. doi:10.1053/apmr.2001.21985. [DOI] [PubMed] [Google Scholar]
- 6.Hoofien D, Gilboa A, Vakil E, Donovick PJ. Traumatic brain injury (TBI) 10-20 years later: a comprehensive outcome study of psychiatric symptomatology, cognitive abilities and psychosocial functioning. Brain Inj BI. 2001;15(3):189–209. doi: 10.1080/026990501300005659. doi:10.1080/026990501300005659. [DOI] [PubMed] [Google Scholar]
- 7.Jorge RE, Robinson RG, Arndt SV, Starkstein SE, Forrester AW, Geisler F. Depression following traumatic brain injury: a 1 year longitudinal study. J Affect Disord. 1993;27(4):233–243. doi: 10.1016/0165-0327(93)90047-n. [DOI] [PubMed] [Google Scholar]
- 8.Morton MV, Wehman P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: a literature review and recommendations. Brain Inj BI. 1995;9(1):81–92. doi: 10.3109/02699059509004574. [DOI] [PubMed] [Google Scholar]
- 9.Ownsworth T, Fleming J. The relative importance of metacognitive skills, emotional status, and executive function in psychosocial adjustment following acquired brain injury. J Head Trauma Rehabil. 2005;20(4):315–332. doi: 10.1097/00001199-200507000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Ruff RM, Marshall LF, Crouch J, et al. Predictors of outcome following severe head trauma: follow-up data from the Traumatic Coma Data Bank. Brain Inj BI. 1993;7(2):101–111. doi: 10.3109/02699059309008164. [DOI] [PubMed] [Google Scholar]
- 11.Hart T, Brenner L, Clark AN, et al. Major and minor depression after traumatic brain injury. Arch Phys Med Rehabil. 2011;92(8):1211–1219. doi: 10.1016/j.apmr.2011.03.005. doi:10.1016/j.apmr.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Lubusko AA, Moore AD, Stambrook M, Gill DD. Cognitive beliefs following severe traumatic brain injury: association with post-injury employment status. Brain Inj BI. 1994;8(1):65–70. doi: 10.3109/02699059409150959. [DOI] [PubMed] [Google Scholar]
- 13.Tate RL, Broe GA. Psychosocial adjustment after traumatic brain injury: what are the important variables? Psychol Med. 1999;29(3):713–725. doi: 10.1017/s0033291799008466. [DOI] [PubMed] [Google Scholar]
- 14.Conrad N, Doering BK, Rief W, Exner C. Looking beyond the importance of life goals. The personal goal model of subjective well-being in neuropsychological rehabilitation. Clin Rehabil. 2010;24(5):431–443. doi: 10.1177/0269215509358930. doi:10.1177/0269215509358930. [DOI] [PubMed] [Google Scholar]
- 15.Man DWK, Lee EWT, Tong ECH, Yip SCS, Lui WF, Lam CS. Health services needs and quality of life assessment of individuals with brain injuries: a pilot cross-sectional study. Brain Inj BI. 2004;18(6):577–591. doi: 10.1080/02699050310001646143. doi:10.1080/02699050310001646143. [DOI] [PubMed] [Google Scholar]
- 16.Payne RL, Cooper CL. Emotions at Work: Theory, Research and Applications for Management. John Wiley & Sons; 2003. [Google Scholar]
- 17.Juengst SB, Arenth PM, Whyte EM, Skidmore ER. Brief report of mood state and depression status after traumatic brain injury. doi: 10.1037/a0036294. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 19.Brown SA, McCauley SR, Levin HS, Contant C, Boake C. Perception of Health and Quality of Life in Minorities After Mild-to-Moderate Traumatic Brain Injury. Appl Neuropsychol. 2004;11(1):54–64. doi: 10.1207/s15324826an1101_7. doi:10.1207/s15324826an1101_7. [DOI] [PubMed] [Google Scholar]
- 20.Sander AM, Clark A, Pappadis MR. What is community integration anyway?: defining meaning following traumatic brain injury. J Head Trauma Rehabil. 2010;25(2):121–127. doi: 10.1097/HTR.0b013e3181cd1635. doi:10.1097/HTR.0b013e3181cd1635. [DOI] [PubMed] [Google Scholar]
- 21.Cicerone KD. Participation as an outcome of traumatic brain injury rehabilitation. J Head Trauma Rehabil. 2004;19(6):494–501. doi: 10.1097/00001199-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Mascialino G, Hirshson C, Egan M, et al. Objective and subjective assessment of long-term community integration in minority groups following traumatic brain injury. NeuroRehabilitation. 2009;24(1):29–36. doi: 10.3233/NRE-2009-0451. doi:10.3233/NRE-2009-0451. [DOI] [PubMed] [Google Scholar]
- 23.Johnston MV, Goverover Y, Dijkers M. Community activities and individuals’ satisfaction with them: quality of life in the first year after traumatic brain injury. Arch Phys Med Rehabil. 2005;86(4):735–745. doi: 10.1016/j.apmr.2004.10.031. doi:10.1016/j.apmr.2004.10.031. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA J Am Med Assoc. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 25.Fann JR, Bombardier CH, Dikmen S, et al. Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. J Head Trauma Rehabil. 2005;20(6):501–511. doi: 10.1097/00001199-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Ownsworth TL, McFarland KM, Young RM. Development and standardization of the Self-regulation Skills Interview (SRSI): a new clinical assessment tool for acquired brain injury. Clin Neuropsychol. 2000;14(1):76–92. doi: 10.1076/1385-4046(200002)14:1;1-8;FT076. doi:10.1076/1385-4046(200002)14:1;1-8;FT076. [DOI] [PubMed] [Google Scholar]
- 27.Hanks RA, Millis SR, Ricker JH, et al. The predictive validity of a brief inpatient neuropsychologic battery for persons with traumatic brain injury. Arch Phys Med Rehabil. 2008;89(5):950–957. doi: 10.1016/j.apmr.2008.01.011. doi:10.1016/j.apmr.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Hartikainen KM, Waljas M, Isoviita T, et al. Persistent symptoms in mild to moderate traumatic brain injury associated with executive dysfunction. J Clin Exp Neuropsychol. 2010;32(7):767–774. doi: 10.1080/13803390903521000. doi:10.1080/13803390903521000. [DOI] [PubMed] [Google Scholar]
- 29.Green RE, Colella B, Hebert DA, et al. Prediction of return to productivity after severe traumatic brain injury: investigations of optimal neuropsychological tests and timing of assessment. Arch Phys Med Rehabil. 2008;89(12 Suppl):S51–60. doi: 10.1016/j.apmr.2008.09.552. doi:10.1016/j.apmr.2008.09.552. [DOI] [PubMed] [Google Scholar]
- 30.Hart T, Whyte J, Kim J, Vaccaro M. Executive function and self-awareness of “real-world” behavior and attention deficits following traumatic brain injury. J Head Trauma Rehabil. 2005;20(4):333–347. doi: 10.1097/00001199-200507000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Mount Sinai School of Medicine Department of Rehabilitation Medicine PART-OS Interviewer Manual. 2007 [Google Scholar]
- 32.Whiteneck GG, Dijkers MP, Heinemann AW, et al. Development of the participation assessment with recombined tools-objective for use after traumatic brain injury. Arch Phys Med Rehabil. 2011;92(4):542–551. doi: 10.1016/j.apmr.2010.08.002. doi:10.1016/j.apmr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Dijkers M, Cicerone KD, Heinemann A, Brown M, Whiteneck G. Poster 89: PART-S: A new measure of satisfaction with participation. Arch Phys Med Rehabil. 2009;90(10):e39. [Google Scholar]
- 34.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 35.Juengst S, Skidmore E, Arenth PM, Niyonkuru C, Raina KD. Unique contribution of fatigue to disability in community-dwelling adults with traumatic brain injury. Arch Phys Med Rehabil. 2013;94(1):74–79. doi: 10.1016/j.apmr.2012.07.025. doi:10.1016/j.apmr.2012.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dumont C, Gervais M, Fougeyrollas P, Bertrand R. [Perceived self-efficacy is associated with social participation in adults with traumatic brain injury]. Can J Occup Ther Rev Can Ergothérapie. 2005;72(4):222–233. doi: 10.1177/000841740507200404. [DOI] [PubMed] [Google Scholar]
- 37.Struchen MA, Davis LC, Bogaards JA, et al. Making connections after brain injury: development and evaluation of a social peer-mentoring program for persons with traumatic brain injury. J Head Trauma Rehabil. 2011;26(1):4–19. doi: 10.1097/HTR.0b013e3182048e98. doi:10.1097/HTR.0b013e3182048e98. [DOI] [PubMed] [Google Scholar]
- 38.Kalpakjian CZ, Lam CS, Toussaint LL, Merbitz NKH. Describing quality of life and psychosocial outcomes after traumatic brain injury. Am J Phys Med Rehabil Assoc Acad Physiatr. 2004;83(4):255–265. doi: 10.1097/01.phm.0000118033.07952.8c. [DOI] [PubMed] [Google Scholar]
- 39.Wood RL, Rutterford NA. Demographic and cognitive predictors of long-term psychosocial outcome following traumatic brain injury. J Int Neuropsychol Soc JINS. 2006;12(3):350–358. doi: 10.1017/s1355617706060498. [DOI] [PubMed] [Google Scholar]
- 40.Dahlberg C, Hawley L, Morey C, Newman J, Cusick CP, Harrison-Felix C. Social communication skills in persons with post-acute traumatic brain injury: three perspectives. Brain Inj BI. 2006;20(4):425–435. doi: 10.1080/02699050600664574. doi:10.1080/02699050600664574. [DOI] [PubMed] [Google Scholar]
- 41.Stålnacke B-M. Community integration, social support and life satisfaction in relation to symptoms 3 years after mild traumatic brain injury. Brain Inj BI. 2007;21(9):933–942. doi: 10.1080/02699050701553189. doi:10.1080/02699050701553189. [DOI] [PubMed] [Google Scholar]


